The Effects of Wearing a Removable-Partial-Denture on the Bite Forces: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
- Bilateral posterior edentulism (class 1 of Kennedy classification) in one arch, or in both arches, rehabilitated with one/two removable prosthesis/es (CoCr/PMMA/Valplast-RPD) with clasps positioned on the bicuspids, that the patient had been using for at least 1 year, since more than 5 months are necessary for the patient to adapt to functional use with the new dentures, as suggested by Moreno et al. [11].
- The prostheses were checked with polyether vinyl materials for pressure points and precision of fit and, if necessary, relined until a good fit was achieved.
- Lack of articular/muscular, dental, or spontaneous pain.
- Sixty-five years old, or older (according to the definition of a geriatric patient) [12].
2.2. Exclusion Criteria
- The patient was suffering from psychiatric diseases or other conditions that could affect the movement.
- The patient was suffering from periodontitis, due to possible reduced bone support and related sensory function, possible mobility and associated symptoms which could compromise chewing strength.
- The patient had diabetes or was undergoing cancer treatment.
2.3. Method Error
2.4. Statistical Analysis
3. Results
3.1. MBF and Gender
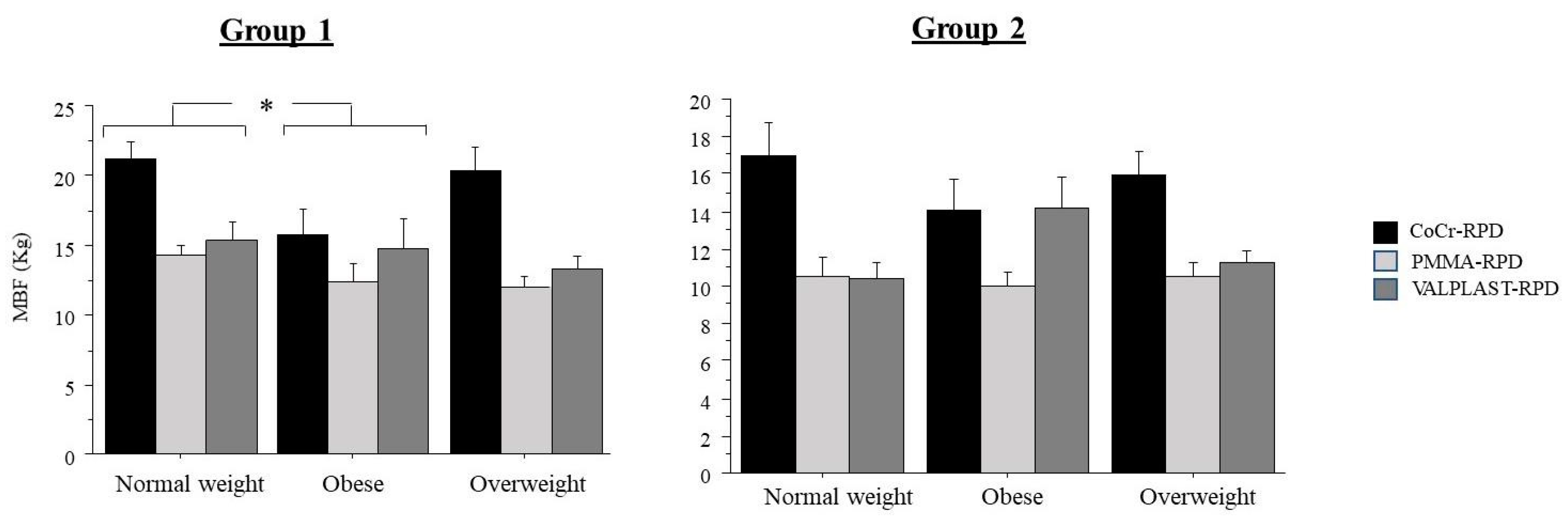
3.2. MBF and Weight Category
3.3. Bite Force and Prosthesis
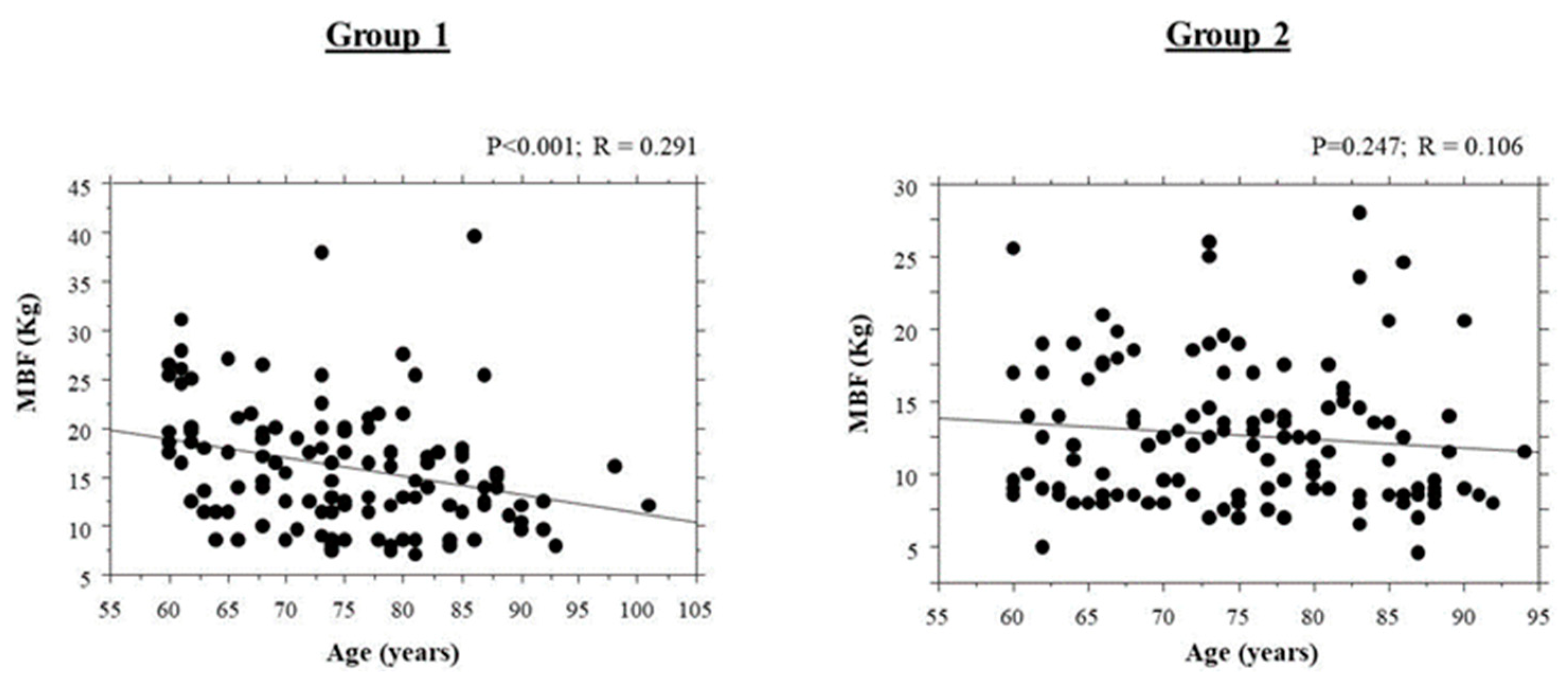
3.4. Correlation of Bite Force with Age
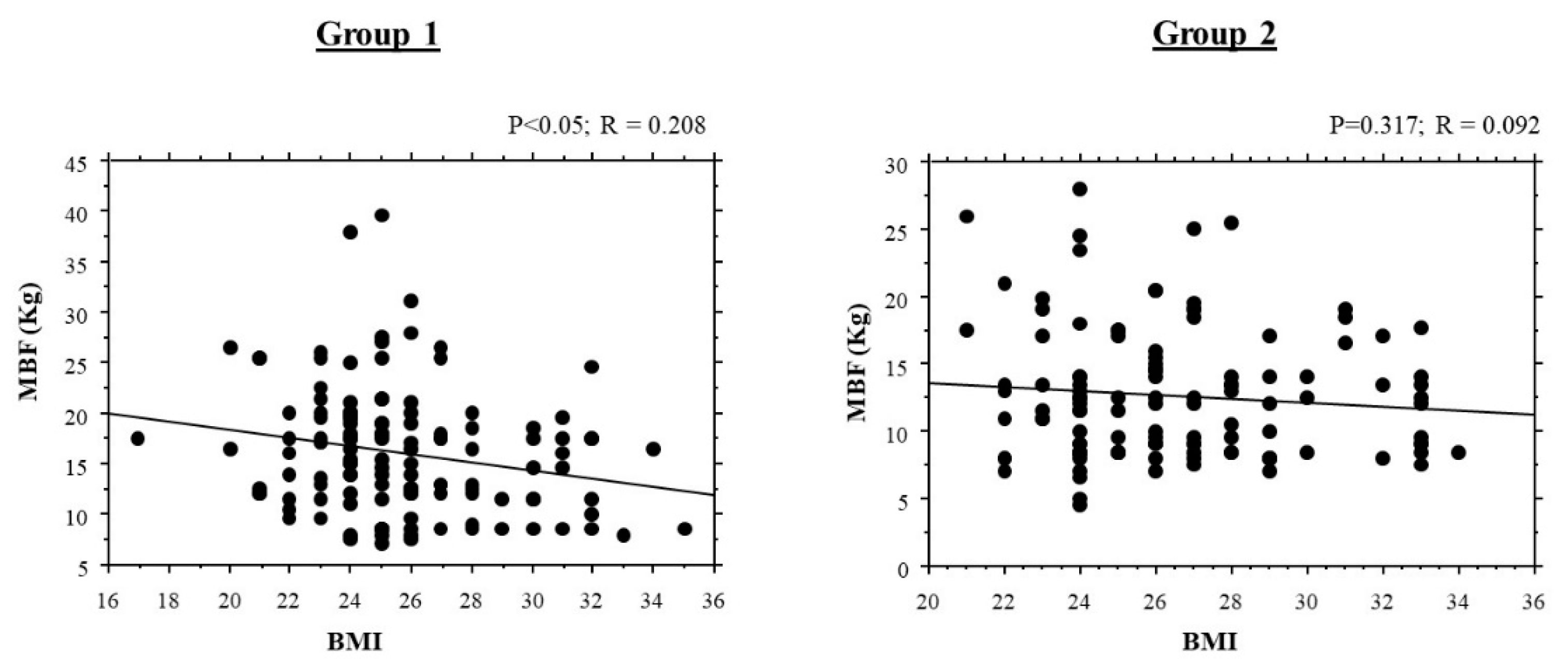
3.5. Correlations of Bite Force with Body Mass Index Values
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Su, Y.; Yuki, M.; Hirayama, K.; Sato, M.; Han, T. Denture Wearing and Malnutrition Risk Among Community-Dwelling Older Adults. Nutrients 2020, 12, 151. [Google Scholar] [CrossRef] [Green Version]
- Craig’s Restorative Dental Materials-13th Edition. Available online: https://www.elsevier.com/books/craigs-restorative-dental-materials/sakaguchi/978-0-323-08108-5 (accessed on 4 June 2020).
- Wadachi, J.; Sato, M.; Igarashi, Y. Evaluation of the rigidity of dentures made of injection-molded materials. Dent. Mater. J. 2013, 32, 508–511. [Google Scholar] [CrossRef] [Green Version]
- Macura-Karbownik, A.; Chladek, G.; Żmudzki, J.; Kasperski, J. Chewing efficiency and occlusal forces in PMMA, acetal and polyamide removable partial denture wearers. Acta Bioeng. Biomech. 2016, 18, 137–144. [Google Scholar] [PubMed]
- Manzon, L.; Fratto, G.; Poli, O.; Infusino, E. Patient and Clinical Evaluation of Traditional Metal and Polyamide Removable Partial Dentures in an Elderly Cohort. J. Prosthodont. 2019, 28, 868–875. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.P.; Dhiman, R.K.; Bedi, R.P.S.; Girish, S.H. Flexible denture base material: A viable alternative to conventional acrylic denture base material. Contemp. Clin. Dent. 2011, 2, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Borie, E.; Orsi, I.A.; Fuentes, R.; Beltrán, V.; Navarro, P.; Pareja, F.; Raimundo, L.B. Maximum bite force in elderly indigenous and non-indigenous denture wearers. Acta Odontol. Latinoam. 2014, 27, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Van Der Bilt, A. Assessment of mastication with implications for oral rehabilitation: A review. J. Oral Rehabil. 2011, 38, 754–780. [Google Scholar] [CrossRef]
- Okamoto, N.; Amano, N.; Nakamura, T.; Yanagi, M. Relationship between tooth loss, low masticatory ability, and nutritional indices in the elderly: A cross-sectional study. BMC Oral Health 2019, 19, 110. [Google Scholar] [CrossRef] [Green Version]
- Manzon, L.; Vozza, I.; Poli, O. Bite Force in Elderly with Full Natural Dentition and Different Rehabilitation Prosthesis. Int. J. Environ. Res. Public Health 2021, 18, 1424. [Google Scholar] [CrossRef]
- Moreno, A. Epidemiological Data and Survival Rate of Removable Partial Dentures. J. Clin. Diagn. Res. 2016, 10, ZC84–ZC87. [Google Scholar] [CrossRef]
- Motegi, E.; Nomura, M.; Tachiki, C.; Miyazaki, H.; Takeuchi, F.; Takaku, S.; Abe, Y.; Miyatani, M.; Ogai, T.; Fuma, A.; et al. Occlusal force in people in their sixties attending college for elderly. Bull. Tokyo Dent. Coll. 2009, 50, 135–140. [Google Scholar] [CrossRef] [Green Version]
- Hu, Z.-G.; Cheng, H.; Zheng, M.; Zheng, Z.-Q.; Ma, S.-Z. Quantitative study on occlusal balance of normal occlusion in intercuspal position. Zhonghua Kou Qiang Yi Xue Za Zhi Zhonghua Kouqiang Yixue Zazhi Chin. J. Stomatol. 2006, 41, 618–620. [Google Scholar]
- Tatematsu, M.; Mori, T.; Kawaguchi, T.; Takeuchi, K.; Hattori, M.; Morita, I.; Nakagaki, H.; Kato, K.; Murakami, T.; Tuboi, S.; et al. Masticatory performance in 80-year-old individuals. Gerodontology 2004, 21, 112–119. [Google Scholar] [CrossRef]
- Sarita, P.T.N.; Witter, D.J.; Kreulen, C.M.; Hof, M.A.V.; Creugers, N.H.J. Chewing ability of subjects with shortened dental arches. Community Dent. Oral Epidemiol. 2003, 31, 328–334. [Google Scholar] [CrossRef]
- Vieira, M.; Bommarito, S.; Takaki, P. Maximum Bite Force Analysis in Different Age Groups. Int. Arch. Otorhinolaryngol. 2014, 18, 272–276. [Google Scholar] [CrossRef] [Green Version]
- Poli, O.; Manzon, L.; Niglio, T.; Ettorre, E.; Vozza, I. Masticatory Force in Relation with Age in Subjects with Full Permanent Dentition: A Cross-Sectional Study. Health 2021, 9, 700. [Google Scholar] [CrossRef] [PubMed]
- Mayil, M.; Keser, G.; Demir, A.; Pekiner, F.N. Assessment of Masseter Muscle Appearance and Thickness in Edentulous and Dentate Patients by Ultrasonography. Open Dent. J. 2018, 12, 723–734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phillips’ Science of Dental Materials-11th Edition. Available online: https://www.elsevier.com/books/phillips-science-of-dental-materials/anusavice/978-1-4557-3461-0 (accessed on 4 June 2020).
- Fayad, M.I.; Alruwaili, H.H.T.; Khan, M.S.; Baig, M.N. Bite force evaluation in complete denture wearer with different denture base materials: A randomized controlled clinical trial. J. Int. Soc. Prev. Community Dent. 2018, 8, 416–419. [Google Scholar] [CrossRef] [PubMed]
- Eerikäinen, E.; Könönen, M. Forces required by complete dentures for penetrating food in simulated function. J. Oral Rehabil. 1987, 14, 607–613. [Google Scholar] [CrossRef]
- Mioche, L.; Bourdiol, P.; Monier, S. Chewing behaviour and bolus formation during mastication of meat with different textures. Arch. Oral Biol. 2003, 48, 193–200. [Google Scholar] [CrossRef]
- Tewksbury, C.D.; Callaghan, K.X.; Fulks, B.A.; Gerstner, G.E. Individuality of masticatory performance and of masticatory muscle temporal parameters. Arch. Oral Biol. 2018, 90, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Luraschi, J.; Schimmel, M.; Bernard, J.-P.; Gallucci, G.O.; Belser, U.; Müller, F. Mechanosensation and maximum bite force in edentulous patients rehabilitated with bimaxillary implant-supported fixed dental prostheses. Clin. Oral Implant. Res. 2011, 23, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, D. Bite force and dental implant treatment: A short review. Med. Devices Évid. Res. 2017, 10, 141–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
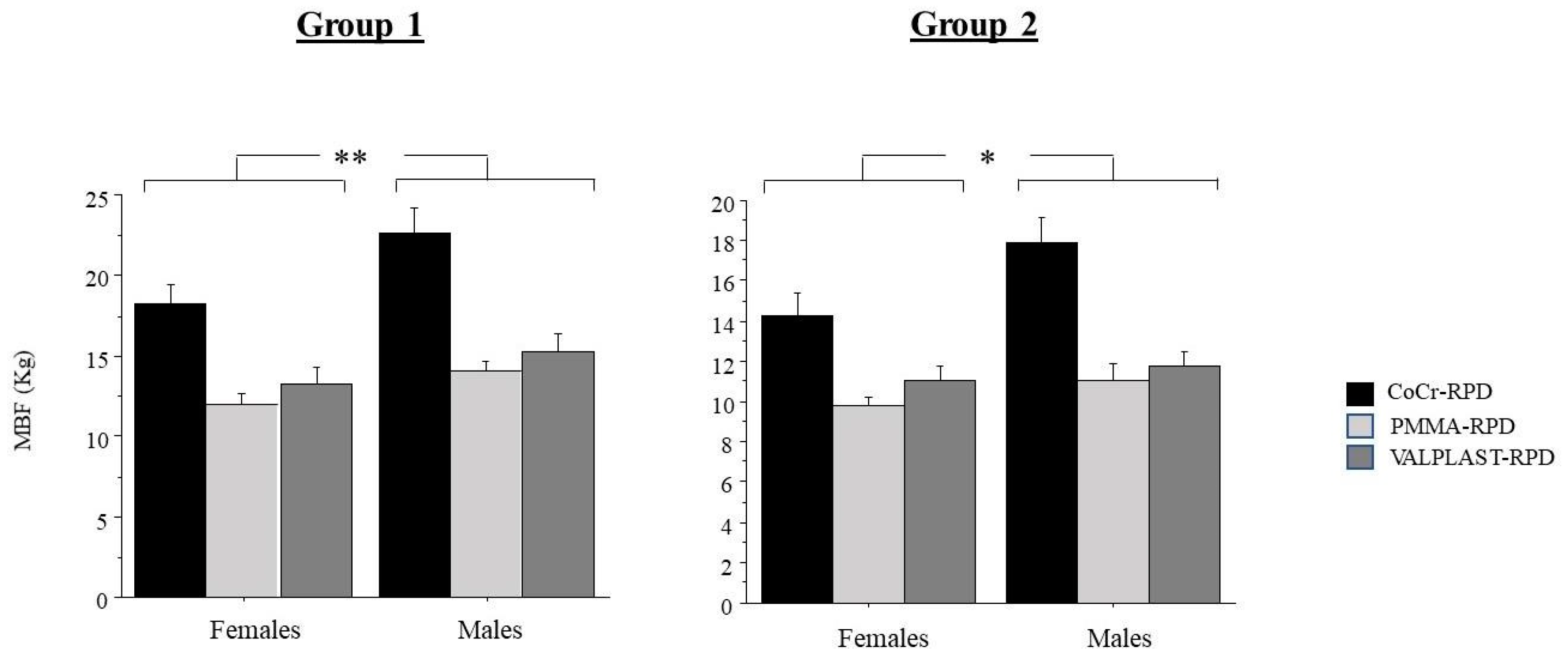
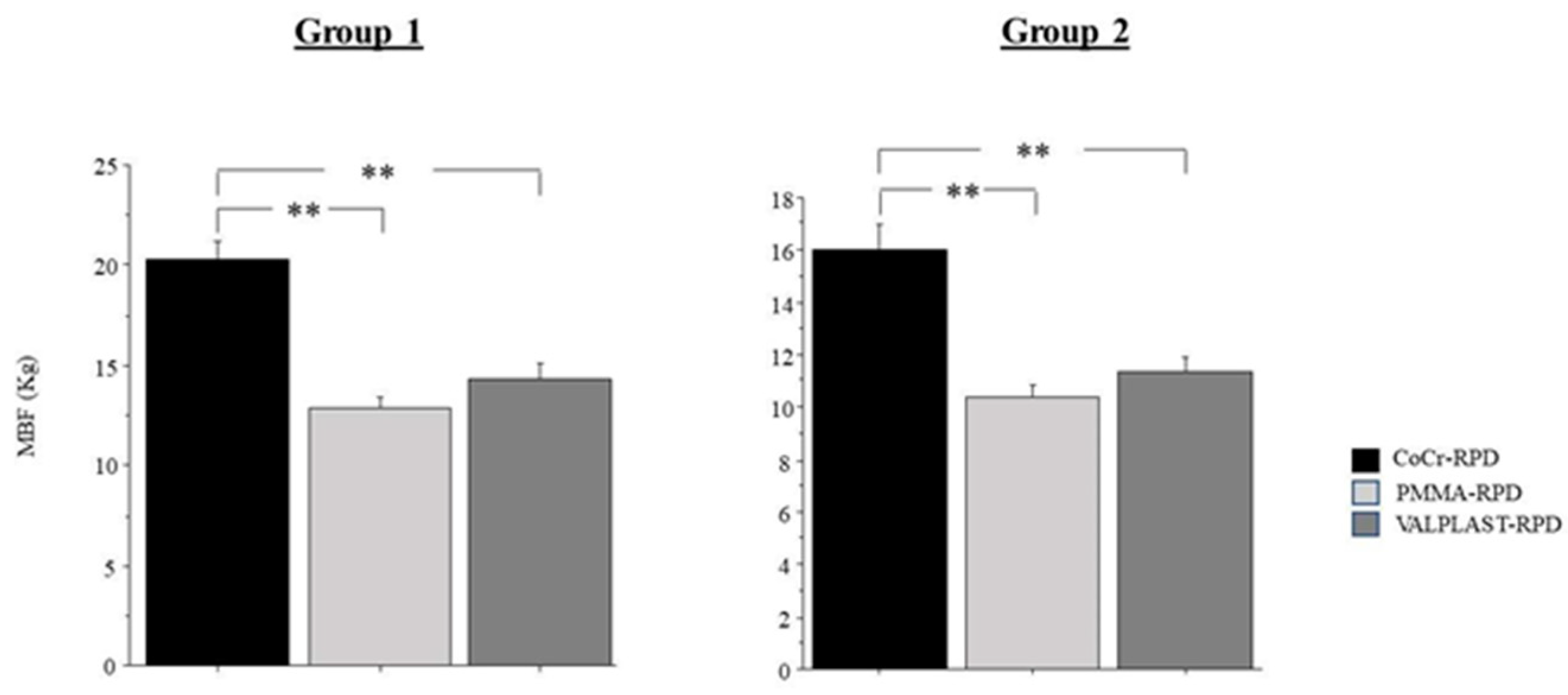
| Type of Prosthesis | Gender | MBF Higher Value | MBF Lower Value | MBF Mean Value | N of Subjects (%) with a UBF > 8 kg | |
|---|---|---|---|---|---|---|
| GROUP 1 | CoCr-RPD | males | 39.5 | 12 | 22 | 14 (63.7%) |
| females | 26.5 | 8.5 | 17.5 | 9 (35%) | ||
| PMMA-RPD | males | 1.5 | 8.5 | 14 | 0 | |
| females | 17 | 7 | 11 | 0 | ||
| V-RPD | male | 24.5 | 7.5 | 15 | 4 (20%) | |
| females | 21.5 | 8.5 | 13 | 2 (10%) | ||
| GROUP 2 | CoCr-RPD | males | 28 | 8.5 | 18 | 7 (35%) |
| females | 25.5 | 4.5 | 14 | 1 (5%) | ||
| PMMA-RPD | males | 17.5 | 5 | 11 | 0 | |
| females | 13.5 | 7.5 | 10 | 0 | ||
| V-RPD | males | 19 | 7 | 11 | 0 | |
| females | 1.7 | 7 | 11 | 0 |
| Type of Prosthesis | Gender | Max Value | Min Value | Mean Value | N of Overweight Subjects (%) | N of Obese Subjects | ||
|---|---|---|---|---|---|---|---|---|
| GROUP 1 RPD/TEETH | CoCr-RPD | males | 32 | 21 | 25.1 | 12 (54%) | 2 | |
| females | 34 | 20 | 25 | 14 (53%) | 3 | |||
| PMMA- RPD | males | 33 | 17 | 26.2 | 13 (65%) | 5 | ||
| females | 33 | 21 | 25.9 | 14 (63%) | 3 | |||
| Valplast- RPD | male | 31 | 23 | 26.3 | 13 (65%) | 4 | ||
| females | 30 | 21 | 25.7 | 12 (60%) | 3 | |||
| GROUP 2 RPD/RPD | CoCr-RPD/ CoCr-RPD | males | 33 | 21 | 26.2 | 13 (65%) | 4 | |
| females | 30 | 22 | 25.9 | 12 (60%) | 2 | |||
| PMMA-RPD/PMMA- RPD | males | 33 | 24 | 27.2 | 14 (70%) | 4 | ||
| females | 31 | 22 | 26.8 | 13 (65%) | 4 | |||
| V-RPD/ V-RPD | males | 33 | 23 | 26.8 | 13 (70%) | 3 | ||
| females | 34 | 22 | 26.1 | 13 (65%) | 3 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vozza, I.; Manzon, L.; Passarelli, P.C.; Pranno, N.; Poli, O.; Grippaudo, C. The Effects of Wearing a Removable-Partial-Denture on the Bite Forces: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 11401. https://doi.org/10.3390/ijerph182111401
Vozza I, Manzon L, Passarelli PC, Pranno N, Poli O, Grippaudo C. The Effects of Wearing a Removable-Partial-Denture on the Bite Forces: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(21):11401. https://doi.org/10.3390/ijerph182111401
Chicago/Turabian StyleVozza, Iole, Licia Manzon, Pier Carmine Passarelli, Nicola Pranno, Ottavia Poli, and Cristina Grippaudo. 2021. "The Effects of Wearing a Removable-Partial-Denture on the Bite Forces: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 21: 11401. https://doi.org/10.3390/ijerph182111401
APA StyleVozza, I., Manzon, L., Passarelli, P. C., Pranno, N., Poli, O., & Grippaudo, C. (2021). The Effects of Wearing a Removable-Partial-Denture on the Bite Forces: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(21), 11401. https://doi.org/10.3390/ijerph182111401








