Diagnostic Difficulties in a Case of Fetal Ventricular Tachycardia Associated with Neonatal COVID Infection: Case Report
Abstract
:1. Introduction
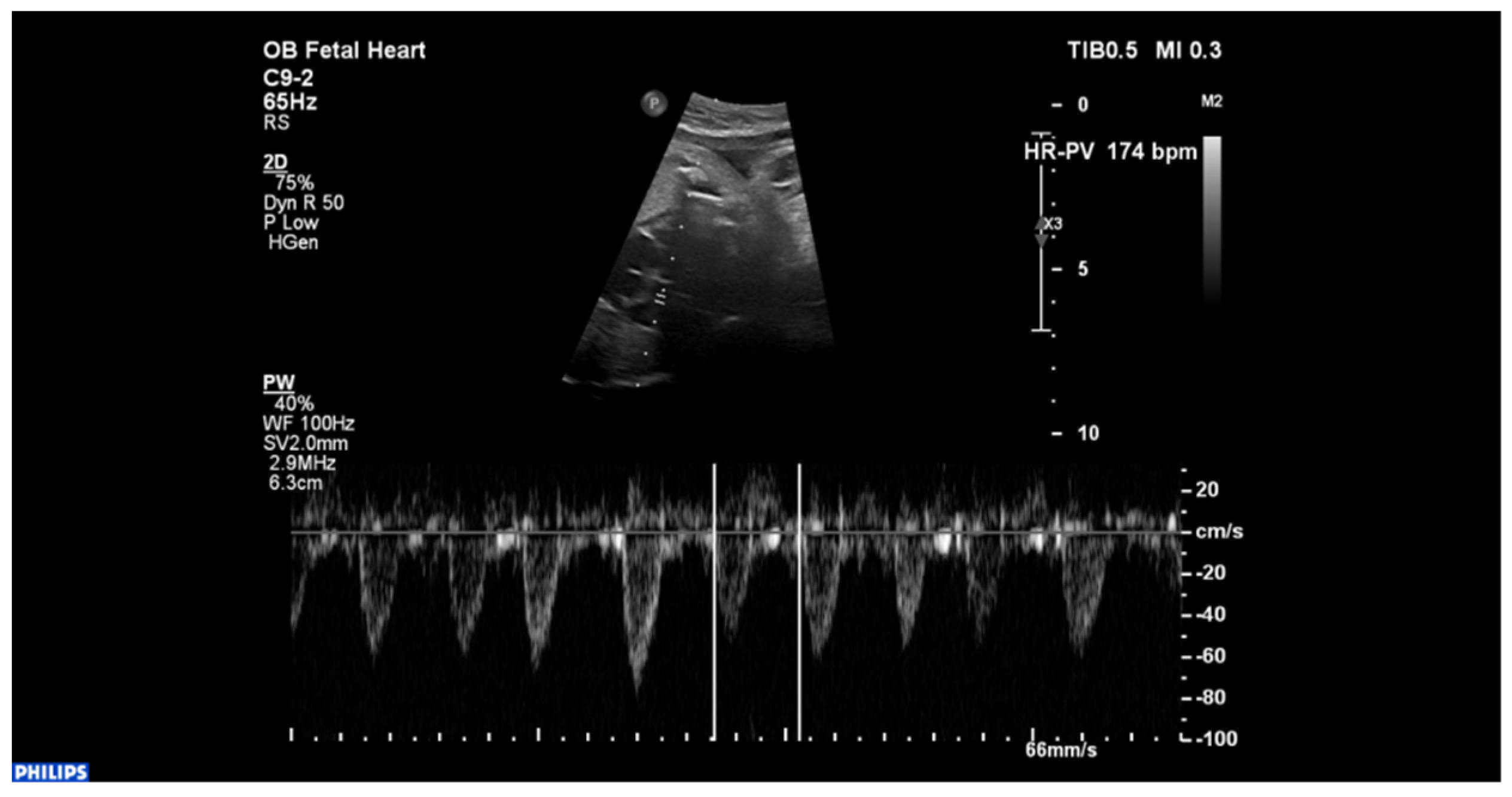
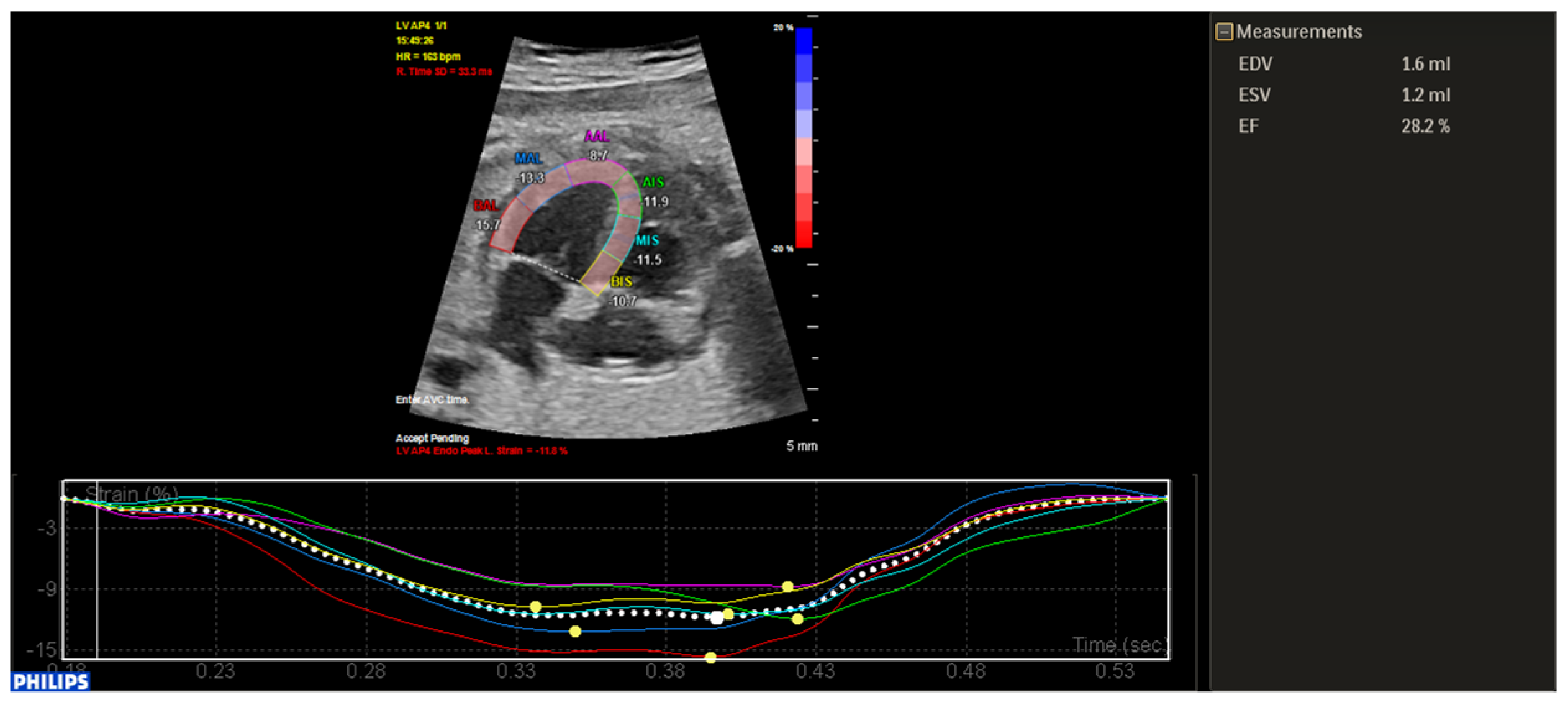
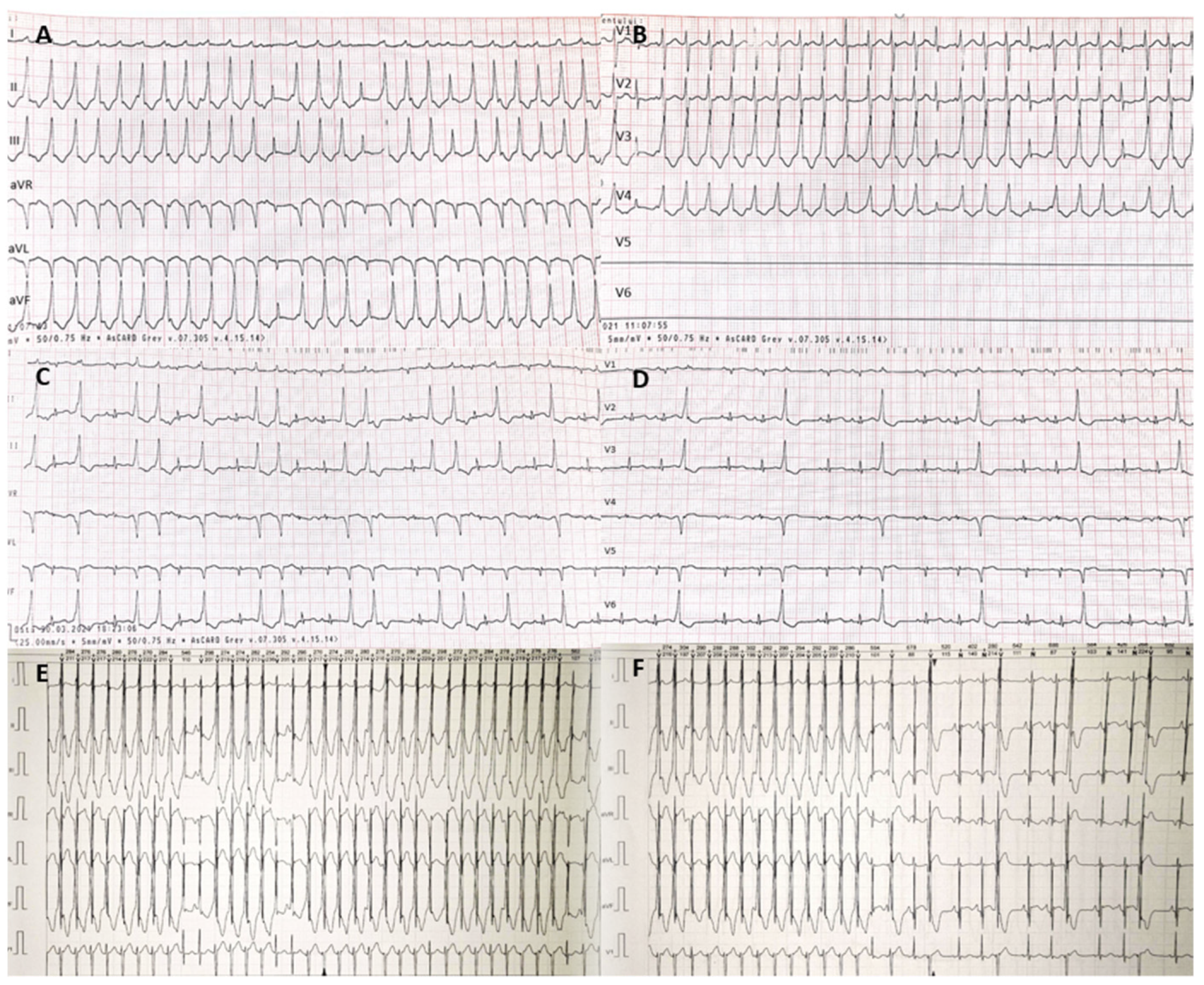
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parri, N.; Lenge, M.; Cantoni, B.; Arrighini, A.; Romanengo, M.; Urbino, A.; Da Dalt, L.; Verdoni, L.; Giacchero, R.; Lanari, M.; et al. COVID-19 in 17 Italian Pediatric Emergency Departments. Pediatrics 2020, 146, e20201235. [Google Scholar] [CrossRef]
- Grimaud, M.; Starck, J.; Levy, M.; Marais, C.; Chareyre, J.; Khraiche, D.; Leruez-Ville, M.; Quartier, P.; Léger, P.L.; Geslain, G.; et al. Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children. Ann. Intensive Care 2020, 10, 69. [Google Scholar] [CrossRef]
- Oualha, M.; Bendavid, M.; Berteloot, L.; Corsia, A.; Lesage, F.; Vedrenne, M.; Salvador, E.; Grimaud, M.; Chareyre, J.; de Marcellus, C.; et al. Severe and fatal forms of COVID-19 in children. Arch. Pédiatrie 2020, 27, 235–238. [Google Scholar] [CrossRef]
- Swann, O.V.; Holden, K.A.; Turtle, L.; Pollock, L.; Fairfield, C.J.; Drake, T.M.; Sohan, S.; Egan, C.; Hardwick, H.E.; Halpin, S.; et al. Clinical characteristics of children and young people admitted to hospital with Covid-19 in United Kingdom: Prospective multicenter observational cohort study. BMJ 2020, 370, m3249. [Google Scholar] [CrossRef]
- Irabien-Ortiz, A.; Carreras-Mora, J.; Sionis, A.; Pamies, J.; Montiel, J.; Tauron, M. Fulminant myocarditis due to COVID-19. Rev. Esp. Cardiol. 2020, 73, 503–515. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA 2020, 5, 811–818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gotzinger, F.; Santiago-Garcia, B.; Noguera-Julian, A.; Lanaspa, M.; Lancella, L.; Carducci, F.I.C.; Gabrovska, N.; Velizarova, S.; Prunk, P.; Osterman, V.; et al. COVID-19 in children and adolescents in Europe: A multinational, multicentre cohort study. Lancet Child. Adolesc. Health 2020, 4, 653–661. [Google Scholar] [CrossRef]
- Amiraskari, R.; Sayarifard, E.; Kharrazi, H.; Nasefar, N.; Sayarifard, A. Neonatal SARS-CoV-2 infection and congenital myocarditis: A case report and literature review. Arch. Pediatr. Infect. Dis. 2020, 8, e103504. [Google Scholar] [CrossRef]
- Saileela, R.; Sachdeva, S.; Saggu, D.K.; Koneti, N.R. Ventricular Tachycardia in a Fetus: Benign Course of a Malignant Arrhythmia. J. Obs. India 2019, 69, 383–386. [Google Scholar] [CrossRef]
- Yang, P.; Liu, P.; Li, D.; Zhao, D. Corona virus disease 2019, a growing threat to children? J. Infect. 2020, 80, 671–693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Tong, S. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics 2020, 145, e20200702. [Google Scholar] [CrossRef] [Green Version]
- Qiu, H.; Wu, J.; Liang, H.; Luo, Y.; Song, Q.; Chen, D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: An observational cohort study. Lancet Infect. Dis. 2020, 20, 689–696. [Google Scholar] [CrossRef] [Green Version]
- Sharma, M.; Gorstein, S.; Aldrich, M.L.; Hsu, D.T.; Choueiter, N.F. Reversible myocardial injury associated with SARS-CoV-2 in an infant. JACC Case Rep. 2020, 2, 2348–2352. [Google Scholar] [CrossRef] [PubMed]
- Kesici, S.; Aykan, H.H.; Orhan, D.; Bayrakci, B. Fulminant COVID-19-related myocarditis in an infant. Cardiovascular Flashlight. 2020, 41, 3021. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, I.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, I.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Zhu, H.; Wang, I.; Fang, C.; Peng, S.; Zhang, I.; Chang, G.; Xia, S.; Zhou, W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 2020, 9, 51–60. [Google Scholar] [CrossRef]
- Tschope, C.; Ammirati, E.; Bozkurt, B.; Caforio, A.L.P.; Cooper, L.T.; Felix, S.B.; Hare, J.M.; Heidecker, B.; Heymans, S.; Hubner, N.; et al. Myocarditis and inflammatory cardiomyopathy: Current evidence and future directions. Nature 2021, 18, 169–193. [Google Scholar] [CrossRef]
- Coomes, E.A.; Haghbayan, H. Interleukin-6 in Covid-19: A systematic review and meta-analysis. Rev. Med. Virol. 2020, 30, 1–9. [Google Scholar] [CrossRef]
- Liu, F.; Li, L.; Xu, M.; Wu, J.; Luo, D.; Zhu, Y.; Li, B.; Song, X.; Zhou, X. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J. Clin. Virol. 2020, 127, 104370. [Google Scholar] [CrossRef]
- Dasgupta, S.; Iannucci, G.; Mao, C.; Clabby, M.; Oster, M.E. Myocarditis in the pediatric population: A review. Congenit. Heart Dis. 2019, 14, 868–877. [Google Scholar] [CrossRef] [PubMed]
| Test | Reference Range | Day 3 after Birth | Day of Illness | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | 5 | 7 | 10 | 11 | 12 | 13 | 15 | 19 | 24 | 27 | |||
| White blood cell | 5–20 × 10³/µL | 8.85 | 13.03 | 13.67 | - | 14.44 | - | - | 9.83 | 11.45 | 10.33 | 12.37 | 10.50 |
| Lymphocytes | 2–17 × 10³/µL | 3.44 | 3.23 | 7.48 | - | 4.64 | - | - | 3.05 | 4.13 | 3.33 | 2.06 | 2.84 |
| Eosinophils | 0.03–0.4 × 10³/µL | 0.41 | 0.00 | 0.42 | - | 0.2 | - | - | 0.33 | 0.34 | 0.01 | 0.01 | 0.03 |
| Basophils | 0.01–0.08 × 10³/µL | 0.03 | 0.01 | 0.01 | - | 0.06 | - | - | 0.09 | 0.06 | 0.02 | 0.01 | 0.01 |
| Hemoglobin | 15.5–21.5 g/dL | 17.00 | 14.1 | 14.60 | - | 13.40 | - | - | 11.3 | 11.8 | 11.1 | 9.9 | 11.3 |
| Hematocrit | 44–60% | 47.80 | 41.1 | 42.10 | - | 38.10 | - | - | 33.9 | 34 | 32.1 | 29.1 | 30.5 |
| Platelets | 150–450 × 10³/µL | 246 | 391 | 329 | - | 659 | - | - | 812 | 942 | 939 | 829 | 517 |
| CRP | 0–5 mg/L | 1.34 | 26.00 | 9.86 | 10.11 | 3.58 | - | - | 0.80 | 0.38 | 0.37 | - | 0.30 |
| Procalcitonin | <0.5 ng/mL | - | 0.28 | - | - | - | - | - | - | - | - | negative | - |
| Ferritin | 15–120 ng/mL | - | - | - | 339.00 | 351.40 | - | 443.80 | - | 401.90 | 370.00 | - | - |
| LDH | 125–220 U/L | - | - | - | - | - | 411 | - | - | 195 | - | 257.00 | 297 |
| D-dimer | <400 ng/mL | 762.00 | 729 | 1402.00 | 2559.60 | 949.66 | - | - | 1005.53 | 496.59 | - | <200 | - |
| Tn-I | 0–15.6 pg/mL | 7.5 | 25.70 | 50.90 | 117.40 | 87.50 | - | - | 134.70 | 48.30 | 24.40 | - | negative |
| CK-MB | 0–24 U/L | 42.70 | 16.70 | 44.20 | 74.00 | 37.10 | - | 42.90 | - | 31.70 | 25.60 | - | 38 |
| CK | 29–168 U/L | 284.00 | 48.00 | 56.00 | - | 31.00 | - | 38.00 | - | 29 | 29.00 | 20.00 | 31 |
| NTproBNP | <450 pg/mL | - | - | - | - | - | - | 645.40 | - | - | 140.22 | - | 22.91 |
| AST | 0–33 U/L | 56.00 | 19.00 | - | - | - | 35.00 | 33.00 | - | - | - | 22.00 | 24 |
| ALT | 0–55 U/L | 38.00 | 17.00 | - | - | - | 39.00 | 41.00 | - | 29 | 34.00 | 26.5 | 32 |
| Urea | 10.91–40.66 mg/dL | 7.70 | 7.50 | 11.80 | - | - | 36.00 | 48.80 | 40.70 | 47.1 | 55.00 | 57.5 | 47 |
| Creatinine | 0.57–1.11 mg/dL | 0.55 | 0.70 | 0.59 | - | - | 0.50 | 0.63 | 0.59 | 0.61 | 0.52 | 0.43 | 0.48 |
| Albumin | 3.8–5.4 g/dL | - | - | 3.10 | - | - | - | - | - | - | - | - | 3.9 |
| Lactic acid | 0.9–1.7 mmol/L | 2.1 | - | 1.7 | - | 2.6 | 1.2 | 2.5 | 1.9 | 1.9 | - | - | 3.95 |
| Na | 133–146 mmol/L | 139.00 | 159.00 | 140.00 | - | - | 133.00 | - | 125 | 131 | 131.00 | 136.00 | 128.8 |
| K | 3.7–5.9 mmol/L | 3.63 | 4.80 | 6.36 | - | - | 5.60 | - | 5.75 | 4.68 | 6.49 | - | 3.61 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gozar, L.; Șuteu, C.C.; Gabor-Miklosi, D.; Cerghit-Paler, A.; Făgărășan, A. Diagnostic Difficulties in a Case of Fetal Ventricular Tachycardia Associated with Neonatal COVID Infection: Case Report. Int. J. Environ. Res. Public Health 2021, 18, 12796. https://doi.org/10.3390/ijerph182312796
Gozar L, Șuteu CC, Gabor-Miklosi D, Cerghit-Paler A, Făgărășan A. Diagnostic Difficulties in a Case of Fetal Ventricular Tachycardia Associated with Neonatal COVID Infection: Case Report. International Journal of Environmental Research and Public Health. 2021; 18(23):12796. https://doi.org/10.3390/ijerph182312796
Chicago/Turabian StyleGozar, Liliana, Carmen Corina Șuteu, Dorottya Gabor-Miklosi, Andreea Cerghit-Paler, and Amalia Făgărășan. 2021. "Diagnostic Difficulties in a Case of Fetal Ventricular Tachycardia Associated with Neonatal COVID Infection: Case Report" International Journal of Environmental Research and Public Health 18, no. 23: 12796. https://doi.org/10.3390/ijerph182312796
APA StyleGozar, L., Șuteu, C. C., Gabor-Miklosi, D., Cerghit-Paler, A., & Făgărășan, A. (2021). Diagnostic Difficulties in a Case of Fetal Ventricular Tachycardia Associated with Neonatal COVID Infection: Case Report. International Journal of Environmental Research and Public Health, 18(23), 12796. https://doi.org/10.3390/ijerph182312796






