Association between Temporomandibular Joint Disorder and Weight Changes: A Longitudinal Follow-Up Study Using a National Health Screening Cohort
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Definition of Temporomandibular Joint Disorder (Independent Variable)
2.3. Definition of Weight Change (Dependent Variable)
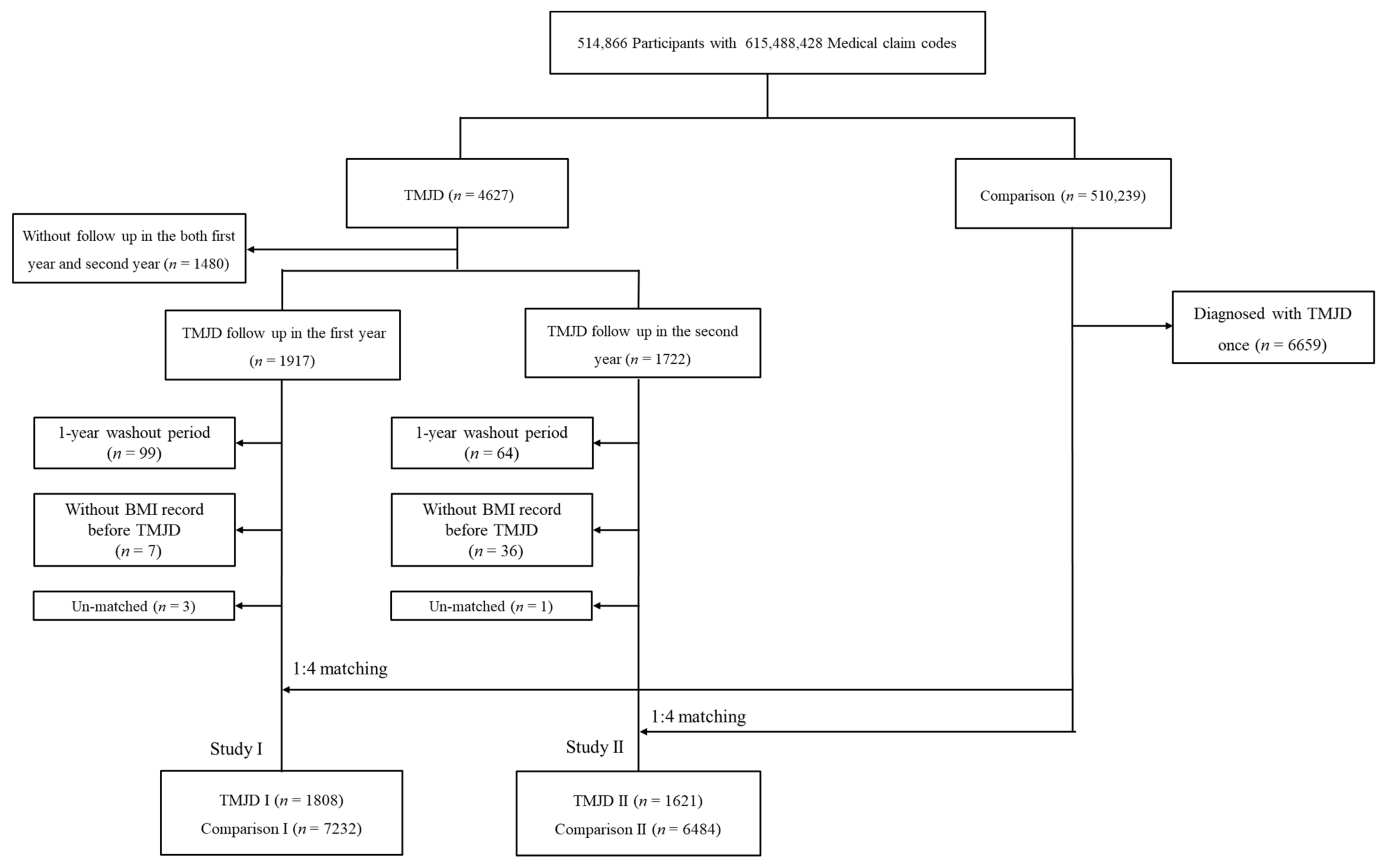
2.4. Participant Selection
2.5. Covariates
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gilheaney, Ó.; Stassen, L.F.; Walshe, M. The epidemiology, nature, and impact of eating and swallowing problems in adults presenting with temporomandibular disorders. Cranio 2020, 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, S.F.; Huggins, K.H.; LeResche, L.; Von Korff, M.; Howard, J.; Truelove, E.; Sommers, E. Epidemiology of Signs and Symptoms in Temporomandibular Disorders: Clinical Signs in Cases and Controls. J. Am. Dent. Assoc. 1990, 120, 273–281. [Google Scholar] [CrossRef]
- Liu, F.; Steinkeler, A. Epidemiology, Diagnosis, and Treatment of Temporomandibular Disorders. Dent. Clin. N. Am. 2013, 57, 465–479. [Google Scholar] [CrossRef] [PubMed]
- Song, H.-S.; Shin, J.-S.; Lee, J.; Lee, Y.J.; Kim, M.-R.; Cho, J.-H.; Kim, K.-W.; Park, Y.; Park, S.-Y.; Kim, S.; et al. Association between temporomandibular disorders, chronic diseases, and ophthalmologic and otolaryngologic disorders in Korean adults: A cross-sectional study. PLoS ONE 2018, 13, e0191336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhim, E.; Han, K.; Yun, K.-I. Association between temporomandibular disorders and obesity. J. Cranio-Maxillofac. Surg. 2016, 44, 1003–1007. [Google Scholar] [CrossRef]
- Chisnoiu, A.M.; Picos, A.M.; Popa, S.; Chisnoiu, P.D.; Lascu, L.; Picos, A.; Chisnoiu, R. Factors involved in the etiology of temporomandibular disorders—A literature review. Med. Pharm. Rep. 2015, 88, 473–478. [Google Scholar] [CrossRef]
- Yadav, S.; Yang, Y.; Dutra, E.H.; Robinson, J.L.; Wadhwa, S. Temporomandibular Joint Disorders in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 1213–1217. [Google Scholar] [CrossRef]
- Gilheaney, Ó.; Stassen, L.F.; Walshe, M. Prevalence, Nature, and Management of Oral Stage Dysphagia in Adults With Temporomandibular Joint Disorders: Findings From an Irish Cohort. J. Oral Maxillofac. Surg. 2018, 76, 1665–1676. [Google Scholar] [CrossRef]
- Byun, S.-H.; Min, C.; Yoo, D.-M.; Yang, B.-E.; Choi, H.-G. Increased Risk of Migraine in Patients with Temporomandibular Disorder: A Longitudinal Follow-Up Study Using a National Health Screening Cohort. Diagnostics 2020, 10, 724. [Google Scholar] [CrossRef]
- Ohrbach, R.; Fillingim, R.B.; Mulkey, F.; Gonzalez, Y.; Gordon, S.; Gremillion, H.; Lim, P.-F.; Ribeiro-Dasilva, M.; Greenspan, J.D.; Knott, C.; et al. Clinical findings and pain symptoms as potential risk factors for chronic TMD: Descriptive data and empirically identified domains from the OPPERA case-control study. J. Pain 2011, 12, T27–T45. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.Y.; Min, C.; Oh, D.J.; Choi, H.G. Tobacco Smoking and Alcohol Consumption Are Related to Benign Parotid Tumor: A Nested Case-Control Study Using a National Health Screening Cohort. Clin. Exp. Otorhinolaryngol. 2019, 12, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Byun, S.-H.; Min, C.; Choi, H.-G.; Hong, S.J. Increased Risk of Temporomandibular Joint Disorder in Patients with Rheumatoid Arthritis: A Longitudinal Follow-Up Study. J. Clin. Med. 2020, 9, 3005. [Google Scholar] [CrossRef]
- Kim, S.Y.; Min, C.; Yoo, D.M.; Chang, J.; Lee, H.-J.; Park, B.; Choi, H.G. Hearing Impairment Increases Economic Inequality. Clin. Exp. Otorhinolaryngol. 2021, 14, 278–286. [Google Scholar] [CrossRef]
- WHO, I. IOTF. The Asia-Pacific Perspective. Redefining Obesity and Its Treatment. In Obesity: Preventing and Managing the Global Epidemic; WHO: Geneva, Switzerland, 2000. [Google Scholar]
- Jordani, P.C.; Campi, L.B.; Braido, G.V.V.; Fernandes, G.; Visscher, C.M.; Gonçalves, D. Obesity, sedentarism and TMD-pain in adolescents. J. Oral Rehabil. 2019, 46, 460–467. [Google Scholar] [CrossRef]
- Ahlberg, J.P.; Kovero, O.A.; Hurmerinta, K.A.; Zepa, I.; Nissinen, M.J.; Könönen, M.H. Maximal bite force and its association with signs and symptoms of TMD, occlusion, and body mass index in a cohort of young adults. Cranio 2003, 21, 248–252. [Google Scholar] [CrossRef]
- Jordani, P.C.; Campi, L.; Circeli, G.Z.; Visscher, C.M.; Bigal, M.E.; Gonçalves, D. Obesity as a risk factor for temporomandibular disorders. J. Oral Rehabil. 2016, 44, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Miettinen, O.; Kämppi, A.; Tanner, T.; Anttonen, V.; Patinen, P.; Päkkilä, J.; Tjäderhane, L.; Sipilä, K. Association of Temporomandibular Disorder Symptoms with Physical Fitness among Finnish Conscripts. Int. J. Environ. Res. Public Health 2021, 18, 3032. [Google Scholar] [CrossRef]
- Pereira, L.J.; Gavião, M.B.D.; Bonjardim, L.R.; Castelo, P.M.; Van Der Bilt, A. Muscle thickness, bite force, and craniofacial dimensions in adolescents with signs and symptoms of temporomandibular dysfunction. Eur. J. Orthod. 2007, 29, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Irving, J.; Wood, G.; Hackett, A. Does temporomandibular disorder pain dysfunction syndrome affect dietary intake? Dent. Update 1999, 26, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Blair, E.H.; Epstein, L.H.; McDermott, M.D. Psychological stress and glucose metabolism in obese and normal-weight subjects: A possible mechanism for differences in stress-induced eating. Health Psychol. 1990, 9, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Edwards, D.C.; Bowes, C.C.; Penlington, C.; Durham, J. Temporomandibular disorders and dietary changes: A cross-sectional survey. J. Oral Rehabil. 2021. [Google Scholar] [CrossRef] [PubMed]
- Perez, C. Temporomandibular disorders in children and adolescents. Gen. Dent. 2018, 66, 51–55. [Google Scholar] [PubMed]
| Characteristics | Study I | Study II | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (n) | TMJD I (n, %) | Total (n) | Comparison I (n, %) | p-Value | Total (n) | TMJD II (n, %) | Total (n) | Comparison II (n, %) | p-Value | |
| Age (years) | 1.000 | 1.000 | ||||||||
| 40–44 | 1808 | 66 (3.7) | 7232 | 264 (3.7) | 1621 | 64 (4.0) | 6484 | 256 (4.0) | ||
| 45–49 | 1808 | 239 (13.2) | 7232 | 956 (13.2) | 1621 | 199 (12.3) | 6484 | 796 (12.3) | ||
| 50–54 | 1808 | 326 (18.0) | 7232 | 1304 (18.0) | 1621 | 358 (22.1) | 6484 | 1432 (22.1) | ||
| 55–59 | 1808 | 359 (19.9) | 7232 | 1436 (19.9) | 1621 | 265 (16.4) | 6484 | 1060 (16.4) | ||
| 60–64 | 1808 | 228 (12.6) | 7232 | 912 (12.6) | 1621 | 192 (11.8) | 6484 | 768 (11.8) | ||
| 65–69 | 1808 | 247 (13.7) | 7232 | 988 (13.7) | 1621 | 209 (12.9) | 6484 | 836 (12.9) | ||
| 70–74 | 1808 | 188 (10.4) | 7232 | 752 (10.4) | 1621 | 221 (13.6) | 6484 | 884 (13.6) | ||
| 75–79 | 1808 | 131 (7.3) | 7232 | 524 (7.3) | 1621 | 80 (4.9) | 6484 | 320 (4.9) | ||
| 80–84 | 1808 | 21 (1.2) | 7232 | 84 (1.2) | 1621 | 30 (1.9) | 6484 | 120 (1.9) | ||
| 85+ | 1808 | 3 (0.2) | 7232 | 12 (0.2) | 1621 | 3 (0.2) | 6484 | 12 (0.2) | ||
| Sex | 1.000 | 1.000 | ||||||||
| Male | 1808 | 849 (47.0) | 7232 | 3396 (47.0) | 1621 | 737 (45.5) | 6484 | 2948 (45.5) | ||
| Female | 1808 | 959 (53.0) | 7232 | 3836 (53.0) | 1621 | 884 (54.5) | 6484 | 3536 (54.5) | ||
| Income | 1.000 | 1.000 | ||||||||
| 1 (lowest) | 1808 | 283 (15.7) | 7232 | 1132 (15.7) | 1621 | 244 (15.1) | 6484 | 976 (15.1) | ||
| 2 | 1808 | 252 (13.9) | 7232 | 1008 (13.9) | 1621 | 231 (14.3) | 6484 | 924 (14.3) | ||
| 3 | 1808 | 281 (15.5) | 7232 | 1124 (15.5) | 1621 | 277 (17.1) | 6484 | 1108 (17.1) | ||
| 4 | 1808 | 375 (20.7) | 7232 | 1500 (20.7) | 1621 | 340 (21.0) | 6484 | 1360 (21.0) | ||
| 5 (highest) | 1808 | 617 (34.1) | 7232 | 2468 (34.1) | 1621 | 529 (32.6) | 6484 | 2116 (32.6) | ||
| Region of residence | 1.000 | 1.000 | ||||||||
| Urban | 1808 | 740 (40.9) | 7232 | 2960 (40.9) | 1621 | 675 (41.6) | 6484 | 2700 (41.6) | ||
| Rural | 1808 | 1068 (59.1) | 7232 | 4272 (59.1) | 1621 | 946 (58.4) | 6484 | 3784 (58.4) | ||
| Obesity † | 1.000 | 1.000 | ||||||||
| Underweight | 1808 | 43 (2.4) | 7232 | 172 (2.4) | 1621 | 38 (2.3) | 6484 | 152 (2.3) | ||
| Normal | 1808 | 725 (40.1) | 7232 | 2900 (40.1) | 1621 | 637 (39.3) | 6484 | 2548 (39.3) | ||
| Overweight | 1808 | 529 (29.3) | 7232 | 2116 (29.3) | 1621 | 472 (29.1) | 6484 | 1888 (29.1) | ||
| Obese I | 1808 | 474 (26.2) | 7232 | 1896 (26.2) | 1621 | 445 (27.5) | 6484 | 1780 (27.5) | ||
| Obese II | 1808 | 37 (2.1) | 7232 | 148 (2.1) | 1621 | 29 (1.8) | 6484 | 116 (1.8) | ||
| Smoking status | 0.036 * | 0.002 * | ||||||||
| Nonsmoker | 1808 | 1346 (74.5) | 7232 | 5357 (74.1) | 1621 | 1250 (77.1) | 6484 | 4820 (74.3) | ||
| Past smoker | 1808 | 228 (12.6) | 7232 | 801 (11.1) | 1621 | 178 (11.0) | 6484 | 671 (10.4) | ||
| Current smoker | 1808 | 234 (12.9) | 7232 | 1074 (14.9) | 1621 | 193 (11.9) | 6484 | 993 (15.3) | ||
| Alcohol consumption | 0.572 | 0.879 | ||||||||
| <1 time a week | 1808 | 1319 (73.0) | 7232 | 5228 (72.3) | 1621 | 1197 (73.8) | 6484 | 4800 (74.0) | ||
| ≥1 time a week | 1808 | 489 (27.1) | 7232 | 2004 (27.7) | 1621 | 424 (26.2) | 6484 | 1684 (26.0) | ||
| Systolic blood pressure | 0.002 * | 0.007 * | ||||||||
| <120 mmHg | 1808 | 629 (34.8) | 7232 | 2338 (32.3) | 1621 | 561 (34.6) | 6484 | 2078 (32.1) | ||
| 120–139 mmHg | 1808 | 900 (49.8) | 7232 | 3531 (48.8) | 1621 | 787 (48.6) | 6484 | 3100 (47.8) | ||
| ≥140 mmHg | 1808 | 279 (15.4) | 7232 | 1363 (18.9) | 1621 | 273 (16.8) | 6484 | 1306 (20.1) | ||
| Diastolic blood pressure | 0.002 * | 0.005 * | ||||||||
| <80 mmHg | 1808 | 930 (51.4) | 7232 | 3524 (48.7) | 1621 | 839 (51.8) | 6484 | 3079 (47.5) | ||
| 80–89 mmHg | 1808 | 647 (35.8) | 7232 | 2545 (35.2) | 1621 | 550 (33.9) | 6484 | 2331 (36.0) | ||
| ≥90 mmHg | 1808 | 231 (12.8) | 7232 | 1163 (16.1) | 1621 | 232 (14.3) | 6484 | 1074 (16.6) | ||
| Fasting blood glucose | 0.188 | 0.381 | ||||||||
| <100 mg/dL | 1808 | 1201 (66.4) | 7232 | 4746 (65.6) | 1621 | 1104 (68.1) | 6484 | 4359 (67.2) | ||
| 100–125 mg/dL | 1808 | 497 (27.5) | 7232 | 1957 (27.1) | 1621 | 411 (25.4) | 6484 | 1636 (25.2) | ||
| ≥126 mg/dL | 1808 | 110 (6.1) | 7232 | 529 (7.3) | 1621 | 106 (6.5) | 6484 | 489 (7.5) | ||
| Total cholesterol | 0.016 * | 0.510 | ||||||||
| <200 mg/dL | 1808 | 999 (55.3) | 7232 | 3788 (52.4) | 1621 | 870 (53.7) | 6484 | 3377 (52.1) | ||
| 200–239 mg/dL | 1808 | 607 (33.6) | 7232 | 2470 (34.2) | 1621 | 544 (33.6) | 6484 | 2261 (34.9) | ||
| ≥240 mg/dL | 1808 | 202 (11.2) | 7232 | 974 (13.5) | 1621 | 207 (12.8) | 6484 | 846 (13.1) | ||
| CCI score | 0.562 | 0.297 | ||||||||
| 0 | 1808 | 1286 (71.1) | 7232 | 5221 (72.2) | 1621 | 1162 (71.7) | 6484 | 4737 (73.1) | ||
| 1 | 1808 | 259 (14.3) | 7232 | 974 (13.5) | 1621 | 225 (13.9) | 6484 | 867 (13.4) | ||
| 2 | 1808 | 143 (7.9) | 7232 | 526 (7.3) | 1621 | 131 (8.1) | 6484 | 434 (6.7) | ||
| 3 | 1808 | 52 (2.9) | 7232 | 245 (3.4) | 1621 | 50 (3.1) | 6484 | 205 (3.2) | ||
| ≥4 | 1808 | 68 (3.8) | 7232 | 266 (3.7) | 1621 | 53 (3.3) | 6484 | 241 (3.7) | ||
| Characteristics | TMJD I | Comparison I | Interaction ‡ | Linear Mixed Model ¶ | |||||
|---|---|---|---|---|---|---|---|---|---|
| Previous (Mean, SD) | Post 1yr (Mean, SD) | p-Value | Previous (Mean, SD) | Post 1yr (Mean, SD) | p-Value | p-Value | EV § | p-Value | |
| Total participants (n = 9040) | 23.58 ± 2.83 | 23.58 ± 2.83 | 0.957 | 23.62 ± 2.84 | 23.62 ± 2.89 | 0.979 | 0.769 | −0.014 | 0.850 |
| Age 40–60 years old, men (n = 2365) | 23.92 ± 2.54 | 24.04 ± 2.54 | 0.010 * | 23.98 ± 2.66 | 24.02 ± 2.67 | 0.154 | 0.146 | 0.044 | 0.736 |
| Age 40–60 years old, women (n = 2585) | 23.45 ± 3.09 | 23.49 ± 3.09 | 0.374 | 23.44 ± 2.92 | 23.47 ± 2.95 | 0.394 | 0.799 | 0.055 | 0.698 |
| Age ≥60 years old, men (n = 1880) | 23.23 ± 2.76 | 23.06 ± 2.62 | 0.032 | 23.28 ± 2.78 | 23.22 ± 2.83 | 0.092 | 0.208 | −0.135 | 0.389 |
| Age ≥60 years old, women (n = 2210) | 23.67 ± 2.84 | 23.61 ± 2.91 | 0.397 | 23.73 ± 2.94 | 23.72 ± 3.02 | 0.668 | 0.468 | −0.069 | 0.656 |
| Characteristics | TMJD I | Comparison I | Interaction ‡ | Linear Mixed Model ¶ | |||||
|---|---|---|---|---|---|---|---|---|---|
| Previous (Mean, SD) | Post 1 Year (Mean, SD) | p-Value | Previous (Mean, SD) | Post 1 Year (Mean, SD) | p-Value | p-Value | EV § | p-Value | |
| Underweight (n = 215) | 17.55 ± 0.80 | 17.99 ± 1.09 | 0.008 * | 17.57 ± 0.79 | 18.05 ± 1.46 | <0.001 * | 0.810 | −0.046 | 0.807 |
| Normal (n = 3625) | 21.26 ± 1.16 | 21.49 ± 1.55 | <0.001 * | 21.26 ± 1.17 | 21.46 ± 1.63 | <0.001 * | 0.649 | 0.042 | 0.465 |
| Overweight (n = 2645) | 23.96 ± 0.56 | 23.91 ± 1.19 | 0.254 | 24.01 ± 0.57 | 23.98 ± 1.29 | 0.334 | 0.584 | −0.068 | 0.154 |
| Obese I (n = 2370) | 26.58 ± 1.19 | 26.34 ± 1.82 | <0.001 * | 26.73 ± 1.26 | 26.47 ± 1.74 | <0.001 * | 0.785 | −0.108 | 0.165 |
| Obese II (n = 185) | 31.99 ± 2.45 | 30.72 ± 3.04 | 0.007 * | 31.52 ± 1.54 | 30.75 ± 2.34 | <0.001 * | 0.165 | −0.087 | 0.821 |
| Characteristics | TMJD II | Comparison II | Interaction ‡ | Linear Mixed Model ¶ | |||||
|---|---|---|---|---|---|---|---|---|---|
| Previous (Mean, SD) | Post 2 Years (Mean, SD) | p-Value | Previous (Mean, SD) | Post 2 Years (Mean, SD) | p-Value | p-Value | EV § | p-Value | |
| Total participants (n = 8105) | 23.70 ± 2.96 | 23.62 ± 2.84 | 0.064 | 23.69 ± 2.82 | 23.72 ± 2.90 | 0.148 | 0.003 † | −0.082 | 0.294 |
| Age 40–60 years, men (n = 2090) | 24.13 ± 2.68 | 24.21 ± 2.55 | 0.156 | 24.07 ± 2.65 | 24.14 ± 2.70 | 0.023 * | 0.879 | 0.047 | 0.740 |
| Age 40–60 years, women (n = 2340) | 23.38 ± 3.41 | 23.28 ± 2.98 | 0.343 | 23.28 ± 2.84 | 23.42 ± 2.87 | <0.001 * | 0.003 † | −0.109 | 0.458 |
| Age ≥60 years, men (n = 1595) | 23.36 ± 2.58 | 23.33 ± 2.83 | 0.763 | 23.39 ± 2.62 | 23.33 ± 2.77 | 0.110 | 0.963 | 0.023 | 0.888 |
| Age ≥60 years, women (n = 2080) | 23.90 ± 2.87 | 23.64 ± 2.88 | 0.001 * | 24.00 ± 3.02 | 23.93 ± 3.14 | 0.109 | 0.023† | −0.272 | 0.098 |
| Characteristics | TMJD II | Comparison II | Interaction ‡ | Linear Mixed Model ¶ | |||||
|---|---|---|---|---|---|---|---|---|---|
| Previous (Mean, SD) | Post 1 Year (Mean, SD) | p-Value | Previous (Mean, SD) | Post 1 Year (Mean, SD) | p-Value | p-Value | EV § | p-Value | |
| Underweight (n = 190) | 17.52 ± 0.88 | 18.58 ± 1.86 | 0.003 * | 17.50 ± 0.91 | 18.13 ± 1.72 | <0.001 * | 0.202 | 0.467 | 0.061 |
| Normal (n = 3185) | 21.39 ± 1.14 | 21.56 ± 1.51 | <0.001 * | 21.38 ± 1.14 | 21.63 ± 1.68 | <0.001 * | 0.151 | −0.071 | 0.248 |
| Overweight (n = 2360) | 23.96 ± 0.57 | 23.90 ± 1.59 | 0.355 | 23.98 ± 0.57 | 23.94 ± 1.40 | 0.292 | 0.574 | −0.039 | 0.488 |
| Obese I (n = 2225) | 26.66 ± 1.25 | 26.24 ± 1.87 | <0.001 * | 26.69 ± 1.25 | 26.45 ± 1.88 | <0.001 * | 0.010 † | −0.200 | 0.017 † |
| Obese II (n = 145) | 33.08 ± 6.27 | 30.84 ± 4.10 | 0.139 | 31.96 ± 3.26 | 31.33 ± 2.83 | 0.057 | 0.095 | −0.541 | 0.460 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Yoo, D.M.; Byun, S.-H.; Min, C.; Kim, J.H.; Kwon, M.J.; Kim, J.-H.; Choi, H.G. Association between Temporomandibular Joint Disorder and Weight Changes: A Longitudinal Follow-Up Study Using a National Health Screening Cohort. Int. J. Environ. Res. Public Health 2021, 18, 11793. https://doi.org/10.3390/ijerph182211793
Kim SY, Yoo DM, Byun S-H, Min C, Kim JH, Kwon MJ, Kim J-H, Choi HG. Association between Temporomandibular Joint Disorder and Weight Changes: A Longitudinal Follow-Up Study Using a National Health Screening Cohort. International Journal of Environmental Research and Public Health. 2021; 18(22):11793. https://doi.org/10.3390/ijerph182211793
Chicago/Turabian StyleKim, So Young, Dae Myoung Yoo, Soo-Hwan Byun, Chanyang Min, Ji Hee Kim, Mi Jung Kwon, Joo-Hee Kim, and Hyo Geun Choi. 2021. "Association between Temporomandibular Joint Disorder and Weight Changes: A Longitudinal Follow-Up Study Using a National Health Screening Cohort" International Journal of Environmental Research and Public Health 18, no. 22: 11793. https://doi.org/10.3390/ijerph182211793
APA StyleKim, S. Y., Yoo, D. M., Byun, S.-H., Min, C., Kim, J. H., Kwon, M. J., Kim, J.-H., & Choi, H. G. (2021). Association between Temporomandibular Joint Disorder and Weight Changes: A Longitudinal Follow-Up Study Using a National Health Screening Cohort. International Journal of Environmental Research and Public Health, 18(22), 11793. https://doi.org/10.3390/ijerph182211793








