The Impact of COVID-19 on Preschool-Aged Children’s Movement Behaviors in Hong Kong: A Longitudinal Analysis of Accelerometer-Measured Data
Abstract
:1. Introduction
2. Materials and Methods
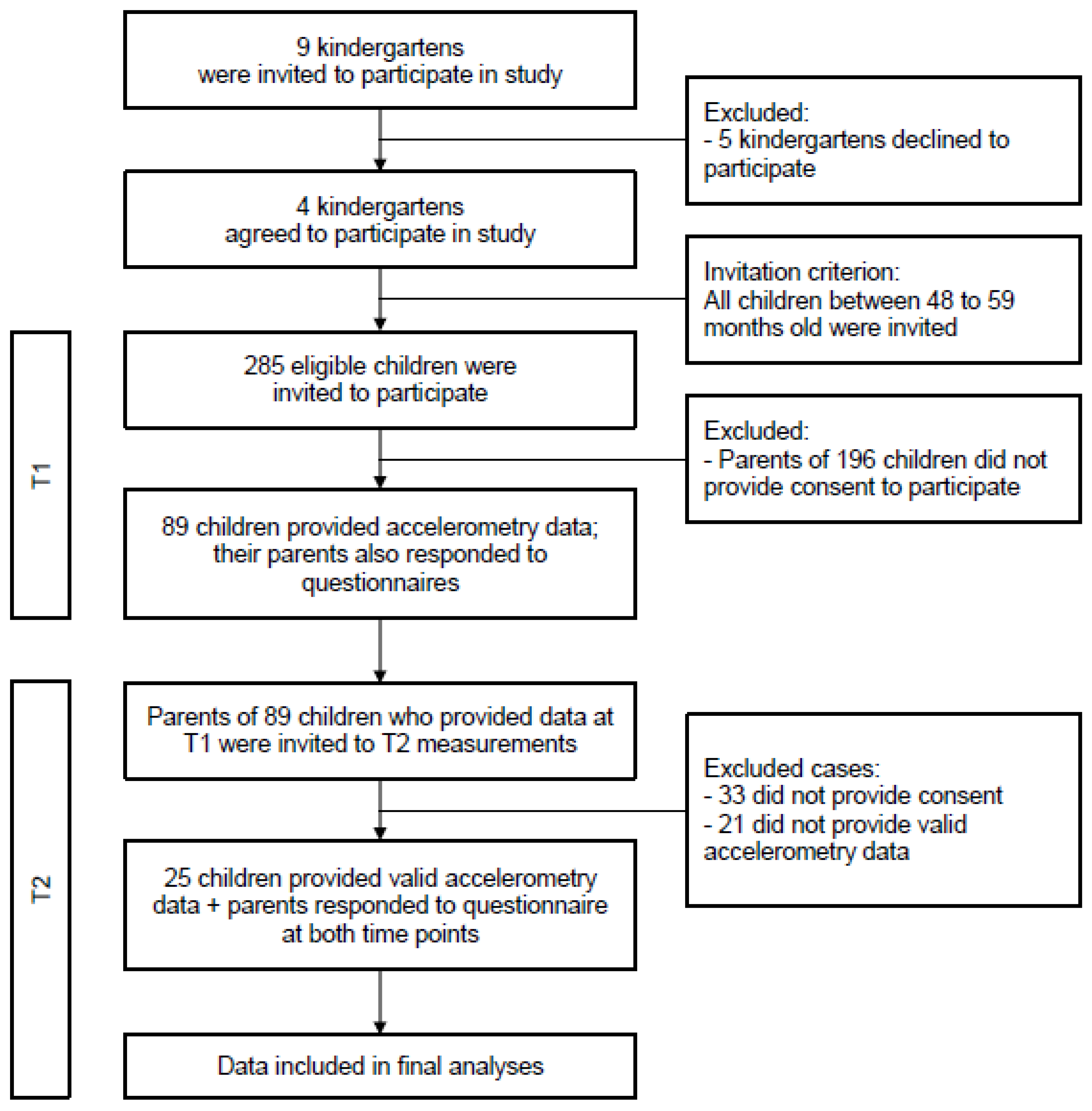
2.1. Participants and Procedures
2.2. Measures
2.3. Data Analyses
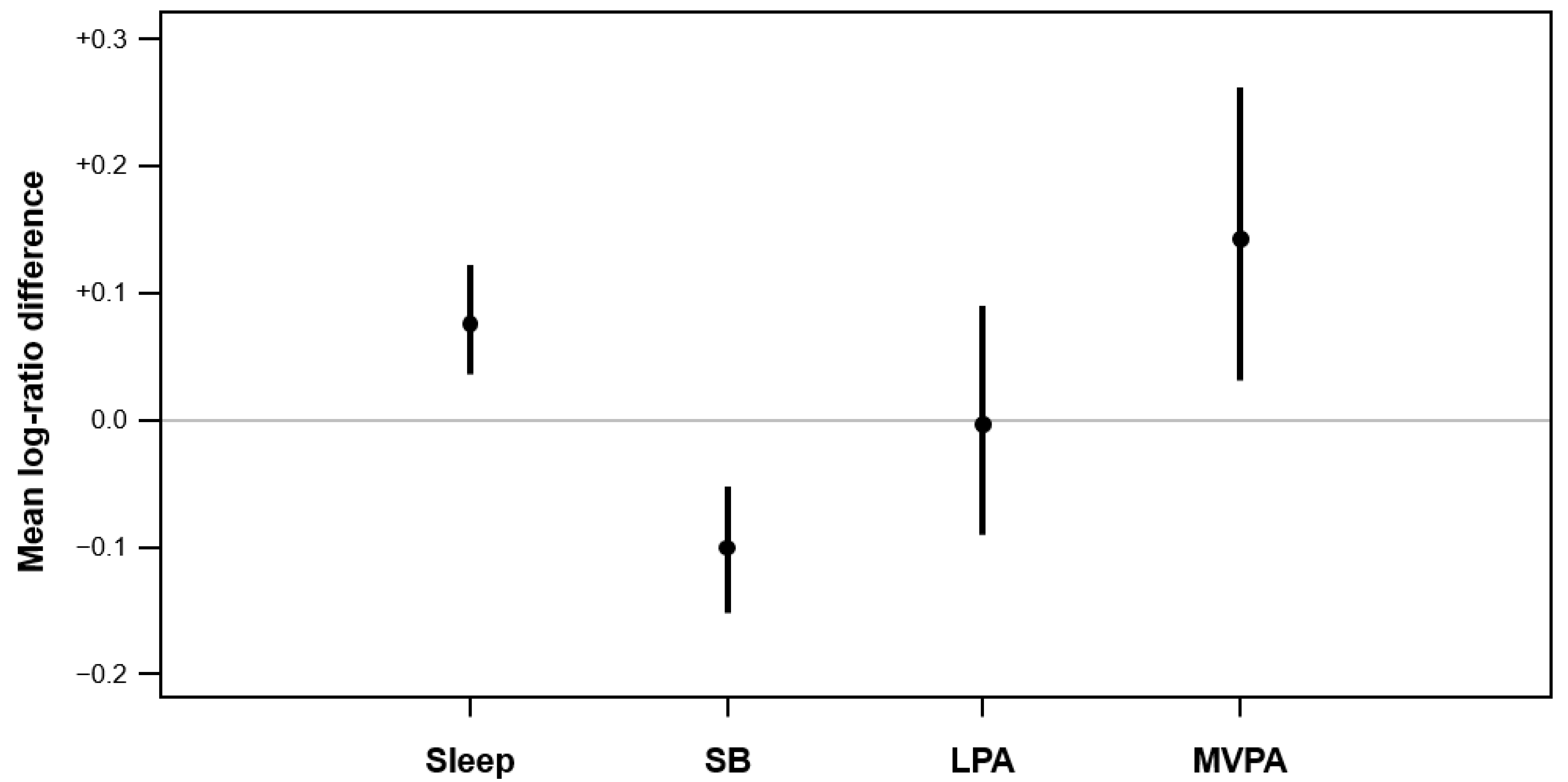
3. Results
Sensitivity Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yomoda, K.; Kurita, S. Influence of social distancing during the COVID-19 pandemic on physical activity in children: A scoping review of the literature. J. Exerc. Sci. Fit. 2021, 19, 195–203. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children under 5 Years of Age; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Vaughn, A.E.; Hales, D.; Ward, D.S. Measuring the physical activity practices used by parents of preschool children. Med. Sci. Sports Exerc. 2013, 45, 2369–2377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delisle Nyström, C.; Alexandrou, C.; Henström, M.; Nilsson, E.; Okely, A.D.; Wehbe El Masri, S.; Löf, M. International Study of Movement Behaviors in the Early Years (SUNRISE): Results from SUNRISE Sweden’s Pilot and COVID-19 Study. Int. J. Environ. Res. Public Health 2020, 17, 8491. [Google Scholar] [CrossRef] [PubMed]
- Cliff, D.P.; Reilly, J.J.; Okely, A.D. Methodological considerations in using accelerometers to assess habitual physical activity in children aged 0–5 years. J. Sci. Med. Sport 2009, 12, 557–567. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Barreira, T.V.; Schuna, J.M.J.; Mire, E.F.; Katzmarzyk, P.T. Fully automated waist-worn accelerometer algorithm for detecting children’s sleep-period time separate from 24-h physical activity or sedentary behaviors. Appl. Physiol. Nutr. Metab. 2014, 39, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Sousa-Sá, E.; Pereira, J.; Chaput, J.-P.; Okely, A.; Feng, X.; Santos, R. Correlates of nocturnal sleep duration, nocturnal sleep variability, and nocturnal sleep problems in toddlers: Results from the GET UP! Study. Sleep Med. 2019, 53, 124–132. [Google Scholar] [CrossRef]
- Pate, R.R.; Almeida, M.J.; McIver, K.L.; Pfeiffer, K.A.; Dowda, M. Validation and Calibration of an Accelerometer in Preschool Children. Obesity 2006, 14, 2000–2006. [Google Scholar] [CrossRef]
- Pate, R.R.; O’Neill, J.R.; Brown, W.H.; Pfeiffer, K.A. Prevalence of compliance with a new physical activity guideline for preschool-age children. Child. Obes. 2015, 11, 415–420. [Google Scholar] [CrossRef]
- Pedisic, Z.; Dumuid, D.; Olds, T.S. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: Definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiology 2017, 49, 252–269. [Google Scholar]
- Dumuid, D.; Pedisic, Z.; Palarea-Albaladejo, J.; Martin-Fernandez, J.A.; Hron, K.; Olds, T. Compositional data analysis in time-use epidemiology: What, why, how. Int. J. Environ. Res. Public Health 2020, 17, 2220. [Google Scholar] [CrossRef] [Green Version]
- Chong, K.H.; Parrish, A.M.; Cliff, D.P.; Dumuid, D.; Okely, A.D. Changes in 24-h movement behaviours during the transition from primary to secondary school among Australian children. Eur. J. Sport Sci. 2021, in press. [Google Scholar] [CrossRef]
- Martin-Fernandez, J.A.; Daunis-i-Estadella, J.; Mateu-Figueras, G. On the interpretation of differences between groups for compositional data. Sort 2015, 39, 231–252. [Google Scholar]
- Moore, S.A.; Faulkner, G.; Rhodes, R.E.; Brussoni, M.; Chulak-Bozzer, T.; Ferguson, L.J.; Mitra, R.; O’Reilly, N.; Spence, J.C.; Vanderloo, L.M.; et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 85. [Google Scholar] [CrossRef] [PubMed]
- Tulchin-Francis, K.; Stevens, W.; Gu, X.; Zhang, T.; Roberts, H.; Keller, J.; Dempsey, D.; Borchard, J.; Jeans, K.; VanPelt, J. The impact of the coronavirus disease 2019 pandemic on physical activity in U.S. children. J. Sport Health Sci. 2021, 10, 323–332. [Google Scholar] [CrossRef] [PubMed]
- López-Gil, J.F.; Tremblay, M.S.; Brazo-Sayavera, J. Changes in healthy behaviors and meeting 24-h movement guidelines in Spanish and Brazilian preschoolers, children and adolescents during the COVID-19 lockdown. Children 2021, 8, 83. [Google Scholar] [CrossRef]
- Cordovil, R.; Ribeiro, L.; Moreira, M.; Pombo, A.; Rodrigues, L.P.; Luz, C.; Veiga, G.; Lopes, F. Effects of the COVID-19 pandemic on preschool children and preschools in Portugal. J. Phys. Educ. Sport 2021, 21, 492–499. [Google Scholar]
- Clarke, J.; Kipping, R.; Chambers, S.; Willis, K.; Taylor, H.; Brophy, R.; Hannam, K.; Simpson, S.A.; Langford, R. Impact of COVID-19 restrictions on preschool children’s eating, activity and sleep behaviours: A qualitative study. BMJ Open 2021, 11, e051497. [Google Scholar] [CrossRef]
- Okely, A.D.; Kariippanon, K.E.; Guan, H.; Taylor, E.K.; Suesse, T.; Cross, P.L.; Chong, K.H.; Suherman, A.; Turab, A.; Staiano, A.E.; et al. Global effect of COVID-19 pandemic on physical activity, sedentary behaviour and sleep among 3- to 5-year-old children: A longitudinal study of 14 countries. BMC Public Health 2021, 21, 940. [Google Scholar] [CrossRef]
- O’Dwyer, M.V.; Fairclough, S.J.; Ridgers, N.D.; Knowles, Z.R.; Foweather, L.; Stratton, G. Effect of a school-based active play intervention on sedentary time and physical activity in preschool children. Health Educ. Res. 2013, 28, 931–942. [Google Scholar] [CrossRef] [Green Version]
- McGowan, A.L.; Ferguson, D.P.; Gerde, H.K.; Pfeiffer, K.A.; Pontifex, M.B. Preschoolers exhibit greater on-task behavior following physically active lessons on the approximate number system. Scand. J. Med. Sci. Sports 2020, 30, 1777–1786. [Google Scholar] [CrossRef]
- Zhang, Z.; Sousa-Sá, E.; Pereira, J.R.; Okely, A.D.; Feng, X.; Santos, R. Correlates of Sleep Duration in Early Childhood: A Systematic Review. Behav Sleep Med. 2020, 1–19. [Google Scholar] [CrossRef]
- Roy, M.; Haszard, J.J.; Savage, J.S.; Yolton, K.; Beebe, D.W.; Xu, Y.; Galland, B.; Paul, I.M.; Mindell, J.A.; Mihrshahi, S.; et al. Bedtime, body mass index and obesity risk in preschool-aged children. Pediatr. Obes. 2020, 15, e12650. [Google Scholar] [CrossRef] [PubMed]
- Janssen, X.; Martin, A.; Hughes, A.R.; Hill, C.M.; Kotronoulas, G.; Hesketh, K.R. Associations of screen time, sedentary time and physical activity with sleep in under 5s: A systematic review and meta-analysis. Sleep Med. Rev. 2020, 49, 101226. [Google Scholar] [CrossRef] [PubMed]
- Lau, E.Y.H.; Lee, K. Parents’ views on young children’s distance learning and screen time during COVID-19 class suspension in Hong Kong. Early Educ Dev. 2020, 32, 863–880. [Google Scholar] [CrossRef]
- Downing, K.L.; Hinkley, T.; Hesketh, K.D. Associations of parental rules and socioeconomic position with preschool children’s sedentary behaviour and screen time. J. Phys. Act. Health 2015, 12, 515–521. [Google Scholar] [CrossRef]
- Schmutz, E.A.; Haile, S.R.; Leeger-Aschmann, C.S.; Kakebeeke, T.H.; Zysset, A.E.; Messerli-Burgy, N.; Stulb, K.; Arhab, A.; Meyer, A.H.; Munsch, S.; et al. Physical activity and sedentary behavior in preschoolers: A longitudinal assessment of trajectories and determinants. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 35. [Google Scholar] [CrossRef] [Green Version]
- Hnatiuk, J.A.; Lamb, K.E.; Ridgers, N.D.; Salmon, J.; Hesketh, K.D. Changes in volume and bouts of physical activity and sedentary time across early childhood: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 42. [Google Scholar] [CrossRef]
- Guan, H.; Okely, A.D.; Aguilar-Farias, N.; del Pozo Cruz, B.; Draper, C.E.; El Hamdouchi, A.; Florindo, A.A.; Jáuregui, A.; Katzmarzyk, P.T.; Kontsevaya, A.; et al. Promoting healthy movement behaviours among children during the COVID-19 pandemic. Lancet Child. Adolesc. Health 2020, 4, 416–418. [Google Scholar] [CrossRef]
- Gassman-Pines, A.; Ananat, E.O.; Fitz-Henley, J. COVID-19 and parent-child psychological well-being. Pediatrics 2020, 146, e2020007294. [Google Scholar] [CrossRef]
| Variable | T1 | T2 |
|---|---|---|
| Accelerometry-measured variables—Compositional means (min/day) a | ||
| Sleep duration | 580 | 627 |
| Sedentary behavior | 663 | 601 |
| Light physical activity | 107 | 107 |
| MVPA | 90 | 105 |
| Sleep schedule | ||
| Bedtime | 22:50 (0:57) | 23:24 (1:19) |
| Wake-up time | 08:00 (0:34) | 09:19 (1:20) |
| Parent-reported measures | ||
| Sleep duration | 688 ± 70 | 652 ± 64 |
| Sedentary screen time | 78 ± 54 | 147 ± 95 |
| Total physical activity | 143 ± 71 | 82 ± 73 |
| MVPA | 36 ± 35 | 23 ± 26 |
| Time spent outdoor (weekdays) | 127 ± 92 | 55 ± 60 |
| Time spent outdoor (weekends) | 237 ± 144 | 127 ± 131 |
| Adherence to WHO guidelines (n and percentage) | ||
| Sleep | 4 (16%) | 10 (40%) |
| Sedentary screen time | 14 (56%) | 5 (20%) |
| Total physical activity | 19 (76%) | 23 (92%) |
| MVPA | 17 (68%) | 18 (72%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, J.Y.Y.; He, Q.; Chong, K.H.; Okely, A.D.; Chan, C.H.S.; Ha, A.S. The Impact of COVID-19 on Preschool-Aged Children’s Movement Behaviors in Hong Kong: A Longitudinal Analysis of Accelerometer-Measured Data. Int. J. Environ. Res. Public Health 2021, 18, 11907. https://doi.org/10.3390/ijerph182211907
Ng JYY, He Q, Chong KH, Okely AD, Chan CHS, Ha AS. The Impact of COVID-19 on Preschool-Aged Children’s Movement Behaviors in Hong Kong: A Longitudinal Analysis of Accelerometer-Measured Data. International Journal of Environmental Research and Public Health. 2021; 18(22):11907. https://doi.org/10.3390/ijerph182211907
Chicago/Turabian StyleNg, Johan Y. Y., Qing He, Kar Hau Chong, Anthony D. Okely, Cecilia H. S. Chan, and Amy S. Ha. 2021. "The Impact of COVID-19 on Preschool-Aged Children’s Movement Behaviors in Hong Kong: A Longitudinal Analysis of Accelerometer-Measured Data" International Journal of Environmental Research and Public Health 18, no. 22: 11907. https://doi.org/10.3390/ijerph182211907
APA StyleNg, J. Y. Y., He, Q., Chong, K. H., Okely, A. D., Chan, C. H. S., & Ha, A. S. (2021). The Impact of COVID-19 on Preschool-Aged Children’s Movement Behaviors in Hong Kong: A Longitudinal Analysis of Accelerometer-Measured Data. International Journal of Environmental Research and Public Health, 18(22), 11907. https://doi.org/10.3390/ijerph182211907





_Okely.png)

