Increased Work from Home and Low Back Pain among Japanese Desk Workers during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
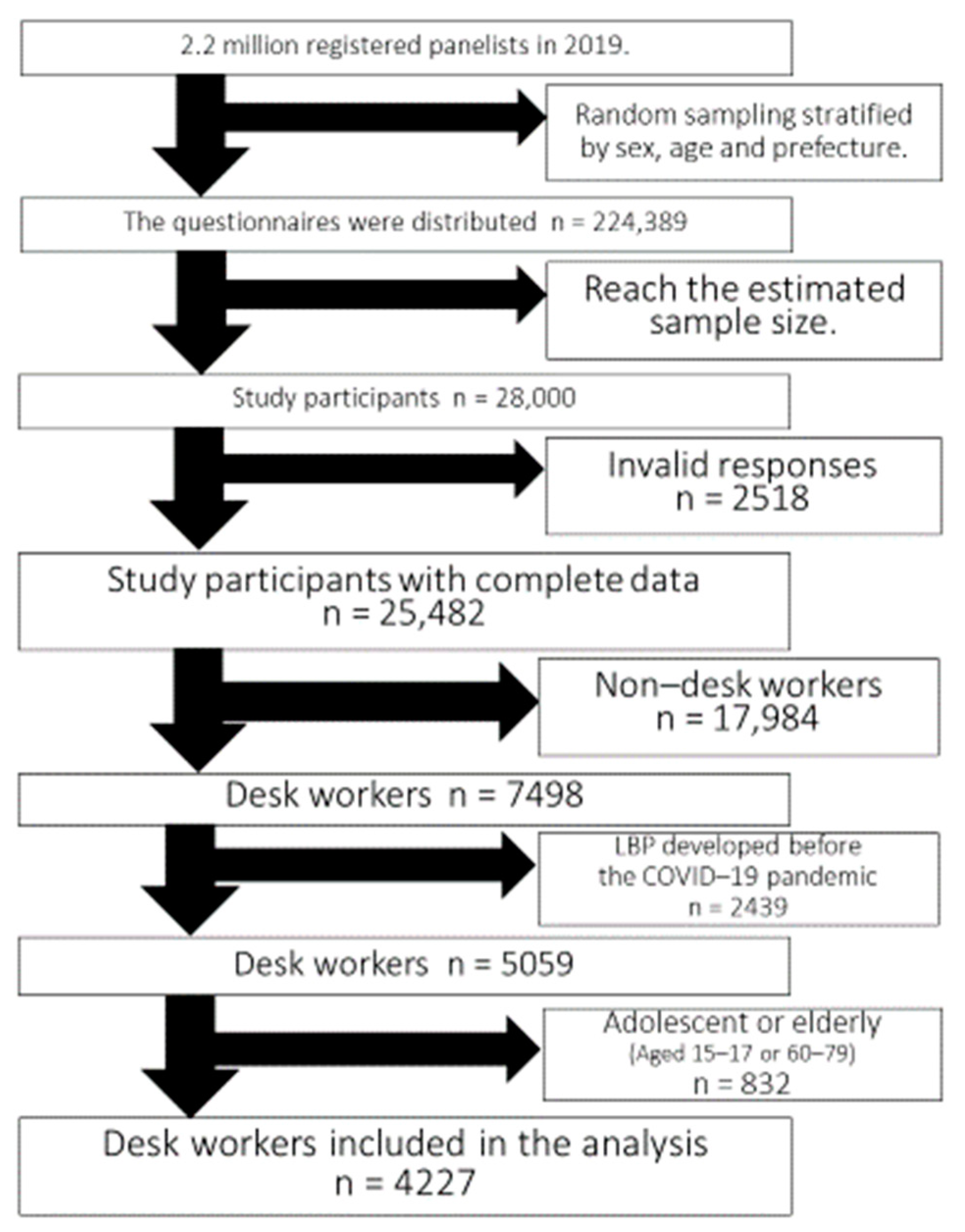
2.2. Study Population
2.3. Exposure Variables
2.4. Outcome Variable
2.5. Adjustment Variables
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Ministry of Health LaW. The Number of People Tested Positive for COVID-19 Number of PCR Tests (From 15 January 2020 to 6 April 2020); Ministry of Health LaW: Tokyo, Japan, 2020.
- Goto, M. Trends in Surveys about Home Teleworking during the COVID-19 Pandemic in Japan. J. Inst. Nucl. Saf. Syst. 2020, 27, 252–274. [Google Scholar]
- Moretti, A.; Menna, F.; Aulicino, M.; Paoletta, M.; Liguori, S.; Iolascon, G. Characterization of Home Working Population during COVID-19 Emergency: A Cross-Sectional Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6284. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Kim, H.J.; Jeong, H.; Kim, H.; Chang, B.S.; Lee, C.K.; Yeom, J.S. Longer sitting time and low physical activity are closely associated with chronic low back pain in population over 50 years of age: A cross-sectional study using the sixth Korea National Health and Nutrition Examination Survey. Spine J. Off. J. N. Am. Spine Soc. 2018, 18, 2051–2058. [Google Scholar] [CrossRef]
- Vassilaki, M.; Hurwitz, E.L. Insights in public health: Perspectives on pain in the low back and neck: Global burden, epidemiology, and management. Hawaii J. Med. Public Health J. Asia Pac. Med. Public Health 2014, 73, 122–126. [Google Scholar]
- Fujii, T.; Matsudaira, K. Prevalence of low back pain and factors associated with chronic disabling back pain in Japan. Eur. Spine J. 2013, 22, 432–438. [Google Scholar] [CrossRef] [Green Version]
- Yabe, Y.; Hagiwara, Y.; Sekiguchi, T.; Sugawara, Y.; Tsuchiya, M.; Koide, M.; Itaya, N.; Yoshida, S.; Sogi, Y.; Yano, T.; et al. Sleep Disturbance Is Associated with New Onset and Continuation of Lower Back Pain: A Longitudinal Study among Survivors of the Great East Japan Earthquake. Tohoku J. Exp. Med. 2018, 246, 9–14. [Google Scholar] [CrossRef] [Green Version]
- Deyo, R.A.; Weinstein, J.N. Low back pain. N. Engl. J. Med. 2001, 344, 363–370. [Google Scholar] [CrossRef]
- Yue, P.; Liu, F.; Li, L. Neck/shoulder pain and low back pain among school teachers in China, prevalence and risk factors. BMC Public Health 2012, 12, 789. [Google Scholar] [CrossRef] [Green Version]
- Berrens, R.P.; Bohara, A.K.; Jenkins-Smith, H.; Silva, C.; Weimer, D.L. The Advent of Internet Surveys for Political Research: A Comparison of Telephone and Internet Samples. Polit. Anal. 2017, 11, 1–22. [Google Scholar] [CrossRef]
- Tabuchi, T.; Gallus, S.; Shinozaki, T.; Nakaya, T.; Kunugita, N.; Colwell, B. Heat-not-burn tobacco product use in Japan: Its prevalence, predictors and perceived symptoms from exposure to secondhand heat-not-burn tobacco aerosol. Tob. Control 2018, 27, e25–e33. [Google Scholar] [CrossRef] [Green Version]
- Tabuchi, T.; Shinozaki, T.; Kunugita, N.; Nakamura, M.; Tsuji, I. Study Profile: The Japan “Society and New Tobacco” Internet Survey (JASTIS): A Longitudinal Internet Cohort Study of Heat-Not-Burn Tobacco Products, Electronic Cigarettes, and Conventional Tobacco Products in Japan. J. Epidemiol. 2019, 29, 444–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schonlau, M.; van Soest, A.; Kapteyn, A.; Couper, M. Selection Bias in Web Surveys and the Use of Propensity Scores. Sociol. Methods Res. 2009, 37, 291–318. [Google Scholar] [CrossRef] [Green Version]
- Kachi, Y.; Inoue, M.; Nishikitani, M.; Yano, E. Differences in self-rated health by employment contract and household structure among Japanese employees: A nationwide cross-sectional study. J. Occup. Health 2014, 56, 339–346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wada, K.; Arakida, M.; Watanabe, R.; Negishi, M.; Sato, J.; Tsutsumi, A. The economic impact of loss of performance due to absenteeism and presenteeism caused by depressive symptoms and comorbid health conditions among Japanese workers. Ind. Health 2013, 51, 482–489. [Google Scholar] [CrossRef] [Green Version]
- Sagat, P.; Bartik, P.; Prieto Gonzalez, P.; Tohanean, D.I.; Knjaz, D. Impact of COVID-19 Quarantine on Low Back Pain Intensity, Prevalence, and Associated Risk Factors among Adult Citizens Residing in Riyadh (Saudi Arabia): A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 7302. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Bakketeig, L.S.; Leboeuf-Yde, C.; Engberg, M.; Lauritzen, T. The association between physical workload and low back pain clouded by the “healthy worker” effect: Population-based cross-sectional and 5-year prospective questionnaire study. Spine 2001, 26, 1788–1792, discussion 1792–1783. [Google Scholar] [CrossRef]
- Di Fabio, R.P.; Mackey, G.; Holte, J.B. Physical therapy outcomes for patients receiving worker’s compensation following treatment for herniated lumbar disc and mechanical low back pain syndrome. J. Orthop. Sports Phys. Ther. 1996, 23, 180–187. [Google Scholar] [CrossRef] [Green Version]
- Mekonnen, T.H. Work-Related Factors Associated with Low Back Pain Among Nurse Professionals in East and West Wollega Zones, Western Ethiopia, 2017: A Cross-Sectional Study. Pain Ther. 2019, 8, 239–247. [Google Scholar] [CrossRef] [Green Version]
- Cheng, J.C.; Li-Tsang, C.W. A comparison of self-perceived physical and psycho-social worker profiles of people with direct work injury, chronic low back pain, and cumulative trauma. Work 2005, 25, 315–323. [Google Scholar]
- Pedersen, P.; Nielsen, C.V.; Jensen, O.K.; Jensen, C.; Labriola, M. Employment status five years after a randomised controlled trial comparing multidisciplinary and brief intervention in employees on sick leave due to low back pain. Scand. J. Public Health 2018, 46, 383–388. [Google Scholar] [CrossRef]
- Rohrlich, J.T.; Sadhu, A.; Sebastian, A.; Ahn, N.U. Risk factors for nonorganic low back pain in patients with worker’s compensation. Spine J. 2014, 14, 1166–1170. [Google Scholar] [CrossRef]
- Wippert, P.M.; Puschmann, A.K.; Driesslein, D.; Banzer, W.; Beck, H.; Schiltenwolf, M.; Schneider, C.; Mayer, F. Personalized Treatment Suggestions: The Validity and Applicability of the Risk-Prevention-Index Social in Low Back Pain Exercise Treatments. J. Clin. Med. 2020, 9, 1197. [Google Scholar] [CrossRef]
- Kesikburun, B.; Eksioglu, E.; Akdag, I.; Cakci, A. Low back pain in hemodialysis patients: Risk factors and its impact on health-related quality of life. Turk. J. Phys. Med. Rehabil. 2018, 64, 66–71. [Google Scholar] [CrossRef]
- Hakim, S.; Mohsen, A. Work-related and ergonomic risk factors associated with low back pain among bus drivers. J. Egypt. Public Health Assoc. 2017, 92, 195–201. [Google Scholar] [CrossRef]
- Tavares, A.I. Telework and health effects review. Int. J. Healthc. 2017, 3, 30. [Google Scholar] [CrossRef] [Green Version]
- Skov, T.; Borg, V.; Orhede, E. Psychosocial and physical risk factors for musculoskeletal disorders of the neck, shoulders, and lower back in salespeople. Occup. Environ. Med. 1996, 53, 351–356. [Google Scholar] [CrossRef] [Green Version]
- Sang, K.; Gyi, D.; Haslam, C. Musculoskeletal symptoms in pharmaceutical sales representatives. Occup. Med. 2010, 60, 108–114. [Google Scholar] [CrossRef] [Green Version]
- Celik, S.; Celik, K.; Dirimese, E.; Tasdemir, N.; Arik, T.; Buyukkara, I. Determination of pain in musculoskeletal system reported by office workers and the pain risk factors. Int. J. Occup. Med. Environ. Health 2018, 31, 91–111. [Google Scholar] [CrossRef]
- Al Amer, H.S. Low back pain prevalence and risk factors among health workers in Saudi Arabia: A systematic review and meta-analysis. J. Occup. Health 2020, 62, e12155. [Google Scholar] [CrossRef]
- Ikeda, T.; Sugiyama, K.; Aida, J.; Tsuboya, T.; Osaka, K. The Contextual Effect of Area-Level Unemployment Rate on Lower Back Pain: A Multilevel Analysis of Three Consecutive Surveys of 962,586 Workers in Japan. Int. J. Environ. Res. Public Health 2019, 16, 4016. [Google Scholar] [CrossRef] [Green Version]
- Nagata, T.; Mori, K.; Ohtani, M.; Nagata, M.; Kajiki, S.; Fujino, Y.; Matsuda, S.; Loeppke, R. Total Health-Related Costs Due to Absenteeism, Presenteeism, and Medical and Pharmaceutical Expenses in Japanese Employers. J. Occup. Environ. Med. 2018, 60, e273–e280. [Google Scholar] [CrossRef]
- Ye, S.; Jing, Q.; Wei, C.; Lu, J. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: A cross-sectional study. BMJ Open 2017, 7, e014914. [Google Scholar] [CrossRef] [Green Version]
- Irmak, A.; Bumin, G.; Irmak, R. The effects of exercise reminder software program on office workers’ perceived pain level, work performance and quality of life. Work 2012, 41 (Suppl. 1), 5692–5695. [Google Scholar] [CrossRef] [Green Version]
- Sitthipornvorakul, E.; Janwantanakul, P.; Lohsoonthorn, V. The effect of daily walking steps on preventing neck and low back pain in sedentary workers: A 1-year prospective cohort study. Eur. Spine J. 2015, 24, 417–424. [Google Scholar] [CrossRef]
- Kayihan, G. Relationship between daily physical activity level and low back pain in young, female desk-job workers. Int. J. Occup. Med. Environ. Health 2014, 27, 863–870. [Google Scholar] [CrossRef]
- Trajkovic, N.; Sporis, G.; Kristicevic, T.; Bogataj, S. Effects of Small-Sided Recreational Volleyball on Health Markers and Physical Fitness in Middle-Aged Men. Int. J. Environ. Res. Public Health 2020, 17, 3021. [Google Scholar] [CrossRef]
- van den Berg, R.; Jongbloed, E.M.; de Schepper, E.I.T.; Bierma-Zeinstra, S.M.A.; Koes, B.W.; Luijsterburg, P.A.J. The association between pro-inflammatory biomarkers and nonspecific low back pain: A systematic review. Spine J. 2018, 18, 2140–2151. [Google Scholar] [CrossRef]
- Daoust, R.; Sirois, M.J.; Lee, J.S.; Perry, J.J.; Griffith, L.E.; Worster, A.; Lang, E.; Paquet, J.; Chauny, J.M.; Emond, M. Painful Memories: Reliability of Pain Intensity Recall at 3 Months in Senior Patients. Pain Res. Manag. 2017, 2017, 5983721. [Google Scholar] [CrossRef] [Green Version]
| Total 1 | LBP− 2 | LBP+ 2 | p Value | ||
|---|---|---|---|---|---|
| (n = 4227) | (n = 4055 [95.9%]) | (n = 172 [4.1%]) | |||
| Working from home has increased | Yes | 1323 (31.3) | 1240 (93.7) | 83 (6.3) | <0.001 |
| No | 2904 (68.7) | 2815 (96.9) | 89 (3.1) | ||
| Age (years) | 18–29 | 742 (17.5) | 713 (96.1) | 29 (3.9) | 0.221 |
| 30–44 | 1681 (39.8) | 1602 (95.3) | 79 (4.7) | ||
| 45–59 | 1804 (42.7) | 1740 (96.5) | 64 (3.5) | ||
| Sex | Female | 1668 (39.5) | 1602 (96.0) | 66 (4.0) | 0.766 |
| Male | 2559 (60.5) | 2453 (95.9) | 106 (4.1) | ||
| Overweight or obese 3 | Yes | 779 (18.4) | 745 (95.6) | 34 (4.4) | 0.644 |
| No | 3448 (81.6) | 3310 (96.0) | 138 (4.0) | ||
| Educational attainment | College or higher | 3385 (80.1) | 3241 (95.7) | 144 (4.3) | 0.222 |
| High school or lower | 842 (19.9) | 814 (96.7) | 28 (3.3) | ||
| Marital status | Never married | 1609 (38.1) | 1549 (96.3) | 60 (3.7) | 0.599 |
| Married | 2348 (55.5) | 2246 (95.7) | 102 (4.3) | ||
| Widowed or separated | 270 (6.4) | 260 (96.3) | 10 (3.7) | ||
| Have children | Yes | 1703 (40.3) | 1616 (94.9) | 87 (5.1) | 0.005 |
| No | 2524 (59.7) | 2439 (96.6) | 85 (3.4) | ||
| Outdoor exercise during the | Yes | 1735 (41.1) | 1645 (94.8) | 90 (5.2) | 0.002 |
| COVID-19 pandemic | No | 2492 (58.9) | 2410 (96.7) | 82 (3.3) | |
| Duration of the COVID-19 state of | Long | 2212 (52.3) | 2116 (95.7) | 96 (4.3) | 0.608 |
| emergency in Japan 4 | Medium | 651 (15.4) | 625 (96.0) | 26 (4.0) | |
| Short | 1364 (32.3) | 1314 (96.3) | 50 (3.7) | ||
| Employment status | Employer | 236 (5.6) | 221 (93.6) | 15 (6.4) | 0.173 |
| Self-employed | 251 (5.9) | 239 (95.2) | 12 (4.8) | ||
| Regular employee | 3071 (72.7) | 2947 (96.0) | 124 (4.0) | ||
| Non-regular employee | 669 (15.8) | 648 (96.9) | 21 (3.1) | ||
| Income level | Low | 805 (19.0) | 763 (94.8) | 42 (5.2) | 0.091 |
| Intermediate | 1201 (28.4) | 1150 (95.7) | 51 (4.2) | ||
| High | 1598 (37.8) | 1535 (96.1) | 63 (3.9) | ||
| Not answered | 623 (14.7) | 607 (97.4) | 16 (2.6) | ||
| Working time (hours per week) | <35 | 979 (23.2) | 922 (94.2) | 57 (5.8) | 0.002 |
| 35–39 | 633 (15.0) | 612 (96.7) | 21 (3.3) | ||
| 40–44 | 1431 (33.8) | 1391 (97.2) | 40 (2.8) | ||
| >45 | 1184 (28.0) | 1130 (95.4) | 54 (4.6) | ||
| Smoking status | Never | 2361 (55.9) | 2289 (97.0) | 72 (3.0) | <0.001 |
| Former | 900 (21.3) | 847 (94.1) | 53 (5.9) | ||
| Current | 966 (22.8) | 919 (95.1) | 47 (4.9) | ||
| Alcohol use | Never | 782 (18.5) | 754 (96.4) | 28 (3.6) | 0.697 |
| Former | 1338 (31.7) | 1280 (95.7) | 58 (4.3) | ||
| Current | 2107 (49.8) | 2021 (95.9) | 86 (4.1) | ||
| Comorbidities | Hypertension | 420 (9.9) | 391 (93.1) | 29 (6.9) | 0.002 |
| Diabetes | 150 (3.5) | 134 (89.3) | 16 (10.7) | <0.001 | |
| Asthma or COPD | 138 (3.3) | 121 (87.7) | 17 (12.3) | <0.001 | |
| Cardiovascular disease | 52 (1.2) | 42 (80.8) | 10 (19.2) | <0.001 | |
| Stroke | 31 (0.7) | 25 (80.7) | 6 (19.3) | <0.001 | |
| Cancer | 48 (1.1) | 38 (79.2) | 10 (20.8) | <0.001 | |
| Psychiatric disorders | 212 (5.0) | 187 (88.2) | 25 (11.8) | <0.001 |
| Model 1 | Model 2 | ||
|---|---|---|---|
| OR (95%CI) | OR (95%CI) | ||
| Working from home has increased | Yes | 2.12 (1.56–2.88) | 2.13 (1.52–2.97) |
| No | Ref. | Ref. | |
| Age (years) | 18–29 | 1.06 (0.68–1.66) | 1.04 (0.61–1.77) |
| 30–44 | 1.33 (0.95–1.86) | 1.28 (0.89–1.843) | |
| 45–59 | Ref. | Ref. | |
| Sex | Female | 1.00 (0.73–1.38) | 1.38 (0.95–2.01) |
| Male | Ref. | Ref. | |
| Overweight or obese 1 | Yes | 0.97 (0.64–1.47) | |
| No | Ref. | ||
| Educational attainment | College or higher | 1.23 (0.79–1.90) | |
| High school or lower | Ref. | ||
| Marital status | Never married | 0.95 (0.57–1.57) | |
| Married | Ref. | ||
| Widowed or separated | 0.78 (0.36–1.66) | ||
| Have children | Yes | 1.71 (1.10–2.66) | |
| No | Ref. | ||
| Outdoor exercise during the COVID-19 | Yes | 1.32 (0.95–1.82) | |
| pandemic | No | Ref. | |
| Duration of the COVID-19 state of | Long | 1.20 (0.82–1.74) | |
| emergency in Japan 2 | Medium | 1.15 (0.70–1.90) | |
| Short | Ref. | ||
| Employment status | Employer | 1.31 (0.71–2.40) | |
| Self-employed | 0.97 (0.50–1.88) | ||
| Regular employee | Ref. | ||
| Non-regular employee | 0.56 (0.32–0.98) | ||
| Income level | Low | 1.42 (0.89–2.25) | |
| Intermediate | Ref. | ||
| High | 0.75 (0.50–1.13) | ||
| Not answered | 0.70 (0.39–1.26) | ||
| Working time (hours per week) | <35 | 1.79 (1.04–3.08) | |
| 35–39 | Ref. | ||
| 40–44 | 0.82 (0.48–1.43) | ||
| >45 | 1.30 (0.76–2.20) | ||
| Smoking status | Never | Ref. | |
| Former | 1.72 (1.15–2.56) | ||
| Current | 1.46 (0.97–2.19) | ||
| Alcohol use | Never | Ref. | |
| Former | 0.97 (0.60–1.58) | ||
| Current | 0.95 (0.59–1.52) | ||
| Comorbidities | Hypertension | 1.43 (0.87–2.36) | |
| Diabetes | 1.45 (0.72–2.92) | ||
| Asthma or COPD | 1.26 (0.61–2.61) | ||
| Cardiovascular disease | 1.44 (0.45–4.58) | ||
| Stroke | 0.37 (0.08–1.72) | ||
| Cancer | 3.45 (1.25–9.50) | ||
| Psychiatric disorders | 2.33 (1.36–4.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minoura, A.; Ishimaru, T.; Kokaze, A.; Tabuchi, T. Increased Work from Home and Low Back Pain among Japanese Desk Workers during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 12363. https://doi.org/10.3390/ijerph182312363
Minoura A, Ishimaru T, Kokaze A, Tabuchi T. Increased Work from Home and Low Back Pain among Japanese Desk Workers during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(23):12363. https://doi.org/10.3390/ijerph182312363
Chicago/Turabian StyleMinoura, Akira, Tomohiro Ishimaru, Akatsuki Kokaze, and Takahiro Tabuchi. 2021. "Increased Work from Home and Low Back Pain among Japanese Desk Workers during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 23: 12363. https://doi.org/10.3390/ijerph182312363
APA StyleMinoura, A., Ishimaru, T., Kokaze, A., & Tabuchi, T. (2021). Increased Work from Home and Low Back Pain among Japanese Desk Workers during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(23), 12363. https://doi.org/10.3390/ijerph182312363





