Predictors of Adherence to Smoking Cessation Medications among Current and Ex-Smokers in Australia: Findings from a National Cross-Sectional Survey
Abstract
1. Background
2. Methods
2.1. Sampling and Recruitment
2.2. Measures
2.3. Outcome Variables
2.4. Data Analysis
2.5. Ethics Approval
3. Results
3.1. Socio-Demographic Characteristics of Participants
3.2. Psychosocial Characteristics of Participants
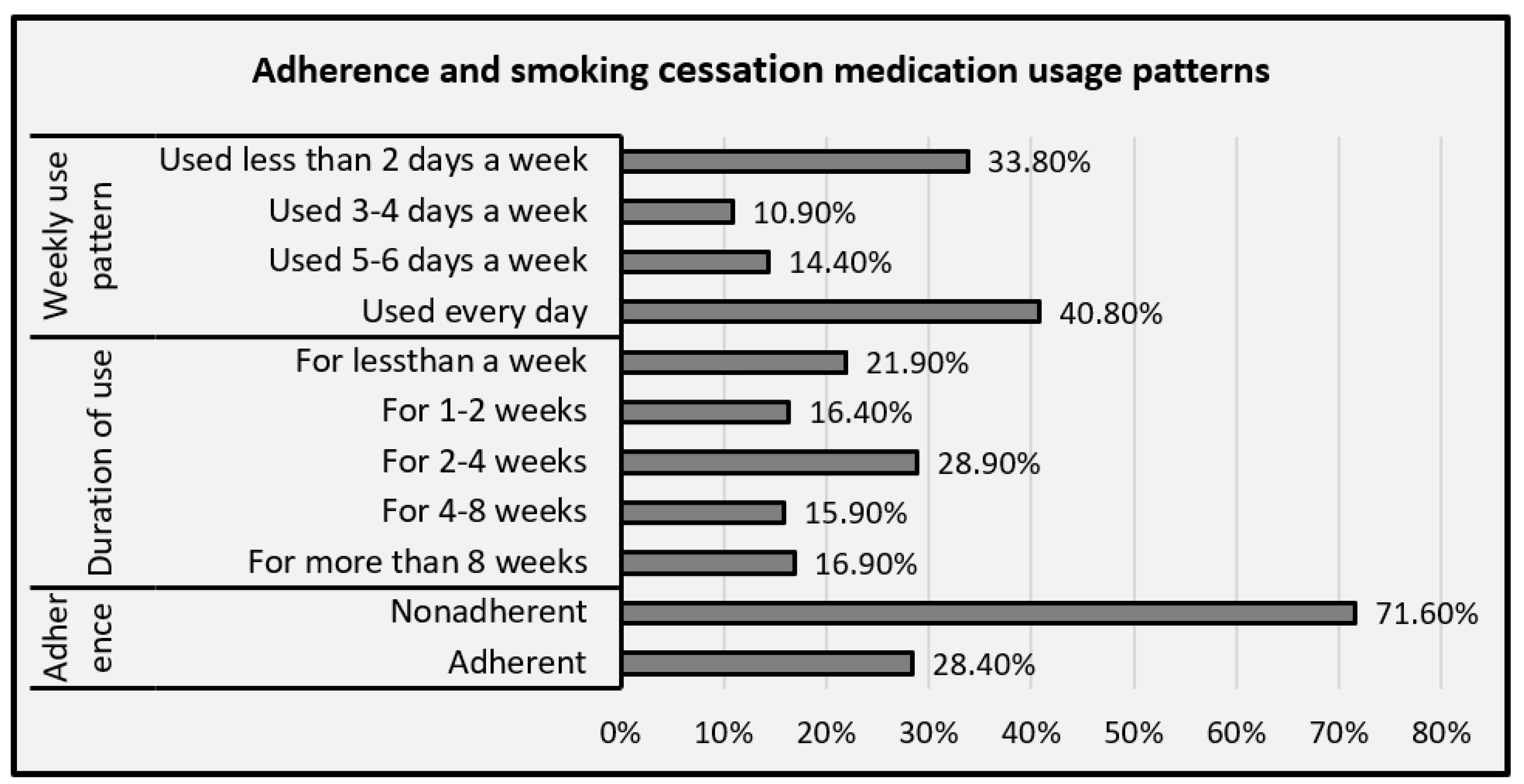
3.3. Adherence to and Pattern of Smoking Cessation Medications Use
3.4. Smoking, Quit Attempt, and Beliefs about Smoking Cessation Medications
3.5. Factors Associated with Adherence to Smoking Cessation Medications
4. Discussion
5. Strength and Limitations of the Study
6. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FTND | Fagerstrom Test for Nicotine Dependence |
| DASS | Depression, Anxiety, and Stress Scale |
| NRT | Nicotine replacement therapy |
| OSSS | Oslo Social Support Scale |
| SCM | Smoking cessation medication |
References
- Reitsma, M.B.; Kendrick, P.J.; Ababneh, E.; Abbafati, C.; Abbasi-Kangevari, M.; Abdoli, A.; Abedi, A.; Abhilash, E.S.; Abila, D.B.; Aboyans, V.; et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021, 397, 2337–2360. [Google Scholar] [CrossRef]
- Moore, D.; Aveyard, P.; Connock, M.; Wang, D.; Fry-Smith, A.; Barton, P. Effectiveness and safety of nicotine replacement therapy assisted reduction to stop smoking: Systematic review and meta-analysis. BMJ 2009, 338, b1024. [Google Scholar] [CrossRef]
- Siu, A.L. Behavioral and Pharmacotherapy Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Women: U.S. Preventive Services Task Force Recommendation Statement. Ann. Intern. Med. 2015, 163, 622–634. [Google Scholar] [CrossRef]
- Krist, A.H.; Davidson, K.W.; Mangione, C.M.; Barry, M.J.; Cabana, M.; Caughey, A.B.; Donahue, K.; Doubeni, C.A.; Epling, J.W.; Kubik, M.; et al. Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Persons: US Preventive Services Task Force Recommendation Statement. JAMA 2021, 325, 265–279. [Google Scholar]
- Hartmann-Boyce, J.; Chepkin, S.C.; Ye, W.; Bullen, C.; Lancaster, T. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst. Rev. 2018, 5, CD000146. [Google Scholar] [CrossRef] [PubMed]
- Hays, J.T.; Leischow, S.J.; Lawrence, D.; Lee, T.C. Adherence to treatment for tobacco dependence: Association with smoking abstinence and predictors of adherence. Nicotine Tob Res. 2010, 12, 574–581. [Google Scholar] [CrossRef]
- Mersha, A.G.; Eftekhari, P.; Bovill, M.; Tollosa, D.N.; Gould, G.S. Evaluating level of adherence to nicotine replacement therapy and its impact on smoking cessation: A systematic review and meta-analysis. Arch. Public Health 2021, 79, 26. [Google Scholar] [CrossRef]
- Leischow, S.J.; Muramoto, M.L.; Matthews, E.; Floden, L.L.; Grana, R.A. Adolescent Smoking Cessation With Bupropion: The Role of Adherence. Nicotine Tob. Res. 2016, 18, 1202–1205. [Google Scholar] [CrossRef]
- Catz, S.L.; Jack, L.M.; McClure, J.B.; Javitz, H.S.; Deprey, M.; Zbikowski, S.M.; McAfee, T.; Richards, J.; Swan, G.E. Adherence to varenicline in the COMPASS smoking cessation intervention trial. Nicotine Tob.Res. Off. J. Soc. Res. Nicotine Tob. 2011, 13, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Mersha, A.G.; Gould, G.S.; Bovill, M.; Eftekhari, P. Barriers and Facilitators of Adherence to Nicotine Replacement Therapy: A Systematic Review and Analysis Using the Capability, Opportunity, Motivation, and Behaviour (COM-B) Model. Int. J. Environ. Res. Public Health 2020, 17, 8895. [Google Scholar] [CrossRef]
- Pacek, L.R.; McClernon, F.J.; Bosworth, H.B. Adherence to Pharmacological Smoking Cessation Interventions: A Literature Review and Synthesis of Correlates and Barriers. Nicotine Tob. Res. 2017, 20, 1163–1172. [Google Scholar] [CrossRef]
- Burns, E.K.; Levinson, A.H. Discontinuation of nicotine replacement therapy among smoking-cessation attempters. Am. J. Prev. Med. 2008, 34, 212–215. [Google Scholar] [CrossRef]
- Hood, N.E.; Ferketich, A.K.; Paskett, E.D.; Wewers, M.E. Treatment adherence in a lay health adviser intervention to treat tobacco dependence. Health Educ. Res. 2013, 28, 72–82. [Google Scholar] [CrossRef]
- Berg, C.J.; Ahluwalia, J.S.; Cropsey, K. Predictors of adherence to behavioral counseling and medication among female prisoners enrolled in a smoking cessation trial. J. Correct. Health Care 2013, 19, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.; McCarthy, D.E.; Loh, W.Y.; Cook, J.W.; Piper, M.E.; Schlam, T.R.; Baker, T.B. Predictors of adherence to nicotine replacement therapy: Machine learning evidence that perceived need predicts medication use. Drug Alcohol Depend. 2019, 205, 107668. [Google Scholar] [CrossRef]
- Alterman, A.I.; Gariti, P.; Cook, T.G.; Cnaan, A. Nicodermal patch adherence and its correlates. Drug Alcohol Depend. 1999, 53, 159–165. [Google Scholar] [CrossRef]
- Vaz, L.R.; Aveyard, P.; Cooper, S.; Leonardi-Bee, J.; Coleman, T. The Association Between Treatment Adherence to Nicotine Patches and Smoking Cessation in Pregnancy: A Secondary Analysis of a Randomized Controlled Trial. Nicotine Tob. Res. 2016, 18, 1952–1959. [Google Scholar] [CrossRef]
- Ben Taleb, Z.; Ward, K.D.; Asfar, T.; Bahelah, R.; Maziak, W. Predictors of adherence to pharmacological and behavioral treatment in a cessation trial among smokers in Aleppo, Syria. Drug Alcohol Depend. 2015, 153, 167–172. [Google Scholar] [CrossRef][Green Version]
- Gong, M.; Dunbar, M.S.; Setodji, C.; Shadel, W.G. Zonnic®: A new player in an old field. Subst. Abuse Treat. Prev. Policy 2017, 12, 40. [Google Scholar] [CrossRef] [PubMed]
- Borland, R.; Li, L.; Driezen, P.; Wilson, N.; Hammond, D.; Thompson, M.E.; Mons, U.; Willemsen, M.C.; McNeill, A.; Thrasher, J.F. Cessation assistance reported by smokers in 15 countries participating in the International Tobacco Control (ITC) policy evaluation surveys. Addiction 2012, 107, 197–205. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare: Tobacco Smoking. Available online: https://www.aihw.gov.au/reports/australias-health/tobacco-smoking (accessed on 21 July 2021).
- Lam, T.H.; Abdullah, A.S.; Chan, S.S.; Hedley, A.J. Adherence to nicotine replacement therapy versus quitting smoking among Chinese smokers: A preliminary investigation. Psychopharmacology 2005, 177, 400–408. [Google Scholar] [CrossRef]
- Combs, P.; Cohen, W.; Siddiqi, U.A.; Jeevanandam, V. An international survey: Tobacco smoking cessation strategies within left ventricular assist device centers. Int. J. Artif. Organs 2021, 44, 110–114. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics (ABS) Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia. 2016. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012016?OpenDocument (accessed on 3 October 2021).
- Ghosh, A.; Charlton, K.E.; Batterham, M.J. Socioeconomic disadvantage and its implications for population health planning of obesity and overweight, using cross-sectional data from general practices from a regional catchment in Australia. BMJ Open 2016, 6, e010405. [Google Scholar] [CrossRef] [PubMed]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerström, K.O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Kocalevent, R.-D.; Berg, L.; Beutel, M.E.; Hinz, A.; Zenger, M.; Härter, M.; Nater, U.; Brähler, E. Social support in the general population: Standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 2018, 6, 31. [Google Scholar] [CrossRef] [PubMed]
- Ng, F.; Trauer, T.; Dodd, S.; Callaly, T.; Campbell, S.; Berk, M. The validity of the 21-item version of the Depression Anxiety Stress Scales as a routine clinical outcome measure. Acta Neuropsychiatr. 2007, 19, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Beaufort, I.N.; De Weert-Van Oene, G.H.; Buwalda, V.A.J.; de Leeuw, J.R.J.; Goudriaan, A.E. The Depression, Anxiety and Stress Scale (DASS-21) as a Screener for Depression in Substance Use Disorder Inpatients: A Pilot Study. Eur. Addict. Res. 2017, 23, 260–268. [Google Scholar] [CrossRef]
- Mersha, A.G.; Eftekhari, P.; Bovill, M.; Tollosa, D.N.; Gould, G.S. Evaluating level of adherence to nicotine replacement therapy and its impact on smoking cessation: A protocol for systematic review and meta-analysis. BMJ Open 2020, 10, e039775. [Google Scholar] [CrossRef]
- Lam, W.Y.; Fresco, P. Medication Adherence Measures: An Overview. Biomed. Res. Int. 2015, 2015, 217047. [Google Scholar] [CrossRef]
- Hollands, G.J.; Sutton, S.; McDermott, M.S.; Marteau, T.M.; Aveyard, P. Adherence to and consumption of nicotine replacement therapy and the relationship with abstinence within a smoking cessation trial in primary care. Nicotine Tob Res. 2013, 15, 1537–1544. [Google Scholar] [CrossRef]
- Lee, J.-Y.; Kim, M.; Jun, H.-J.; Kang, M.; Park, A.; Oh, D.; Choi, Y.H.; Hwang, J.H. Adherence to Varenicline and Abstinence Rates for Quitting Smoking in a Private Health Promotion Center-Based Smoking Cessation Clinic. Tuberc. Respir. Dis. 2012, 72, 426–432. [Google Scholar] [CrossRef][Green Version]
- Meijer, E.; Van der Kleij, R.M.J.J.; Chavannes, N.H. Facilitating smoking cessation in patients who smoke: A large-scale cross-sectional comparison of fourteen groups of healthcare providers. BMC Health Serv. Res. 2019, 19, 750. [Google Scholar] [CrossRef]
- McDaid, L.; Thomson, R.; Emery, J.; Coleman, T.; Cooper, S.; Phillips, L.; Naughton, F. Agreement and Disparities between Women and Stop-Smoking Specialists about How to Promote Adherence to Nicotine Replacement Therapy in Pregnancy. Int. J. Environ. Res. Public Health 2021, 18, 4673. [Google Scholar] [CrossRef] [PubMed]
- Gould, G.S.; Twyman, L.; Stevenson, L.; Gribbin, G.R.; Bonevski, B.; Palazzi, K.; Zeev, Y.B. What components of smoking cessation care during pregnancy are implemented by health providers? A systematic review and meta-analysis. BMJ Open 2019, 9, e026037. [Google Scholar] [CrossRef] [PubMed]
- Bowker, K.; Campbell, K.A.; Coleman, T.; Lewis, S.; Naughton, F.; Cooper, S. Understanding Pregnant Smokers’ Adherence to Nicotine Replacement Therapy During a Quit Attempt: A Qualitative Study. Nicotine Tob Res. 2016, 18, 906–912. [Google Scholar] [CrossRef] [PubMed]
- Harrison-Woolrych, M.; Ashton, J. Utilization of the smoking cessation medicine varenicline: An intensive post-marketing study in New Zealand. Pharmacoepidemiol. Drug Saf. 2010, 19, 949–953. [Google Scholar] [CrossRef] [PubMed]
- Kushnir, V.; Sproule, B.A.; Cunningham, J.A. Mailed distribution of free nicotine patches without behavioral support: Predictors of use and cessation. Addict. Behav. 2017, 67, 73–78. [Google Scholar] [CrossRef]
- Ferguson, S.G.; Gitchell, J.G.; Shiffman, S. Continuing to wear nicotine patches after smoking lapses promotes recovery of abstinence. Addiction 2012, 107, 1349–1353. [Google Scholar] [CrossRef]
- Velicer, W.F.; Diclemente, C.C.; Rossi, J.S.; Prochaska, J.O. Relapse situations and self-efficacy: An integrative model. Addict. Behav. 1990, 15, 271–283. [Google Scholar] [CrossRef]
- Gu, L.; Wu, S.; Zhao, S.; Zhou, H.; Zhang, S.; Gao, M.; Qu, Z.; Zhang, W.; Tian, D. Association of Social Support and Medication Adherence in Chinese Patients with Type 2 Diabetes Mellitus. Int. J. Environ. Res. Public Health 2017, 14, 1522. [Google Scholar] [CrossRef]
- Mondesir, F.L.; Carson, A.P.; Durant, R.W.; Lewis, M.W.; Safford, M.M.; Levitan, E.B. Association of functional and structural social support with medication adherence among individuals treated for coronary heart disease risk factors: Findings from the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. PLoS ONE 2018, 13, e0198578. [Google Scholar] [CrossRef]
- Burns, R.J.; Rothman, A.J.; Fu, S.S.; Lindgren, B.; Joseph, A.M. The relation between social support and smoking cessation: Revisiting an established measure to improve prediction. Ann. Behav. Med. 2014, 47, 369–375. [Google Scholar] [CrossRef]
- Vyavaharkar, M.; Moneyham, L.; Tavakoli, A.; Phillips, K.D.; Murdaugh, C.; Jackson, K.; Meding, G. Social support, coping, and medication adherence among HIV-positive women with depression living in rural areas of the southeastern United States. AIDS Patient Care STDS 2007, 21, 667–680. [Google Scholar] [CrossRef] [PubMed]
- Santomauro, D.F.; Mantilla Herrera, A.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Osibogun, O.; Bursac, Z.; Maziak, W. E-Cigarette Use and Regular Cigarette Smoking among Youth: Population Assessment of Tobacco and Health Study (2013–2016). Am. J. Prev. Med. 2020, 58, 657–665. [Google Scholar] [CrossRef]
- Ojo-Fati, O.; Thomas, J.L.; Vogel, R.I.; Ogedegbe, O.; Jean-Louis, G.; Okuyemi, K.S. Predictors of Adherence to Nicotine Replacement Therapy (Nicotine Patch) Among Homeless Persons Enrolled in a Randomized Controlled Trial Targeting Smoking Cessation. J. Fam. Med. 2016, 3, 1079. [Google Scholar]
- Chidambaram, A.G.; Dennis, R.A.; Biko, D.M.; Hook, M.; Allen, J.; Rapp, J.B. Clinical and radiological characteristics of e-cigarette or vaping product use associated lung injury. Emerg. Radiol. 2020, 27, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Handschin, J.; Hitsman, B.; Blazekovic, S.; Veluz-Wilkins, A.; Wileyto, E.P.; Leone, F.T.; Ashare, R.L.; Schnoll, R.A. Factors Associated with Adherence to Transdermal Nicotine Patches within a Smoking Cessation Effectiveness Trial. J. Smok. Cessat. 2018, 13, 33–43. [Google Scholar] [CrossRef]
- Zvolensky, M.J.; Bakhshaie, J.; Sheffer, C.; Perez, A.; Goodwin, R.D. Major depressive disorder and smoking relapse among adults in the United States: A 10-year, prospective investigation. Psychiatry Res. 2015, 226, 73–77. [Google Scholar] [CrossRef]
- McClave, A.K.; Dube, S.R.; Strine, T.W.; Kroenke, K.; Caraballo, R.S.; Mokdad, A.H. Associations between smoking cessation and anxiety and depression among U.S. adults. Addict. Behav. 2009, 34, 491–497. [Google Scholar] [CrossRef]
- OʼCleirigh, C.; Zvolensky, M.J.; Smits, J.A.J.; Labbe, A.K.; Coleman, J.N.; Wilner, J.G.; Stanton, A.M.; Gonzalez, A.; Garey, L.; Regenauer, K.S.; et al. Integrated Treatment for Smoking Cessation, Anxiety, and Depressed Mood in People Living With HIV: A Randomized Controlled Trial. J. Acquir. Immune Defic. Syndr. 2018, 79, 261–268. [Google Scholar] [CrossRef] [PubMed]
- AIHW. National Drug Strategy Household Survey 2019. Available online: https://www.aihw.gov.au/getmedia/7ebfd47a-9063-4ae0-b22f-1aeff56a30dc/aihw-phe-270-Chapter2-Tobacco.pdf.aspx (accessed on 20 August 2021).
- Australian Bureau of Statistics Census—2016 Report. Available online: https://www.abs.gov.au/census/find-census-data (accessed on 20 August 2021).
| Variables | Adherence n = 201 | p-Value | |
|---|---|---|---|
| No Frequency (%) | Yes Frequency (%) | ||
| Age | Median—47 years old | 0.002 * | |
| 18–55 | 100 (69.4%) | 26 (45.6%) | |
| ≥56 | 44 (30.6%) | 31 (54.4%) | |
| Gender | 0.552 | ||
| Female | 100 (69.4%) | 42 (73.7%) | |
| Male | 44 (30.6%) | 15 (26.3%) | |
| Education level | |||
| Completed primary or secondary school | 71 (49.3%) | 28 (49.1%) | 0.981 |
| Completed college and above | 73 (50.7%) | 29 (50.9%) | |
| Employment status | 0.037 * | ||
| Employed | 89 (61.8%) | 26 (45.6%) | |
| Unemployed | 55 (38.2%) | 31 (54.4%) | |
| Marital status | 0.066 | ||
| Married | 60 (41.7%) | 22 (38.7%) | |
| Never married | 48 (33.3%) | 12 (21%) | |
| Divorced/Widowed/Separated | 36 (25%) | 23 (40.3%) | |
| Remoteness | 0.005 * | ||
| Major cities of Australia | 116 (80.6%) | 35 (61.4%) | |
| Regional and remote Australia | 28 (19.4%) | 22 (38.6%) | |
| Socioeconomic disadvantage (SEIFA) | 0.808 | ||
| High | 76 (52.8%) | 29 (50.9%) | |
| Low | 68 (47.2%) | 28 (49.1) | |
| State of residence | 0.088 | ||
| New South Wales | 59 (50%) | 10 (17.5%) | |
| Victoria | 35 (24.3%) | 17 (29.8%) | |
| Queensland | 19 (13.2%) | 15 (26.3%) | |
| South Australia | 14 (9.7%) | 8 (14%) | |
| Western Australia | 17 (11.81%) | 7 (12.3%) | |
| Drinking alcohol | 0.015 * | ||
| No | 59 (41%) | 15 (26.3%) | |
| Yes | 85 (59%) | 42 (73.7%) | |
| Social support | |||
| Good social support (OSSS-3 score ≥ 9) | 55 (38.2%) | 43 (75.4%) | 0.001 * |
| Poor social support (OSSS-3 score ≤ 8) | 89 (61.8%) | 14 (24.6%) | |
| Stress | 0.004 * | ||
| No stress (DASS score ≤ 18) | 76 (53.1%) | 43 (75.4%) | |
| Had symptoms of stress(DASS score ≥ 19) | 67 (46.9%) | 14 (24.6%) | |
| Anxiety | 0.001 * | ||
| No anxiety (DASS score ≤ 9) | 64 (44.4%) | 49 (86%) | |
| Had symptoms of anxiety (DASS score ≥ 10) | 80 (55.6%) | 8 (14%) | |
| Depression | 0.001 * | ||
| No depression (DASS score ≤ 12) | 79 (54.9%) | 49 (86%) | |
| Had symptoms of depression (DASS score ≥ 13) | 65 (45.1%) | 8 (14%) | |
| Variables | Adherence n = 201 | p-Value | |
|---|---|---|---|
| No Frequency (%) | Yes Frequency (%) | ||
| Level of nicotine dependence | 0.002 * | ||
| Low dependence (FTND score ≤ 4) | 98 (68.1%) | 25 (43.9%) | |
| Moderate to high dependence (FTND score ≥ 5) | 46 (31.9%) | 32 (56.1%) | |
| Ever had quit attempt previously | 0.060 | ||
| Yes | 119 (82.6%) | 53 (93%) | |
| No | 25 (17.6%) | 4 (7%) | |
| Ever used SCMs during a previous quit attempt | 0.003 * | ||
| Yes | 83 (69.7%) | 48 (90.6%) | |
| No | 36 (30.3) | 5 (9.4%) | |
| Type of SCM in the current quit attempt | 0.027 * | ||
| NRT | 108 (75%) | 36 (63.2) | |
| Varenicline | 22 (15.3%) | 18 (31.5%) | |
| Bupropion | 14 (9.7%) | 3 (5.3%) | |
| Ever forget to take the SCMs | 0.016 * | ||
| Yes | 75 (52.1%) | 19 (33.3%) | |
| No | 69 (47.9%) | 38 (66.7%) | |
| Believe SCMs are safe | 0.107 | ||
| Yes | 100 (69.4%) | 46 (80.7%) | |
| No | 44 (30.6%) | 11 (19.3%) | |
| Believe SCMs are effective | 0.570 | ||
| Yes | 77 (53.5%) | 33 (57.9%) | |
| No | 67 (46.5%) | 24 (42.11%) | |
| Intentionally missed SCMs | 0.026 * | ||
| Yes | 65 (45.1%) | 16 (28.1) | |
| No | 79 (54.9%) | 41 (71.9%) | |
| Skip SCMs when feeling better | 0.063 | ||
| Yes | 84 (58.3%) | 25 (43.9%) | |
| No | 60 (41.7%) | 32 (56.1%) | |
| Relaps | 0.043 * | ||
| Yes | 99 (68.7%) | 30 (52.6%) | |
| No | 45 (31.3%) | 27 (47.4%) | |
| Experienced sleeping problems since quitting | 0.420 | ||
| Yes | 62 (43.1%) | 21 (36.8%) | |
| No | 82 (56.9%) | 36 (63.2%) | |
| Experienced eating problems since quitting | 0.640 | ||
| Yes | 68 (47.2%) | 29 (50.9%) | |
| No | 76 (52.8%) | 28 (49.1%) | |
| Do physical exercise during the quit attempt | 0.140 | ||
| Yes | 67 (46.5%) | 20 (35.1%) | |
| No | 77 (53.5%) | 37 (64.9%) | |
| Experienced craving since quitting | 0.086 | ||
| Yes | 114 (79.2%) | 51 (89.5%) | |
| No | 30 (20.8%) | 6 (10.5%) | |
| Others smoking inside living home | 0.625 | ||
| Yes | 61 (42.4%) | 22 (38.6%) | |
| No | 83 (57.6%) | 35 (61.4%) | |
| Variables | Adherence n = 201 | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| No Frequency (%) | Yes Frequency (%) | |||
| Age | ||||
| 18–55 | 100 (69.4%) | 26 (45.6%) | 1 | 1 |
| ≥56 | 44 (30.6%) | 31 (54.4%) | 2.71 (1.44–5.08) ** | 1.50 (0.47–4.78) |
| Employment status | ||||
| Employed | 89 (61.8%) | 26 (45.6%) | 0.52 (0.29–0.96) * | 0.92 (0.34–2.49) |
| Unemployed | 55 (38.2%) | 31 (54.4%) | 1 | 1 |
| Remoteness | ||||
| Major cities of Australia | 116 (80.6%) | 35 (61.4%) | 1 | 1 |
| Regional and remote Australia | 28 (19.4%) | 22 (38.6%) | 2.60 (1.33–5.11) ** | 1.11 (0.42–2.89) |
| Alcohol drinking | ||||
| No | 49 (34.1%) | 30 (52.6%) | 2.15 (1.15–4.02)* | 1.16 (0.45–2.98) |
| Yes | 95 (65.9%) | 27 (47.4%) | 1 | 1 |
| Level of social support | ||||
| Good social support | 55 (38.2%) | 43 (75.4%) | 4.97 (2.49–9.91) ** | 3.28 (2.30–6.27)* |
| Poor social support | 89 (61.8%) | 14 (24.6%) | 1 | 1 |
| Level of stress | ||||
| No symptom of stress | 76 (53.1%) | 43 (75.4%) | 2.70 (1.36–5.38) ** | 0.57 (0.17–1.90) |
| Symptom of stress | 67 (46.9%) | 14 (24.6%) | 1 | 1 |
| Level of anxiety | ||||
| No symptom of anxiety | 64 (44.4%) | 49 (86%) | 7.66 (3.38–17.32) ** | 4.41 (3.64–14.68)* |
| Symptom of anxiety | 80 (55.6%) | 8 (14%) | 1 | 1 |
| Level of depression | ||||
| No symptom of depression | 79 (54.9%) | 49 (86%) | 5.04 (2.23–11.39) ** | 1.80 (0.46–7.07) |
| Symptom of depression | 65 (45.1%) | 8 (14%) | 1 | 1 |
| Level of nicotine dependence | ||||
| Low dependence | 98 (68.1%) | 25 (43.9%) | 1 | 1 |
| Moderate to high dependence | 46 (31.9%) | 32 (56.1%) | 2.73 (1.45–5.11) ** | 3.53 (1.40–8.95) ** |
| Previous SCMs use | ||||
| Yes | 83 (69.7%) | 48 (90.6% | 4.16(1.53–11.32) ** | 3.87 (1.11–13.44) * |
| No | 36 (30.3) | 5 (9.4%) | 1 | 1 |
| Type of SCM used | ||||
| NRT | 108 (75%) | 36 (63.2) | ||
| Varenicline | 22 (15.3%) | 18 (31.5%) | 2.45 (1.18–5.08) * | 1.48 (0.53–4.13) |
| Bupropion | 14 (9.7%) | 3 (5.3%) | 0.64 (0.17–2.36) | 0.24 (0.39–1.49) |
| Ever forget to take the SCMs | ||||
| Yes | 75 (52.1%) | 19 (33.3%) | 1 | 1 |
| No | 69 (47.9%) | 38 (66.7%) | 2.17 (1.15–4.12)* | 1.67 (0.61–4.57) |
| Relapse | ||||
| Yes | 99 (68.7%) | 30 (52.6%) | 1 | 1 |
| No | 45 (31.3%) | 27 (47.4%) | 1.98 (1.05–3.71) * | 2.88 (1.21–6.88) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mersha, A.G.; Kennedy, M.; Eftekhari, P.; Gould, G.S. Predictors of Adherence to Smoking Cessation Medications among Current and Ex-Smokers in Australia: Findings from a National Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 12225. https://doi.org/10.3390/ijerph182212225
Mersha AG, Kennedy M, Eftekhari P, Gould GS. Predictors of Adherence to Smoking Cessation Medications among Current and Ex-Smokers in Australia: Findings from a National Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2021; 18(22):12225. https://doi.org/10.3390/ijerph182212225
Chicago/Turabian StyleMersha, Amanual Getnet, Michelle Kennedy, Parivash Eftekhari, and Gillian Sandra Gould. 2021. "Predictors of Adherence to Smoking Cessation Medications among Current and Ex-Smokers in Australia: Findings from a National Cross-Sectional Survey" International Journal of Environmental Research and Public Health 18, no. 22: 12225. https://doi.org/10.3390/ijerph182212225
APA StyleMersha, A. G., Kennedy, M., Eftekhari, P., & Gould, G. S. (2021). Predictors of Adherence to Smoking Cessation Medications among Current and Ex-Smokers in Australia: Findings from a National Cross-Sectional Survey. International Journal of Environmental Research and Public Health, 18(22), 12225. https://doi.org/10.3390/ijerph182212225







