Acceptance of COVID-19 Vaccination among Healthcare and Non-Healthcare Workers of Hospitals and Outpatient Clinics in the Northern Region of Slovakia
Abstract
:1. Introduction
2. Materials and Methods
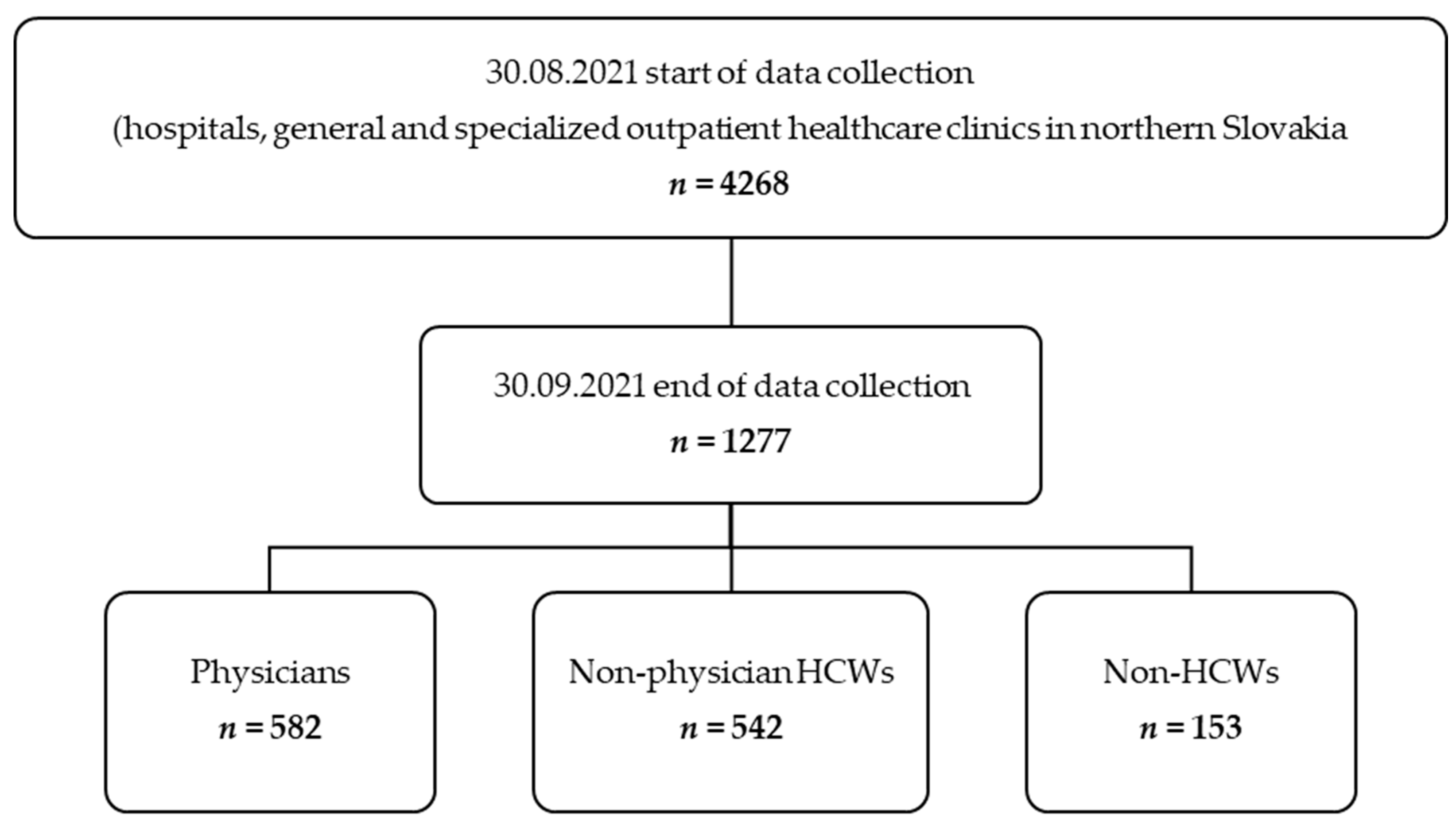
2.1. Study Population
2.2. Survey Questionnaire
2.3. Statistical Analyses
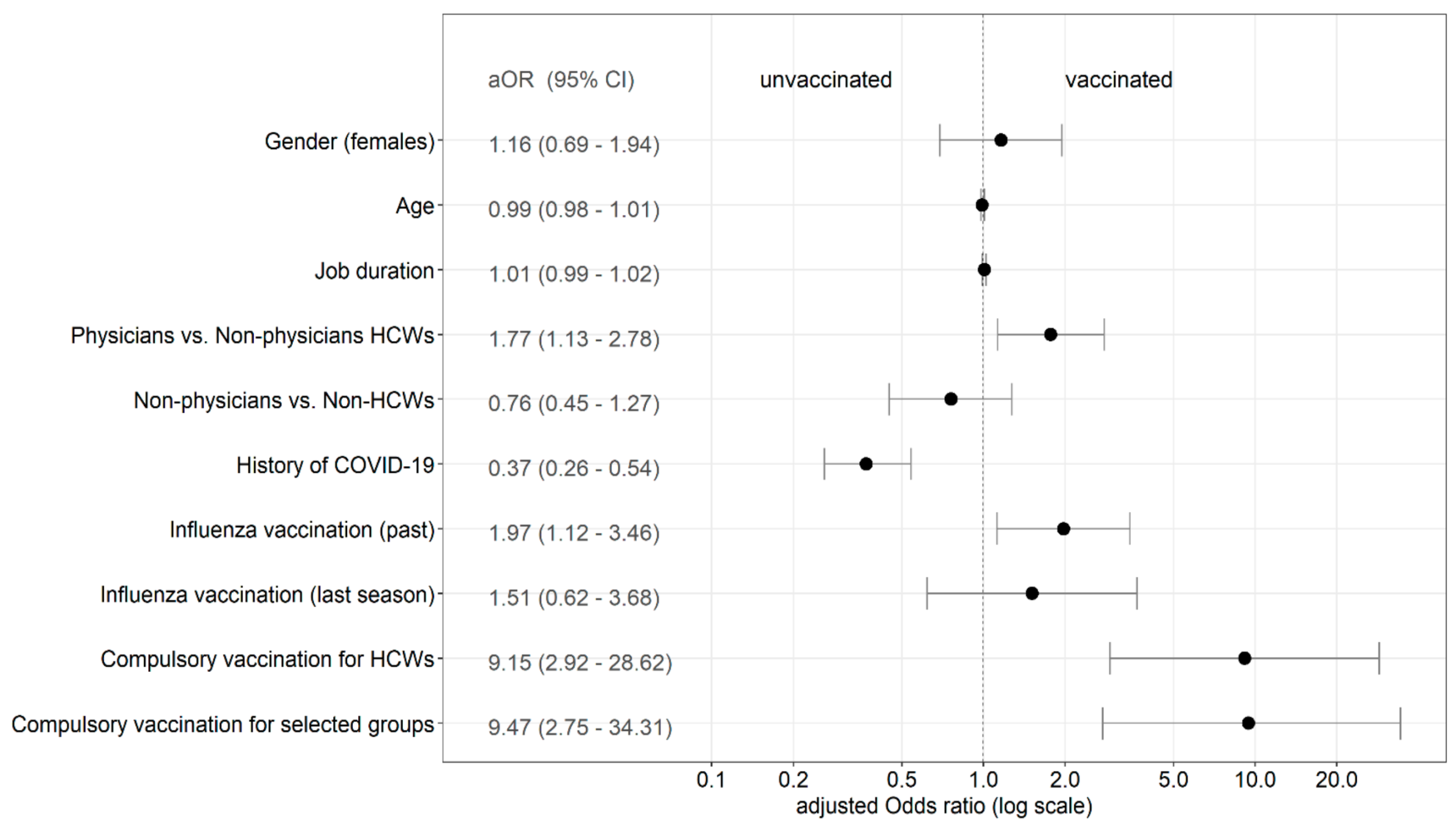
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Director-General’s Opening Remarks at the Media Briefing on COVID-19–11 March. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 18 October 2021).
- Ing, E.B.; Xu, Q.A.; Salimi, A.; Torun, N. Physician Deaths from Corona Virus (COVID-19) Disease. Occup. Med. 2020, 70, 370–374. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). COVID-19 Vaccines. 2021. Available online: https://www.who.int/westernpacific/emergencies/covid-19/covid-19-vaccines (accessed on 19 October 2021).
- World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard. 2021. Available online: https://covid19.who.int/ (accessed on 16 November 2021).
- Ministry of Health of Slovak Republic. National Vaccination Strategy against COVID-19 in the Conditions of the Slovak Republic; Ministry of Health of Slovak Republic: Bratislava, Slovakia, 2021. Available online: https://www.health.gov.sk/Zdroje?/Sources/tlacove_spravy/covid-19/Strategia-ockovania-COVID-19.pdf (accessed on 12 September 2021).
- Bartsch, S.M.; O’Shea, K.J.; Ferguson, M.C.; Bottazzi, M.E.; Wedlock, P.T.; Strych, U.; McKinnell, J.A.; Siegmund, S.S.; Cox, S.N.; Hotez, P.J.; et al. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am. J. Prev. Med. 2020, 59, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Social Care of United Kingdom. Coronavirus (COVID-19) Vaccination of People Working or Deployed in Care Homes: Operational Guidance; Department of Health and Social Care: London, UK, 2021. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1010601/coronavirus-covid-19-vaccination-of-people-working-or-deployed-in-care-homes-operational-guidance.pdf (accessed on 7 October 2021).
- Decree Law 1 April 2021, No. 44. Misure Urgenti per il Contenimento Dell’Epidemia da COVID-19, in Materia di Vaccinazioni Anti SARS-CoV-2, di Giustizia e di Concorsi Pubblici. GU Serie Generale [Official Gazette of Italian Republic] n. 79 del 01-04-202.1 [Internet]. 1 April 2021. Available online: http://www.normattiva.it/eli/stato/DECRETO-LEGGE/2021/04/01/44/CONSOLIDATED (accessed on 18 October 2021).
- Wise, J. Covid-19: France and Greece make vaccination mandatory for healthcare workers. BMJ 2021, 374, n1797. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Slovak Republic (NCZI National Health Information Centre). Number and Structure of Health Professionals Annual Report; NCZI National Health Information Centre: Bratislava, Slovakia, 2021. Available online: http://www.nczisk.sk/Statisticke_vystupy/Tematicke_statisticke_vystupy/Siet_poskytovatelov_zdravotnej_starostlivosti/Pages/default.aspx (accessed on 2 October 2021).
- Stepanek, L.; Janosikova, M.; Nakladalova, M.; Stepanek, L.; Borikova, A.; Vildova, H. Motivation to COVID-19 Vaccination and Reasons for Hesitancy in Employees of a Czech Tertiary Care Hospital: A Cross-Sectional Survey. Vaccines 2021, 9, 863. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). Threat Assessment Brief: Emergence of SARS-CoV-2 B.1.617 Variants in India and Situation in the EU/EEA; European Centre for Disease Prevention and Control (ECDC): Stockholm, Sweden, 2021. Available online: https://www.ecdc.europa.eu/en/publications-data/threat-assessment -emergence-sars-cov-2-b1617-variants (accessed on 2 October 2021).
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARSCoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Lopez, B.J.; Andrews, N.; Gower, C.; Gallagher, E.; Simmons, R.; Thelwall, S.; Stowe, J.; Tessier, E.; Groves, N.; Dabrera, G.; et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N. Engl. J. Med. 2021, 385, 585–594. [Google Scholar] [CrossRef] [PubMed]
- COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020, 107, 1440–1449. [Google Scholar]
- Shehata, I.M.; Elhassan, A.; Jung, J.W.; Urits, I.; Viswanath, O.; Kaye, A.D. Elective cardiac surgery during the COVID-19 pandemic: Proceed or postpone? Best Pract. Res. Clin. Anaesthesiol. 2020, 343, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N. Intracranial hemorrhage and COVID-19, but please do not forget “old diseases” and elective surgery. Brain Behav. Immun. 2021, 92, 207–208. [Google Scholar] [CrossRef] [PubMed]
- Herzog, R.; Álvarez-Pasquin, M.J.; Díaz, C.; Del Barrio, J.L.; Estrada, J.M.; Gil, A. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 2013, 13, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.W.; Wen, W.; Wang, N.; Zhou, M.Y.; Wang, C.Y.; Ni, J.; Jiang, J.J.; Zhang, X.W.; Feng, Z.H.; Cheng, Y.R. COVID-19 Vaccination Acceptance Among Healthcare Workers and Non-healthcare Workers in China: A Survey. Front. Public Health 2021, 9, 709056. [Google Scholar] [CrossRef] [PubMed]
- Holzmann-Littig, C.; Braunisch, M.C.; Kranke, P.; Popp, M.; Seeber, C.; Fichtner, F.; Littig, B.; Carbajo-Lozoya, J.; Allwang, C.; Frank, T.; et al. COVID-19 Vaccination Acceptance and Hesitancy among Healthcare Workers in Germany. Vaccines 2021, 9, 777. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Slovak Republic (NCZI National Health Information Centre). Healthcare Workers of the Slovak Republic in 2019; NCZI National Health Information Centre: Bratislava, Slovakia, 2021. Available online: https://www.nczisk.sk/aktuality/Pages/Pracovnici-v-zdravotnictve-Slovenskej-republiky-v-roku-2019.aspx (accessed on 20 November 2021).
- Fakonti, G.; Kyprianidou, M.; Toumbis, G.; Giannakou, K. Attitudes and Acceptance of COVID-19 Vaccination Among Nurses and Midwives in Cyprus: A Cross-Sectional Survey. Front. Public Health 2021, 9, 656138. [Google Scholar] [CrossRef] [PubMed]
- Di Gennaro, F.; Murri, R.; Segala, F.V.; Cerruti, L.; Abdulle, A.; Saracino, A.; Bavaro, D.F.; Fantoni, M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses 2021, 13, 371. [Google Scholar] [CrossRef] [PubMed]
- Colbert, G.B.; Venegas-Vera, A.V.; Lerma, E.V. Utility of telemedicine in the COVID-19 era. Rev. Cardiovasc. Med. 2020, 21, 583–587. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N.; Perrini, P. Will COVID-19 change neurosurgical clinical practice? Br. J. Neurosurg. 2020, 1–2. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 1277) | Vaccinated (n = 1076) | Unvaccinated (n = 201) | p Value | |
|---|---|---|---|---|
| Age (years; average ± SD) | 48.3 ± 12.6 | 48.7 ± 12.6 | 46.3 ± 12.2 | 0.014 * |
| Job duration (years; average ± SD) | 21.1 ± 15.1 | 21.9 ± 15.0 | 17.1 ± 14.8 | <0.001 * |
| Level of fear of COVID-19 (average ± SD) | 5.7 ± 2.7 | 6.1 ± 2.7 | 3.7 ± 2.4 | <0.001 * |
| Male N (%) Female N (%) | 280 997 | 249 (88.9) 827 (82.9) | 31 (11.1) 170 (17.1) | 0.016 ** 0.016 ** |
| Physicians N (%) Non-physician HCWs N (%) Non-HCWs N (%) | 582 542 153 | 542 (93.1) 417 (76.9) 117 (76.5) | 40 (6.9) 125 (23.1) 36 (23.5) | <0.001 ** <0.001 ** 0.005 ** |
| Hospitals N (%) Outpatient healthcare clinic N (%) | 745 532 | 592 (79.5) 484 (91.0) | 153 (20.5) 48 (9.0) | <0.001 ** <0.001 ** |
| History of COVID-19 N (%) | 354 | 250 (70.6) | 104 (29.4) | <0.001 ** |
| Influenza vaccinated at any time in the past N (%) Influenza vaccinated last season N (%) | 477 283 | 449 (94.1) 274 (96.8) | 28 (5.9) 9 (3.2) | <0.001 ** <0.001 ** |
| Motives | Physicians N = 542 | Physicians N = 542 | Non-Physician HCWs N = 417 | Hospitals N = 592 | History of COVID-19 N =250 |
|---|---|---|---|---|---|
| Non-Physician HCWs N = 417 | Non-HCWs N = 117 | Non-HCWs N = 117 | Outpatient HC N =484 | No history of COVID-19 N = 826 | |
| Concerns about COVID-19 itself | 380 (70.1%) * | 380 (70.1%) * | 233 (55.9%) | 346 (58.5%) * | 137 (54.8%) * |
| 233 (55.9%) | 70 (59.8%) | 70 (59.8%) | 337 (69.6%) | 546 (66.1%) | |
| An effort to prevent the spread of COVID-19 during the performance of my profession | 474 (87.5%) | 474 (87.5%) * | 347 (83.2%) | 492 (83.1%) | 206 (82.4%) |
| 347 (83.2%) | 91 (77.8%) | 91 (77.8%) | 420 (86.8%) | 706 (85.5%) | |
| An effort to protect family members | 393 (72.5%) | 393 (72.5%) | 287 (68.8%) | 404 (68.2%) * | 167 (66.8%) |
| 287 (68.8%) | 81 (69.2%) | 81 (69.2%) | 357 (73.8%) | 594 (71.9%) | |
| Being exempted from restrictive anti-pandemic measures after vaccination | 160 (29.5%) | 160 (29.5%) | 126 (30.2%) | 174 (29.4%) | 82 (32.8%) |
| 126 (30.2%) | 29 (24.8%) | 29 (24.8%) | 141 (29.1%) | 233 (28.2%) | |
| Others | 37 (6.8%) | 37 (6.8%) | 34 (8.1%) | 40 (6.8%) | 18 (7.2%) |
| 34 (8.1%) | 7 (5.9%) | 7 (5.9%) | 38 (7.9%) | 60 (7.3%) |
| Reasons | Physicians N = 40 | Physicians N = 40 | Non-Physician HCWs N =125 | Hospitals N = 153 | History of COVID-19 N = 104 |
|---|---|---|---|---|---|
| Non-Physician HCWs N = 125 | Non-HCWs N = 36 | Non-HCWs N = 36 | Outpatient HC N = 48 | No History of COVID-19 N = 97 | |
| I am not afraid of COVID-19, its course and consequences | 5 (12.5%) | 5 (12.5%) | 15 (12.0%) | 15 (9.8%) | 10 (9.6%) |
| 15 (12.0%) | 3 (8.3%) | 3 (8.3%) | 5 (10.4%) | 13 (13.4%) | |
| I do not find getting infected with COVID-19 likely | 0 (0.0%) | 0 (0.0%) | 9 (7.2%) | 8 (5.2%) | 2 (1.9%) |
| 9 (7.2%) | 0 (0.0%) | 0 (0.0%) | 1 (2.1%) | 7 (7.2%) | |
| I do not trust the efficacy of vaccines against COVID-19 | 11 (27.5%) * | 11 (27.5%) | 58 (46.4%) | 68 (44.4%) * | 34 (32.7%) * |
| 58 (46.4%) | 13 (36.1%) | 13 (36.1%) | 7 (15.6%) | 48 (49.5%) | |
| I have concerns about the safety and side effects of vaccines against COVID-19 | 28 (70.0%) | 28 (70.0%) | 86 (68.8%) | 112 (73.2%) * | 66 (63.5%) |
| 86 (68.8%) | 28 (77.8%) | 28 (77.8%) | 25 (52.1%) | 71 (73.2%) | |
| I went through COVID-19 and assume lasting immunity against disease | 12 (30.0%) | 12 (30.0%) | 43 (34.4%) | 55 (35.9%) | 68 (65.4%) * |
| 43 (34.4%) | 14 (38.9%) | 14 (38.9%) | 14 (29.2%) | 1 (1.0%) | |
| I have contraindications of expect a complicated vaccination course in my case | 10 (25.0%) | 10 (25.0%) | 30 (24.0%) | 33 (21.6%) | 22 (21.2%) |
| 30 (24.0%) | 8 (22.2%) | 8 (22.2%) | 15 (31.3%) | 26 (26.8%) | |
| Others | 15 (37.5%) * | 15 (37.5%) * | 19 (15.2%) | 24 (15.7%) * | 20 (19.2%) |
| 19 (15.2%) | 6 (16.7%) | 6 (16.7%) | 16 (33.3%) | 20 (20.7%) |
| COVID-19 Vaccination | Occupation | |||||
|---|---|---|---|---|---|---|
| Compulsory Vaccination | Vaccinated N = 1076 | Unvaccinated N = 201 | p Value | Physicians N = 582 | Non-Physician HCWs N = 542 | p Value |
| Only HCWs | 658 (61.2%) | 5 (2.5%) | <0.001 * | 378 (64.9%) | 213 (39.3%) | <0.001 * |
| Selected population | 644 (59.9%) | 4 (1.9%) | <0.001 * | 377 (64.7%) | 204 (37.6%) | <0.001 * |
| Whole population | 432 (40.2%) | 1 (0.5%) | <0.001 * | 241 (41.4%) | 148 (27.3%) | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ulbrichtova, R.; Svihrova, V.; Tatarkova, M.; Hudeckova, H.; Svihra, J. Acceptance of COVID-19 Vaccination among Healthcare and Non-Healthcare Workers of Hospitals and Outpatient Clinics in the Northern Region of Slovakia. Int. J. Environ. Res. Public Health 2021, 18, 12695. https://doi.org/10.3390/ijerph182312695
Ulbrichtova R, Svihrova V, Tatarkova M, Hudeckova H, Svihra J. Acceptance of COVID-19 Vaccination among Healthcare and Non-Healthcare Workers of Hospitals and Outpatient Clinics in the Northern Region of Slovakia. International Journal of Environmental Research and Public Health. 2021; 18(23):12695. https://doi.org/10.3390/ijerph182312695
Chicago/Turabian StyleUlbrichtova, Romana, Viera Svihrova, Maria Tatarkova, Henrieta Hudeckova, and Jan Svihra. 2021. "Acceptance of COVID-19 Vaccination among Healthcare and Non-Healthcare Workers of Hospitals and Outpatient Clinics in the Northern Region of Slovakia" International Journal of Environmental Research and Public Health 18, no. 23: 12695. https://doi.org/10.3390/ijerph182312695
APA StyleUlbrichtova, R., Svihrova, V., Tatarkova, M., Hudeckova, H., & Svihra, J. (2021). Acceptance of COVID-19 Vaccination among Healthcare and Non-Healthcare Workers of Hospitals and Outpatient Clinics in the Northern Region of Slovakia. International Journal of Environmental Research and Public Health, 18(23), 12695. https://doi.org/10.3390/ijerph182312695






