Dissemination and Implementation Science Approaches for Occupational Safety and Health Research: Implications for Advancing Total Worker Health
Abstract
:1. Introduction
- The intervention is THE THING;
- Effectiveness research looks at whether THE THING works;
- Implementation research looks at how best to help people (e.g., employers and workers)/(work)places DO THE THING;
- Implementation strategies are the stuff researchers do to try to help people/(work)places DO THE THING as designed/intended (i.e., with fidelity), such as provide training, technical assistance, and/or incentives;
- Main implementation outcomes are HOW MUCH and HOW WELL they DO THE THING.
2. What Is D&I Science? A Brief Overview for TWH Researchers and Practitioners
Translational Science vs. D&I Science: Where Do They Overlap?
3. D&I in Plain Language
3.1. Does “the Thing” Work? Efficacy and Effectiveness Research
3.2. How Best to Do “the thing”? A Very Brief Overview of D&I Models, Theories, Frameworks, Methods, and Measures
3.3. D&I Strategies: The “Stuff” Researchers Do to Help Others Do “the Thing”
3.4. D&I Outcomes: How Much and How Well They “Do the Thing”
3.5. Context Matters
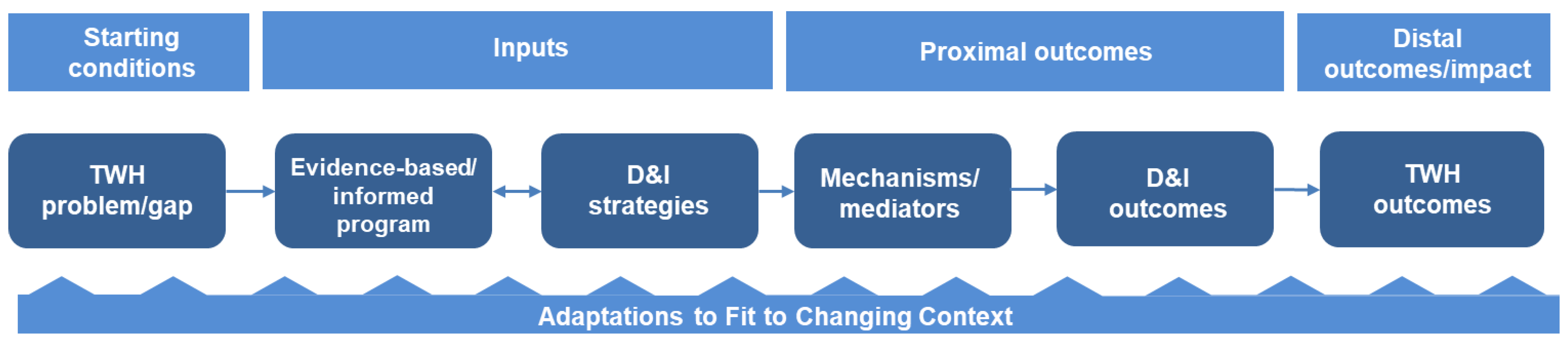
3.6. Putting It All Together: A Logic Model for D&I in TWH
3.7. A Few Other Important D&I Distinctions for TWH Researchers
4. Translating an Evidence-Based, Young Worker Program for TWH: A Case Study Example
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- NIOSH. What Is Total Worker Health? Available online: https://www.cdc.gov/niosh/twh/totalhealth.html (accessed on 17 April 2021).
- Tamers, S.L.; Chosewood, L.C.; Childress, A.; Hudson, H.; Nigam, J.; Chang, C.C. Total Worker Health® 2014–2018: The novel approach to worker safety, health, and well-being evolves. Int. J. Environ. Res. Public Health 2019, 16, 321. [Google Scholar] [CrossRef] [Green Version]
- Anger, W.K.; Elliot, D.L.; Bodner, T.; Olson, R.; Rohlman, D.S.; Truxillo, D.M.; Kuehl, K.S.; Hammer, L.B.; Montgomery, D. Effectiveness of Total Worker Health interventions. J. Occup. Health Psychol. 2015, 20, 226–247. [Google Scholar] [CrossRef] [Green Version]
- Carr, L.J.; Leonhard, C.; Tucker, S.; Fethke, N.; Benzo, R.; Gerr, F. Total Worker Health intervention increases activity of sedentary workers. Am. J. Prev. Med. 2016, 50, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, G.; Stoddard, A.M.; LaMontagne, A.D.; Emmons, K.; Hunt, M.K.; Youngstrom, R.; McLellan, D.; Christiani, D.C. A comprehensive worksite cancer prevention intervention: Behavior change results from a randomized controlled trial (United States). J. Public Health Policy 2003, 24, 5–25. [Google Scholar] [CrossRef] [PubMed]
- Tamers, S.L.; Streit, J.; Pana-Cryan, R.; Ray, T.; Syron, L.; Flynn, M.A.; Castillo, D.; Roth, G.; Geraci, C.; Guerin, R.; et al. Envisioning the future of work to safeguard the safety, health, and well-being of the workforce: A perspective from the CDC’s National Institute for Occupational Safety and Health. Am. J. Ind. Med. 2020, 63, 1065–1084. [Google Scholar] [CrossRef] [PubMed]
- Schulte, P.A.; Delclos, G.; Felknor, S.A.; Chosewood, L.C. Toward an expanded focus for occupational safety and health: A commentary. Int. J. Environ. Res. Public Health 2019, 16, 4946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glasgow, R.E.; Harden, S.M.; Gaglio, B.; Rabin, B.A.; Smith, M.L.; Porter, G.C.; Ory, M.G.; Estabrooks, P.A. RE-AIM planning and evaluation framework: Adapting to new science and practice with a twenty-year review. Front. Public Health 2019, 7, 64. [Google Scholar] [CrossRef] [Green Version]
- Bradley, C.J.; Grossman, D.C.; Hubbard, R.A.; Ortega, A.N.; Curry, S.J. Integrated interventions for improving Total Worker Health: A panel report from the National Institutes of Health Pathways to Prevention Workshop: Total Worker Health-what’s work got to do with it? Ann. Intern. Med. 2016, 165, 279–283. [Google Scholar] [CrossRef] [Green Version]
- Tamers, S.L.; Goetzel, R.; Kelly, K.M.; Luckhaupt, S.; Nigam, J.; Pronk, N.P.; Rohlman, D.S.; Baron, S.; Brosseau, L.M.; Bushnell, T.; et al. Research methodologies for Total Worker Health®: Proceedings from a workshop. J. Occup. Environ. Med. 2018, 60, 968. [Google Scholar] [CrossRef]
- Punnett, L.; Cavallari, J.M.; Henning, R.A.; Nobrega, S.; Dugan, A.G.; Cherniack, M.G. Defining ‘integration’ for Total Worker Health®: A new proposal. Ann. Work Expo. Health 2020, 64, 223–235. [Google Scholar] [CrossRef] [Green Version]
- NIH. Dissemination and Implementation Research in Health, PAR-19-274. Available online: https://grants.nih.gov/grants/guide/pa-files/PAR-19-274.html (accessed on 7 May 2021).
- Pawson, R. The Science of Evaluation: A Realist Manifesto; Sage: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Curran, G.M. Implementation science made too simple: A teaching tool. Implement. Sci. Commun. 2020, 1, 27. [Google Scholar] [CrossRef]
- Nilsen, P.; Bernhardsson, S. Context matters in implementation science: A scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv. Res. 2019, 19, 1–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stange, K.C.; Breslau, E.S.; Dietrich, A.J.; Glasgow, R.E. State-of-the-art and future directions in multilevel interventions across the cancer control continuum. J. Natl. Cancer Inst. Monogr. 2012, 44, 20–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feltner, C.; Peterson, K.; Palmieri Weber, R.; Cluff, L.; Coker-Schwimmer, E.; Viswanathan, M.; Lohr, K.N. The effectiveness of Total worker health interventions: A systematic review for a National Institutes of Health pathways to prevention workshop. Ann. Intern. Med. 2016, 165, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Dugan, A.G.; Punnett, L. Dissemination and implementation research for occupational safety and health. Occup. Health Sci. 2017, 1, 29–45. [Google Scholar] [CrossRef] [Green Version]
- Schulte, P.A.; Cunningham, T.R.; Nickels, L.; Felknor, S.; Guerin, R.; Blosser, F.; Chang, C.C.; Check, P.; Eggerth, D.; Flynn, M.; et al. Translation research in occupational safety and health: A proposed framework. Am. J. Ind. Med. 2017, 60, 1011–1022. [Google Scholar] [CrossRef]
- Birken, S.A.; Powell, B.J.; Shea, C.M.; Haines, E.R.; Alexis Kirk, M.; Leeman, J.; Rohweder, C.; Damschroder, L.; Presseau, J. Criteria for selecting implementation science theories and frameworks: Results from an international survey. Implement. Sci. 2017, 12, 124. [Google Scholar] [CrossRef]
- Strifler, L.; Cardoso, R.; McGowan, J.; Cogo, E.; Nincic, V.; Khan, P.A.; Scott, A.; Ghassemi, M.; MacDonald, H.; Lai, Y.; et al. Scoping review identifies significant number of knowledge translation theories, models, and frameworks with limited use. J. Clin. Epidemiol. 2018, 100, 92–102. [Google Scholar] [CrossRef]
- Tabak, R.G.; Khoong, E.C.; Chambers, D.; Brownson, R.C. Models in dissemination and implementation research: Useful tools in public health services and systems research. Front. Public Health Serv. Syst. Res. 2013, 2, 8. [Google Scholar] [CrossRef]
- Tabak, R.G.; Hook, M.; Chambers, D.A.; Brownson, R.C. The conceptual basis for dissemination and implementation research. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: New York, NY, USA, 2018; pp. 73–88. [Google Scholar]
- Brown, C.H.; Curran, G.; Palinkas, L.A.; Aarons, G.A.; Wells, K.B.; Jones, L.; Collins, L.M.; Duan, N.; Mittman, B.S.; Wallace, A.; et al. An overview of research and evaluation designs for dissemination and implementation. Annu. Rev. Public Health 2017, 38, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Landsverk, J.; Brown, C.H.; Smith, J.D.; Chamberlain, P.; Curran, G.M.; Palinkas, L.; Ogihara, M.; Czaja, S.; Goldhaber-Fiebert, J.D.; Vermeer, W.; et al. Design and analysis in dissemination and implementation research. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: New York, NY, USA, 2018; pp. 201–227. [Google Scholar]
- Glasgow, R.E.; Riley, W.T. Pragmatic measures: What they are and why we need them. Am. J. Prev. Med. 2013, 45, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Stanick, C.F.; Halko, H.M.; Nolen, E.A.; Powell, B.J.; Dorsey, C.N.; Mettert, K.D.; Weiner, B.J.; Barwick, M.; Wolfenden, L.; Damschroder, L.J.; et al. Pragmatic measures for implementation research: Development of the Psychometric and Pragmatic Evidence Rating Scale (PAPERS). Transl. Behav. Med. 2021, 11, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Fixsen, D.L.; Naoom, S.F.; Blase, K.A.; Friedman, R.M.; Wallace, F. Implementation Research: A Synthesis of the Literature; The National Implementation Research Network, FMHI Publication No. 231; University of South Florida, Louis de la Parte Florida Mental Health Institute: Tampa, FL, USA, 2005. [Google Scholar]
- Estabrooks, P.A.; Brownson, R.C.; Pronk, N.P. Dissemination and implementation science for public health professionals: An overview and call to action. Prev. Chronic Dis. 2018, 15, 180525. [Google Scholar] [CrossRef] [Green Version]
- Rogers, E.J. Diffusion of Innovations, 5th ed.; Free Press: New York, NY, USA, 2003. [Google Scholar]
- Luke, D.A.; Morshed, A.B.; McKay, V.R.; Combs, T.B. Systems science methods in dissemination and implementation research. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: New York, NY, USA, 2018; pp. 157–174. [Google Scholar]
- Glasgow, R.E.; Chambers, D. Developing robust, sustainable, implementation systems using rigorous, rapid and relevant science. Clin. Transl. Sci. 2012, 5, 48–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brownson, R.C.; Jacobs, J.A.; Tabak, R.G.; Hoehner, C.M.; Stamatakis, K.A. Designing for dissemination among public health researchers: Findings from a national survey in the United States. Am. J. Public Health 2013, 103, 1693–1699. [Google Scholar] [CrossRef] [PubMed]
- Bridging the Science and Practice of Designing for Dissemination: Going from Unicorns to Workhorses (Workshop). Available online: https://www1.ucdenver.edu/docs/librariesprovider94/di-docs/guides-and-tools/2018-d4d-workbook_revised2.pdf?sfvrsn=463c06b9_2 (accessed on 2 October 2021).
- Nobrega, S.; Kernan, L.; Plaku-Alakbarova, B.; Robertson, M.; Warren, N.; Henning, R.; CPH-NEW Research Team. Field tests of a participatory ergonomics toolkit for Total Worker Health. Appl. Erg. 2017, 60, 366–379. [Google Scholar] [CrossRef] [Green Version]
- Rabin, B.A.; Brownson, R.C. Terminology for dissemination and implementation research. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: New York, NY, USA, 2018; pp. 19–45. [Google Scholar]
- Crawford, J.O.; Davis, A.; Walker, G.; Cowie, H.; Ritchie, P. Evaluation of knowledge transfer for occupational safety and health in an organizational context: Development of an evaluation framework. Policy Pract. Health Saf. 2016, 14, 7–21. [Google Scholar] [CrossRef]
- Duryan, M.; Smyth, H.; Roberts, A.; Rowlinson, S.; Sherratt, F. Knowledge transfer for occupational health and safety: Cultivating health and safety learning culture in construction firms. Accid. Anal. Prev. 2020, 139, 105496. [Google Scholar] [CrossRef]
- Rondinone, B.M.; Boccuni, F.; Iavicoli, S. Trends and priorities in occupational health research and knowledge transfer in Italy. Scand. J. Work Environ. Health 2010, 36, 339–348. [Google Scholar] [CrossRef] [Green Version]
- Van Eerd, D.; Saunders, R. Integrated knowledge transfer and exchange: An organizational approach for stakeholder engagement and communications. Sch. Res. Commun. 2017, 8. [Google Scholar] [CrossRef]
- Cunningham, T.R.; Tinc, P.; Guerin, R.J.; Schulte, P.A. Translation research in occupational health and safety settings: Common ground and future directions. J. Saf. Res. 2020, 74, 161–167. [Google Scholar] [CrossRef]
- Austin, C.P. Translating translation. Nat. Rev. Drug Discov. 2018, 17, 455–456. [Google Scholar] [CrossRef]
- Fort, D.G.; Herr, T.M.; Shaw, P.L.; Gutzman, K.E.; Starren, J.B. Mapping the evolving definitions of translational research. J. Clin. Transl. Sci. 2017, 1, 60–66. [Google Scholar] [CrossRef]
- Leppin, A.L.; Mahoney, J.E.; Stevens, K.R.; Bartels, S.J.; Baldwin, L.M.; Dolor, R.J.; Proctor, E.K.; Scholl, L.; Moore, J.B.; Baumann, A.A.; et al. Situating dissemination and implementation sciences within and across the translational research spectrum. J. Clin. Transl. Sci. 2019, 4, 152–158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NIH. National Center for Advancing Translational Sciences (NCATS), Translational Science Spectrum. Available online: https://ncats.nih.gov/translation/spectrum (accessed on 17 April 2021).
- Shelton, R.C.; Lee, M.; Brotzman, L.E.; Wolfenden, L.; Nathan, N.; Wainberg, M.L. What is dissemination and implementation science?: An introduction and opportunities to advance behavioral medicine and public health globally. Int. J. Behav. Med. 2020, 27, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm. Policy Ment. Health 2011, 38, 65–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curran, G.M.; Bauer, M.; Mittman, B.; Pyne, J.M.; Stetler, C. Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Med. Care 2012, 50, 217. [Google Scholar] [CrossRef] [Green Version]
- Kemp, C.G.; Wagenaar, B.H.; Haroz, E.E. Expanding hybrid studies for implementation research: Intervention, implementation strategy, and context. Front. Public Health 2019, 7, 325. [Google Scholar] [CrossRef]
- Landes, S.J.; McBain, S.A.; Curran, G.M. An introduction to effectiveness-implementation hybrid designs. Psychiatry Res. 2020, 283, 112630. [Google Scholar] [CrossRef]
- Bauer, M.S.; Damschroder, L.; Hagedorn, H.; Smith, J.; Kilbourne, A.M. An introduction to implementation science for the non-specialist. BMC Psychol. 2015, 16, 32. [Google Scholar] [CrossRef] [Green Version]
- Damschroder, L.J. Clarity out of chaos: Use of theory in implementation research. Psychiatry Res. 2020, 283, 112461. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, P. Making sense of implementation theories, models and frameworks. Implement. Sci. 2015, 10, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aarons, G.A.; Hurlburt, M.; Horwitz, S.M. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm. Policy Ment. Health 2011, 38, 4–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michie, S.; Johnston, M.; Abraham, C.; Lawton, R.; Parker, D.; Walker, A. Making psychological theory useful for implementing evidence based practice: A consensus approach. Qual. Saf. Health Care 2005, 14, 26–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, K.M.; Brady, T.J.; Lesesne, C.; NCCDPHP Work Group on Translation. An organizing framework for translation in public health: The Knowledge to Action Framework. Prev. Chronic Dis. 2011, 8, A46. [Google Scholar]
- Feldstein, A.C.; Glasgow, R.E. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt. Comm. J. Qual. Patient Saf. 2008, 34, 228–243. [Google Scholar] [CrossRef]
- McCreight, M.S.; Rabin, B.A.; Glasgow, R.E.; Ayele, R.A.; Leonard, C.A.; Gilmartin, H.M.; Frank, J.W.; Hess, P.L.; Burke, R.E.; Battaglia, C.T. Using the Practical, Robust Implementation and Sustainability Model (PRISM) to qualitatively assess multilevel contextual factors to help plan, implement, evaluate, and disseminate health services programs. Transl. Behav. Med. 2019, 9, 1002–1011. [Google Scholar] [CrossRef]
- Moullin, J.C.; Dickson, K.S.; Stadnick, N.A.; Rabin, B.; Aarons, G.A. Systematic review of the Exploration, Preparation, Implementation, Sustainment (EPIS) framework. Implement. Sci. 2019, 14, 1. [Google Scholar] [CrossRef] [Green Version]
- Weiner, B.J.; Lewis, C.C.; Stanick, C.; Powell, B.J.; Dorsey, C.N.; Clary, A.S.; Boynton, M.H.; Halko, H. Psychometric assessment of three newly developed implementation outcome measures. Implement. Sci. 2017, 12, 1–12. [Google Scholar] [CrossRef]
- Luke, D.A.; Calhoun, A.; Robichaux, C.B.; Elliott, M.B.; Moreland-Russell, S. The program sustainability assessment tool: A new instrument for public health programs. Prev. Chronic Dis. 2014, 11, 130184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rabin, B.A.; Purcell, P.; Naveed, S.; Moser, R.P.; Henton, M.D.; Proctor, E.K.; Brownson, R.C.; Glasgow, R.E. Advancing the application, quality and harmonization of implementation science measures. Implement. Sci. 2012, 7, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKibbon, K.A.; Lokker, C.; Wilczynski, N.L.; Ciliska, D.; Dobbins, M.; Davis, D.A.; Haynes, R.B.; Straus, S.E. A cross-sectional study of the number and frequency of terms used to refer to knowledge translation in a body of health literature in 2006: A Tower of Babel? Implement. Sci. 2010, 5, 16. [Google Scholar] [CrossRef] [Green Version]
- Reilly, K.L.; Kennedy, S.; Porter, G.; Estabrooks, P. Comparing, Contrasting, and Integrating Dissemination and Implementation Outcomes Included in the RE-AIM and Implementation Outcomes Frameworks. Front. Public Health 2020, 8, 430. [Google Scholar] [CrossRef] [PubMed]
- Tinc, P.J.; Jenkins, P.; Sorensen, J.A.; Weinehall, L.; Gadomski, A.; Lindvall, K. Key factors for successful implementation of the National Rollover Protection Structure Rebate Program: A correlation analysis using the consolidated framework for implementation research. Scand. J. Work Environ. Health 2020, 46, 85–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- von Thiele Schwarz, U.; Hasson, H.; Lindfors, P. Applying a fidelity framework to understand adaptations in an occupational health intervention. Work 2015, 51, 195–203. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Cooper, B.R. Mixed methods evaluation in dissemination and implementation science. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: New York, NY, USA, 2018; pp. 336–353. [Google Scholar]
- Brownson, R.C.; Kumanyika, S.K.; Kreuter, M.W.; Haire-Joshu, D. Implementation science should give higher priority to health equity. Implement. Sci. 2021, 16, 28. [Google Scholar] [CrossRef]
- Golden, C.A. A Dissemination Strategy to Identify Communities Ready to Implement a Pediatric Weight Management Intervention in Medically Underserved Areas. Prev. Chronic Dis. 2021, 18, E10. [Google Scholar] [CrossRef]
- Wolfenden, L.; Foy, R.; Presseau, J.; Grimshaw, J.M.; Ivers, N.M.; Powell, B.J.; Taljaard, M.; Wiggers, J.; Sutherland, R.; Nathan, N.; et al. Designing and undertaking randomised implementation trials: Guide for researchers. BMJ 2021, 372. [Google Scholar] [CrossRef]
- Powell, B.J.; Beidas, R.S.; Lewis, C.C.; Aarons, G.A.; McMillen, J.C.; Proctor, E.K.; Mandell, D.S. Methods to improve the selection and tailoring of implementation strategies. J. Behav. Health Serv. Res. 2017, 44, 177–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Proctor, E.K.; Powell, B.J.; McMillen, J.C. Implementation strategies: Recommendations for specifying and reporting. Implement. Sci. 2013, 8, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolk, C.L.; Powell, B.J.; Beidas, R.S. Contextual influences and strategies for dissemination and implementation in mental health. Dep. Pap. (Psychiatry) 2015. [Google Scholar] [CrossRef] [Green Version]
- Powell, B.J.; Waltz, T.J.; Chinman, M.J.; Damschroder, L.J.; Smith, J.L.; Matthieu, M.M.; Proctor, E.K.; Kirchner, J.E. A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implement. Sci. 2015, 10, 21. [Google Scholar] [CrossRef] [Green Version]
- Cook, C.R.; Lyon, A.R.; Locke, J.; Waltz, T.; Powell, B.J. Adapting a compilation of implementation strategies to advance school-based implementation research and practice. Prev. Sci. 2019, 20, 914–935. [Google Scholar] [CrossRef]
- Wolfenden, L.; Goldman, S.; Stacey, F.G.; Grady, A.; Kingsland, M.; Williams, C.M.; Wiggers, J.; Milat, A.; Rissel, C.; Bauman, A.; et al. Strategies to improve the implementation of workplace-based policies or practices targeting tobacco, alcohol, diet, physical activity and obesity. Cochrane Database Syst. Rev. 2018, 11. [Google Scholar] [CrossRef]
- Ahonen, E.Q.; Fujishiro, K.; Cunningham, T.; Flynn, M. Work as an inclusive part of population health inequities research and prevention. Am. J. Public Health 2018, 108, 306–311. [Google Scholar] [CrossRef]
- Gaglio, B.; Glasgow, R.E. Evaluation approaches for dissemination and implementation research. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: New York, NY, USA, 2018; pp. 317–334. [Google Scholar]
- Lewis, C.C.; Klasnja, P.; Powell, B.J.; Lyon, A.R.; Tuzzio, L.; Jones, S.; Walsh-Bailey, C.; Weiner, B. From classification to causality: Advancing understanding of mechanisms of change in implementation science. Front. Public Health 2018, 6, 136. [Google Scholar] [CrossRef] [Green Version]
- Grimshaw, J.M.; Eccles, M.P.; Lavis, J.N.; Hill, S.J.; Squires, J.E. Knowledge translation of research findings. Implement. Sci. 2012, 7, 1–17. [Google Scholar] [CrossRef]
- Movsisyan, A.; Arnold, L.; Evans, R.; Hallingberg, B.; Moore, G.; O’Cathain, A.; Pfadenhauer, L.M.; Segrott, J.; Rehfuess, E. Adapting evidence-informed complex population health interventions for new contexts: A systematic review of guidance. Implement. Sci. 2019, 14, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Chambers, D.A.; Glasgow, R.E.; Stange, K.C. The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implement. Sci. 2013, 8, 117. [Google Scholar] [CrossRef] [Green Version]
- Neta, G.; Glasgow, R.E.; Carpenter, C.R.; Grimshaw, J.M.; Rabin, B.A.; Fernandez, M.E.; Brownson, R.C. A framework for enhancing the value of research for dissemination and implementation. Am. J. Public Health 2015, 105, 49–57. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Emmons, K.M. How can we increase translation of research into practice? Types of evidence needed. Annu. Rev. Public Health. 2007, 28, 413–433. [Google Scholar] [CrossRef] [Green Version]
- May, C.R.; Johnson, M.; Finch, T. Implementation, context and complexity. Implement. Sci. 2016, 11, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Henning, R.; Warren, N.; Robertson, M.; Faghri, P.; Cherniack, M.; CPH-NEW Research Team. Workplace health protection and promotion through participatory ergonomics: An integrated approach. Public Health Rep. 2009, 124 (Suppl. 1), 26–35. [Google Scholar] [CrossRef] [Green Version]
- Lemke, M.K. Is the Total Worker Health Program missing its mark?: Integrating complex systems approaches to unify vision and epistemology. J. Occup. Environ. Med. 2021, 63, e304–e307. [Google Scholar] [CrossRef]
- Rabin, B.A.; McCreight, M.; Battaglia, C.; Ayele, R.; Burke, R.E.; Hess, P.L.; Frank, J.W.; Glasgow, R.E. Systematic, multimethod assessment of adaptations across four diverse health systems interventions. Front. Public Health 2018, 6, 102. [Google Scholar] [CrossRef] [PubMed]
- Dissemination & Implementation Models in Health Research & Practice. Available online: https://dissemination-implementation.org/content/plan.aspx (accessed on 2 October 2021).
- Holtrop, J.S.; Estabrooks, P.A.; Gaglio, B.; Harden, S.M.; Kessler, R.S.; King, D.K.; Kwan, B.M.; Ory, M.G.; Rabin, B.A.; Shelton, R.C.; et al. Understanding and applying the RE-AIM framework: Clarifications and resources. J. Clin. Transl. Sci. 2021, 5, e126. [Google Scholar] [CrossRef] [PubMed]
- NIOSH. Research to Practice (r2p). Available online: https://www.cdc.gov/niosh/r2p/default.html (accessed on 2 October 2021).
- NIOSH. Translation Research. Available online: https://www.cdc.gov/niosh/topics/translationresearch/default.html (accessed on 2 October 2021).
- Introduction to Program Evaluation for Public Health Programs: A Self-Study Guide; Centers for Disease Control and Prevention (CDC): Atlanta, GA, USA. Available online: https://www.cdc.gov/eval/guide/introduction/index.htm (accessed on 2 October 2021).
- Granger, B.B. Science of improvement versus science of implementation: Integrating both into clinical inquiry. AACN Adv. Crit. Care 2018, 29, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Khoury, M.J.; Gwinn, M.; Yoon, P.W.; Dowling, N.; Moore, C.A.; Bradley, L. The continuum of translation research in genomic medicine: How can we accelerate the appropriate integration of human genome discoveries into health care and disease prevention? Genet. Med. 2007, 10, 665–674. [Google Scholar] [CrossRef] [Green Version]
- Westfall, J.M.; Mold, J.; Fagnan, L. Practice-based research—“Blue Highways” on the NIH roadmap. JAMA 2007, 297, 403–406. [Google Scholar] [CrossRef]
- Woolf, S.H. The meaning of translational research and why it matters. JAMA 2008, 299, 211–213. [Google Scholar] [CrossRef]
- Dougherty, D.; Conway, P.H. The “3T’s” road map to transform U.S. health care: The “how” of high-quality care. JAMA 2008, 299, 2319–2321. [Google Scholar] [CrossRef] [PubMed]
- Guerin, R.J.; Reichard, A.A.; Derk, S.; Hendricks, K.J.; Menger-Ogle, L.M.; Okun, A.H. Nonfatal occupational injuries to younger workers—United States, 2012–2018. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1204–1209. [Google Scholar] [CrossRef]
- Koehoorn, M.; Breslin, F.C.; Xu, F. Investigating the longer-term health consequences of work-related injuries among youth. J. Adolesc. Health 2008, 43, 466–473. [Google Scholar] [CrossRef] [PubMed]
- Guerin, R.J.; Castillo, D.; Hendricks, K.J.; Howard, J.; Piacentino, J.; Okun, A.H. Preparing the future workforce for safe and healthy employment. Am. J. Public Health 2020, 110, 69–71. [Google Scholar] [CrossRef] [PubMed]
- Runyan, C.W.; Schulman, M.; Dal Santo, J.; Bowling, J.M.; Agans, R.; Ta, M. Work-related hazards and workplace safety of U.S. adolescents employed in the retail and service sectors. Pediatrics 2007, 119, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Zierold, K.M. Teen worker safety training: Methods used, lessons taught, and time spent. New Solut. 2015, 25, 25–41. [Google Scholar] [CrossRef]
- Miara, C.; Gallagher, S.; Bush, D.; Dewey, R. Developing an effective tool for teaching teens about workplace safety. Am. J. Health Educ. 2003, 34, 30–34. [Google Scholar] [CrossRef]
- NIOSH. Promoting Safe Work for Young Workers—A Community-Based Approach; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health: Cincinnati, OH, USA, 1999; DHHS (NIOSH) Publication No. 1999-141.
- NIOSH. Youth@Work—Talking Safety: A Safety and Health Curriculum for Young Workers. Available online: http://www.cdc.gov/niosh/talkingsafety/states/ok/2015-168/default.html (accessed on 2 October 2021).
- Okun, A.H.; Guerin, R.J.; Schulte, P.A. Foundational workplace safety and health competencies for the emerging workforce. J. Saf. Res. 2016, 59, 43–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guerin, R.J.; Toland, M.D.; Okun, A.H.; Rojas-Guyler, L.; Bernard, A.L. Using a modified theory of planned behavior to examine adolescents’ workplace safety and health knowledge, perceptions, and behavioral intention: A structural equation modeling approach. J. Youth Adolesc. 2018, 47, 1595–1610. [Google Scholar] [CrossRef] [PubMed]
- Guerin, R.J.; Okun, A.H.; Barile, J.P.; Emshoff, J.G.; Ediger, M.D.; Baker, D.S. Preparing teens to stay safe and healthy on the job: A multilevel evaluation of the Talking Safety curriculum for middle schools and high schools. Prev. Sci. 2019, 20, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Rohlman, D.S.; Parish, M.; Elliot, D.L.; Montgomery, D.; Hanson, G. Characterizing the needs of a young working population: Making the case for Total Worker Health in an emerging workforce. J. Occup. Environ. Med. 2013, 55, S69–S72. [Google Scholar] [CrossRef] [PubMed]
- Elliot, D.; Rohlman, D.; Parish, M. Focus groups move online: Feasibility of Tumblr use for ehealth curriculum development. JMIR Res. Protoc. 2015, 4. [Google Scholar] [CrossRef]
- Rohlman, D.S.; Parish, M.; Elliot, D.L.; Hanson, G.; Perrin, N. Addressing younger workers’ needs: The Promoting U through Safety and Health (PUSH) trial outcomes. Healthcare 2016, 4, 55. [Google Scholar] [CrossRef] [Green Version]
- Aryal, A.; Parish, M.; Rohlman, D.S. Generalizability of Total Worker Health® online training for young workers. Int. J. Environ. Res. Public Health 2019, 16, 577. [Google Scholar] [CrossRef] [Green Version]
- Baumann, A.A.; Cabassa, L.J.; Stirman, S.W. Adaptation in dissemination and implementation science. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: New York, NY, USA, 2018; pp. 285–300. [Google Scholar]
- Stirman, S.W.; Baumann, A.A.; Miller, C.J. The FRAME: An expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement. Sci. 2019, 14, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Brownson, R.C.; Eyler, A.A.; Harris, J.K.; Moore, J.B.; Tabak, R.G. Getting the word out: New approaches for disseminating public health science. J. Public Health Manag. Pr. 2018, 24, 102–111. [Google Scholar] [CrossRef] [Green Version]
- Huebschmann, A.G.; Leavitt, I.M.; Glasgow, R.E. Making health research matter: A call to increase attention to external validity. Annu. Rev. Public Health 2019, 40, 45–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kessler, R.; Glasgow, R.E. A proposal to speed translation of healthcare research into practice: Dramatic change is needed. Am. J. Prev. Med. 2011, 40, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Piacentino, J.; MacMahon, K.; Schulte, P. Using systematic review in occupational safety and health. Am. J. Ind. Med. 2017, 60, 921–929. [Google Scholar] [CrossRef] [PubMed]
- Miles, A.; Loughlin, M. Models in the balance: Evidence-based medicine versus evidence-informed individualized care. J. Eval. Clin. Pr. 2011, 17, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Knoepke, C.E.; Ingle, M.P.; Matlock, D.D.; Brownson, R.C.; Glasgow, R.E. Dissemination and stakeholder engagement practices among dissemination & implementation scientists: Results from an online survey. PLoS ONE 2019, 14, e0216971. [Google Scholar] [CrossRef] [Green Version]
- Tabak, R.G.; Stamatakis, K.A.; Jacobs, J.A.; Brownson, R.C. What predicts dissemination efforts among public health researchers in the United States? Public Health Rep. 2014, 129, 361–368. [Google Scholar] [CrossRef] [Green Version]
- Beidas, R.S.; Edmunds, J.M.; Marcus, S.C.; Kendall, P.C. Training and consultation to promote implementation of an empirically supported treatment: A randomized trial. Psychiatr. Serv. 2012, 63, 660–665. [Google Scholar] [CrossRef] [Green Version]
- NIOSH. Evaluation Capacity-Building Plan 2021–2025. Available online: https://www.cdc.gov/niosh/programs/review/ecb (accessed on 17 April 2021).
- Proctor, E.K.; Chambers, D.A. Training in dissemination and implementation research: A field-wide perspective. Transl. Behav. Med. 2017, 7, 624–635. [Google Scholar] [CrossRef] [Green Version]
- Baumann, A.A.; Cabassa, L.J. Reframing implementation science to address inequities in healthcare delivery. BMC Health Serv. Res. 2020, 20, 190. [Google Scholar] [CrossRef]
- Flynn, M.A.; Eggerth, D.E.; Keller, B.M.; Check, P. Reaching “hard to reach” workers: Evaluating approaches to disseminate worker safety information via the Mexican consular network. J. Occup. Environ. Hyg. 2021, 18, 180–191. [Google Scholar] [CrossRef]
- Jaramillo, D.; Krisher, L.; Schwatka, N.V.; Tenney, L.; Fisher, G.G.; Clancy, R.L.; Shore, E.; Asensio, C.; Tetreau, S.; Castrillo, M.E.; et al. International Total Worker Health: Applicability to Agribusiness in Latin America. Int. J. Environ. Res. Public Health 2021, 18, 2252. [Google Scholar] [CrossRef] [PubMed]
- NIOSH/ASSE. Overlapping Vulnerabilities: The Occupational Safety and Health of Young Workers in Small Construction Firms; Flynn, M.A., Cunningham, T.R., Guerin, R.J., Keller, B., Chapman, L.J., Hudson, D., Salgado, C., Eds.; NIOSH/ASSE, National Institute for Occupational Safety and Health and American Society of Safety Engineers: Cincinnati, OH, USA, 2015; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2015-178. Available online: https://www.cdc.gov/niosh/docs/2015-178/pdfs/2015-178.pdf?id=10.26616/NIOSHPUB2015178 (accessed on 13 October 2021).
| Characteristics | Implications | TWH Considerations |
|---|---|---|
| Systems Perspective | ||
| Context is critical | Research should focus on and describe context | What are the key circumstances and factors within and outside of the workplace that influence the uptake, implementation, and sustained use of TWH programs? |
| Multilevel complexity needs to be considered | Most problems and interventions are dynamic, multilevel, and complex | What levels of influence (policy/regulatory, community, organizational, managers/supervisors, worksite/team, and individual workers) are addressed? |
| Focus on systems characteristics | More emphasis needed on interrelationships among system elements and system rules | Were there specific resources, values, or missions that drove the success or hindrance of the TWH effort? Are there unintended consequences? |
| Robust, Practical Goals | ||
| Representativeness and reach | Focus on reaching broader segments of the population and those most in need | Of the eligible workers, who participated? What recruitment efforts could be made for more equity and inclusion? |
| Generalizability | Study generalization and replication (or lack of such) across workplace settings | What efforts are made to ensure the TWH intervention can be scaled to other settings and delivered by other staff? |
| Pragmatic and practical | Producing answers to specific questions relevant to stakeholders at reasonable costs | What needs assessments were conducted? How is the fit of the TWH effort with stakeholder needs measured/assessed? Are the costs realistic/feasible? |
| Scalability and sustainability | From the outset, a greater focus on scale-up potential and likelihood of sustainability (designing for dissemination and sustainment [34]) | What are the startup and sustainability resources and costs the setting will need to consider for full institutionalization? What adaptations will need to be made (iteratively) to support continued use of the TWH program and scale-up to other setting/systems? |
| Research Methods to Enhance Relevance | ||
| Rigorous | Identifying and addressing plausible threats to validity in context of questions and a greater focus on replication | What is the best research design to answer the specific TWH question? What are the details necessary for replication? |
| Rapid | Approaches that produce faster answers | What is the current translational lag time? In what ways are research efforts speeding up that process? |
| Adaptive | The best solutions usually evolve over time, as a result of informed hypotheses and iterative mini-tests with feedback | What are the core elements of the TWH effort (things that cannot change) and what things need iterative assessment? How are these core components communicated to those external to the team? How much guidance is provided for adaptation to local context? |
| Integration of methods; triangulation | For greater understanding, integrated quantitative and qualitative methods are often required | Who and what experiences in the TWH effort need to be captured to understand the richer context and outcomes? What are the best methods for this? |
| Relevant | Relevance to stakeholders should be a top priority | Do stakeholders find the TWH effort a high priority, feasible, acceptable, and appropriate? What are strategic ways to obtain unbiased responses? |
| Equitable | All stakeholders and relevant community sectors are represented and engaged | Does the intervention advance/support occupational health equity? Are hard-to-reach and hardly reached worker groups engaged? Are program outcomes equitable? Can the intervention be conducted in settings frequented by and serving disadvantaged populations? Does it unintentionally enhance OSH disparities? |
| Respect for diverse approaches; humility | Different perspectives, goals, methods and approaches are needed. Continuing the same existing approaches will produce the same unsatisfactory results | What about the research is novel, comprehensive, and holistic? How is this communicated to various stakeholders? Are multiple disciplines involved? |
| Tool/Resource | Brief Description |
|---|---|
| Select D&I Theories, Models, and Frameworks (TMFs) | |
| Consolidated Framework for Implementation Research (CFIR) [55] | A widely used D&I framework that considers a range of implementation determinants (i.e., barriers and facilitators). The CFIR comprises five major domains (the intervention, inner and outer settings, the individuals involved, and the implementation process). Within these domains, multiple constructs reflect determinants of implementation. For example, complexity and cost are constructs within the intervention characteristics domain; external policies are a construct in the outer setting domain; culture is a construct within the inner setting domain; planning and engaging are constructs within the process domain; and the characteristics of the individuals involved domain focuses on individual-level constructs such as self-efficacy and knowledge, attitudes, and beliefs about the intervention [55]. |
| RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) framework [8,9] | A widely used D&I framework that includes five key dimensions: Adoption, Reach, Implementation, Effectiveness, and Maintenance. RE-AIM was designed to enhance the quality, efficiency, and public health impact of interventions. Cutting across all five of the RE-AIM implementation outcomes are equity concerns related to the representativeness of those who participate or benefit from evidence-based programs. The RE-AIM framework can be used for intervention planning, evaluation, and (iteratively) guiding adaptations to implementation strategies. |
| Practical, Robust, Implementation, and Sustainability Model (PRISM) [9,59,60]. | An extension of the RE-AIM framework, PRISM considers key contextual factors that influence implementation at multiple socioecological levels. PRISM contextual factors include: the program characteristics from the perspective of organizational and individual recipients, the characteristics of diverse, multilevel recipients of the program, the implementation and sustainability infrastructure, and the external environment. PRISM may be used to guide researchers during the program planning, implementation, evaluation, and dissemination phases. |
| EPIS (Exploration, Planning, Implementation, Sustainment) framework [56,61] | The EPIS framework consists of four phases (Exploration, Planning, Implementation, Sustainment) that align with the implementation process, the identification of outer system and inner organizational contexts, and “bridging and innovation factors” that are concerned with the intervention being implemented and the interaction between outer and inner contexts. |
| Diffusion of innovations theory [31] | A widely used theory that seeks to explain the processes and factors influencing the spread and adoption of innovations through certain channels over time, considering components such as perceived characteristics of the innovation; innovativeness of the adopter; social system(s); individual adoption processes; and the diffusion system. |
| Theoretical Domains Framework (TDF) [57] | A compilation of theories relevant to implementation that resulted from a systematic review of published D&I frameworks. |
| CDC Knowledge to Action (K2A) Framework for Public Health [58] | A framework that can be used to explore how evidence-based interventions are translated into effective (public health) programs and practices. The framework consists of three phases: research, translation, and institutionalization. Under each of the three phases are supporting structures and evaluation. |
| D&I Models in Health: www.dissemination-implementation.org (accessed on 13 October 2021) | A free interactive webtool for the selection of TMFs that can be used for study planning, combining and adapting TMFs, and selecting measurement tools to explore D&I constructs. |
| Examples/Select D&I Measures, Instruments, and Tools | |
| Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM) | Measures by Weiner and colleagues [62] to assess intervention acceptability, appropriateness and feasibility (12 items, four for each construct). |
| The Program Sustainability Assessment Tool (PSAT): https://sustaintool.org/psat/ | A reliable, 40-item instrument from Luke and colleagues [63] with eight domains (5 items per domain) that can be used to assess the capacity for the sustainability of public health programs. |
| The EPIS framework website: https://episframework.com/measures (accessed on 13 October 2021) | Provides examples of and free access to webinars and other quantitative measures that assess constructs for inner (such as individual program adopter characteristics) and outer (such as sociopolitical and economic contexts that influence the process of implementation) contexts [56,61]. |
| The Society for Implementation Research Collaboration Instrument Review Project: https://societyforimplementationresearchcollaboration.org/sirc-instrument-project (accessed on 13 October 2021) | Provides an overview of measures for both implementation outcomes and multilevel contextual domains. This resource requires a membership for access. |
| The National Cancer Institute, Grid-Enabled Measures Database (GEM): https://www.gem-measures.org/Public/Home.aspx (accessed on 13 October 2021) | Houses tools to enhance the quality and harmonization of measures for D&I [64]. |
| The CFIR website: cfirguide.org (accessed on 13 October 2021) | Provides free access to data collection tools based on CFIR constructs [55]. |
| The RE-AIM and PRISM frameworks website: https://www.re-aim.org (accessed on 13 October 2021) | Provides free templates of focus group and one-on-one interview guides for assessing RE-AIM constructs [8,9] before, during, and after program implementation. The website also includes videos, interactive tools, and presentations on PRISM/RE-AIM. |
| Acceptability | Perception among key stakeholders that the TWH program or practice is agreeable or satisfactory |
| Adoption | Agreement among key stakeholders and settings to use a TWH intervention (i.e., “uptake”) |
| Appropriateness | Perceived fit of the TWH intervention for a given context/population/health and safety problem |
| Costs | Resources needed for the uptake, implementation, and sustainment of TWH interventions |
| Feasibility | Extent to which the TWH intervention can be used successfully within a given workplace setting |
| Fidelity | Degree to which a TWH intervention is implemented as intended by program developers |
| Penetration | Extent of integration of a TWH intervention within a workplace, community, or system |
| Reach | Absolute number, proportion, and representativeness of individuals who are willing to participate in a given TWH initiative, intervention, or program, and reasons why or why not |
| Adaptation | Degree to which evidence-based TWH initiatives are modified to better fit with the local context |
| Sustainability | Extent to which a newly implemented TWH intervention is maintained or institutionalized within an organization/workplace |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerin, R.J.; Harden, S.M.; Rabin, B.A.; Rohlman, D.S.; Cunningham, T.R.; TePoel, M.R.; Parish, M.; Glasgow, R.E. Dissemination and Implementation Science Approaches for Occupational Safety and Health Research: Implications for Advancing Total Worker Health. Int. J. Environ. Res. Public Health 2021, 18, 11050. https://doi.org/10.3390/ijerph182111050
Guerin RJ, Harden SM, Rabin BA, Rohlman DS, Cunningham TR, TePoel MR, Parish M, Glasgow RE. Dissemination and Implementation Science Approaches for Occupational Safety and Health Research: Implications for Advancing Total Worker Health. International Journal of Environmental Research and Public Health. 2021; 18(21):11050. https://doi.org/10.3390/ijerph182111050
Chicago/Turabian StyleGuerin, Rebecca J., Samantha M. Harden, Borsika A. Rabin, Diane S. Rohlman, Thomas R. Cunningham, Megan R. TePoel, Megan Parish, and Russell E. Glasgow. 2021. "Dissemination and Implementation Science Approaches for Occupational Safety and Health Research: Implications for Advancing Total Worker Health" International Journal of Environmental Research and Public Health 18, no. 21: 11050. https://doi.org/10.3390/ijerph182111050
APA StyleGuerin, R. J., Harden, S. M., Rabin, B. A., Rohlman, D. S., Cunningham, T. R., TePoel, M. R., Parish, M., & Glasgow, R. E. (2021). Dissemination and Implementation Science Approaches for Occupational Safety and Health Research: Implications for Advancing Total Worker Health. International Journal of Environmental Research and Public Health, 18(21), 11050. https://doi.org/10.3390/ijerph182111050






