Examining the Theoretical Relationship between Constructs in the Person-Centred Practice Framework: A Structural Equation Model
Abstract
:1. Introduction
Background
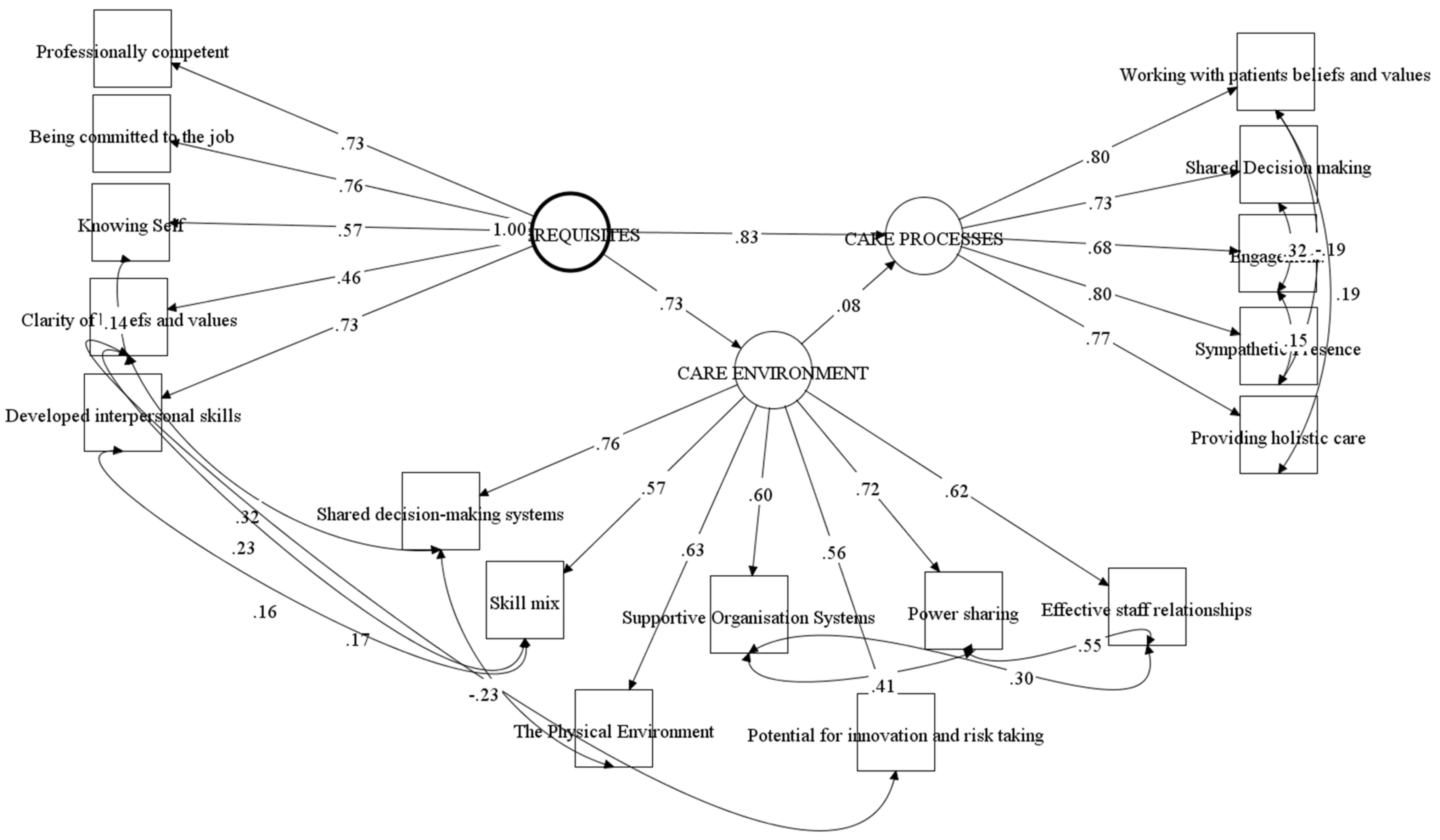
- Prerequisites focus on the attributes of staff and include: being professionally competent, having developed interpersonal skills, being committed to the job, being able to demonstrate clarity of beliefs and values, and knowing self.
- The practice environment reflects the complexity of the context in which healthcare is experienced and includes: appropriate skill mix; systems that facilitate shared decision making; the sharing of power; effective staff relationships; organisational systems that are supportive; potential for innovation and risk taking; and the physical environment.
- Person-centred processes focus on ways of engaging that are necessary to create connections between persons, which include: working with the person’s beliefs and values; engaging authentically; being sympathetically present; sharing decision making; and working holistically.
- The outcome from the development of effective person-centred practice is a healthful culture that enables human flourishing.
2. Materials and Methods
2.1. Sample
2.2. Ethical Approval
2.3. Procedure
2.4. Measurement Model
2.5. Statistical Analysis
- within factors inter-item correlated errors were permitted and based on criteria of being theoretically relevant introduced one at a time and selected on highest score first (exceeding scores of 3.98).
- across factors inter-item correlated errors were permitted and based on criteria of being theoretically relevant introduced one at a time and selected on highest score first (exceeding scores of 3.98)
- only statistically significant relationship retained to help produce as parsimonious a model as possible.
3. Results
3.1. Theoretical Framework
3.2. Correlated Error of Variances
3.3. Relationship between Second Order Latent Variables
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Global Strategy on People-Centred and Integrated Health Services; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Department of Health. Health and Well-Being 2026—Delivering Together; DoH: Belfast, UK, 2016. [Google Scholar]
- McCormack, B.; McCance, T. Person-Centred Practice in Nursing and Healthcare: Theory and Practice, 2nd ed.; Wiley-Blackwell: Oxford, UK, 2017. [Google Scholar]
- Health Foundation. Person-Centred Care Made Simple; The Health Foundation: London, UK, 2014. [Google Scholar]
- McCormack, B. Action research for the implementation of complex interventions, in DA Richards and I Rahm Hallberg. In Complex Interventions in Health: An Overview of Research Methods; Routledge: London, UK, 2015. [Google Scholar]
- Dewing, J.; McCormack, B. Editorial: Tell me, how do you define person-centredness. J. Clin. Nurs. 2016, 26, 2509–2510. [Google Scholar] [CrossRef] [PubMed]
- Røsvik, J.; Kirkevold, M.; Engedal, K.; Brooker, D.; Kirkevold, Ø. A model for using the VIPS framework for person-centred care for persons with dementia in nursing homes: A qualitative evaluative study. Int. J. Older People Nurs. 2011, 6, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Lynch, B.M.; McCance, T.; McCormack, B.; Brown, D. The development of the Person-Centred Situational Leadership Framework: Revealing the being of person-centredness in nursing homes. J. Clin. Nurs. 2018, 27, 427–440. [Google Scholar] [CrossRef] [PubMed]
- DeSilva, D. Helping Measure Person-Centred Care: A Review of Evidence about Commonly Used Approaches and Tools Used to Help Measure Person-Centred Care; The Health Foundation: London, UK, 2014. [Google Scholar]
- Dewing, J.; McCormack, B.; McCance, T. Person-Centred Practice in Nursing and Healthcare: Theory and Practice; Wiley-Blackwell: Oxford, UK, 2010. [Google Scholar]
- McCance, T.; McCormack, B. The Person-Centred Practice Framework; McCormack, B., McCance, T., Martin, S., McMillan, A., Bulley, C., Eds.; Fundamentals of Person-centred Healthcare Practice Wiley: Oxford, UK, 2021. [Google Scholar]
- Slater, P.; McCance, T.; McCormack, B. The development and testing of the Person-centred Practice Inventory—Staff (PCPI-S). Int. J. Qual. Healthc. 2017, 29, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.; Britten, N.; Lydahl, D.; Naldemirci, Ö.; Elam, M.; Wolf, A. Barriers and facilitators to the implementation of person-centred care in different healthcare contexts. Scand. J. Caring Sci. 2017, 31, 662–673. [Google Scholar] [CrossRef] [PubMed]
- Sharp, S.; McAllister, M.; Broadbent, M. The tension between person-centred and task focused care in an acute surgical setting: A critical ethnography. Collegian 2018, 25, 11–17. [Google Scholar] [CrossRef]
- Soklaridis, S.; Ravitz, P.; Adler Nevo, G.; Lieff, S. Relationship-centred care in health: A 20-year scoping review. Patient Exp. J. 2016, 3, 130–145. [Google Scholar] [CrossRef] [Green Version]
- Crawford, P.; Brown, B.; Kvangarsnes, M.; Gilbert, P. The design of compassionate care. J. Clin. Nurs. 2014, 23, 3589–3599. [Google Scholar] [CrossRef] [PubMed]
- Williams, V.; Kinnear, D.; Victor, C. It’s the little things that count: Healthcare professionals’ views on delivering dignified care: A qualitative study. J. Adv. Nurs. 2016, 72, 782–790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. WHO Global Strategy on Integrated People-Centred Health Services 2016–2026. Executive Summar. 2015. Available online: https://interprofessional.global/wp-content/uploads/2019/11/WHO-2015-Global-strategy-on-integrated-people-centred-health-services-2016-2026.pdf (accessed on 1 December 2021).
- McCormack, B.; McCance, T.V. Development of a framework for person-centred nursing. J. Adv. Nurs. 2006, 56, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, J. Analysis and Evaluation of Conceptual Models of Nursing; FA Davis: Philadelphia, PA, USA, 1995. [Google Scholar]
- McCormack, B. A conceptual framework for person-centred practice with older people. Int. J. Nurs. Pract. 2003, 9, 202–209. [Google Scholar] [CrossRef]
- McCance, T.V. Caring in nursing practice: The development of a conceptual framework. Res. Theory Nurs. Pract. Int. J. 2003, 17, 101–116. [Google Scholar] [CrossRef] [PubMed]
- Bing-Jonsson, P.C.; Slater, P.; McCormack, B.; Fagerström, L. Norwegian translation, cultural adaption and testing of the Person-centred Practice Inventory–Staff (PCPI-S). BMC Health Serv. Res. 2018, 18, 555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Wang, X. Structural Equation Modelling: Applications Using Mplus; John Wiley & Sons: New York, NY, USA, 2019. [Google Scholar]
- Kenny, D. Respecification of Latent Variable Models. 2011. Available online: http://davidakenny.net/cm/respec.htm (accessed on 5 April 2020).
- Byrne, B.M. Structural Equation Modeling with Mplus: Basic Concepts, Applications, and Programming; Routledge: London, UK, 2013. [Google Scholar]
- Black Multivariate Data Analysis. Available online: https://www.drnishikantjha.com/papersCollection/Multivariate%20Data%20Analysis.pdf (accessed on 1 December 2021).
- Harding, E.; Wait, S.; Scrutton, J. The State of Play in Person-Centred Care; The Health Foundation: London, UK, 2015. [Google Scholar]
- Laird, E.A.; McCance, T.; McCormack, B.; Gribben, B. Patients’ experiences of in-hospital care when nursing staff were engaged in a practice development programme to promote person-centredness: A narrative analysis study. Int. J. Nurs. Stud. 2015, 52, 1454–1462. [Google Scholar] [CrossRef] [PubMed]
- McCance, T.V.; Gribben, B.; McCormack, B.; Laird, E. Promoting person-centred practice within acute care: The impact of culture and context on a facilitated practice development programme. Int. Pract. Dev. J. 2013, 3. [Google Scholar]
- McCormack, B.; Dickson, C.; Smith, T.; Ford, H.; Ludwig, S.; Moyes, R.; Lee, L.; Adam, E.; Paton, T.; Lydon, B.; et al. ‘It’s a nice place, a nice place to be’. The story of a practice development programme to further develop person-centred cultures in palliative and end-of-life care. Int. Pract. Dev. J. 2018, 8, 2. [Google Scholar] [CrossRef]
- Dogba, M.J.; Menear, M.; Stacey, D.; Brière, N.; Légaré, F. The Evolution of an Interprofessional Shared Decision-Making Research Program: Reflective Case Study of an Emerging Paradigm. Int. J. Integr. Care 2016, 16, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekman, I.; Swedberg, K.; Taft, C.; Lindseth, A.; Norberg, A.; Brink, E.; Carlsson, J.; Dahlin-Ivanoff, S.; Johansson, I.L.; Kjellgren, K.; et al. Person-centered care—Ready for prime time. Eur. J. Cardiovasc. Nurs. 2011, 10, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Ekman, I.; Wolf, A.; Olsson, L.E.; Taft, C.; Dudas, K.; Schaufelberger, M.; Swedberg, K. Effects of person-centred care in patients with chronic heart failure: The PCC-HF study. Eur. Heart J. 2012, 33, 1112–1119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slater, P.; McCance, T.V.; McCormack, B. Exploring person-centred practice within acute hospital settings. Int. Pract. Dev. J. 2015, 5, 9. [Google Scholar] [CrossRef]

| Profession | Experience | Nurses Only | |||
|---|---|---|---|---|---|
| Nursing | 84.4% (n = 1088) | <1 year | 3.6% (n = 46) | Band 5 | 64.1% (431) |
| Medical | 6.7% (n = 86) | 1–5 years | 24.1% (n = 305) | Band 6 | 20.1% (135) |
| Allied Health Professional | 7.0% (n = 90) | 6–10 years | 15.7% (n = 199) | Band 7 | 14.6% (98) |
| Health Care Assistant | 1.9% (n = 25) | Over 10 years | 56.5% (n = 715) | Band 8 | 1.2% (8) |
| Code | CONSTRUCTS | Mean | SD | Skewness | Kurtosis | Alpha |
|---|---|---|---|---|---|---|
| PREREQUISITES | 4.16 | 0.37 | −0.46 | 1.89 | 0.77 | |
| V1 | Professionally Competent | 4.24 | 0.46 | −0.50 | 1.55 | 0.48 |
| V2 | Developed Interpersonal Skills | 4.32 | 0.43 | −0.34 | 0.76 | 0.67 |
| V3 | Being committed to the job | 4.39 | 0.47 | −0.75 | 0.75 | 0.74 |
| V4 | Knowing Self | 3.96 | 0.58 | −0.77 | 1.32 | 0.63 |
| V5 | Clarity of beliefs and values | 3.90 | 0.58 | −0.85 | 2.69 | 0.62 |
| THE CARE ENVIRONMENT | 3.76 | 0.51 | −0.70 | 1.20 | 0.75 | |
| V6 | Skill mix | 4.15 | 0.51 | −0.65 | 1.51 | 0.40 |
| V7 | Shared decision making systems | 3.55 | 0.78 | −0.61 | 0.264 | 0.75 |
| V8 | Effective staff relationships | 3.94 | 0.76 | −1.15 | 1.80 | 0.83 |
| V9 | Power sharing | 3.78 | 0.74 | −0.89 | 1.09 | 0.79 |
| V10 | Potential for innovation and risk taking | 3.80 | 0.67 | −0.57 | 0.95 | 0.87 |
| V11 | The Physical Environment | 3.96 | 0.60 | −0.72 | 1.50 | 0.84 |
| V12 | Supportive Organisation Systems | 3.18 | 0.83 | −0.46 | −0.13 | 0.86 |
| CARE PROCESSES | 4.18 | 0.44 | −0.33 | 1.41 | 0.88 | |
| V13 | Working with patients beliefs and values | 4.06 | 0.56 | −0.46 | 1.48 | 0.78 |
| V14 | Shared Decision making | 4.09 | 0.58 | −0.43 | 0.88 | 0.74 |
| V15 | Engagement. | 4.20 | 0.47 | −0.21 | 2.51 | 0.78 |
| V16 | Sympathetic Presence | 4.21 | 0.51 | −0.53 | 1.63 | 0.70 |
| V17 | Providing holistic care | 4.30 | 0.53 | −0.57 | 0.62 | 0.78 |
| V1 | V2 | V3 | V4 | V5 | V6 | V7 | V8 | V9 | V10 | V11 | V12 | V13 | V14 | V15 | V16 | V17 | |
| V1 | 1 | ||||||||||||||||
| V2 | 0.543 | 1 | |||||||||||||||
| V3 | 0.557 | 0.570 | 1 | ||||||||||||||
| V4 | 0.377 | 0.441 | 0.438 | 1 | |||||||||||||
| V5 | 0.321 | 0.300 | 0.345 | 0.380 | 1 | ||||||||||||
| V6 | 0.357 | 0.410 | 0.355 | 0.315 | 427 | 1 | |||||||||||
| V7 | 0.378 | 0.329 | 0.335 | 0.304 | 0.446 | 0.454 | 1 | ||||||||||
| V8 | 0.287 | 0.323 | 0.264 | 0.225 | 0.314 | 0.343 | 0.570 | 1 | |||||||||
| V9 | 0.365 | 0.351 | 0.299 | 0.278 | 0.305 | 0.378 | 0.626 | 0.744 | 1 | ||||||||
| V10 | 0.365 | 0.322 | 0.298 | 0.286 | 0.344 | 0.339 | 0.401 | 0.354 | 0.457 | 1 | |||||||
| V11 | 0.385 | 0.380 | 0.457 | 0.355 | 0.359 | 0.355 | 0.386 | 0.330 | 0.397 | 0.341 | 1 | ||||||
| V12 | 0.250 | 0.246 | 0.249 | 0.309 | 0.268 | 0.285 | 0.516 | 0.566 | 0.666 | 0.347 | 0.387 | 1 | |||||
| V13 | 0.517 | 0.463 | 0.520 | 0.422 | 0.344 | 0.351 | 0.340 | 0.332 | 0.418 | 0.382 | 0.469 | 0.368 | 1 | ||||
| V14 | 0.438 | 0.447 | 0.465 | 0.339 | 0.307 | 0.347 | 0.337 | 0.340 | 0.391 | 0.293 | 0.387 | 0.337 | 0.601 | 1 | |||
| V15 | 0.448 | 0.505 | 0.466 | 0.337 | 0.292 | 0.373 | 0.260 | 0.229 | 0.296 | 0.315 | 0.347 | 0.212 | 0.552 | 0.655 | 1 | ||
| V16 | 0.570 | 0.566 | 0.565 | 0.399 | 0.330 | 0.352 | 0.320 | 0.300 | 0.352 | 0.342 | 0.383 | 0.282 | 0.571 | 0.590 | 0.618 | 1 | |
| V17 | 0.456 | 0.480 | 0.555 | 0.380 | 0.259 | 0.321 | 0.310 | 0.336 | 0.396 | 0.292 | 0.477 | 0.313 | 0.696 | 0.560 | 0.516 | 0.612 | 1 |
| Model | RMSEA | 90% RMSEA | CFI | TLI | SRMR |
|---|---|---|---|---|---|
| Original Model | 0.079 | 0.075–0.083 | 0.889 | 0.870 | 0.076 |
| Accepted Model | 0.034 | 0.033–0.035 | 0.901 | 0.893 | 0.049 |
| CONSTRUCTS | Estimate | S.E. | Est./S.E. | Variance |
|---|---|---|---|---|
| PREREQUISITES | ||||
| Professionally Competent | 0.73 | 0.02 | 36.73 | 47% |
| Developed Interpersonal Skills | 0.73 | 0.02 | 39.19 | 47% |
| Being committed to the job | 0.76 | 0.02 | 38.29 | 43% |
| Knowing Self | 0.57 | 0.02 | 24.69 | 67% |
| Clarity of beliefs and values | 0.46 | 0.03 | 14.44 | 79% |
| THE CARE ENVIRONMENT | ||||
| Skill mix | 0.57 | 0.03 | 21.63 | 68% |
| Shared decision-making systems | 0.76 | 0.02 | 39.64 | 42% |
| Effective staff relationships | 0.62 | 0.03 | 24.96 | 61% |
| Power sharing | 0.73 | 0.02 | 35.44 | 47% |
| Potential for innovation and risk taking | 0.56 | 0.03 | 19.35 | 69% |
| The Physical Environment | 0.63 | 0.03 | 24.60 | 60% |
| Supportive Organisation Systems | 0.60 | 0.02 | 25.27 | 64% |
| CARE PROCESSES | ||||
| Working with patients beliefs and values | 0.80 | 0.02 | 47.32 | 37% |
| Shared Decision making | 0.73 | 0.02 | 39.07 | 47% |
| Engagement. | 0.68 | 0.02 | 30.42 | 54% |
| Sympathetic Presence | 0.80 | 0.02 | 50.18 | 36% |
| Providing holistic care | 0.77 | 0.02 | 49.42 | 41% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCance, T.; McCormack, B.; Slater, P.; McConnell, D. Examining the Theoretical Relationship between Constructs in the Person-Centred Practice Framework: A Structural Equation Model. Int. J. Environ. Res. Public Health 2021, 18, 13138. https://doi.org/10.3390/ijerph182413138
McCance T, McCormack B, Slater P, McConnell D. Examining the Theoretical Relationship between Constructs in the Person-Centred Practice Framework: A Structural Equation Model. International Journal of Environmental Research and Public Health. 2021; 18(24):13138. https://doi.org/10.3390/ijerph182413138
Chicago/Turabian StyleMcCance, Tanya, Brendan McCormack, Paul Slater, and Donna McConnell. 2021. "Examining the Theoretical Relationship between Constructs in the Person-Centred Practice Framework: A Structural Equation Model" International Journal of Environmental Research and Public Health 18, no. 24: 13138. https://doi.org/10.3390/ijerph182413138
APA StyleMcCance, T., McCormack, B., Slater, P., & McConnell, D. (2021). Examining the Theoretical Relationship between Constructs in the Person-Centred Practice Framework: A Structural Equation Model. International Journal of Environmental Research and Public Health, 18(24), 13138. https://doi.org/10.3390/ijerph182413138







