Hypothermia Outcome Prediction after Extracorporeal Life Support for Hypothermic Cardiac Arrest Patients: Assessing the Performance of the HOPE Score in Case Reports from the Literature
Abstract
:1. Introduction
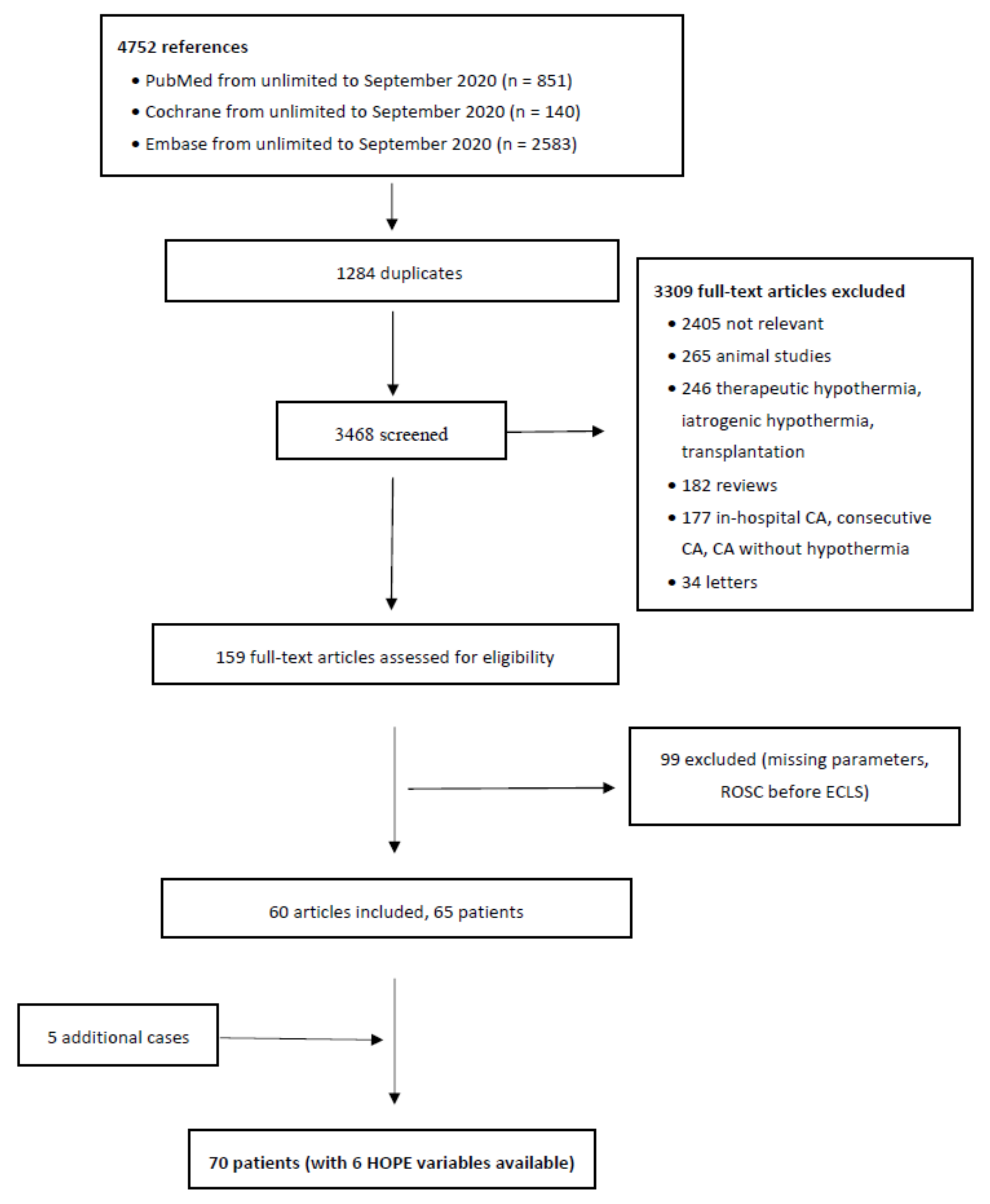
2. Methods
Statistical Analysis
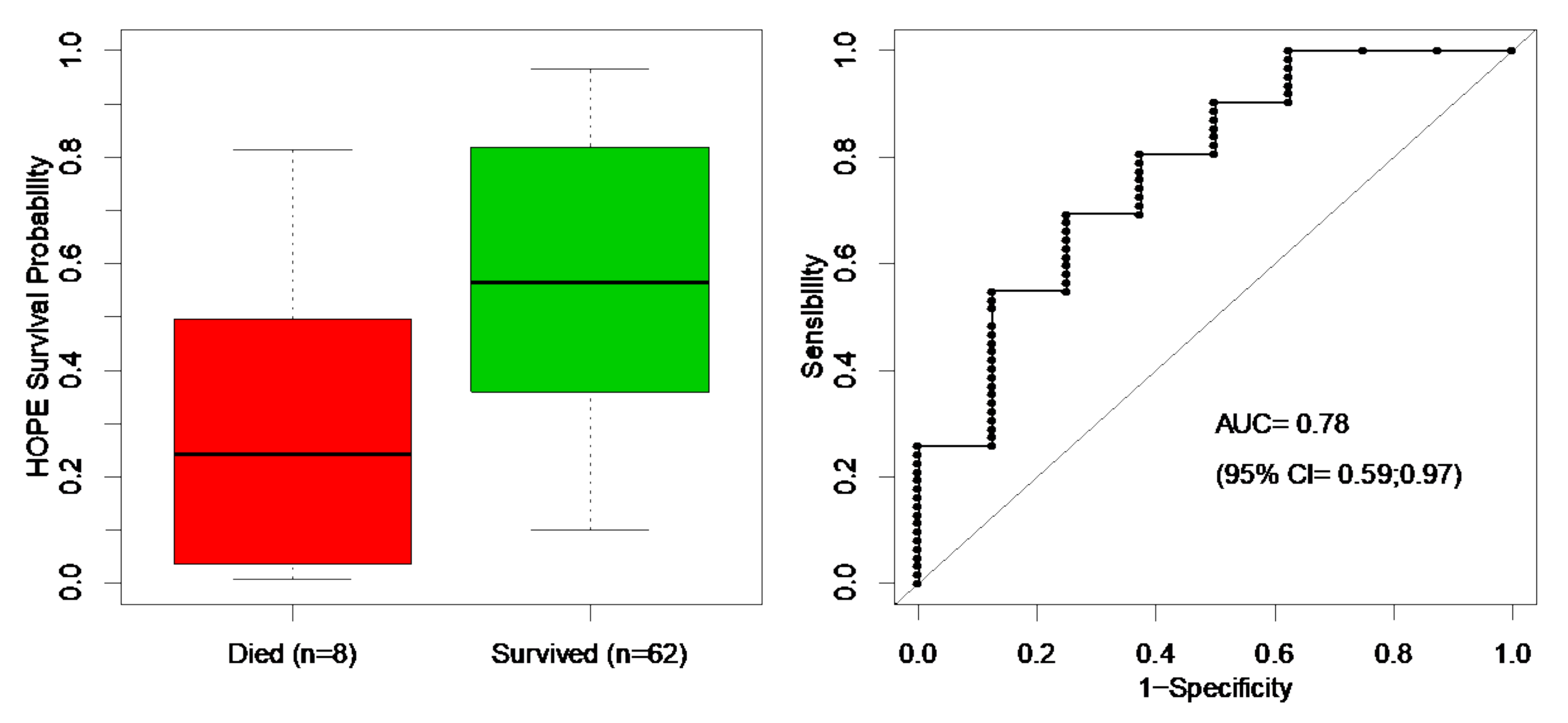
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Link, M.S.; Berkow, L.C.; Kudenchuk, P.J.; Halperin, H.R.; Hess, E.P.; Moitra, V.K.; Neumar, R.W.; O’Neil, B.J.; Paxton, J.H.; Silvers, S.M.; et al. Part 7: Adult advanced cardiovascular life support: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S444–S464. [Google Scholar] [CrossRef] [PubMed]
- Walpoth, B.H.; Walpoth-Aslan, B.N.; Mattle, H.P.; Radanov, B.P.; Schroth, G.; Schaeffler, L.; Fischer, A.P.; von Segesser, L.; Althaus, U. Outcome of survivors of accidental deep hypothermia and circulatory arrest treated with extracorporeal blood warming. N. Engl. J. Med. 1997, 337, 1500–1505. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, M.; Hugli, O.; Paal, P.; Darocha, T.; Blancher, M.; Husby, P.; Silfvast, T.; Carron, P.N.; Rousson, V. Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: The HOPE score. Resuscitation 2018, 126, 58–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pasquier, M.; Rousson, V.; Darocha, T.; Bouzat, P.; Kosiński, S.; Sawamoto, K.; Champigneulle, B.; Wiberg, S.; Wanscher, M.C.J.; Brodmann Maeder, M.; et al. Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: An external validation of the HOPE score. Resuscitation 2019, 139, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 339. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, E.H.; Lowenstein, S.R.; Koziol-McLain, J.; Barta, D.C.; Steiner, J. Chart reviews in emergency medicine research: Where are the methods? Ann. Emerg. Med. 1996, 27, 305–308. [Google Scholar] [CrossRef]
- Easterbrook, P.J.; Berlin, J.A.; Gopalan, R. Matthews D.R. Publication bias in clinical research. Lancet 1991, 337, 867–872. [Google Scholar] [CrossRef]
- Begg, C.B.; Berlin, J.A. Publication bias and dissemination of clinical research. J. Natl. Cancer. Inst. 1989, 81, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Kicinski, M.; Springate, D.A.; Kontopantelis, E. Publication bias in meta-analyses from the Cochrane Database of Systematic Reviews. Stat. Med. 2015, 34, 2781–2793. [Google Scholar] [CrossRef] [PubMed]
- Stern, J.M.; Simes, R.J. Publication bias evidence of delayed publication in a cohort study of clinical research projects. BMJ 1997, 315, 640–645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saczkowski, R.S.; Brown, D.J.A.; Abu-Laban, R.B.; Fradet, G.; Schulze, C.J.; Kuzak, N.D. Prediction and risk stratification of survival in accidental hypothermia requiring extracorporeal life support: An individual patient data meta-analysis. Resuscitation 2018, 127, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, M.; Hugli, O.; Rousson, V. Reply to: Combining individual patient data from multiple trials require specific modelling techniques in order to provide accurate predictions. Resuscitation 2018, 129, e2. [Google Scholar] [CrossRef] [PubMed]
- Antretter, H.; Dapunt, O.E.; Mueller, L.C. Portable cardiopulmonary bypass: Resuscitation from prolonged ice-water submersion and asystole. Ann. Thorac. Surg. 1994, 58, 1786–1787. [Google Scholar] [CrossRef]
- Lott, C.; Truhlář, A.; Alfonzo, A.; Barelli, A.; González-Salvado, V.; Hinkelbein, J.; Nolan, J.P.; Paal, P.; Perkins, G.D.; Thies, K.C. European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances. Resuscitation 2021, 161, 152–219. [Google Scholar] [CrossRef] [PubMed]
- Rünitz, K.; Thornberg, K.; Wanscher, M. Resuscitation of severely hypothermic and multitraumatised female following long-term cardiac arrest. Ugeskr. Laeg. 2009, 171, 328–329. [Google Scholar] [PubMed]
| Overall (n = 70) | Survivors 62 (89%) | Non-Survivors 8 (11%) | p Value | |
|---|---|---|---|---|
| Continuous variables, median (IQR) | ||||
| Age (years) | 33 (1–95) | 39.5 (1–95) | 10.5 (2–65) | 0.02 |
| Temperature (°C) | 22.7 (13.5–28.9) | 23 (13.5–28.9) | 22 (20.7–25) | 0.70 |
| Potassium (mmol/L) | 4.2 (2.4–16.1) | 4.2 (2.4–11.8) | 5.8 (2.9–16.1) | 0.16 |
| CPR duration (min) | 95 (20–307) | 95 (20–307) | 125 (60–263) | 0.12 |
| pH (60/70 patients) | 7.0 (6.4–7.8) | 7.0 (6.4– 7.8) | 6.8 (6.4–7.3) | 0.28 |
| Lactate (mmol/L) (30/70 patients) | 13 (3–31) | 13 (3–25) | 31 (31–31) | 0.09 |
| PaCO2 (kPa) (41/70 patients) | 7.33 (2.48–29.73) | 6.3 (2.48–19.1) | 10.38 (7.3–29.73) | 0.08 |
| Categorical variables, n (%) | ||||
| Sex | 0.19 | |||
| Female | 23 (33%) | 22 (96%) | 1 (4%) | |
| Male | 47 (67%) | 40 (85%) | 7 (15%) | |
| Mechanism | 0.02 | |||
| Exposure | 41 (59%) | 39 (95%) | 2 (5%) | |
| Immersion | 9 (13%) | 9 (100%) | 0 (0%) | |
| Submersion | 15 (21%) | 10 (67%) | 5 (33%) | |
| Avalanche | 5 (7%) | 4 (80%) | 1 (20%) | |
| Asphyxia-related mechanism | 0.002 | |||
| Yes a | 20 (29%) | 14 (70%) | 6 (30%) | |
| No b | 50 (71%) | 48 (96%) | 2 (4%) | |
| Cardiac rhythm | 0.20 | |||
| Asystole | 36 (54%) | 30 (83%) | 6 (17%) | |
| Ventricular fibrillation | 28 (42%) | 27 (96%) | 1 (4%) | |
| PEA | 3 (4%) | 3 (100%) | 0 (0%) | |
| CA circumstance | 0.09 | |||
| Unwitnessed CA | 52 (75%) | 44 (85%) | 8 (15%) | |
| Witnessed CA | 17 (25%) | 17 (100%) | 0 (0%) | |
| Type of ECLS | 0.25 | |||
| CPB | 49 (70%) | 42 (86%) | 7 (14%) | |
| ECMO | 21 (30%) | 20 (95%) | 1 (5%) | |
| Sensitivity a | Specificity b | PPV c | NPV d | FP e | FN e | |
|---|---|---|---|---|---|---|
| HOPE derivation study (n = 286) f | ||||||
| HOPE ≥ 10% | 106/106 = 100% | 92/180 = 51% | 106/194 = 55% | 92/92 = 100% | 88/286 = 31% | 0/286 = 0% |
| (95% CI) | (97–100%) | (44–58%) | (48–61%) | (96–100%) | (26–36%) | (0–1%) |
| HOPE validation study (n = 122) f | ||||||
| HOPE ≥ 10% | 50/51 = 98% | 34/71 = 48% | 50/87 = 57% | 34/35 = 97% | 37/122 = 30% | 1/122 = 1% |
| (95% CI) | (90–100%) | (37–59%) | (47–67%) | (85–99%) | (85–99%) | (0–4%) |
| Present study (n = 70) | ||||||
| HOPE ≥ 10% | 61/62 = 98% | 3/8 = 38% | 61/66 = 92% | 3/4 = 75% | 5/70 = 7% | 1/70 = 1% |
| (95% CI) | (91–100%) | (14–69%) | (83–97%) | (30–95%) | (3–16%) | (0–8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grin, N.; Rousson, V.; Darocha, T.; Hugli, O.; Carron, P.-N.; Zingg, T.; Pasquier, M. Hypothermia Outcome Prediction after Extracorporeal Life Support for Hypothermic Cardiac Arrest Patients: Assessing the Performance of the HOPE Score in Case Reports from the Literature. Int. J. Environ. Res. Public Health 2021, 18, 11896. https://doi.org/10.3390/ijerph182211896
Grin N, Rousson V, Darocha T, Hugli O, Carron P-N, Zingg T, Pasquier M. Hypothermia Outcome Prediction after Extracorporeal Life Support for Hypothermic Cardiac Arrest Patients: Assessing the Performance of the HOPE Score in Case Reports from the Literature. International Journal of Environmental Research and Public Health. 2021; 18(22):11896. https://doi.org/10.3390/ijerph182211896
Chicago/Turabian StyleGrin, Nolan, Valentin Rousson, Tomasz Darocha, Olivier Hugli, Pierre-Nicolas Carron, Tobias Zingg, and Mathieu Pasquier. 2021. "Hypothermia Outcome Prediction after Extracorporeal Life Support for Hypothermic Cardiac Arrest Patients: Assessing the Performance of the HOPE Score in Case Reports from the Literature" International Journal of Environmental Research and Public Health 18, no. 22: 11896. https://doi.org/10.3390/ijerph182211896
APA StyleGrin, N., Rousson, V., Darocha, T., Hugli, O., Carron, P.-N., Zingg, T., & Pasquier, M. (2021). Hypothermia Outcome Prediction after Extracorporeal Life Support for Hypothermic Cardiac Arrest Patients: Assessing the Performance of the HOPE Score in Case Reports from the Literature. International Journal of Environmental Research and Public Health, 18(22), 11896. https://doi.org/10.3390/ijerph182211896









