Breastmilk as a Multisensory Intervention for Relieving Pain during Newborn Screening Procedures: A Randomized Control Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Sample and Setting
2.3. Measurement of Pain in Newborns
2.4. Heel Sticks
2.5. Treatment Conditions
2.6. Data Collection
2.7. Study Integrity
2.8. Data Analysis
3. Results
3.1. Newborn Characteristics
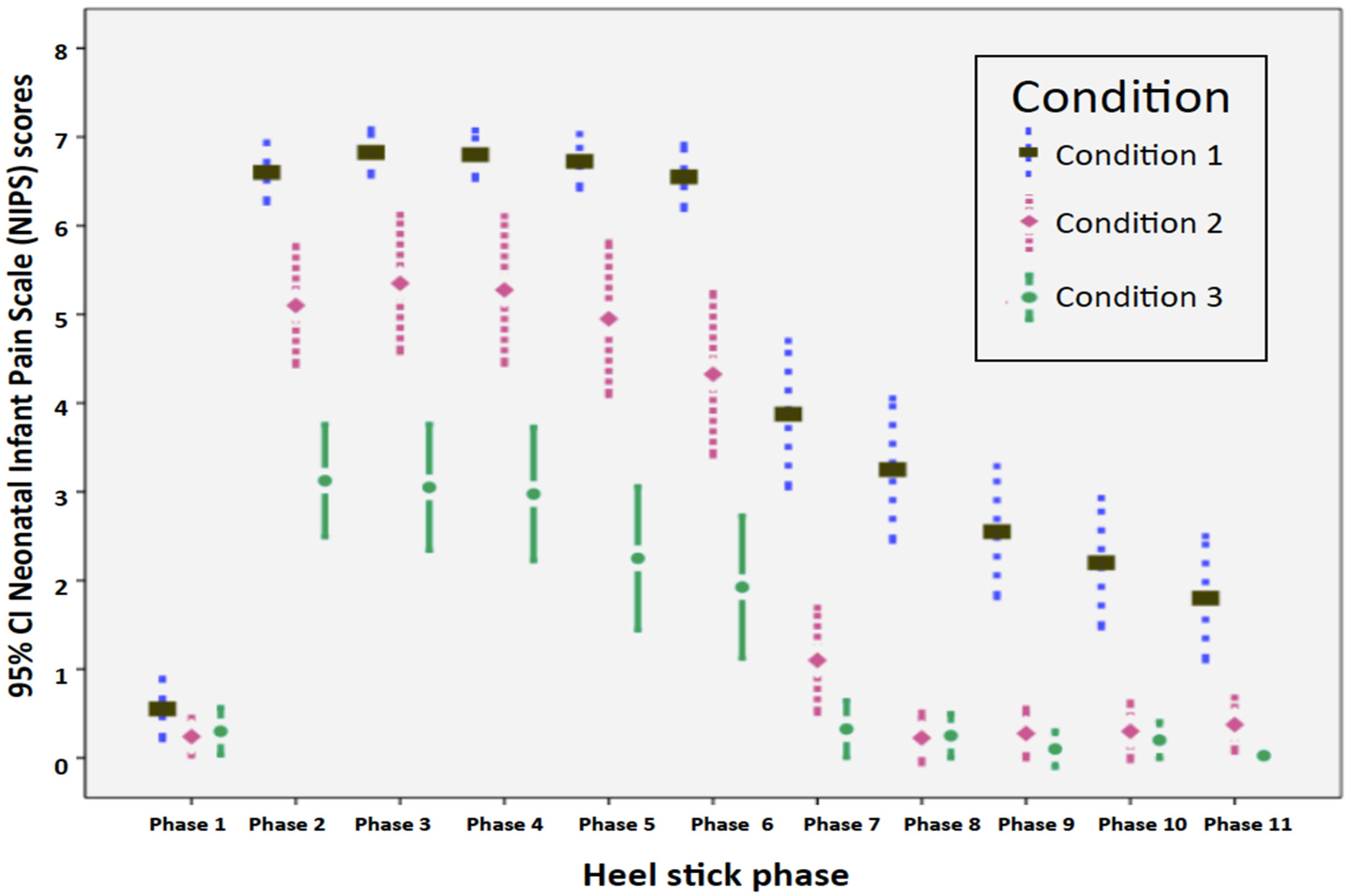
3.2. Pain
4. Discussion
4.1. Clinical Implications
4.2. Study Limitations and Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Crude Birth Rate. 2021. Available online: https://www.who.int/data/maternal-newborn-child-adolescent-ageing/indicator-explorer-new/mca/crude-birth-rate-(births-per-1000-population) (accessed on 5 August 2021).
- Ministry of the Interior, Department of Household Registration. Monthly Bulletin of Interior Statistics. 2021. Available online: https://ws.moi.gov.tw/001/Upload/400/relfile/0/4413/d02039cb-499a-4aea-a6c1-99a565721a18/month/month.html (accessed on 5 August 2021).
- Chien, H.Y.; Hwu, W.L.; Lee, N.C. Newborn screening: Taiwanese experience. Ann. Transl. Med. 2019, 7, 281. [Google Scholar] [CrossRef] [PubMed]
- Health Promotion Administration. The First Line of Defense for Health: Three Decades of Newborn Screening in Taiwan. 2016. Available online: https://www.hpa.gov.tw/EngPages/Detail.aspx?nodeid=1307&pid=7179 (accessed on 5 August 2021).
- Liaw, J.J.; Zeng, W.P.; Yang, L.; Yuh, Y.S.; Yin, T.; Yang, M.H. Nonnutritive sucking and oral sucrose relieve neonatal pain during intramuscular injection of hepatitis vaccine. J. Pain Symptom Manag. 2011, 42, 918–930. [Google Scholar] [CrossRef] [PubMed]
- Pineda, R.G.; Neil, J.; Dierker, D.; Smyser, C.D.; Wallendorf, M.; Kidokoro, H.; Reynolds, L.C.; Walker, S.; Rogers, C.; Mathur, A.M.; et al. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J. Pediatr. 2014, 164, 52–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tortora, D.; Severino, M.; Di Biase, C.; Malova, M.; Parodi, A.; Minghetti, D.; Traggiai, C.; Uccella, S.; Boeri, L.; Morana, G.; et al. Early pain exposure influences functional brain connectivity in very preterm neonates. Front. Neurosci. 2019, 13, 899. [Google Scholar] [CrossRef] [PubMed]
- Brummelte, S.; Chau, C.M.; Cepeda, I.L.; Degenhardt, A.; Weinberg, J.; Synnes, A.R.; Grunau, R.E. Cortisol levels in former preterm children at school age are predicted by neonatal procedural pain-related stress. Psychoneuroendocrinology 2015, 51, 151–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waxman, J.A.; Pillai Riddell, R.R.; Tablon, P.; Schmidt, L.A.; Pinhasov, A. Development of cardiovascular indices of acute pain responding in infants: A systematic review. Pain Res. Manag. 2016, 2016, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Maitre, N.L.; Key, A.P.; Chorna, O.D.; Slaughter, J.C.; Matusz, P.J.; Wallace, M.T.; Murray, M.M. The dual nature of early-life experience on somatosensory processing in the human infant brain. Curr. Biol. 2017, 27, 1048–1054. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartley, C.; Duff, E.P.; Green, G.; Mellado, G.S.; Worley, A.; Rogers, R.; Slater, R. Nociceptive brain activity as a measure of analgesic efficacy in infants. Sci. Transl. Med. 2017, 9, 1–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eccleston, C.; Fisher, E.; Howard, R.F.; Slater, R.; Forgeron, P.; Palermo, T.M.; Birnie, K.A.; Anderson, B.J.; Chambers, C.T.; Crombez, G.; et al. Delivering transformative action in paediatric pain: A Lancet Child & Adolescent Health Commission. Lancet Child Adolesc. Health 2020, 5, 47–87. [Google Scholar] [CrossRef]
- Stevens, B.; Yamada, J.; Ohlsson, A.; Haliburton, S.; Shorkey, A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst. Rev. 2016, 7. [Google Scholar] [CrossRef] [PubMed]
- Liaw, J.J.; Yang, L.; Wang, K.W.K.; Chen, C.M.; Chang, Y.C.; Yin, T. Non-nutritive sucking and facilitated tucking relieve preterm infant pain during heel-stick procedures: A prospective, randomised controlled crossover trial. Int. J. Nurs. Stud. 2012, 49, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.F.; Yin, T.; Yang, L.; Wang, C.; Chang, Y.C.; Jeng, M.J.; Liaw, J.J. Non-nutritive sucking, oral breast milk, and facilitated tucking relieve preterm infant pain during heel-stick procedures: A prospective, randomized controlled trial. Int. J. Nurs. Stud. 2018, 77, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Ranjbar, A.; Bernstein, C.; Shariat, M.; Ranjbar, H. Comparison of facilitated tucking and oral dextrose in reducing the pain of heel stick in preterm infants: A randomized clinical trial. BMC Pediatr. 2020, 20, 2–9. [Google Scholar] [CrossRef] [Green Version]
- Cirik, V.A.; Efe, E. The effect of expressed breast milk, swaddling and facilitated tucking methods in reducing the pain caused by orogastric tube insertion in preterm infants: A randomized controlled trial. Int. J. Nurs. Stud. 2020, 104, 103532. [Google Scholar] [CrossRef]
- Locatelli, C.; Bellieni, C.V. Sensorial saturation and neonatal pain: A review. J. Matern. Fetal Neonatal. Med. 2018, 31, 3209–3213. [Google Scholar] [CrossRef]
- World Health Organization. Breastfeeding. 2018. Available online: https://www.who.int/nutrition/topics/exclusive_breastfeeding/en/ (accessed on 5 August 2021).
- Erkut, Z.; Yildiz, S. The effect of swaddling on pain, vital signs, and crying duration during heel lance in newborns. Pain Manag. Nurs. 2017, 18, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Collados-Gómez, L.; Ferrera-Camacho, P.; Fernandez-Serrano, E.; Camacho-Vicente, V.; Flores-Herrero, C.; García-Pozo, A.M.; Jiménez-García, R. Randomised crossover trial showed that using breast milk or sucrose provided the same analgesic effect in preterm infants of at least 28 weeks. Acta Paediatr. 2018, 107, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.R.; Ling, P.R.; Blackburn, G.L. Review of infant feeding: Key features of breast milk and infant formula. Nutrients 2016, 8, 279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agarwal, S.; Karmaus, W.; Davis, S.; Gangur, V. Immune markers in breast milk and fetal and maternal body fluids: A systematic review of perinatal concentrations. J. Hum. Lact. 2011, 27, 171–186. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Su, F.; Li, J.; Chen, W. The analgesic effects of maternal milk odor on newborns: A meta-analysis. Breastfeed. Med. 2018, 13, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Blass, E.M. Milk-induced hypoalgesia in human newborns. Pediatrics 1997, 99, 825–829. [Google Scholar] [CrossRef]
- Baudesson de Chanville, A.; Brevaut-Malaty, V.; Garbi, A.; Tosello, B.; Baumstarck, K.; Gire, C.; Cozannet, R.L. Analgesic effect of maternal human milk odor on premature neonates: A randomized controlled trial. J. Hum. Lact. 2017, 33, 300–308. [Google Scholar] [CrossRef]
- Barrett, T.; Kent, S.; Voudouris, N. Does melatonin modulate beta-endorphin, corticosterone, and pain threshold? Life Sci. 2000, 66, 467–476. [Google Scholar] [CrossRef]
- Dewar, G. The Newborn Senses: What Does Your Baby Feel, See, Hear, Smell, and Taste? Parent Science. 2017. Available online: https://www.parentingscience.com/newborn-senses.html (accessed on 5 August 2021).
- Bennett, A.J.; Hopkins, W.D.; Feldmann, T.; Gazzola, V.; Giedd, J.; Lamb, M.E.; Tottenham, N. Neural foundation of variability in attachment. In The Cultural Nature of Attachment and Contextualizing Relationships and Development; Keller, H., Bard, K.A., Eds.; MIT Press: Cambridge, MA, USA, 2017. [Google Scholar]
- Beker, F.; Opie, G.; Noble, E.; Jiang, Y.; Bloomfield, F.H. Smell and taste to improve nutrition in very preterm infants: A randomized controlled pilot trial. Neonatology 2017, 111, 260–266. [Google Scholar] [CrossRef]
- Bloomfield, F.H.; Alexander, T.; Muelbert, M.; Beker, F. Smell and taste in the preterm infant. Early Hum. Dev. 2017, 114, 31–34. [Google Scholar] [CrossRef] [Green Version]
- Zeraati, H.; Shahinfar, J.; Vashani, H.B.; Reyhani, T. Effect of multisensory stimulation on pain of eye examination in preterm infants. Anesth. Pain Med. 2017, 7, e42561. [Google Scholar] [CrossRef] [Green Version]
- Melzack, R.; Wall, P.D. Pain mechanisms: A new theory. Science 1965, 150, 971–979. [Google Scholar] [CrossRef]
- Kisilvesky, B.S. Fetal auditory processing: Implications for language development? In Fetal Development: Research on Brain and Behavior, Environmental Influences, and Emerging Technology; Reissland, N., Kisilvesky, B.S., Eds.; Springer: Cham, Switzerland, 2016; pp. 133–154. [Google Scholar]
- Kahraman, A.; Gümüş, M.; Akar, M.; Sipahi, M.; Yılmaz, H.B.; Başbakkal, Z. The effects of auditory interventions on pain and comfort in premature newborns in the neonatal intensive care unit; a randomised controlled trial. Intensive Crit. Care Nurs. 2020, 61, 102904. [Google Scholar] [CrossRef]
- Lawrence, J.; Alcock, D.; McGrath, P.; Kay, J.; MacMurray, S.B.; Dulberg, C. The development of a tool to assess neonatal pain. Neonatal Netw. 1993, 12, 59–66. [Google Scholar] [CrossRef]
- Aydin, D.; İnal, S. Effects of breastfeeding and heel warming on pain levels during heel stick in neonates. Int. J. Nurs. Pract. 2019, 25, 1–8. [Google Scholar] [CrossRef]
- Shah, P.S.; Herbozo, C.; Aliwalas, L.L.; Shah, V.S. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database Syst. Rev. 2012, 12, 1–77. [Google Scholar] [CrossRef]
- Wu, H.P.; Yin, T.; Hsieh, K.H.; Lan, H.Y.; Feng, R.C.; Chang, Y.C.; Liaw, J.J. Integration of different sensory interventions from mother’s breast milk for preterm infant pain during peripheral venipuncture procedures: A prospective randomized controlled trial. J. Nurs. Scholarsh. 2020, 52, 75–84. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lan, H.-Y.; Yang, L.; Lin, C.-H.; Hsieh, K.-H.; Chang, Y.-C.; Yin, T. Breastmilk as a Multisensory Intervention for Relieving Pain during Newborn Screening Procedures: A Randomized Control Trial. Int. J. Environ. Res. Public Health 2021, 18, 13023. https://doi.org/10.3390/ijerph182413023
Lan H-Y, Yang L, Lin C-H, Hsieh K-H, Chang Y-C, Yin T. Breastmilk as a Multisensory Intervention for Relieving Pain during Newborn Screening Procedures: A Randomized Control Trial. International Journal of Environmental Research and Public Health. 2021; 18(24):13023. https://doi.org/10.3390/ijerph182413023
Chicago/Turabian StyleLan, Hsiang-Yun, Luke Yang, Chiao-Hsuan Lin, Kao-Hsian Hsieh, Yue-Cune Chang, and Ti Yin. 2021. "Breastmilk as a Multisensory Intervention for Relieving Pain during Newborn Screening Procedures: A Randomized Control Trial" International Journal of Environmental Research and Public Health 18, no. 24: 13023. https://doi.org/10.3390/ijerph182413023
APA StyleLan, H.-Y., Yang, L., Lin, C.-H., Hsieh, K.-H., Chang, Y.-C., & Yin, T. (2021). Breastmilk as a Multisensory Intervention for Relieving Pain during Newborn Screening Procedures: A Randomized Control Trial. International Journal of Environmental Research and Public Health, 18(24), 13023. https://doi.org/10.3390/ijerph182413023





