Evaluation of the Effectiveness of Outdoor Fitness Equipment Intervention in Achieving Fitness Goals for Seniors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Ethics Approval
2.3. Equipment and Interventions
2.3.1. Phase 1: Cardiorespiratory Endurance Training
Assessment
2.3.2. Phase 2: Muscle Strength, Balance, and Flexibility Training
Strength Training
Assessment
Flexibility Training
Assessment
Balance Training
Assessment
2.4. Statistical Analyses
3. Results
3.1. Participant Characteristics
3.2. Changes in Cardiorespiratory Endurance Training
3.3. Changes in Muscle Strength
3.4. Changes in Flexibility
3.5. Changes in Balance
4. Discussion
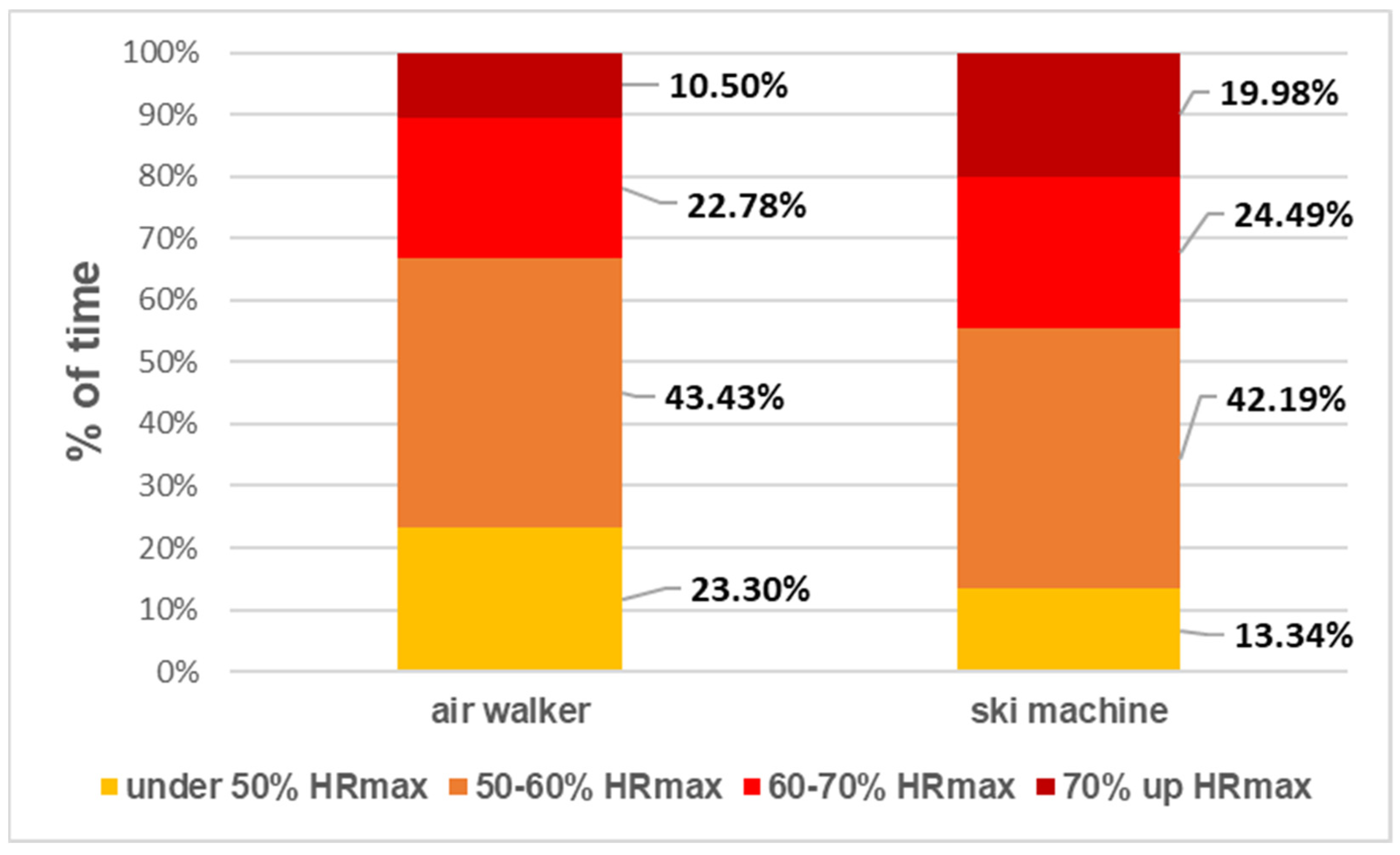
4.1. The Air Walker and Ski Machine OFE Training Achieves Moderate Cardiorespiratory Training
4.2. The Rowing Machine and Bonny Rider OFE Training Cannot Change Body Composition but Can Improve Both Upper and Lower Limb Muscle Strength
4.3. Arm Stretch and Shoulder Wheel OFE Improve Partial Shoulder Range of Motion
4.4. Single Leg Standing Training on the Waist Twister OFE Enhances Seniors’ Static Balance Tests
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beaglehole, R.; Bonita, R.; Horton, R.; Adams, C.; Alleyne, G.; Asaria, P.; Baugh, V.; Bekedam, H.; Billo, N.; Casswell, S. Priority actions for the non-communicable disease crisis. Lancet 2011, 377, 1438–1447. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1435. [Google Scholar] [CrossRef] [Green Version]
- Godbey, G.; Burnett-Wolle, S.; Chow, H.-w. New ideas for promoting physical activity among middle age and older adults. J. Phys. Educ. Recreat. Danc. 2007, 78, 1–58. [Google Scholar] [CrossRef]
- Godbey, G.; Mowen, A. The Benefits of Physical Activity Provided by Park and Recreation Services: The Scientific Evidence; National Recreation and Park Association: Ashburn, VA, USA, 2010. [Google Scholar]
- Marcus, B.H.; Forsyth, L.H. How are we doing with physical activity? Am. J. Health Promot. 1999, 14, 118–124. [Google Scholar] [CrossRef]
- Han, B.; Cohen, D.; McKenzie, T.L. Quantifying the contribution of neighborhood parks to physical activity. Prev. Med. 2013, 57, 483–487. [Google Scholar] [CrossRef] [Green Version]
- Berke, E.M.; Koepsell, T.D.; Moudon, A.V.; Hoskins, R.E.; Larson, E.B. Association of the built environment with physical activity and obesity in older persons. Am. J. Public Health 2007, 97, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, J.L.; Sallis, J.F.; Saelens, B.E.; Cain, K.L.; Black, J.B. The association of neighborhood design and recreational environments with physical activity. Am. J. Health Promot. 2005, 19, 304–309. [Google Scholar] [CrossRef]
- Cunningham, G.; Michael, Y.L. Concepts guiding the study of the impact of the built environment on physical activity for older adults: A review of the literature. Am. J. Health Promot. 2004, 18, 435–443. [Google Scholar] [CrossRef]
- Brownson, R.C.; Hoehner, C.M.; Day, K.; Forsyth, A.; Sallis, J.F. Measuring the built environment for physical activity: State of the science. Am. J. Prev. Med. 2009, 36, S99–S123. [Google Scholar] [CrossRef] [Green Version]
- Li, F.Z.; Harmer, P.A.; Cardinal, B.J.; Bosworth, M.; Acock, A.; Johnson-Shelton, D.; Moore, J.M. Built environment, adiposity, and physical activity in adults aged 50–75. Am. J. Prev. Med. 2008, 35, 38–46. [Google Scholar] [CrossRef] [Green Version]
- Sallis, J.F. Measuring physical activity environments: A brief history. Am. J. Prev. Med. 2009, 36, S86–S92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brug, J.; van der Ploeg, H.P.; Loyen, A.; Ahrens, W.; Allais, O.; Andersen, L.F.; Cardon, G.; Capranica, L.; Chastin, S.; De Bourdeaudhuij, I.; et al. Determinants of diet and physical activity (DEDIPAC): A summary of findings. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlin, A.; Perchoux, C.; Puggina, A.; Aleksovska, K.; Buck, C.; Burns, C.; Cardon, G.; Chantal, S.; Ciarapica, D.; Condello, G. A life course examination of the physical environmental determinants of physical activity behaviour: A “Determinants of Diet and Physical Activity”(DEDIPAC) umbrella systematic literature review. PLoS ONE 2017, 12, e0182083. [Google Scholar] [CrossRef]
- Cohen, D.A.; Marsh, T.; Williamson, S.; Golinelli, D.; McKenzie, T.L. Impact and cost-effectiveness of family Fitness Zones: A natural experiment in urban public parks. Health Place 2012, 18, 39–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Copeland, J.L.; Currie, C.; Walker, A.; Mason, E.; Willoughby, T.; Amson, A. Outdoor Fitness Equipment in Urban Parks: Public Use, Perceived Benefit and Suggested Enhancements; Alberta Centre for Child, Family and Community Research: Edmonton, AB, Canada, 2016. [Google Scholar]
- Cranney, L.; Phongsavan, P.; Kariuki, M.; Stride, V.; Scott, A.; Hua, M.; Bauman, A. Impact of an outdoor gym on park users’ physical activity: A natural experiment. Health Place 2016, 37, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Rodríguez, E.F.; Merino-Marban, R.; Romero-Ramos, O.; López-Fernández, I. A systematic review about the characteristics and patterns of use of outdoor gyms. Int. J. Environ. Res. Public Health 2020, 3, 698–707. [Google Scholar]
- Sami, M.; Smith, M.; Ogunseitan, O.A. Placement of Outdoor Exercise Equipment and Physical Activity: A Quasi-Experimental Study in Two Parks in Southern California. Int. J. Environ. Res. Public Health 2020, 17, 2605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, D.A.; Marsh, T.; Williamson, S.; Derose, K.; Martinez, H.; Setodji, C.; McKenzie, T.L. Parks and physical activity: Why are some parks used more than others? Prev. Med. 2010, 50, S9–S12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bettencourt, L.; Neves, R. Seniors’ playground and physical activity: Perceptions and practices. J. Aging Phys. Act. 2012, 20, S276. [Google Scholar]
- Greyling, G.A. The Usage of Outdoor Gyms in South Africa; Nelson Mandela Metropolitan University: Gqeberha, South Africa, 2016. [Google Scholar]
- Grigoletto, A.; Mauro, M.; Maietta Latessa, P.; Iannuzzi, V.; Gori, D.; Campa, F.; Greco, G.; Toselli, S. Impact of Different Types of Physical Activity in Green Urban Space on Adult Health and Behaviors: A Systematic Review. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 263–275. [Google Scholar] [CrossRef] [PubMed]
- The Trust for Public Land. Fitness Zone® Program: From Miami to Los Angeles, There Are 68 Fitness Zone Areas Already in Use and More on the Way. Available online: http://www.tpl.org/our-work/parks-people/fitness-zone-area (accessed on 10 August 2019).
- Scott, A.; Stride, V.; Neville, L.; Hua, M. Design and promotion of an outdoor gym for older adults: A collaborative project. Health Promot. J. Aust. 2014, 25, 212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, A. Playgrounds for Seniors in Europe, Asia and North America. Available online: http://www.athleticbusiness.com/articles/article.aspx?articleid=3609&zoneid=10 (accessed on 24 November 2016).
- Furber, S.; Pomroy, H.; Grego, S.; Tavener-Smith, K. People’s experiences of using outdoor gym equipment in parks. Health Promot. J. Aust. 2014, 25, 211. [Google Scholar] [CrossRef] [Green Version]
- Zhai, Y.; Li, D.; Wang, D.; Shi, C. Seniors’ Physical Activity in Neighborhood Parks and Park Design Characteristics. Front. Public Health 2020, 8, 322. [Google Scholar] [CrossRef]
- Mora, R.; Weisstaub, G.; Greene, M.; Herrmann, G. Outdoor gyms in Santiago: Urban distribution and effects on physical activity. Mot. Rev. Educ. Física 2017, 23. [Google Scholar] [CrossRef] [Green Version]
- Stride, V.; Cranney, L.; Scott, A.; Hua, M. Outdoor gyms and older adults–acceptability, enablers and barriers: A survey of park users. Health Promot. J. Aust. 2017, 28, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Chow, H.-w. Outdoor fitness equipment in parks: A qualitative study from older adults’ perceptions. BMC Public Health 2013, 13, 1216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Copeland, J.L.; Currie, C.; Walker, A.; Mason, E.; Willoughby, T.N.; Amson, A. Fitness equipment in public parks: Frequency of use and community perceptions in a small urban centre. J. Phys. Act. Health 2017, 14, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, P.; Camargo, D.; Quiroga, V. Physical activity in outdoor gym users in Bucaramanga, Colombia. Eur. J. Physiother. 2017, 19, 54–55. [Google Scholar] [CrossRef]
- Sibson, R.; Scherrer, P.; Ryan, M.M. ‘I think it adds value, but I don’t use it’: Use, perceptions and attitudes of outdoor exercise equipment in an urban public park. Ann. Leis. Res. 2018, 21, 58–73. [Google Scholar] [CrossRef]
- Chow, H.-w.; Wu, D.-R. Outdoor fitness equipment usage behaviors in natural settings. Int. J. Environ. Res. Public Health 2019, 16, 391. [Google Scholar] [CrossRef] [Green Version]
- Jansson, A.K.; Lubans, D.R.; Smith, J.J.; Duncan, M.J.; Haslam, R.; Plotnikoff, R.C. A systematic review of outdoor gym use: Current evidence and future directions. J. Sci. Med. Sport 2019, 22, 1335–1343. [Google Scholar] [CrossRef]
- Sharma, R.; Chaudhary, M. Perceptions of outdoor gymnasiums in National Capital Region, India: Creating active environments for health promotion. Health Promot. Int. 2021, 36, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Chow, H.-w. The current status and analysis of outdoor fitness equipment. Q. Chin. Phys. Educ. 2017, 31, 229–236. [Google Scholar]
- Chow, H.-w.; Ho, C.-h. Does the use of outdoor fitness equipment by older adults qualify as moderate to vigorous physical activity? PLoS ONE 2018, 13, e0196507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bettencourt, L.; Neves, R. Senior playgrounds in the promotion of physical activity among the elderly—Characteristics of use. J. Kairós Gerontol. 2016, 19, 59–72. [Google Scholar]
- Chow, H.-w.; Mowen, A.; Wu, G.-l. Who is using outdoor fitness equipment and how? The case of Xihu Park. Int. J. Environ. Res. Public Health 2017, 14, 448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-I.; Lee, D.H.; Hong, S.; Jo, S.-w.; Won, Y.-s.; Jeon, J.Y. Six weeks of combined aerobic and resistance exercise using outdoor exercise machines improves fitness, insulin resistance, and chemerin in the Korean elderly: A pilot randomized controlled trial. Arch. Gerontol. Geriatr. 2018, 75, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-C.; Yang, W.-W.; Fang, I.-Y.; Pan, H.L.-L.; Chen, W.-H.; Liu, C. Training Program With Outdoor Fitness Equipment in Parks Offers No Substantial Benefits for Functional Fitness in Active Seniors: A Randomized Controlled Trial. J. Aging Phys. Act. 2020, 1, 1–8. [Google Scholar] [CrossRef]
- Chow, H.-w.; Fang, I.-Y.; Ho, H.-H.; Hoc, C.-H. Use of outdoor fitness equipment in the park and functional fitness among Taiwanese older adults. In Proceedings of the 6th Biennial Congress of the International Society for Physical Activity and Health (ISPAH), Bangkok, Thailand, 16–19 November 2016. [Google Scholar]
- Kershaw, C.; Lim, J.; McIntosh, J.; Cornwall, J.; Marques, B. Developing Resilience, Independence and Well-Being in Older Adults through Interactive Outdoor Spaces; Victoria University of Wellington: Wellington, New Zealand, 2017. [Google Scholar]
- Warburton, D.E.; Jamnik, V.; Bredin, S.S.; Shephard, R.J.; Gledhill, N. The 2019 physical activity readiness questionnaire for everyone (PAR-Q+) and electronic physical activity readiness medical examination (ePARmed-X+). Health Fit. J. Can. 2018, 11, 80–83. [Google Scholar]
- Fletcher, G.F.; Balady, G.J.; Amsterdam, E.A.; Chaitman, B.; Eckel, R.; Fleg, J.; Froelicher, V.F.; Leon, A.S.; Piña, I.L.; Rodney, R. Exercise standards for testing and training: A statement for healthcare professionals from the American Heart Association. Circulation 2001, 104, 1694–1740. [Google Scholar] [CrossRef] [Green Version]
- Carter, J.B.; Banister, E.W.; Blaber, A.P. Effect of endurance exercise on autonomic control of heart rate. Sports Med. 2003, 33, 33–46. [Google Scholar] [CrossRef]
- Strath, S.J.; Swartz, A.M.; Bassett Jr, D.R.; O’Brien, W.L.; King, G.A.; Ainsworth, B.E. Evaluation of heart rate as a method for assessing moderate intensity physical activity. Med. Sci. Sports Exerc. 2000, 32, S465–S470. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A.V. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.J.; Rikli, R.E. Measuring functional fitness of older adults. J. Act. Aging 2002, 1, 24–30. [Google Scholar]
- Liu, C.j.; Latham, N.K. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst. Rev. 2009, 3, 1–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zatsiorsky, V.M.; Kraemer, W.J.; Fry, A.C. Science and Practice of Strength Training; Human Kinetics: Champaign, IL, USA, 2020. [Google Scholar]
- Massy-Westropp, N.; Rankin, W.; Ahern, M.; Krishnan, J.; Hearn, T.C. Measuring grip strength in normal adults: Reference ranges and a comparison of electronic and hydraulic instruments. J. Hand Surg. 2004, 29, 514–519. [Google Scholar] [CrossRef]
- Porto, J.M.; Nakaishi, A.P.M.; Cangussu-Oliveira, L.M.; Júnior, R.C.F.; Spilla, S.B.; de Abreu, D.C.C. Relationship between grip strength and global muscle strength in community-dwelling older people. Arch. Gerontol. Geriatr. 2019, 82, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, H.; Kasagi, F.; Yamada, M.; Fujita, S. Grip strength predicts cause-specific mortality in middle-aged and elderly persons. Am. J. Med. 2007, 120, 337–342. [Google Scholar] [CrossRef]
- Mijnarends, D.M.; Meijers, J.M.; Halfens, R.J.; ter Borg, S.; Luiking, Y.C.; Verlaan, S.; Schoberer, D.; Jentoft, A.J.C.; van Loon, L.J.; Schols, J.M. Validity and Reliability of Tools to Measure Muscle Mass, Strength, and Physical Performance in Community-Dwelling Older People: A Systematic Review. J. Am. Med. Dir. Assoc. 2013, 3, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Morrison, W. Understanding the Normal Shoulder Range of Motion. Available online: https://www.healthline.com/health/shoulder-range-of-motion#1 (accessed on 24 November 2019).
- Yim-Chiplis, P.K.; Talbot, L.A. Defining and measuring balance in adults. Biol. Res. Nurs. 2000, 1, 321–331. [Google Scholar] [CrossRef]
- Biodex Medical systems Inc. Biosway Portable Balance System: Operation Manual; Biodex Medical Systems Inc.: Upton, NY, USA, 2014. [Google Scholar]
- Michikawa, T.; Nishiwaki, Y.; Takebayashi, T.; Toyama, Y. One-leg standing test for elderly populations. J. Orthop. Sci. 2009, 14, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Nnodim, J.O.; Yung, R.L. Balance and its clinical assessment in older adults—A review. J. Geriatr. Med. Gerontol. 2015, 1, 3. [Google Scholar] [CrossRef] [PubMed]
- Verma, J. Sports Research with Analytical Solution Using SPSS; John Wiley & Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Huang, G.; Gibson, C.A.; Tran, Z.V.; Osness, W.H. Controlled endurance exercise training and VO2max changes in older adults: A meta-analysis. Prev. Cardiol. 2005, 8, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.P.; Teo, K.K.; Rangarajan, S.; Lopez-Jaramillo, P.; Avezum, A., Jr.; Orlandini, A.; Seron, P.; Ahmed, S.H.; Rosengren, A.; Kelishadi, R. Prognostic value of grip strength: Findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet 2015, 386, 266–273. [Google Scholar] [CrossRef]
- Swank, A.M.; Funk, D.C.; Urham, M.P.D.; Roberts, S. Adding weights to stretching exercise increases passive range of motion for healthy elderly. J. Strength Cond. Res. 2003, 17, 374–378. [Google Scholar]
- Hrysomallis, C. Balance ability and athletic performance. Sports Med. 2011, 41, 221–232. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.-G.; Cheon, E.-J.; Bai, D.-S.; Lee, Y.H.; Koo, B.-H. Stress and heart rate variability: A meta-analysis and review of the literature. Psychiatry Investig. 2018, 15, 235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madaniyazi, L.; Zhou, Y.; Li, S.; Williams, G.; Jaakkola, J.J.; Liang, X.; Liu, Y.; Wu, S.; Guo, Y. Outdoor temperature, heart rate and blood pressure in Chinese adults: Effect modification by individual characteristics. Sci. Rep. 2016, 6, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, T.; Lole, L.; Oorloff, A.; Aprile, K. “It’s about getting the best bang for your buck”: Exploring local councils’ perceptions about providing exercise infrastructure in public parks. Health Promot. J. Aust. 2021, 32, 483–491. [Google Scholar] [CrossRef] [PubMed]
| Fitness Goal | Intervention Frequency | OFE | Exercise Prescription | Duration | Research Device | Functional Fitness Test | |
|---|---|---|---|---|---|---|---|
| Cardiorespiratory endurance | 5 days/week |  Air walker | Operation tempo 60 bpm | 20 min |  POLAR H10 |  RPE scale | 2 min Step |
 Ski machine | 20 min | ||||||
| Muscle strength | 2 days/week |  Rowing machine | Week 1–6, 8 reps 3 sets | 10 min (1.5 min break between every set) |  Inbody 270 |  Handgrip dynamometer | 30 s Chair stand |
 Bonny rider | Week 7–12, 12 reps 3 sets | ||||||
| Flexibility | 2 days/week |  Arm stretch | Per stretching time for 30 s | 5 min |  Joint angle protractor | Back Scratch | |
 Shoulder wheel | Operation tempo 60 bpm | 5 min | |||||
| Balance | 2 days/week |  Waist twister | Operation tempo 60 bpm | 10 min |  Biosway | Single-leg stand, 8-Foot Up-and-Go | |
| Week 1–4, 2 feet for 10 min | |||||||
| Week 5–8, 2 feet for 10 min, 1 foot for 2 min | |||||||
| Week 6–12, 2 feet for 6 min, 1 foot for 4 min | |||||||
| Fitness Data | |||
|---|---|---|---|
| Test | Pre | Mid | Post |
| Cardiorespiratory endurance | |||
| 2 min step (times) | 96.60 ± 2.62 bc | 106.90 ± 3.08 ac | 115.70 ± 3.07 ab |
| Muscle strength | |||
| Skeletal muscle weight (kg) | 22.00 ± 0.81 | 21.35 ± 1.15 | 22.00 ± 0.86 |
| Body fat percentage (%) | 29.46 ± 1.28 | 29.49 ± 1.56 | 30.14 ± 1.16 |
| SMI (kg/m2) | 6.53 ± 0.21 | 6.62 ± 0.20 | 6.52 ± 0.22 |
| Handgrip strength (kg) | 24.52 ± 1.31 c | 24.82 ± 1.56 c | 27.97 ± 1.61 ab |
| 30 s chair stand (times) | 20.72 ± 1.11 c | 21.31 ± 1.04 c | 24.35 ± 1.17 ab |
| Flexibility | |||
| Back scratch (cm) | −3.13 ± 2.52 | −3.97 ± 2.81 | −1.56 ± 2.97 |
| Shoulder horizontal abduction (left) (deg) | 52.93 ± 2.44 | 57.45 ± 1.70 | 57.76 ± 2.70 |
| Shoulder horizontal abduction (right) (deg) | 54.17 ± 2.15 b | 63.24 ± 1.90 a | 58.66 ± 2.45 |
| Shoulder horizontal adduction (left) (deg) | 126.00 ± 4.05 | 133.55 ± 3.76 | 133.17 ± 4.59 |
| Shoulder horizontal adduction (right)(deg) | 127.66 ± 2.42 | 129.10 ± 2.79 | 125.48 ± 4.54 |
| Shoulder internal rotation (left)(deg) | 70.45 ± 3.27 | 67.59 ± 2.95 | 66.41 ± 3.70 |
| Shoulder internal rotation (right)(deg) | 68.72 ± 2.71 | 67.10 ± 1.98 | 62.86 ± 2.45 |
| Shoulder external rotation (left)(deg) | 90.41 ± 3.17 | 85.86 ± 2.91 | 86.07 ± 2.11 |
| Shoulder external rotation (right)(deg) | 95.86 ± 2.73 | 88.79 ± 2.56 | 89.10 ± 3.86 |
| Shoulder flexion (left)(deg) | 169.59 ± 4.47 | 169.97 ± 1.59 | 174.86 ± 3.86 |
| Shoulder flexion (right)(deg) | 169.52 ± 4.20 | 166.35 ± 1.49 c | 178.38 ± 2.05 b |
| Shoulder extension left hand (deg) | 61.28 ± 2.82 | 57.24 ± 2.55 | 56.03 ± 3.06 |
| Shoulder extension right hand (deg) | 53.72 ± 3.02 | 48.83 ± 2.08 | 52.97 ± 2.82 |
| Shoulder abduction left hand (deg) | 140.45 ± 4.41 | 154.55 ± 2.91 | 143.90 ± 6.64 |
| Shoulder abduction right hand (deg) | 148.03 ± 4.17 | 156.35 ± 3.30 | 151.17 ± 4.63 |
| Balance | |||
| 8-ft up and go (s) | 4.93 ± 0.11 | 4.92 ± 0.12 | 4.73 ± 0.10 |
| Single-leg stance (s) | 23.84 ± 1.69 bc | 27.79 ± 1.07 a | 27.80 ± 1.09 a |
| Eyes open firm surface | 0.78 ± 0.06 | 0.68 ± 0.04 | 0.73 ± 0.06 |
| Eyes closed firm surface | 0.79 ± 0.05 | 0.75 ± 0.07 | 0.75 ± 0.04 |
| Eyes open foam surface | 1.38 ± 0.07 b | 1.16 ± 0.06 a | 1.20 ± 0.06 |
| Eyes closed foam surface | 2.36 ± 0.15 | 2.35 ± 0.15 | 2.10 ± 0.13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chow, H.-W.; Chang, K.-T.; Fang, I.-Y. Evaluation of the Effectiveness of Outdoor Fitness Equipment Intervention in Achieving Fitness Goals for Seniors. Int. J. Environ. Res. Public Health 2021, 18, 12508. https://doi.org/10.3390/ijerph182312508
Chow H-W, Chang K-T, Fang I-Y. Evaluation of the Effectiveness of Outdoor Fitness Equipment Intervention in Achieving Fitness Goals for Seniors. International Journal of Environmental Research and Public Health. 2021; 18(23):12508. https://doi.org/10.3390/ijerph182312508
Chicago/Turabian StyleChow, Hsueh-Wen, Kun-Tang Chang, and I-Yao Fang. 2021. "Evaluation of the Effectiveness of Outdoor Fitness Equipment Intervention in Achieving Fitness Goals for Seniors" International Journal of Environmental Research and Public Health 18, no. 23: 12508. https://doi.org/10.3390/ijerph182312508
APA StyleChow, H.-W., Chang, K.-T., & Fang, I.-Y. (2021). Evaluation of the Effectiveness of Outdoor Fitness Equipment Intervention in Achieving Fitness Goals for Seniors. International Journal of Environmental Research and Public Health, 18(23), 12508. https://doi.org/10.3390/ijerph182312508






