Effects of Different Types of Contraction Exercises on Shoulder Function and Muscle Strength in Patients with Adhesive Capsulitis
Abstract
:1. Introduction
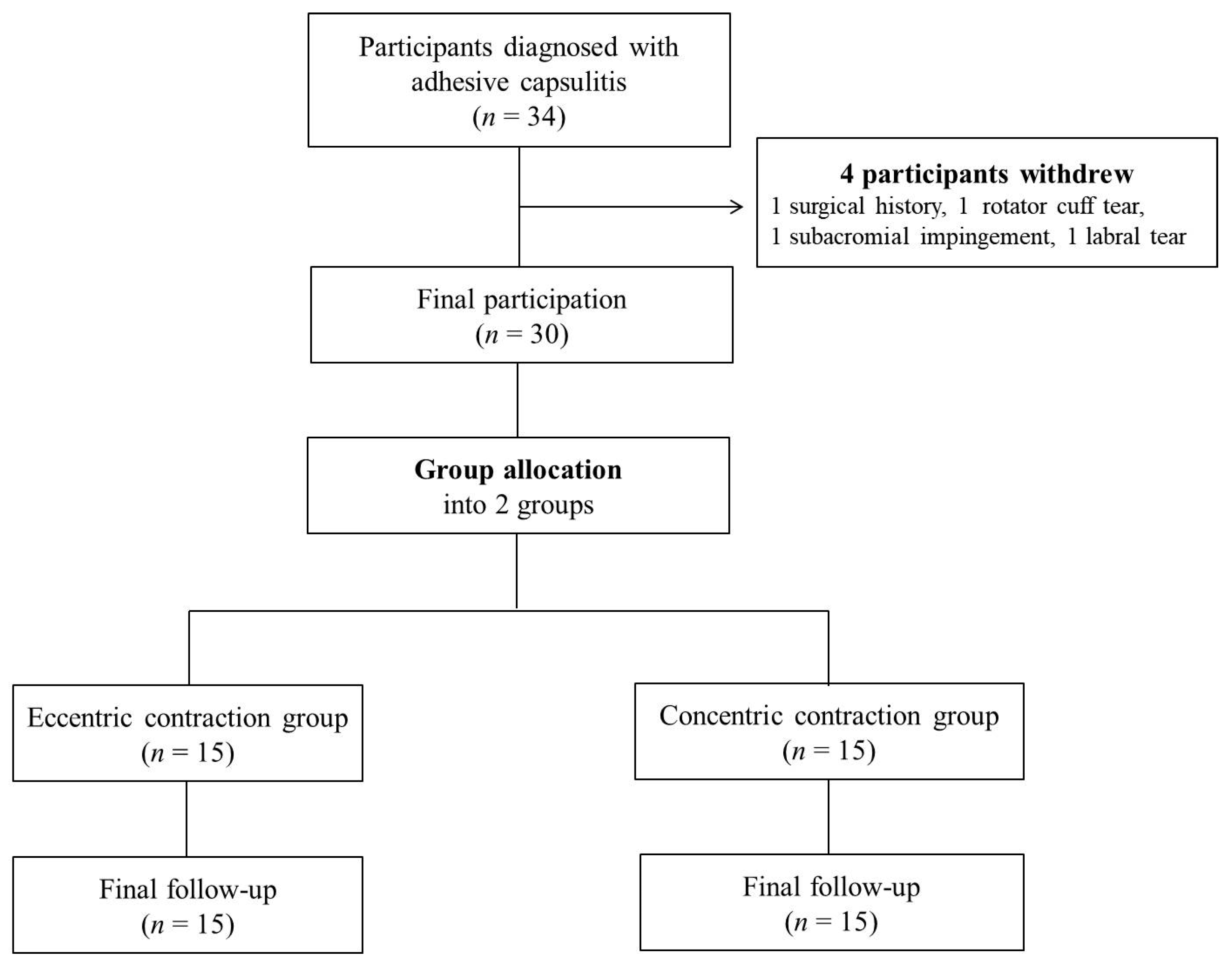
2. Materials and Methods
2.1. Study Design
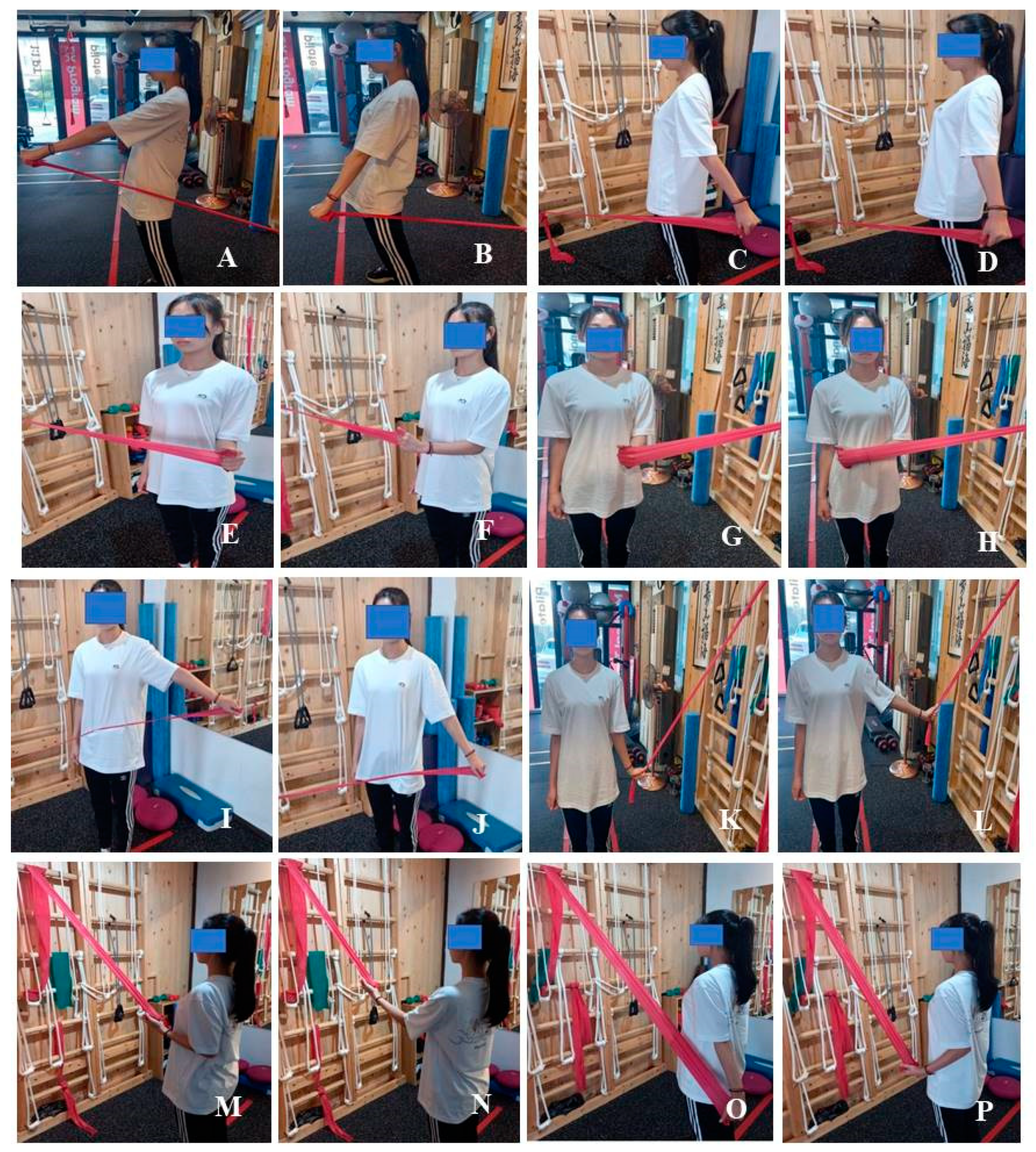
2.2. Exercise Program
2.3. Outcome Assessments
2.3.1. Constant–Murley Score (CMS)
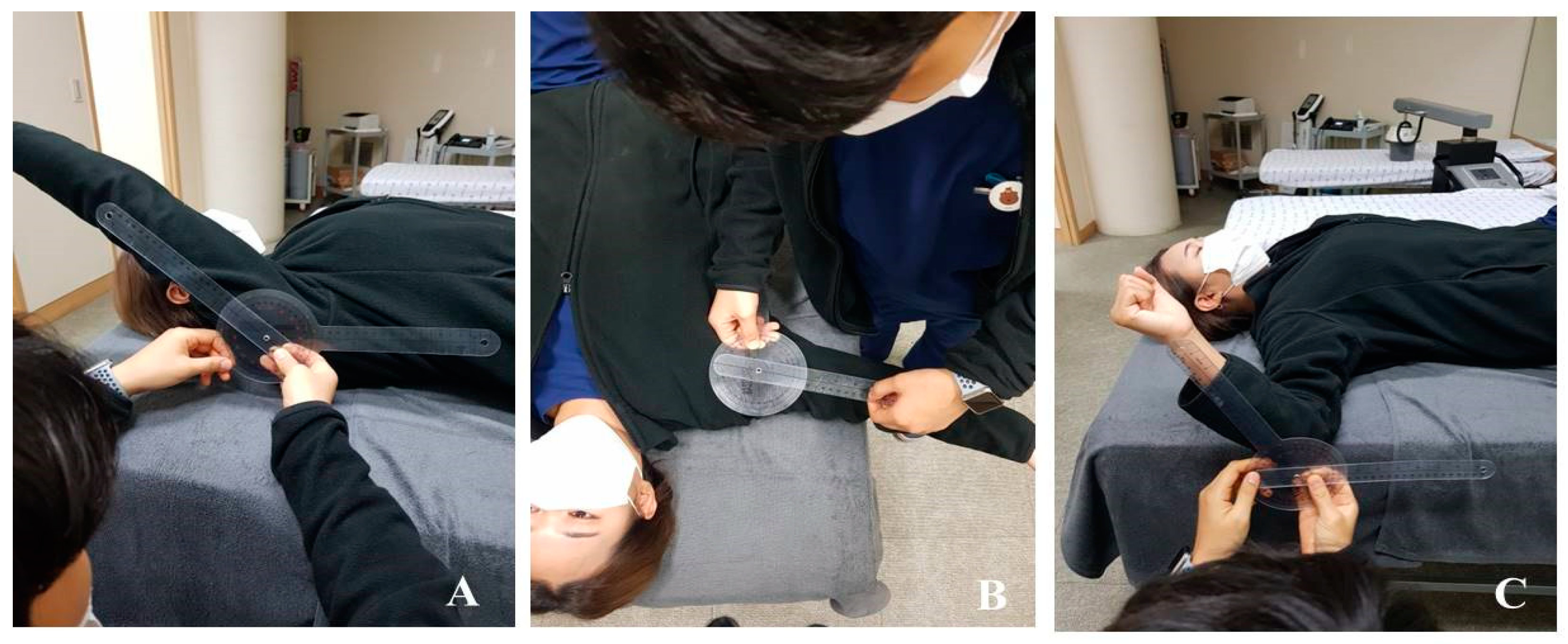
2.3.2. ROM Measurement
2.3.3. Muscle Strength
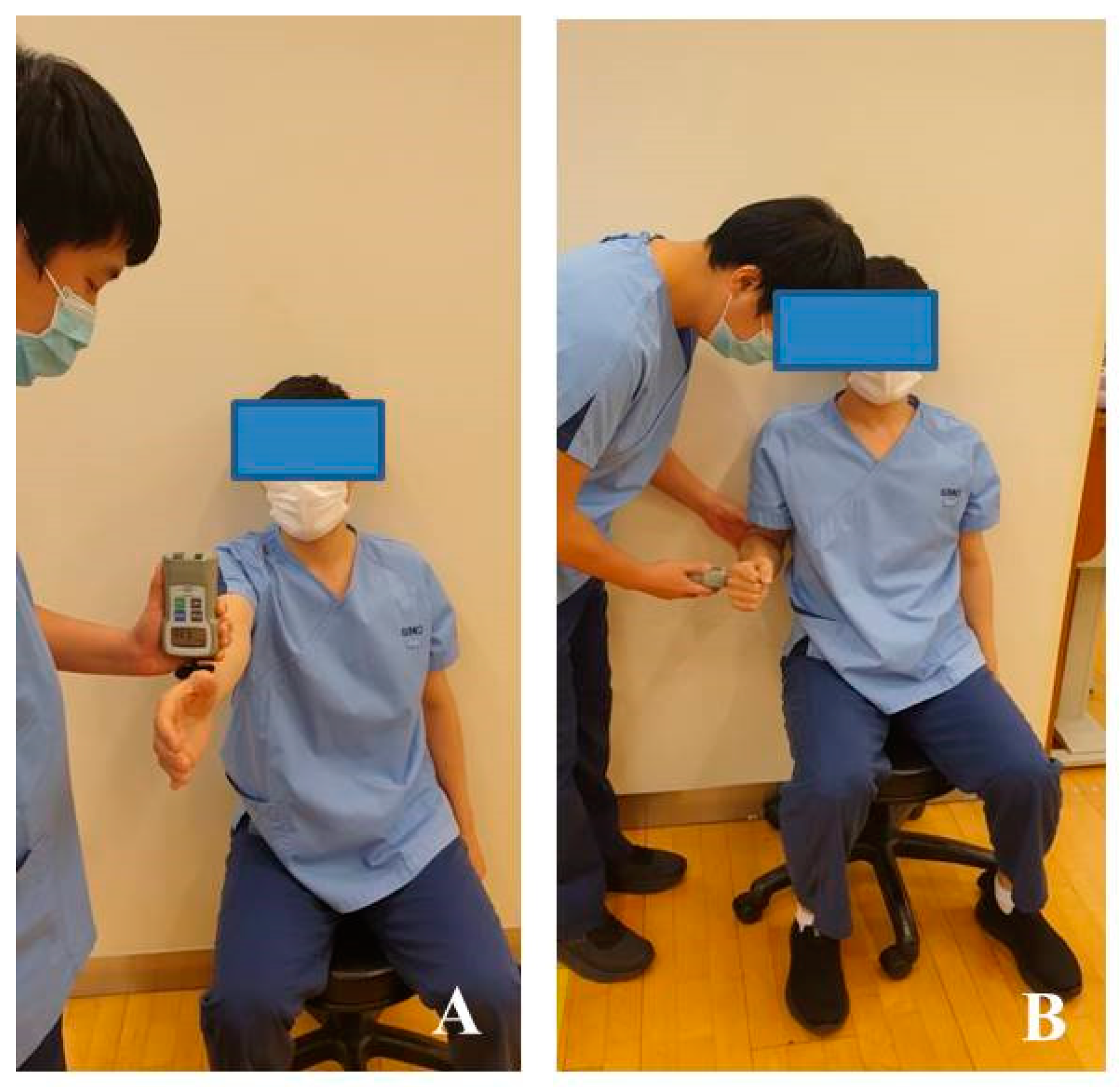
2.4. Statistical Methods
3. Results
3.1. Shoulder Pain
3.2. Shoulder ROM
3.3. Shoulder Muscle Strength
3.4. Shoulder Function
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Celik, D. Comparison of the outcomes of two different exercise programs on frozen shoulder. Acta Orthop. Traumatol. Turc. 2010, 44, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Ogilvie-Harris, D.J.; Myerthall, S. The diabetic frozen shoulder: Arthroscopic release. Arthroscopy 1997, 13, 1–8. [Google Scholar] [CrossRef]
- Harrast, M.A.; Rao, A.G. The stiff shoulder. Phys. Med. Rehabil. Clin. N. Am. 2004, 15, 557–573. [Google Scholar] [CrossRef]
- Loew, M.; Heichel, T.O.; Lehner, B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J. Shoulder Elb. Surg. 2005, 14, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Akpinar, S.; Ozalay, M.; Hersekli, M.A.; Ozkoc, G.; Tandogan, R.N. Arthroscopic capsular release for frozen shoulder. Acta Orthop. Traumatol. Turc. 2003, 37, 213–218, (In Turkish: English Abstract). [Google Scholar] [PubMed]
- Homsi, C.; Bordalo-Rodrigues, M.; da Silva, J.J.; Xavier MGRG Stump. Ultrasound in adhesive capsulitis of the shoulder: Is assessment of the coracohumeral ligament a valuable diagnostic tool. Skelet. Radiol. 2006, 35, 673–678. [Google Scholar] [CrossRef]
- Dudkiewicz, I.; Oran, A.; Salai, M.; Palti, R.; Pritsch, M. Idiopathic adhesive capsulitis: Long-term results of conservative treatment. Isr. Med. Assoc. J. 2004, 6, 524–526. [Google Scholar] [PubMed]
- Cho, C.H.; Bae, K.C.; Kim, D.H. Treatment strategy for frozen shoulder. Clin. Orthop. Surg. 2019, 11, 249–257. [Google Scholar] [CrossRef]
- Challoumas, D.; Biddle, M.; McLean, M.; Milar, N.L. Comparison of treatments for frozen shoulder: A systematic review and meta-analysis. JAMA Netw. Open 2020, 3, e202958. [Google Scholar] [CrossRef]
- Seo, B.D.; Shin, H.S. The effect of self stretching exercise in patients with shoulder adhesive capsulitis. J. Korean Soc. Phys. Ther. 2010, 22, 19–26. [Google Scholar]
- Diercks, R.L.; Stevens, M. Gentle thawing of the frozen shoulder: A prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two years. J. Shoulder Elb. Surg. 2004, 13, 499–502. [Google Scholar] [CrossRef]
- Griggs, S.M.; Ahn, A.; Green, A. Idiopathic adhesive capsulitis: A prospective functional outcome study of nonoperative treatment. J. Bone Jt. Surg. Am. 2000, 82, 1398–1407. [Google Scholar] [CrossRef] [Green Version]
- Russell, S.; Jariwala, A.; Conlon, R.; Selfe, J.; Richards, J.; Walton, M. A blinded, randomized, controlled trial assessing conservative management strategies for frozen shoulder. J. Shoulder Elb. Surg. 2014, 23, 500–507. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; Green, S.; Kramer, S.; Johnston, R.V.; McBain, B.; Chau, M.; Buchbinder, R. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst. Rev. 2014, 26, CD011275. [Google Scholar] [CrossRef]
- Guler-Uysal, F.; Kozanoglu, E. Comparison of the early response to two methods of rehabilitation in adhesive capsulitis. Swiss Med. Wkly. 2004, 134, 353–358. [Google Scholar]
- Vermeulen, H.M.; Rozing, P.M.; Obermann, W.R.; le Cessie, S.; Vliet, V.T.P.M. Comparison of high-grade and low-grade mobilization techniques in the management of adhesive capsulitis of the shoulder: Randomized controlled trial. Phys. Ther. 2006, 86, 355–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padulo, J.; Laffaye, G.; Chaman, K.; Concu, A. Concentric and eccentric: Muscle contraction or exercise? Sports Health 2013, 5, 306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hody, S.; Croisier, J.L.; Bury, T.; Rogister, B.; Leprince, P. Eccentric muscle contractions: Risks and benefits. Front. Physiol. 2019, 10, 536. [Google Scholar] [CrossRef] [PubMed]
- Chaconas, E.J.; Kolber, M.J.; Hanney, W.J.; Daugherty, M.L.; Wilson, S.H.; Sheets, C. Shoulder external rotator eccentric training versus general shoulder exercise for subacromial pain syndrome: A randomized controlled trial. Int. J. Sports Phys. Ther. 2017, 12, 1121–1133. [Google Scholar] [CrossRef] [Green Version]
- Dejaco, B.; Habets, B.; Loon, C.; Girnsven, S.; Cingel, R. Eccentric versus conventional exercise therapy in patients with rotator cuff tendinopathy: A randomized, single blinded, clinical trial. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2051–2059. [Google Scholar] [CrossRef]
- Blume, C.; Wang-Price, S.; Trudelle-Jackson, E.; Ortiz, A. Comparison of eccentric and concentric exercise interventions in adults with subacromial impingement syndrome. Int. J. Sports Phys. Ther. 2015, 10, 441–455. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Lorbach, O.; Anagnostakos, K.; Scherf, C.; Seil, R.; Kohn, D.; Pape, D. Nonoperative management of adhesive capsulitis of the shoulder: Oral cortisone application versus intra-articular cortisone injections. J. Shoulder Elb. Surg. 2010, 19, 172–179. [Google Scholar] [CrossRef]
- D’Orsi, G.M.; Via, A.G.; Frizziero, A.; Oliva, F. Treatment of adhesive capsulitis: A review. Muscles Ligaments Tendons J. 2012, 2, 70–78. [Google Scholar] [PubMed]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Hayes, K.; Walton, J.R.; Szomor, Z.L.; Murrell, G.A. Reliability of five methods for assessing shoulder range of motion. Aust. J. Physiother. 2001, 47, 289–294. [Google Scholar] [CrossRef] [Green Version]
- Kolber, M.J.; Beekhuizen, K.; Cheng, M.S.S.; Fiebert, I.M. The reliability of hand-held dynamometry in measuring isometric strength of the shoulder internal and external rotator musculature using a stabilization device. Physiother. Theory Pract. 2007, 23, 119–124. [Google Scholar] [CrossRef]
- Noël, G.; Verbruggen, L.A.; Barbaix, E.; Duquet, W. Adding compression to mobilization in a rehabilitation program after knee surgery. A preliminary clinical observational study. Man. Ther. 2000, 5, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Hoppeler, H. Moderate load eccentric exercise; a distinct novel training modality. Front. Physiol. 2016, 7, 483. [Google Scholar] [CrossRef] [Green Version]
- Komi, P.V.; Buskirk, E.R. Effect of eccentric and concentric muscle conditioning on tension and electrical activity of human muscle. Ergonomics 1972, 15, 417–434. [Google Scholar] [CrossRef]
- Vogt, M.; Hoppeler, H.H. Eccentric exercise: Mechanisms and effects when used as training regime or training adjunct. J. Appl. Physiol. 2014, 116, 1446–1454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holmgren, T.; Oberg, B.; Adolfsson, L.; Björnsson, H.H.; Johansson, K. Minimal important changes in the Constant-Murley score in patients with subacromial pain. J. Shoulder Elb. Surg. 2014, 23, 1083–1090. [Google Scholar] [CrossRef] [PubMed]
- Nosaka, K.; Aoki, M.S. Repeated bout effect: Research update and future perspective. Braz. J. Biomot. 2011, 5, 5–15. [Google Scholar]
| Variables | ECG (n = 15) | CCG (n = 15) | p-Value |
|---|---|---|---|
| Age (years) | 51.53 ± 4.73 | 52.40 ± 4.03 | 0.594 |
| Height (cm) | 157.36 ± 4.49 | 160.00 ± 4.58 | 0.122 |
| Weight (kg) | 58.96 ± 4.79 | 61.15 ± 5.39 | 0.249 |
| BMI (kg/m2) | 25.28 ± 1.67 | 25.03 ± 1.40 | 0.664 |
| VAS | 7.27 ± 0.70 | 7.40 ± 0.51 | 0.556 |
| Involved site (right:left) | 7:8 | 7:8 | - |
| ROM in flexion (°) | 109.13 ± 10.77 | 109.73 ± 9.08 | 0.870 |
| ROM in abduction (°) | 60.20 ± 9.92 | 60.87 ± 7.02 | 0.833 |
| ROM in ER (°) | 25.53 ± 3.87 | 25.13 ± 3.50 | 0.769 |
| Strength in flexion (kg) | 6.83 ± 0.65 | 6.80 ± 0.66 | 0.912 |
| Strength in ER (kg) | 9.21 ± 0.92 | 9.50 ± 0.86 | 0.375 |
| Constant–Murley score | 35.67 ± 1.72 | 34.67 ± 3.18 | 0.298 |
| Variables | ECG (n = 15) | CCG (n = 15) |
|---|---|---|
| Exercise frequency | 3 times/week | 3 times/week |
| Exercise intensity | VAS 3–4 | VAS 3–4 |
| Exercise time | 60 min | 60 min |
| Contraction time | Concentric contraction: 2 s Eccentric contraction: 10–15 s | Concentric contraction: 2 s Eccentric contraction: 3 s |
| Exercise type | Forward flexion, extension, ER, IR, abduction, adduction, rowing, rowing plus | Forward flexion, extension, ER, IR, abduction, adduction, rowing, rowing plus |
| Maximal exercise volume | 15 reps, 3 sets | 15 repetition, 3 Sets |
| Exercise progression | Initial reps: 10 reps Increase until 15 reps | Initial reps: 10 reps Increase until 15 reps |
| Variables | Group | Pre | Post | t | Δ% | F-Value | p-Value | |
|---|---|---|---|---|---|---|---|---|
| VAS | ECG | 7.27 ± 0.70 | 2.87 ± 0.64 | 20.579 *** | −61 | T | 749.75 | <0.001 |
| G | 12.064 | 0.002 ** | ||||||
| CCG | 7.40 ± 0.51 | 3.93 ± 0.59 | 18.065 *** | −47 | ||||
| T × G | 10.554 | 0.003 ** | ||||||
| ROM in flexion (°) | ECG | 109.13 ± 10.77 | 157.20 ± 11.73 | −12.019 *** | 31 | T | 152.370 | <0.001 |
| G | 1.995 | 0.021 * | ||||||
| CCG | 109.73 ± 9.08 | 141.27 ± 16.40 | −6.234 *** | 22 | ||||
| T × G | 6.573 | 0.016 * | ||||||
| ROM in abduction (°) | ECG | 60.20 ± 9.92 | 123.67 ± 7.67 | −20.081 *** | 51 | T | 712.549 | <0.001 |
| G | 1.720 | 0.200 | ||||||
| CCG | 60.87 ± 7.02 | 116.07 ± 12.30 | −17.657 *** | 48 | ||||
| T × G | 3.458 | 0.073 | ||||||
| ROM in ER (°) | ECG | 25.53 ± 3.87 | 56.00 ± 10.47 | −11.179 *** | 54 | T | 255.584 | <0.001 |
| G | 4.235 | 0.049 * | ||||||
| CCG | 25.13 ± 3.50 | 49.27 ± 6.37 | −11.725 *** | 49 | ||||
| T × G | 3.439 | 0.074 | ||||||
| Strength in flexion (kg) | ECG | 6.83 ± 0.65 | 9.09 ± 0.93 | −17.466 *** | 25 | T | 326.767 | <0.001 |
| G | 1.503 | 0.230 | ||||||
| CCG | 6.80 ± 0.66 | 8.52 ± 0.63 | −9.655 *** | 20 | ||||
| T × G | 6.015 | 0.021 * | ||||||
| Strength in ER (kg) | ECG | 9.21 ± 0.92 | 12.67 ± 0.90 | −22.664 *** | 27 | T | 813.889 | <0.001 |
| G | 4.726 | 0.038 * | ||||||
| CCG | 9.50 ± 0.86 | 10.99 ± 0.96 | −18.096 *** | 14 | ||||
| T × G | 130.047 | <0.001 | ||||||
| Constant–Murley score | ECG | 35.67 ± 1.72 | 69.20 ± 5.31 | −23.121 *** | 48 | T | 577.340 | <0.001 |
| G | 9.515 | 0.005 ** | ||||||
| CCG | 34.67 ± 3.18 | 62.13 ± 7.64 | −13.182 *** | 44 | ||||
| T × G | 5.710 | 0.024 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, W.-M.; Seo, Y.-G.; Park, Y.-J.; Cho, H.-S.; Lee, S.-A.; Jeon, S.-J.; Ji, S.-M. Effects of Different Types of Contraction Exercises on Shoulder Function and Muscle Strength in Patients with Adhesive Capsulitis. Int. J. Environ. Res. Public Health 2021, 18, 13078. https://doi.org/10.3390/ijerph182413078
Kim W-M, Seo Y-G, Park Y-J, Cho H-S, Lee S-A, Jeon S-J, Ji S-M. Effects of Different Types of Contraction Exercises on Shoulder Function and Muscle Strength in Patients with Adhesive Capsulitis. International Journal of Environmental Research and Public Health. 2021; 18(24):13078. https://doi.org/10.3390/ijerph182413078
Chicago/Turabian StyleKim, Won-Moon, Yong-Gon Seo, Yun-Jin Park, Han-Su Cho, Su-Ah Lee, Sang-Jun Jeon, and Sang-Min Ji. 2021. "Effects of Different Types of Contraction Exercises on Shoulder Function and Muscle Strength in Patients with Adhesive Capsulitis" International Journal of Environmental Research and Public Health 18, no. 24: 13078. https://doi.org/10.3390/ijerph182413078
APA StyleKim, W.-M., Seo, Y.-G., Park, Y.-J., Cho, H.-S., Lee, S.-A., Jeon, S.-J., & Ji, S.-M. (2021). Effects of Different Types of Contraction Exercises on Shoulder Function and Muscle Strength in Patients with Adhesive Capsulitis. International Journal of Environmental Research and Public Health, 18(24), 13078. https://doi.org/10.3390/ijerph182413078







