Influence of COVID-19 Pandemic Uncertainty in Negative Emotional States and Resilience as Mediators against Suicide Ideation, Drug Addiction and Alcoholism
Abstract
:1. Introduction
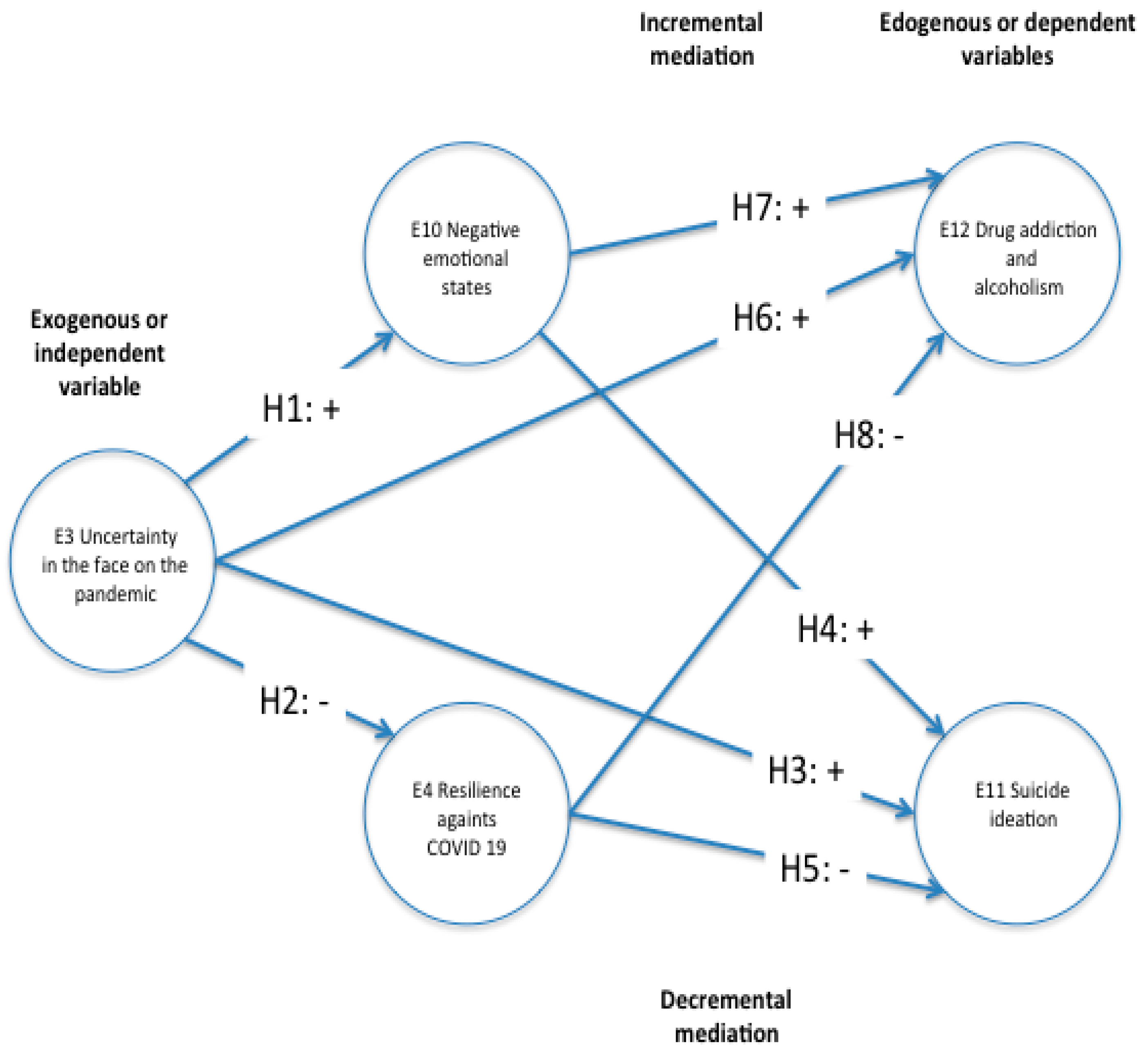
1.1. Hypotheses
1.2. Negative Emotional States
1.3. Resilience against COVID-19
1.4. Suicidal Ideation
1.5. Drug Addiction and Alcoholism
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Instruments
- Students questions regarding their sociodemographic characteristics including gender, marital status, age, scholarity, academic demographic information such as academic program and scholarship status to categorize the demographic variables.
- COVID-19 pandemic uncertainty: we developed this part using 6 questions to measure uncertainty as a unidimensional variable with a Likert scale of five points. Examples of the questions used are: “I was afraid when facing the pandemic”, “I felt that life is very fragile”, “I feared to be infected”, “I was terrified to imagine someone dear was going to die”.
- Resilience scale CD-RISC25 [61]. Focused on determining resilience. Resilience is the ability of human beings to adapt and overcome adverse situations, measured through their level of positive response to risk situations as a multidimensional construct. This instrument consists of 25 items that must be answered in a 5-point Likert scale (1 to 5). It consists of five dimensions: persistence/tenacity/self-efficacy (items 10–12, 16, 17, 23–25); control under pressure (items 6, 7, 14, 15, 18, 19, 20); adaptability and support networks (items 1, 2, 4, 5, 8); control and meaning (items 13, 21, 22) and spirituality (items 3, 9).
- DASS-21 questionnaire short version (anxiety scale [62]). This scale has six states that measure what the respondent is “feeling at this moment.”
- Adaptation of the Scale for Suicide Ideation. Focused on determining the suicidal ideas of students in the face of the pandemic. It is based on the Scale for Suicide Ideation (SSI-W) and it consists of six questions that must be answered in a range of one to two [63].
- Adaptation of the Scale for Disorders by Drug Addiction and Alcoholism. Focused on determining trends in alcohol and drug use. It is based on the scale Alcohol Use Disorders Identification Test (AUDIT) proposed by Saunders et al., 1993 [64] and it consists of 8 items that must be answered on a scale of zero to three.
2.4. Statistical Analyses
3. Results
3.1. Unit of Analysis
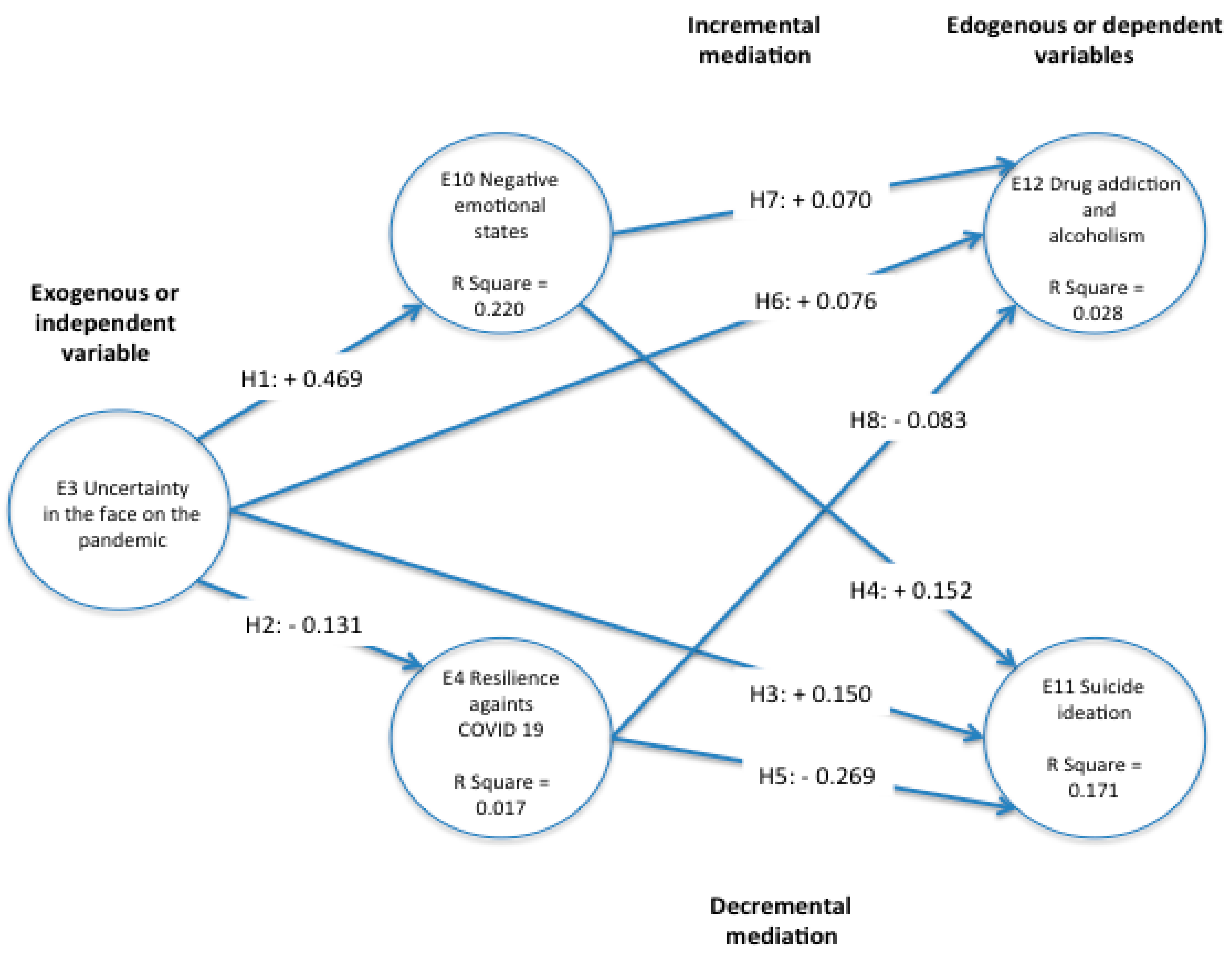
3.2. Contrast of the Hypotheses
3.3. Reliability and Validity
3.4. Correlations between the Subscales of the Instrument
3.5. Significant Differences between Resilience and the Subscales of Suicide Ideation, Emotional States, and Drug Addiction and Alcoholism Regarding Students’ Sex
3.6. Explained Variance of Subscales in the SEM PLS
3.7. Mediation Analysis
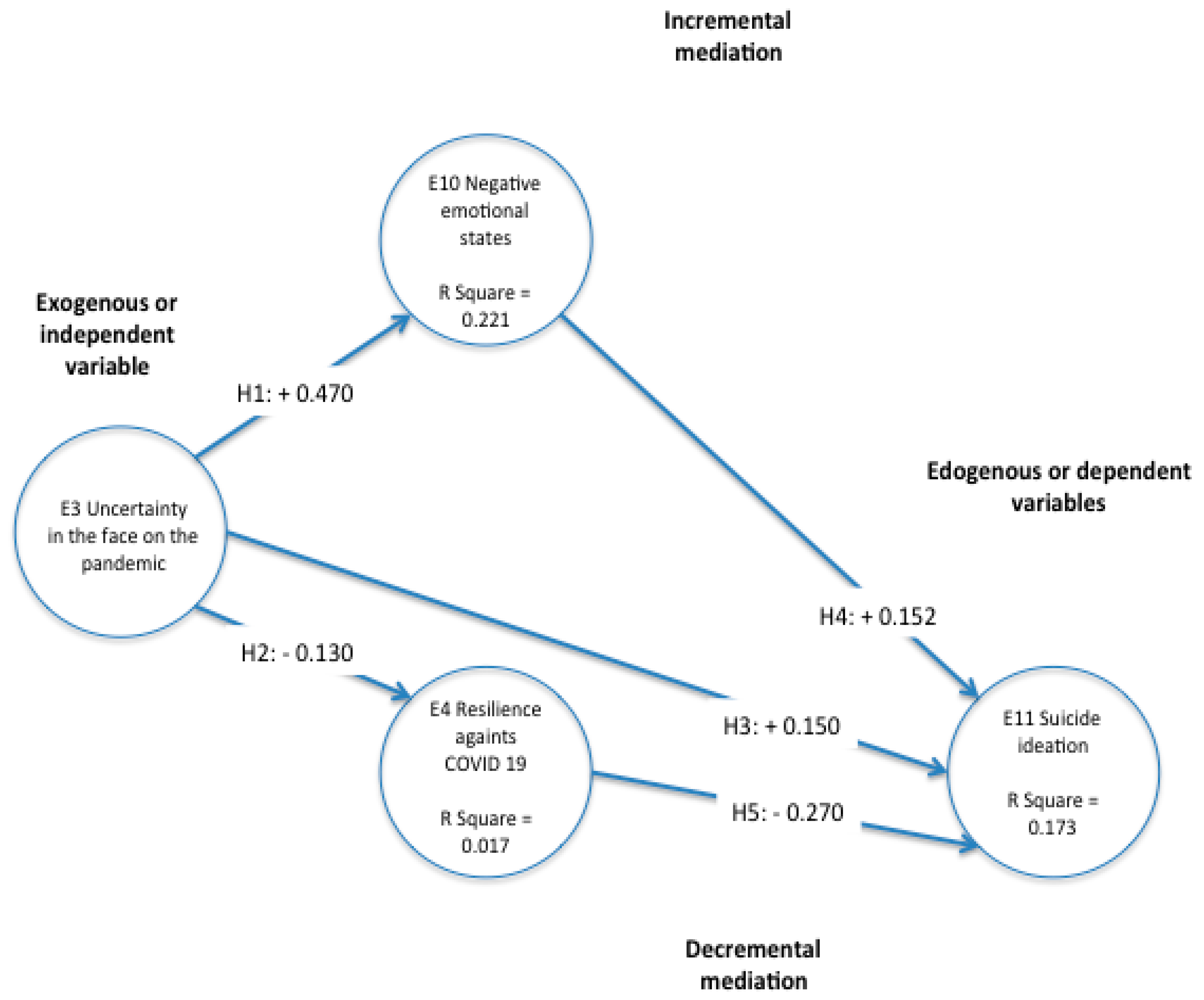
3.8. Increasing Mediation
3.9. Decreasing Mediation
4. Discussion
4.1. Limitations to this Research
4.2. Implications and Opportunities for Further Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Factor Loading of the Items
| Items | E10 | E11 | E12 | E14 | E3 |
|---|---|---|---|---|---|
| Q33R2 | 0.828 | ||||
| Q33R3 | 0.78 | ||||
| Q33R6 | 0.81 | ||||
| Q36R1 | 0.797 | ||||
| Q36R2 | 0.802 | ||||
| Q36R3 | 0.814 | ||||
| Q36R4 | 0.821 | ||||
| Q39R5 | 0.895 | ||||
| Q39R7 | 0.891 | ||||
| Q39R8 | 0.743 | ||||
| Q45R11 | 0.824 | ||||
| Q45R17 | 0.819 | ||||
| Q45R21 | 0.842 | ||||
| Q45R5 | 0.817 | ||||
| Q23R1 | 0.851 | ||||
| Q23R2 | 0.791 | ||||
| Q23R3 | 0.868 |
References
- Díaz-Castrillón, F.J.; Toro-Montoya, A.I. SARS-CoV-2/COVID-19: El virus, la enfermedad y la pandemia. Med. Lab. 2020, 24, 183–205. [Google Scholar] [CrossRef]
- Li, L.-Q.; Huang, T.; Wang, Y.-Q.; Wang, Z.-P.; Liang, Y.; Huang, T.-B.; Zhang, H.-Y.; Sun, W.; Wang, Y. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020, 92, 577–583. [Google Scholar] [CrossRef]
- Tedros, A.G. WHO Director General´s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 29 November 2021).
- Cielo, F.; Ulberg, R.; Di Giacomo, D. Psychological Impact of the COVID-19 Outbreak on Mental Health Outcomes among Youth: A Rapid Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 6067. [Google Scholar] [CrossRef] [PubMed]
- Wen, W.; Su, W.; Tang, H.; Le, W.; Zhang, X.; Zheng, Y.; Liu, X.; Xie, L.; Li, J.; Ye, J.; et al. Immune cell profiling of COVID-19 patients in the recovery stage by single-cell sequencing. Cell Discov. 2020, 6, 31. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Yan, Q.; Tang, Y.; Yan, D.; Wang, J.; Yang, L.; Yang, X.; Tang, S. Impact of media reports on the early spread of COVID-19 epidemic. J. Theor. Biol. 2020, 502, 110385. [Google Scholar] [CrossRef]
- McGinty, E.E.; Presskreischer, R.; Han, H.; Barry, C.L. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA 2020, 324, 93–94. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Fernández, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef]
- Rubin, G.J.; Wessely, S. The psychological effects of quarantining a city. BMJ 2020, 368, m313. [Google Scholar] [CrossRef] [Green Version]
- Szcześniak, D.; Gładka, A.; Misiak, B.; Cyran, A.; Rymaszewska, J. The SARS-CoV-2 and mental health: From biological mechanisms to social consequences. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 104, 110046. [Google Scholar] [CrossRef]
- Garfin, D.R.; Silver, R.C.; Holman, E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020, 39, 355–357. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.-T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef] [Green Version]
- Gale, S.D.; Berrett, A.N.; Erickson, L.D.; Brown, B.L.; Hedges, D.W. Association between virus exposure and depression in US adults. Psychiatry Res. 2018, 261, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Hu, M.; Ji, Q. Financial markets under the global pandemic of COVID-19. Financ. Res. Lett. 2020, 36, 101528. [Google Scholar] [CrossRef]
- Stacey, G.; Cook, G.; Aubeeluck, A.; Stranks, B.; Long, L.; Krepa, M.; Lucre, K. The implementation of resilience based clinical supervision to support transition to practice in newly qualified healthcare professionals. Nurse Educ. Today 2020, 94, 104564. [Google Scholar] [CrossRef]
- Moni, A.S.B.; Abdullah, S.; Bin Abdullah, M.F.I.L.; Kabir, M.S.; Alif, S.M.; Sultana, F.; Salehin, M.; Islam, S.M.S.; Cross, W.; Rahman, M.A. Psychological distress, fear and coping among Malaysians during the COVID-19 pandemic. PLoS ONE 2021, 16, e0257304. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schimmenti, A.; Starcevic, V.; Giardina, A.; Khazaal, Y.; Billieux, J. Multidimensional Assessment of COVID-19-Related Fears (MAC-RF): A Theory-Based Instrument for the Assessment of Clinically Relevant Fears During Pandemics. Front. Psychiatry 2020, 11, 748. [Google Scholar] [CrossRef]
- Baloch, G.M.; Sundarasen, S.; Chinna, K.; Nurunnabi, M.; Kamaludin, K.; Khoshaim, H.B.; Hossain, S.F.A.; AlSukayt, A. COVID-19: Exploring impacts of the pandemic and lockdown on mental health of Pakistani students. PeerJ 2021, 9, e10612. [Google Scholar] [CrossRef] [PubMed]
- Bourion-Bédès, S.; Tarquinio, C.; Batt, M.; Tarquinio, P.; Lebreuilly, R.; Sorsana, C.; Legrand, K.; Rousseau, H.; Baumann, C. Psychological impact of the COVID-19 outbreak on students in a French region severely affected by the disease: Results of the PIMS-CoV 19 study. Psychiatry Res. 2021, 295, 113559. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on col-lege students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef] [PubMed]
- Faize, F.A.; Husain, W. Students with severe anxiety during COVID-19 lockdown—Exploring the impact and its management. J. Ment. Health Train. Educ. Pract. 2021, 16, 153–163. [Google Scholar] [CrossRef]
- Cahill, C.R. Cinco retos psicológicos de la crisis del COVID-19. J. Negat. No Posit. Results 2020, 5, 583–588. [Google Scholar]
- Steven, T. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease; Cambridge Scholars Publishing: Newcastle, UK, 2019; p. 178. Available online: https://cambridgescholars.com/product/978-1-5275-3959-4 (accessed on 29 November 2021).
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Wenham, C.; Smith, J.; Morgan, R. COVID-19: The gendered impacts of the outbreak. Lancet 2020, 395, 846–848. [Google Scholar] [CrossRef] [Green Version]
- Lima, C.K.T.; Carvalho, P.M.D.M.; Lima, I.D.A.A.S.; Nunes, J.V.A.D.O.; Saraiva, J.S.; de Souza, R.I.; da Silva, C.G.L.; Neto, M.L.R. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. 2020, 287, 112915. [Google Scholar] [CrossRef]
- Idowu, S.O.; de Vries, H.J.; Mijatovic, I.; Choi, D. Sustainable Development: Knowledge and Education About Standardisation, 1st ed.; CSR, Sustainability, Ethics & Governance, Ed.; Springer: Cham, Switzerland, 2020; p. 221. Available online: https://link.springer.com/content/pdf/10.1007%2F978-3-030-28715-3.pdf (accessed on 18 September 2021).
- Killgore, W.D.; Cloonan, S.A.; Taylor, E.C.; Dailey, N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 2020, 290, 113117. [Google Scholar] [CrossRef]
- Gong, H.; Hassink, R.; Tan, J.; Huang, D. Regional Resilience in Times of a Pandemic Crisis: The Case of COVID-19 in China. Tijdschr. Econ. Soc. Geogr. 2020, 111, 497–512. [Google Scholar] [CrossRef]
- Khan, K.; Li, Y.; Liu, S.; Li, C. Psychological Distress and Trust in University Management Among International Students During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 679661. [Google Scholar] [CrossRef]
- Torok, M.; Han, J.; Baker, S.; Werner-Seidler, A.; Wong, I.; Larsen, M.E.; Christensen, H. Suicide prevention using self-guided digital interventions: A systematic review and meta-analysis of randomised controlled trials. Lancet Digit. Health 2020, 2, e25–e36. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Suicide. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 18 September 2021).
- Batterham, P.; Sunderland, M.; Slade, T.; Calear, A.; Carragher, N. Assessing distress in the community: Psychometric properties and crosswalk comparison of eight measures of psychological distress. Psychol. Med. 2018, 48, 1316–1324. [Google Scholar] [CrossRef]
- Etheridge, B.; Spantig, L. The gender gap in mental well-being during the COVID-19 outbreak: Evidence from the UK. ISER Inst. Soc. Econ. Res. 2020, 1, 26. Available online: https://www.iser.essex.ac.uk/research/publications/working-papers/iser/2020-08.pdf (accessed on 21 September 2021).
- Denis-Rodríguez, E.; Alarcón, M.E.B.; Delgadillo-Castillo, R.; Denis-Rodríguez, P.B.; Melo-Santiesteban, G. Prevalencia de la ideación suicida en estudiantes de Medicina en Latinoamérica: Un meta análisis / Prevalence of Suicidal Ideation in Medical Students of Latin America: A Meta-analysis. RIDE Rev. Iberoam. Investig. Desarro. Educ. 2017, 8, 387–418. [Google Scholar] [CrossRef] [Green Version]
- Franco, S.A.; Gutiérrez, M.L.; Sarmiento, J.; Cuspoca, D.; Tatis, J.; Castillejo, A.; Barrios, M.; del Pilar Ballesteros-Cabrera, M.; Zamora, S.; Rodríguez, C.I. Suicidio en estudiantes universitarios en Bogotá, Colombia, 2004–2014. Ciência Saúde Coletiva 2017, 22, 269–278. Available online: https://www.redalyc.org/pdf/630/63049169031.pdf (accessed on 21 September 2021). [CrossRef] [PubMed] [Green Version]
- Horesh, D.; Brown, A.D. Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 331–335. [Google Scholar] [CrossRef]
- Jiang, F.; Deng, L.; Zhang, L.; Cai, Y.; Cheung, C.W.; Xia, Z. Review of the Clinical Characteristics of Coronavirus Disease 2019 (COVID-19). J. Gen. Intern. Med. 2020, 35, 1545–1549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wand, A.P.F.; Zhong, B.-L.; Chiu, H.F.K.; Draper, B.; De Leo, D. COVID-19: The implications for suicide in older adults. Int. Psychogeriatr. 2020, 32, 1225–1230. [Google Scholar] [CrossRef]
- Mekonen, E.G.; Workneh, B.S.; Ali, M.S.; Muluneh, N.Y. The Psychological Impact of COVID-19 Pandemic on Graduating Class Students at the University of Gondar, Northwest Ethiopia. Psychol. Res. Behav. Manag. 2021, 14, 109–122. [Google Scholar] [CrossRef]
- Padrón, I.; Fraga, I.; Vieitez, L.; Montes, C.; Romero, E. A Study on the Psychological Wound of COVID-19 in University Students. Front. Psychol. 2021, 12, 589927. [Google Scholar] [CrossRef] [PubMed]
- Faust, J.S.; Shah, S.B.; Du, C.; Li, S.-X.; Lin, Z.; Krumholz, H.M. Suicide Deaths during the Stay-at-Home Advisory in Massachusetts. medRxiv 2020, 10. [Google Scholar] [CrossRef]
- Reger, M.A.; Stanley, I.H.; Joiner, T.E. Suicide Mortality and Coronavirus Disease 2019—A Perfect Storm? JAMA Psychiatry 2020, 77, 1093–1094. [Google Scholar] [CrossRef] [Green Version]
- Parola, A.; Rossi, A.; Tessitore, F.; Troisi, G.; Mannarini, S. Mental Health Through the COVID-19 Quarantine: A Growth Curve Analysis on Italian Young Adults. Front. Psychol. 2020, 11, 567484. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef] [PubMed]
- Baiano, C.; Zappullo, I.; The LabNPEE Group; Conson, M. Tendency to Worry and Fear of Mental Health during Italy’s COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2020, 17, 5928. [Google Scholar] [CrossRef] [PubMed]
- Kleiman, E.M.; Turner, B.J.; Fedor, S.; Beale BA, E.E.; Picard ScD, R.W.; Huffman, J.C.; Nock, M.K. Digital phenotyping of suicidal thoughts. Depress. Anxiety 2018, 35, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.W.; Gao, Y.; Tam, W.W.S. Anxiety among university students during the SARS epidemic in Hong Kong. Stress Health 2007, 23, 31–35. [Google Scholar] [CrossRef]
- Golpe, S.; Isorna, M.; Barreiro, C.; Braña, T.; Rial, A. Consumo intensivo de alcohol en adolescentes: Prevalencia, conductas de riesgo y variables asociadas. Adicciones 2017, 29, 256–267. [Google Scholar] [CrossRef]
- Lisha, N.E.; Sussman, S. Relationship of high school and college sports participation with alcohol, tobacco, and illicit drug use: A review. Addict. Behav. 2010, 35, 399–407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pierobon, M.; Barak, M.; Hazrati, S.; Jacobsen, K.H. Alcohol Consumption and Violence among Argentine Adolescents. J. Pediatr. 2013, 89, 100–107. [Google Scholar] [CrossRef]
- Rial, A.; Kim-Harris, S.; Knight, J.R.; Araujo, M.; Gomez, P.; Braña, T.; Varela, J.; Golpe, S. Validación empírica del CRAFFT Abuse Screening Test en una muestra de adolescentes españoles. Adicciones 2018, 31, 160–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H. “Chris” Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D. Collision of the COVID-19 and Addiction Epidemics. Ann. Intern. Med. 2020, 173, 61–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiao, H.; Shu, W.; Li, M.; Li, Z.; Tao, F.; Wu, X.; Yu, Y.; Meng, H.; Vermund, S.H.; Hu, Y. Social Distancing among Medical Students during the 2019 Coronavirus Disease Pandemic in China: Disease Awareness, Anxiety Disorder, Depression, and Behavioral Activities. Int. J. Environ. Res. Public Health 2020, 17, 5047. [Google Scholar] [CrossRef]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Castillo Apraiz, J.; Cepeda Carrión, G.; Roldán, J.L. Manual de Partial Least Squares Structural Equation Modeling (PLS-SEM), 2nd ed.; OmniaScience: Tarrasa, Spain, 2019; Available online: https://www.aemark.org/index.php/es-es/component/content/article/89-noticias/430-publicacion-del-libro-manual-de-partial-least-squares-structural-equation-modeling-pls-sem-segunda-edicion?Itemid=558#:~:text=https%3A//www.omniascience.com/books/index.php/scholar/catalog/book/108 (accessed on 13 September 2021).
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Spielberger, C.D. Manual for the State-Trait Anxiety Inventory (Form Y1–Y2); Consulting Psychologists Press: Palo Alto, CA, USA, 1983; Volume IV, Available online: https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=380614 (accessed on 23 September 2021).
- Beck, A.T.; Brown, G.K.; Steer, R.A. Psychometric characteristics of the Scale for Suicide Ideation with psychiatric outpatients. Behav. Res. Ther. 1997, 35, 1039–1046. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De La Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Dion, M.-J.; Tousignant, P.; Bourbeau, J.; Menzies, D.; Schwartzman, K. Feasibility and reliability of health-related quality of life measurements among tuberculosis patients. Qual. Life Res. 2004, 13, 653–665. [Google Scholar] [CrossRef]
- Martínez-Martí, M.L.; Ruch, W. Character strengths predict resilience over and above positive affect, self-efficacy, optimism, social support, self-esteem, and life satisfaction. J. Posit. Psychol. 2017, 12, 110–119. [Google Scholar] [CrossRef]
- OECD; The World Bank. Health at a Glance: Latin America and the Caribbean. 2020. Available online: https://www.oecd.org/health/health-at-a-glance-latin-america-and-the-caribbean-2020-6089164f-en.htm (accessed on 23 September 2021).
- Killgore, W.D.; Cloonan, S.A.; Taylor, E.C.; Fernandez, F.-X.; Grandner, M.A.; Dailey, N.S. Suicidal ideation during the COVID-19 pandemic: The role of insomnia. Psychiatry Res. 2020, 290, 113134. [Google Scholar] [CrossRef]
- Son, C.; Hegde, S.; Smith, A.; Wang, X.; Sasangohar, F. Effects of COVID-19 on College Students’ Mental Health in the United States: Interview Survey Study. J. Med. Internet Res. 2020, 22, e21279. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.M. Stigma and student mental health in higher education. High. Educ. Res. Dev. 2010, 29, 259–274. [Google Scholar] [CrossRef]
- Zuckerman, D.M. Stress, self-esteem, and mental health: How does gender make a difference? Sex Roles 1989, 20, 429–444. [Google Scholar] [CrossRef]
- Jacobson, N.C.; Lekkas, D.; Price, G.; Heinz, M.V.; Song, M.; O’Malley, A.J.; Barr, P.J. Flattening the Mental Health Curve: COVID-19 Stay-at-Home Orders Are Associated with Alterations in Mental Health Search Behavior in the United States. JMIR Ment. Health 2020, 7, e19347. [Google Scholar] [CrossRef] [PubMed]
- Acharya, L.; Jin, L.; Collins, W. College life is stressful today—Emerging stressors and depressive symptoms in college students. J. Am. Coll. Health 2018, 66, 655–664. [Google Scholar] [CrossRef] [PubMed]
| Hypothesis | Exogenous Variables | Influence | Sign | Endogenous Variables |
|---|---|---|---|---|
| 1 | E3 Uncertainty in the face of the pandemic | ====˃˃ | + | E10 Negative emotional states |
| 2 | E3 Uncertainty in the face of the pandemic | ====˃˃ | − | E14 Resilience against COVID-19 |
| 3 | E3 Uncertainty in the face of the pandemic | ====˃˃ | + | E11 Suicide ideation |
| 4 | E10 negative emotional states | ====˃˃ | + | |
| 5 | E14 Resilience against COVID-19 | ====˃˃ | − | |
| 6 | E3 Uncertainty in the face of the pandemic | ====˃˃ | + | E12 Drug addiction and alcoholism |
| 7 | E10 negative emotional states | ====˃˃ | + | |
| 8 | E14 Resilience against COVID-19 | ====˃˃ | − |
| Hypothesis | Expression |
|---|---|
| 1 | “E3 Uncertainty in the face of the pandemic influences in a direct significant way in E10 negative emotional states”. |
| 2 | “E3 Uncertainty in the face of the pandemic influences in an inverse significant way in E14 resilience against COVID-19”. |
| 3 | “E3 Uncertainty in the face of the pandemic influences in a direct significant way in E11 suicide ideation”. |
| 4 | “E10 Negative emotional states influence in a direct significant way in E11 suicide ideation”. |
| 5 | “E14 Resilience against COVID-19 influences in an inverse significant way in E11 suicide ideation”. |
| 6 | “E3 Uncertainty in the face of the pandemic influences in a direct significant way in E12 drug addiction and alcoholism”. |
| 7 | “E10 Negative emotional states influence in a direct significant way in E12 drug addiction and alcoholism”. |
| 8 | “E14 Resilience against COVID-19 influences in an inverse significant way in E12 drug addiction and alcoholism”. |
| Subscales | Mean | Standard Deviation | Cronbach’s Alpha | Rho_A | R-Squared | CR | AVE | E10 | E11 | E12 | E3 | E14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| E10 Negative emotional states | 2.53 | 0.78 | 0.73 | 0.74 | 0.220 | 0.85 | 0.65 | 0.81 | ||||
| E11 Suicide ideation | 1.22 | 0.48 | 0.83 | 0.86 | 0.173 | 0.88 | 0.65 | 0.306 ** | 0.81 | |||
| E12 Drug addiction and alcoholism | 1.10 | 0.38 | 0.80 | 0.80 | 0.028 | 0.88 | 0.72 | 0.130 ** | 0.264 ** | 0.85 | ||
| E3 Uncertainty in the face of the pandemic | 2.35 | 1.10 | 0.79 | 0.82 | - | 0.88 | 0.70 | 0.461 ** | 0.254 ** | 0.177 ** | 0.84 | |
| E14 Resilience against COVID-19 | 3.66 | 0.94 | 0.85 | 0.85 | 0.017 | 0.90 | 0.68 | −0.283 ** | −3.36 ** | −0.111 ** | −0.127 ** | 0.83 |
| Subscales | Sex | N | Mean | Deviation Dev. | Average Error Dev. | |
|---|---|---|---|---|---|---|
| E10 Negative emotional states | Women | 3551 | 2.62 | 0.76 | 0.01 | ** |
| Men | 2006 | 2.38 | 0.79 | 0.02 | ||
| E11 Suicide ideation | Women | 3551 | 1.23 | 0.48 | 0.01 | |
| Men | 2006 | 1.22 | 0.48 | 0.01 | ||
| E12 Drug addiction and alcoholism | Women | 3551 | 1.08 | 0.35 | 0.01 | ** |
| Men | 2006 | 1.12 | 0.43 | 0.01 | ||
| E14 Resilience against COVID-19 | Women | 3551 | 3.63 | 0.93 | 0.02 | ** |
| Men | 2006 | 3.71 | 0.94 | 0.02 | ||
| E3 Uncertainty in the face of the pandemic | Women | 3551 | 2.49 | 1.11 | 0.02 | ** |
| Men | 2006 | 2.11 | 1.05 | 0.02 |
| Independent Samples Testing | Levene’s Test for Equality of Variances t-Test for Equality of Means | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Subscales | F | Sig. | t | DF | Two-Tailed Sig. | Mean Difference | SE Difference | 95% of Confidence Interval of the Difference | |||
| Lower | Upper | ||||||||||
| E10 Negative emotional states | Equal variances are assumed Equal variances are not assumed | 3.292 | 0.07 | 10.953 | 5555.00 | 0 | 0.24 | 0.02 | 0.19 | 0.28 | ** |
| 10.858 | 4053.05 | 0 | 0.24 | 0.02 | 0.19 | 0.28 | ** | ||||
| E11 Suicide ideation | Equal variances are assumed Equal variances are not assumed | 0.012 | 0.912 | 0.738 | 5555.00 | 0.46 | 0.01 | 0.01 | −0.02 | 0.04 | |
| 0.738 | 4153.59 | 0.46 | 0.01 | 0.01 | −0.02 | 0.04 | |||||
| E12 Drug addiction and alcoholism | Equal variances are assumed Equal variances are not assumed | 39.6 | 0 | −3.329 | 5555.00 | 0 | −0.04 | 0.01 | −0.06 | −0.01 | ** |
| −3.159 | 3553.66 | 0 | −0.04 | 0.01 | −0.06 | −0.01 | ** | ||||
| E14 Resilience against COVID-19 | Equal variances are assumed Equal variances are not assumed | 0.34 | 0.56 | −2.796 | 5555.00 | 0.01 | −0.07 | 0.03 | −0.12 | −0.02 | ** |
| −2.787 | 4120.29 | 0.01 | −0.07 | 0.03 | −0.12 | −0.02 | ** | ||||
| E3 Uncertainty in the face of the pandemic | Equal variances are assumed Equal variances are not assumed | 17.748 | 0 | 12.377 | 5555.00 | 0 | 0.38 | 0.03 | 0.32 | 0.44 | ** |
| 12.598 | 4384.21 | 0 | 0.38 | 0.03 | 0.32 | 0.44 | ** | ||||
| Hypothesis | Subscale | Original (O) Sample | Mean (M) of the Sample | Standard Deviation (Std Dev) | T Statistics (|O/Std Dev|) | p Values |
|---|---|---|---|---|---|---|
| H4 | E10 Negative emotional states -> E11 Suicide ideation | 0.152 | 0.151 | 0.013 | 11.341 | 0 |
| H5 | E14 Resilience against COVID-19 -> E11 Suicide ideation | −0.27 | −0.27 | 0.014 | 18.947 | 0 |
| H1 | E3 Uncertainty in the face of the pandemic -> E10 Negative emotional states | 0.47 | 0.469 | 0.01 | 45.374 | 0 |
| H2 | E3 Uncertainty in the face of the pandemic -> E11 Suicide ideation | 0.15 | 0.151 | 0.016 | 9.586 | 0 |
| H3 | E3 Uncertainty in the face of the pandemic -> E14 Resilience against COVID-19 | −0.13 | −0.131 | 0.014 | 9.474 | 0 |
| Hypothesis | Exogenous Variables | Influence | Standardized Beta Coefficient | Endogenous Variables | R Squared | Decision |
|---|---|---|---|---|---|---|
| 1 | E3 Uncertainty facing the pandemic | ====>> | 0.47 | E10 Negative emotional states | 0.2021 | Accept |
| 2 | E3 Uncertainty facing the pandemic | ====>> | −0.13 | E14 Resilience against COVID-19 | 0.017 | Accept |
| 3 | E3 Uncertainty facing the pandemic | ====>> | 0.15 | E11 Suicide ideation | 0.173 | Accept |
| 4 | E10 Negative emotional states | ====>> | 0.152 | Accept | ||
| 5 | E14 Resilience against COVID-19 | ====>> | −0.27 | Accept |
| Hypotheses | Method | Path | Phat Coefficient | Indirect Effect | Standard dv | Total Effects | VAF | T | Sig. | p-Value | Decision |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Incremental moderator effect/H1, H4, H3 | Step 1. Direct effect (without mediation) | E3 ==˃E11 | 0.255 | N/A | 0.0128 | 0.255 | N/A | 19.86 | *** | 0 | Accept |
| Step 2. Indirect effect (with mediation) | E3 ==˃E11 | 0.151 | 0.106 | N/A | 0.412 | 15.39 | *** | 0 | |||
| E3 ==˃E10 | 0.469 | 0.0069 | 0.257 | ||||||||
| E10 ==˃E11 | 0.226 | ||||||||||
| Hypotheses | Method | Path | Path Coefficient | Indirect Effects | Standard Dv | Total Effects | VAF | T | Sig. | p-Value | Decision |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Decreasing moderating effect/H2, H3, H5 | Step 1. Direct effect (without mediation) | E3 ==˃E11 | 0.255 | N/A | 0.013 | 0.255 | N/A | 19.864 | ** | 0.000 | Reject |
| Step 2. Indirect effect (with mediation) | E3 ==˃E11 | 0.217 | 0.040 | N/A | 0.155 | 8.626 | ** | 0.000 | |||
| E3 ==˃E14 | −0.132 | 0.005 | 0.257 | ||||||||
| E14 ==˃E11 | −0.301 | ||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Rivera, B.R.; García-Alcaraz, J.L.; Mendoza-Martínez, I.A.; Olguin-Tiznado, J.E.; García-Alcaráz, P.; Aranibar, M.F.; Camargo-Wilson, C. Influence of COVID-19 Pandemic Uncertainty in Negative Emotional States and Resilience as Mediators against Suicide Ideation, Drug Addiction and Alcoholism. Int. J. Environ. Res. Public Health 2021, 18, 12891. https://doi.org/10.3390/ijerph182412891
García-Rivera BR, García-Alcaraz JL, Mendoza-Martínez IA, Olguin-Tiznado JE, García-Alcaráz P, Aranibar MF, Camargo-Wilson C. Influence of COVID-19 Pandemic Uncertainty in Negative Emotional States and Resilience as Mediators against Suicide Ideation, Drug Addiction and Alcoholism. International Journal of Environmental Research and Public Health. 2021; 18(24):12891. https://doi.org/10.3390/ijerph182412891
Chicago/Turabian StyleGarcía-Rivera, Blanca Rosa, Jorge Luis García-Alcaraz, Ignacio Alejandro Mendoza-Martínez, Jesús Everardo Olguin-Tiznado, Pedro García-Alcaráz, Mónica Fernanda Aranibar, and Claudia Camargo-Wilson. 2021. "Influence of COVID-19 Pandemic Uncertainty in Negative Emotional States and Resilience as Mediators against Suicide Ideation, Drug Addiction and Alcoholism" International Journal of Environmental Research and Public Health 18, no. 24: 12891. https://doi.org/10.3390/ijerph182412891
APA StyleGarcía-Rivera, B. R., García-Alcaraz, J. L., Mendoza-Martínez, I. A., Olguin-Tiznado, J. E., García-Alcaráz, P., Aranibar, M. F., & Camargo-Wilson, C. (2021). Influence of COVID-19 Pandemic Uncertainty in Negative Emotional States and Resilience as Mediators against Suicide Ideation, Drug Addiction and Alcoholism. International Journal of Environmental Research and Public Health, 18(24), 12891. https://doi.org/10.3390/ijerph182412891











