Usability of Virtual Visits for the Routine Clinical Care of Trans Youth during the COVID-19 Pandemic: Youth and Caregiver Perspectives
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedures
2.2. Participants
2.3. Measures
2.3.1. Socio-Demographic and Clinical Characteristics
2.3.2. Telehealth Usability Questionnaire
2.3.3. Differences between Virtual and In-Person Visits, Challenges, and Future Preferences
2.4. Data Analysis
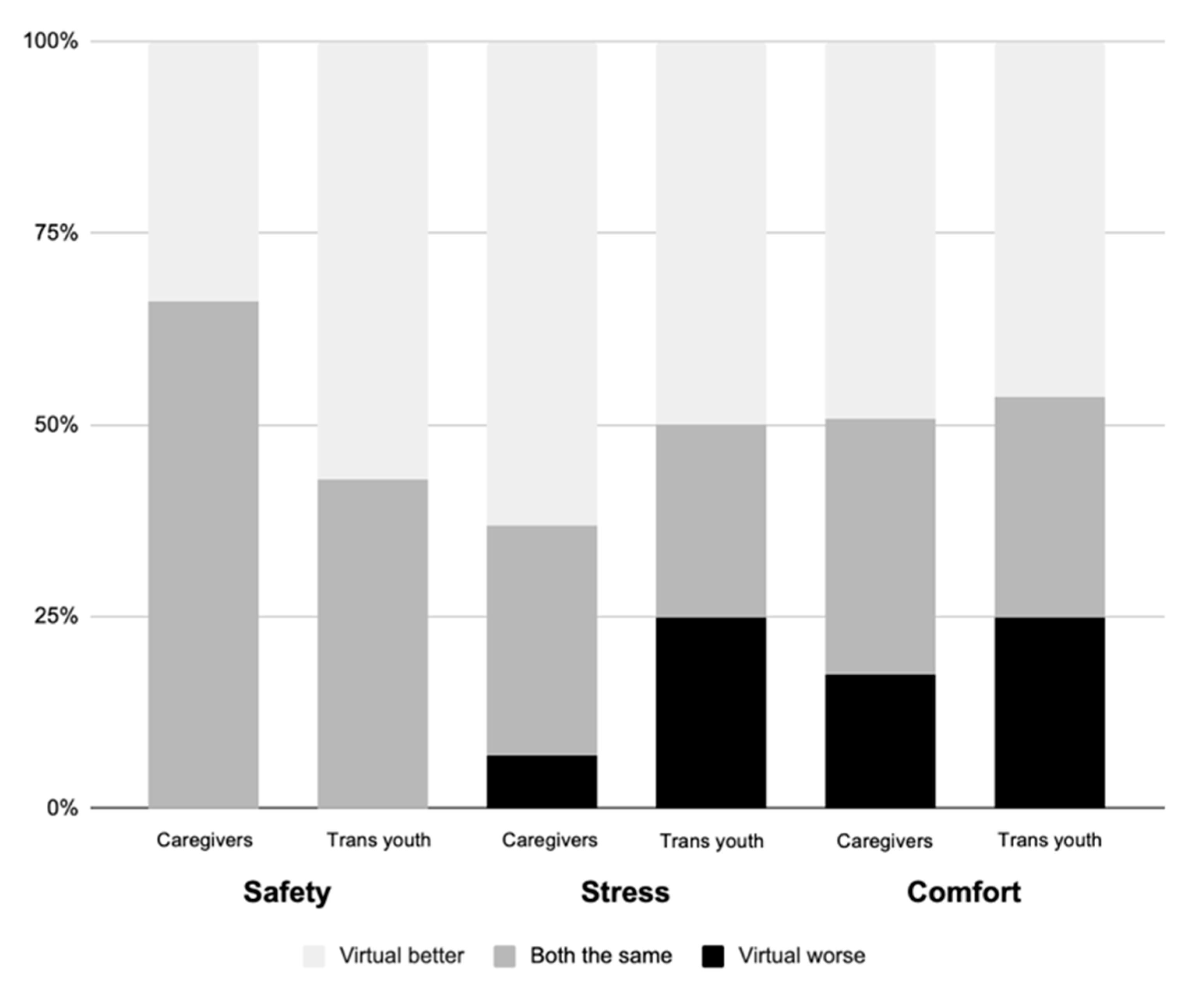
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychological Association. Guidelines for psychological practice with transgender and gender nonconforming people. Am. Psychol. 2015, 70, 832–864. [Google Scholar] [CrossRef]
- Thorne, N.; Yip, A.K.-T.; Bouman, W.P.; Marshall, E.; Arcelus, J. The terminology of identities between, outside and beyond the gender binary—A systematic review. Int. J. Transgend. 2019, 20, 138–154. [Google Scholar] [CrossRef]
- Scandurra, C.; Mezza, F.; Maldonato, N.M.; Bottone, M.; Bochicchio, V.; Valerio, P.; Vitelli, R. Health of Nonbinary and Genderqueer People: A Systematic Review. Front. Psychol. 2019, 10, 1453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coleman, E.; Bockting, W.; Botzer, M.; Cohen-Kettenis, P.; De Cuypere, G.; Feldman, J.; Fraser, L.; Green, J.; Knudson, G.; Meyer, W.J.; et al. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. Int. J. Transgend. 2012, 13, 165–232. [Google Scholar] [CrossRef]
- Sumia, M.; Lindberg, N.; Työläjärvi, M.; Kaltiala-Heino, R. Current and recalled childhood gender identity in community youth in comparison to referred adolescents seeking sex reassignment. J. Adolesc. 2017, 56, 34–39. [Google Scholar] [CrossRef] [Green Version]
- Eisenberg, M.E.; Gower, A.; McMorris, B.J.; Nic Rider, G.; Shea, G.; Coleman, E. Risk and Protective Factors in the Lives of Transgender/Gender Nonconforming Adolescents. J. Adolesc. Health 2017, 61, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Kidd, K.M.; Sequeira, G.M.; Douglas, C.; Paglisotti, T.; Inwards-Breland, D.J.; Miller, E.; Coulter, R.W.S. Prevalence of Gender-Diverse Youth in an Urban School District. Pediatrics 2021, 147, e2020049823. [Google Scholar] [CrossRef] [PubMed]
- van der Miesen, A.I.; Steensma, T.D.; de Vries, A.L.; Bos, H.; Popma, A. Psychological Functioning in Transgender Adolescents Before and After Gender-Affirmative Care Compared With Cisgender General Population Peers. J. Adolesc. Health 2020, 66, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Olson-Kennedy, J.; Okonta, V.; Clark, L.F.; Belzer, M. Physiologic Response to Gender-Affirming Hormones Among Transgender Youth. J. Adolesc. Health 2017, 62, 397–401. [Google Scholar] [CrossRef]
- De Vries, A.L.; McGuire, J.K.; Steensma, T.; Wagenaar, E.C.F.; Doreleijers, T.A.; Cohen-Kettenis, P.T. Young Adult Psychological Outcome After Puberty Suppression and Gender Reassignment. Pediatrics 2014, 134, 696–704. [Google Scholar] [CrossRef] [Green Version]
- Turban, J.L.; King, D.; Carswell, J.M.; Keuroghlian, A. Pubertal Suppression for Transgender Youth and Risk of Suicidal Ideation. Pediatrics 2020, 145, e20191725. [Google Scholar] [CrossRef]
- Fox, D.A.; Tan, M.; Lalani, R.; Atkinson, L.; Hursh, B.; Metzger, D.L. MON-LB302 Evaluating the Impact of a New Intake Process for British Columbia Children’s Hospital Gender Clinic. J. Endocr. Soc. 2020, 4, MON-LB302. [Google Scholar] [CrossRef]
- Wood, H.; Sasaki, S.; Bradley, S.J.; Singh, D.; Fantus, S.; Owen-Anderson, A.; Di Giacomo, A.; Bain, J.; Zucker, K.J. Patterns of Referral to a Gender Identity Service for Children and Adolescents (1976–2011): Age, Sex Ratio, and Sexual Orientation. J. Sex Marital. Ther. 2013, 39, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kaltiala-Heino, R.; Bergman, H.; Työläjärvi, M.; Frisen, L. Gender dysphoria in adolescence: Current perspectives. Adolesc. Health Med. Ther. 2018, 9, 31–41. [Google Scholar] [CrossRef] [Green Version]
- Safer, J.D.; Coleman, E.; Feldman, J.; Garofalo, R.; Hembree, W.; Radix, A.; Sevelius, J. Barriers to healthcare for transgender individuals. Curr. Opin. Endocrinol. Diabetes Obes. 2016, 23, 168–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, A.B.; Chan, A.; Hall, S.L.; Coronel Villabos, M.; Frohard-Dourlent, H.; Mehta, Y.; Millar, S.; O’Dwyer, C.; Susset, F.; Canadian Trans & Non-binary Youth Health Survey Research Group. Being Safe, Being Me 2019: Results of the Canadian Trans and Non-binary Youth Health Survey; Stigma and Resilience among Vulnerable Youth Centre, University of British Columbia: Vancouver, Canada, 2020; Available online: https://apsc-saravyc.sites.olt.ubc.ca/files/2020/12/Being-Safe-Being-Me-2019_SARAVYC_ENG_1.2.pdf (accessed on 5 January 2021).
- Sansfaçon, A.P.; Temple-Newhook, J.; Suerich-Gulick, F.; Feder, S.; Lawson, M.L.; Ducharme, J.; Ghosh, S.; Holmes, C.; On behalf of the Stories of Gender-Affirming Care Team. The experiences of gender diverse and trans children and youth considering and initiating medical interventions in Canadian gender-affirming speciality clinics. Int. J. Transgend. 2019, 20, 371–387. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Pan, B.; Liu, Y.; Wilson, A.; Ou, J.; Chen, R. Health care and mental health challenges for transgender individuals during the COVID-19 pandemic. Lancet Diabetes Endocrinol. 2020, 8, 564–565. [Google Scholar] [CrossRef]
- Kidd, J.D.; Jackman, K.B.; Barucco, R.; Dworkin, J.D.; Dolezal, C.; Navalta, T.V.; Belloir, J.; Bockting, W.O. Understanding the Impact of the COVID-19 Pandemic on the Mental Health of Transgender and Gender Nonbinary Individuals Engaged in a Longitudinal Cohort Study. J. Homosex. 2021, 68, 592–611. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine. Telemedicine: A Guide to Assessing Telecommunications in Health Care; Field, M.J., Ed.; National Academies Press: Washington, DC, USA, 1996. Available online: https://www.ncbi.nlm.nih.gov/books/NBK45440/ (accessed on 1 September 2021).
- Committee on Pediatric Workforce. The Use of Telemedicine to Address Access and Physician Workforce Shortages. Pediatrics 2015, 136, 202–209. [Google Scholar] [CrossRef] [Green Version]
- Fung, A.; Irvine, M.; Ayub, A.; Ziabakhsh, S.; Amed, S.; Hursh, B.E. Evaluation of telephone and virtual visits for routine pediatric diabetes care during the COVID-19 pandemic. J. Clin. Transl. Endocrinol. 2020, 22, 100238. [Google Scholar] [CrossRef]
- Sequeira, G.M.; Kidd, K.M.; Coulter, R.W.; Miller, E.; Fortenberry, D.; Garofalo, R.; Richardson, L.P.; Ray, K.N. Transgender Youths’ Perspectives on Telehealth for Delivery of Gender-Affirming Care. J. Adolesc. Health 2020, 68, 1207–1210. [Google Scholar] [CrossRef] [PubMed]
- Stoehr, J.R.; Jahromi, A.H.; Hunter, E.L.; Schechter, L.S. Telemedicine for Gender-Affirming Medical and Surgical Care: A Systematic Review and Call-to-Action. Transgender Health 2021. [Google Scholar] [CrossRef]
- Grasso, C.; Campbell, J.; Yunkun, E.; Todisco, D.; Thompson, J.; Gonzalez, A.; Brewster, A.; Keuroghlian, A.S. Gender-Affirming Care Without Walls: Utilization of Telehealth Services by Transgender and Gender Diverse People at a Federally Qualified Health Center. Transgender Health 2021. [Google Scholar] [CrossRef]
- Smalley, J.M.; Lozano, J.M.; McMahon, C.J.; Colburn, J.A. Improving Global Access to Transgender Healthcare: Outcomes of a Telehealth Quality Improvement Study for the Air Force Transgender Program. Transgender Health 2021. [Google Scholar] [CrossRef]
- Lock, L.; Anderson, B.; Hill, B.J. Transgender Care and the COVID-19 Pandemic: Exploring the Initiation and Continuation of Transgender Care In-Person and Through Telehealth. Transgender Health 2021. [Google Scholar] [CrossRef]
- Apple, D.E.; Lett, E.; Wood, S.; Baber, K.F.; Chuo, J.; Schwartz, L.A.; Petsis, D.; Faust, H.; Dowshen, N. Acceptability of Telehealth for Gender-Affirming Care in Transgender and Gender Diverse Youth and Their Caregivers. Transgender Health 2021. [Google Scholar] [CrossRef]
- Sequeira, G.M.; Kidd, K.M.; Rankine, J.; Miller, E.; Ray, K.N.; Fortenberry, J.D.; Richardson, L.P. Gender-Diverse Youth’s Experiences and Satisfaction with Telemedicine for Gender-Affirming Care During the COVID-19 Pandemic. Transgender Health 2021. [Google Scholar] [CrossRef]
- UBC Clinical Research Ethics General Guidance Notes|Office of Research Ethics. Available online: https://ethics.research.ubc.ca/ore/ubc-clinical-research-ethics-general-guidance-notes (accessed on 13 September 2021).
- Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans—TCPS 2 (2018)—Chapter 2: Scope and Ap-proach. Available online: https://ethics.gc.ca/eng/tcps2-eptc2_2018_chapter2-chapitre2.html (accessed on 13 September 2021).
- Alberta Innovates. ARECCI Ethics Guideline Tool. 2017. Available online: Albertainno-vates.ca/wp-content/uploads/2017/11/ARECCI-Ethics-Guideline-Tool.pdf (accessed on 13 September 2021).
- Parmanto, B.; Lewis, J.A.N.; Graham, K.M.; Bertolet, M. Development of the Telehealth Usability Questionnaire (TUQ). Int. J. Telerehabilitation 2016, 8, 3–10. [Google Scholar] [CrossRef]
- ISO 9241-11:1998(en), Ergonomic Requirements for Office Work with Visual Display Terminals (VDTs)—Part 11: Guidance on Usability. Available online: https://www.iso.org/obp/ui/#iso:std:iso:9241:-11:ed-1:v1:en (accessed on 13 September 2021).
- Norman, G. Likert scales, levels of measurement and the “laws” of statistics. Adv. Health Sci. Educ. 2010, 15, 625–632. [Google Scholar] [CrossRef]
- Nagelkerke, N.J.D. A note on a general definition of the coefficient of determination. Biometrika 1991, 78, 691–692. [Google Scholar] [CrossRef]
- Abramovich, A.; De Oliveira, C.; Kiran, T.; Iwajomo, T.; Ross, L.E.; Kurdyak, P. Assessment of Health Conditions and Health Service Use Among Transgender Patients in Canada. JAMA Netw. Open 2020, 3, e2015036. [Google Scholar] [CrossRef]
- Winter, S.; Diamond, M.; Green, J.; Karasic, D.; Reed, T.; Whittle, S.; Wylie, K. Transgender people: Health at the margins of society. Lancet 2016, 388, 390–400. [Google Scholar] [CrossRef]
- Hamnvik, O.-P.R.; Agarwal, S.; AhnAllen, C.G.; Goldman, A.L.; Reisner, S.L. Telemedicine and Inequities in Health Care Access: The Example of Transgender Health. Transgender Health 2020. [Google Scholar] [CrossRef]
- Testa, R.J.; Michaels, M.S.; Bliss, W.; Rogers, M.L.; Balsam, K.F.; Joiner, T. Suicidal ideation in transgender people: Gender minority stress and interpersonal theory factors. J. Abnorm. Psychol. 2017, 126, 125–136. [Google Scholar] [CrossRef]
- Markovic, L.; McDermott, D.; Stefanac, S.; Seiler-Ramadas, R.; Iabloncsik, D.; Smith, L.; Yang, L.; Kirchheiner, K.; Crevenna, R.; Grabovac, I. Experiences and Interactions with the Healthcare System in Transgender and Non-Binary Patients in Austria: An Exploratory Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 6895. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, A.E.; Kuvalanka, K.A.; Budge, S.L.; Benz, M.B.; Smith, J.Z. Health Care Experiences of Transgender Binary and Nonbinary University Students. Couns. Psychol. 2019, 47, 59–97. [Google Scholar] [CrossRef]
- Daikeler, J.; Bošnjak, M.; Lozar Manfreda, K. Web Versus Other Survey Modes: An Updated and Extended Meta-Analysis Comparing Response Rates. J. Survey Stat. Methodol. 2020, 8, 513–539. [Google Scholar] [CrossRef]
- De Koning, R.; Egiz, A.; Kotecha, J.; Ciuculete, A.C.; Ooi, S.Z.Y.; Bankole, N.D.A.; Erhabor, J.; Higginbotham, G.; Khan, M.; Dalle, D.U.; et al. Survey Fatigue During the COVID-19 Pandemic: An Analysis of Neurosurgery Survey Response Rates. Front Surg. 2021, 8, 690680. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Fredriksen-Goldsen, K.I.; McClain, C.; Kim, H.-J.; Suzer-Gurtekin, Z.T. Are Sexual Minorities Less Likely to Participate in Surveys? An Examination of Proxy Nonresponse Measures and Associated Biases with Sexual Orientation in a Population-Based Health Survey. Field Methods 2018, 30, 208–224. [Google Scholar] [CrossRef]

| All Participants n = 87 | Caregiver Filled the Survey n = 59 | Youth Filled the Survey n = 28 | |
|---|---|---|---|
| Age (years), mean (SD) | 15.55 (3.01) | 14.63 (2.65) | 17.48 (2.84) |
| Duration of follow-up at Gender Clinic (months), mean (SD) | 21.2 (20.5) | 19.4 (21.3) | 25 (18.5) |
| Sex assigned at birth, female, n (%) | 52 (60) | 33 (55) | 19 (67) |
| Reported gender identity (%) | |||
| Trans male/trans masculine | 46 (53) | 28 (47) | 18 (64) |
| Trans female/trans feminine | 35 (41) | 26 (44) | 9 (32) |
| Gender non-binary | 3 (3) | 3 (5) | 0 |
| Other | 3 (3) | 2 (3) | 1 (4) |
| Current endocrine therapies, n (%) | |||
| No medications | 21 (23) | 19 (32) | 2 (7) |
| Leuprolide | 31 (35) | 26 (44) | 5 (17) |
| Testosterone | 29 (33) | 11 (19) | 18 (64) |
| Estrogen | 13 (15) | 8 (14) | 5 (18) |
| Spironolactone | 5 (6) | 1 (2) | 4 (14) |
| Bleeding cessation and other | 4 (5) | 3 (5) | 1 (4) |
| Caregiver Filled the Survey n = 59 | Youth Filled the Survey n = 28 | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | ||
| Usefulness | 3.5 | 0.5 | 1–4 | 3.4 | 0.6 | 1–4 | 0.12 |
| A virtual visit improves my access to healthcare services | 3.3 | 0.8 | 1–4 | 2.8 | 1.2 | 1–4 | 0.04 * |
| A virtual visit saves me time traveling to a hospital or specialist clinic | 3.7 | 0.7 | 1–4 | 3.8 | 0.5 | 2–4 | 0.9 |
| A virtual visit provides for my healthcare needs | 3.7 | 0.6 | 2–4 | 3.5 | 0.7 | 2–4 | 0.18 |
| Ease of Use and Learnability | 3.6 | 0.5 | 1–4 | 3.5 | 0.6 | 1–4 | 0.34 |
| It was simple to use the virtual system | 3.7 | 0.6 | 1–4 | 3.5 | 0.7 | 2–4 | 0.12 |
| It was easy to learn to use the virtual system | 3.7 | 0.5 | 2–4 | 3.7 | 0.6 | 2–4 | 0.96 |
| I could become productive quickly using the virtual system | 3.5 | 0.7 | 2–4 | 3.4 | 0.8 | 1–4 | 0.31 |
| Interface Quality | 3.4 | 0.6 | 1–4 | 3.1 | 0.6 | 1–4 | 0.05 |
| The way I interact with the virtual system is pleasant | 3.3 | 0.8 | 1–4 | 3.0 | 1.0 | 1–4 | 0.16 |
| I like using the virtual system | 3.2 | 0.9 | 1–4 | 2.8 | 0.9 | 1–4 | 0.02 * |
| The virtual system is simple and easy to understand | 3.6 | 0.6 | 2–4 | 3.5 | 0.7 | 1–4 | 0.47 |
| This virtual system is able to do everything I would want it to do | 3.5 | 0.8 | 1–4 | 3.1 | 0.7 | 1–4 | 0.05 |
| Interaction Quality | 3.6 | 0.6 | 1–4 | 3.3 | 0.5 | 1–4 | 0.04 * |
| I could easily talk to the clinician using the virtual system | 3.7 | 0.6 | 2–4 | 3.4 | 0.6 | 2–4 | 0.1 |
| I could hear the clinician clearly using the virtual system | 3.7 | 0.6 | 2–4 | 3.7 | 0.5 | 3–4 | 0.63 |
| I felt I was able to express myself effectively using the virtual system | 3.6 | 0.7 | 2–4 | 3.2 | 0.7 | 2–4 | 0.02 * |
| I could see the clinician as well as if we met in person | 3.3 | 0.9 | 1–4 | 2.9 | 0.9 | 1–4 | 0.02 * |
| Reliability | 2.9 | 0.8 | 1–4 | 2.6 | 0.8 | 1–4 | 0.07 |
| Visits provided this way are the same as in-person visits | 2.9 | 0.9 | 1–4 | 2.2 | 1.0 | 1–4 | 0.0006 * |
| I was able to recover easily and quickly, if I made a mistake using the virtual system | 3.4 | 0.8 | 1–4 | 3.4 | 0.8 | 2–4 | 0.37 |
| The virtual system gave me error messages that clearly told me how to fix problems | 2.5 | 1.3 | 1–4 | 2.2 | 1.3 | 2–4 | 0.96 |
| Satisfaction and Future Use | 3.5 | 0.5 | 1–4 | 2.9 | 0.8 | 1–4 | 0.007 * |
| I felt comfortable communicating with the clinician during the virtual visit | 3.6 | 0.7 | 2–4 | 3.1 | 0.7 | 2–4 | 0.001 * |
| The virtual visit was an acceptable way to receive healthcare services | 3.3 | 0.8 | 1–4 | 2.8 | 1.0 | 1–4 | 0.01 * |
| I would use these services again | 3.5 | 0.8 | 1–4 | 2.5 | 1.1 | 1–4 | 0.0004 * |
| Overall, I am satisfied with this type of visit | 3.4 | 0.5 | 1–4 | 2.9 | 0.8 | 1–4 | 0.005 * |
| Overall usability | 3.4 | 0.8 | 1–4 | 3.1 | 0.9 | 1–4 | 0.01 * |
| Perceived Hard to Build a Relationship with Provider 1 | Would Desire to Continue Virtual Visits 2 | |||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | p-Value | aOR | 95% CI | p-Value | |
| Age (years) | 0.81 | 0.67–0.99 | 0.04 * | 1.06 | 0.73–1.53 | 0.76 |
| Sex assigned at birth (male) | 0.82 | 0.28–2.38 | 0.71 | 0.87 | 0.19–3.98 | 0.86 |
| Duration of follow up (months) | 1 | 0.98–1.03 | 0.89 | 0.99 | 0.96–1.03 | 0.71 |
| Distance from hospital (50-km) | - | - | 0.95 | 0.8–1.13 | 0.56 | |
| First visit was virtual (yes) | 0.63 | 0.12–3.27 | 0.56 | 0.06 | 0–1.15 | 0.06 |
| Current medications | - | - | ||||
| 0.54 | 0.03–10.15 | 0.678 | |||
| 1 | 0.03–36.24 | 0.998 | |||
| Starting a medication after virtual visit | - | - | ||||
| 11.84 | 0.7–199.8 | 0.087 | |||
| 4.83 | 0.2–119.58 | 0.336 | |||
| 6.29 | 0.38–104.07 | 0.199 | |||
| Trans youth filled out the survey (yes) | 2.79 | 0.85–9.16 | 0.09 | 1.25 | 0.26–6.01 | 0.78 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, C.; Fung, A.; Irvine, M.A.; Ziabakhsh, S.; Hursh, B.E. Usability of Virtual Visits for the Routine Clinical Care of Trans Youth during the COVID-19 Pandemic: Youth and Caregiver Perspectives. Int. J. Environ. Res. Public Health 2021, 18, 11321. https://doi.org/10.3390/ijerph182111321
Silva C, Fung A, Irvine MA, Ziabakhsh S, Hursh BE. Usability of Virtual Visits for the Routine Clinical Care of Trans Youth during the COVID-19 Pandemic: Youth and Caregiver Perspectives. International Journal of Environmental Research and Public Health. 2021; 18(21):11321. https://doi.org/10.3390/ijerph182111321
Chicago/Turabian StyleSilva, Carolina, Alex Fung, Michael A. Irvine, Shabnam Ziabakhsh, and Brenden E. Hursh. 2021. "Usability of Virtual Visits for the Routine Clinical Care of Trans Youth during the COVID-19 Pandemic: Youth and Caregiver Perspectives" International Journal of Environmental Research and Public Health 18, no. 21: 11321. https://doi.org/10.3390/ijerph182111321
APA StyleSilva, C., Fung, A., Irvine, M. A., Ziabakhsh, S., & Hursh, B. E. (2021). Usability of Virtual Visits for the Routine Clinical Care of Trans Youth during the COVID-19 Pandemic: Youth and Caregiver Perspectives. International Journal of Environmental Research and Public Health, 18(21), 11321. https://doi.org/10.3390/ijerph182111321






