Clustering of Physical Activity, Diet and Sedentary Behavior among Youth from Low-, Middle-, and High-Income Countries: A Scoping Review
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Screening Process
2.4. Data Extraction and Synthesis
2.5. Critical Appraisal of Individual Sources of Evidence
3. Results
3.1. Selection of Sources of Evidence
3.2. Characteristics of Sources of Evidence
3.3. Critical Appraisal within Sources of Evidence
3.4. Behavior Measurement
3.5. Analytical Approaches
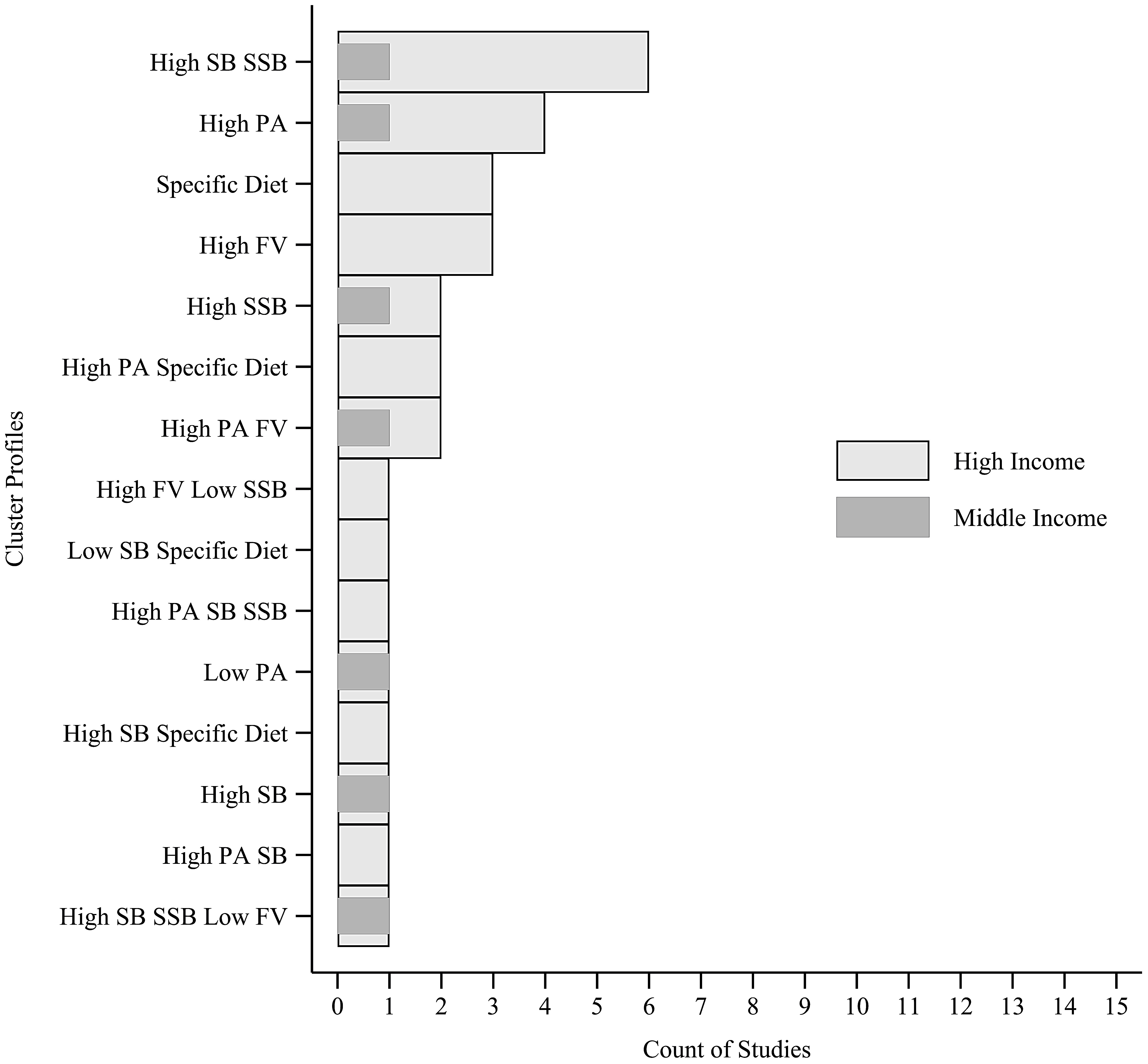
3.6. Cluster Profile
3.7. Cluster Analysis
3.8. Dimensionality Reduction Techniques
4. Discussion
4.1. Risk of Bias
4.2. Studies Characteristics
4.3. Outcomes
4.4. Analysis
4.5. Clusters
4.6. Strengths and Limitations
4.7. Futures Researches
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raychaudhuri, M.; Sanyal, D. Childhood obesity: Determinants, evaluation, and prevention. Indian J. Endocrinol. Metab. 2012, 16, S192–S194. [Google Scholar] [PubMed]
- Ells, L.J.; Rees, K.; Brown, T.; Mead, E.; Al-Khudairy, L.; Azevedo, L.; McGeechan, G.J.; Baur, L.; Loveman, E.; Clements, H.; et al. Interventions for treating children and adolescents with overweight and obesity: An overview of Cochrane reviews. Int. J. Obes. 2018, 42, 1823–1833. [Google Scholar] [CrossRef] [PubMed]
- Weihrauch-Blüher, S.; Kromeyer-Hauschild, K.; Graf, C.; Widhalm, K.; Korsten-Reck, U.; Jödicke, B.; Markert, J.; Müller, M.J.; Moss, A.; Wabitsch, M.; et al. Current guidelines for obesity prevention in childhood and adolescence. Obes. Facts 2018, 11, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. Clustering of diet, physical activity and sedentary behaviour among Australian children: Cross-sectional and longitudinal associations with overweight and obesity. Int. J. Obes. 2015, 39, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Matias, T.S.; Lopes, M.V.V.; de Mello, G.T.; Silva, K.S. Clustering of obesogenic behaviors and association with body image among Brazilian adolescents in the national school-based health survey (PeNSE 2015). Prev. Med. Rep. 2019, 16, 101000. [Google Scholar] [CrossRef] [PubMed]
- Dumuid, D.; Olds, T.; Lewis, L.K.; Martin-Fernández, J.A.; Katzmarzyk, P.T.; Barreira, T.; Broyles, S.T.; Chaput, J.P.; Fogelholm, M.; Hu, G.; et al. Health-related quality of life and lifestyle behavior clusters in school-aged children from 12 countries. J. Pediatr. 2017, 183, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Dumuid, D.; Olds, T.; Martín-Fernández, J.A.; Lewis, L.K.; Cassidy, L.; Maher, C. Academic performance and lifestyle behaviors in Australian school children: A cluster analysis. Health Educ. Behav. 2017, 44, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Gubbels, J.S.; van Assema, P.; Kremers, S.P.J. Physical activity, sedentary behavior, and dietary patterns among children. Curr. Nutr. Rep. 2013, 2, 105–112. [Google Scholar] [CrossRef]
- Kreuter, M.W.; Wray, R.J. Tailored and targeted health communication: Strategies for enhancing information relevance. Am. J. Health Behav. 2003, 27, S227–S232. [Google Scholar] [CrossRef]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. The clustering of diet, physical activity and sedentary behavior in children and adolescents: A review. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 4. [Google Scholar] [CrossRef]
- Miguel-Berges, M.L.; Zachari, K.; Santaliestra-Pasias, A.M.; Mouratidou, T.; Androutsos, O.; Iotova, V.; Galcheva, S.; De Craemer, M.; Cardon, G.; Koletzko, B.; et al. Clustering of energy balance-related behaviours and parental education in European preschool children: The ToyBox study. Br. J. Nutr. 2017, 118, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Ottevaere, C.; Huybrechts, I.; Benser, J.; De Bourdeaudhuij, I.; Cuenca-Garcia, M.; Dallongeville, J.; Zaccaria, M.; Gottrand, F.; Kersting, M.; Rey-López, J.P.; et al. Clustering patterns of physical activity, sedentary and dietary behavior among European adolescents: The HELENA study. BMC Public Health 2011, 11, 328. [Google Scholar] [CrossRef] [PubMed]
- Matias, T.S.; Silva, K.S.; da Silva, J.A.; da Mello, G.T.; de Salmon, J. Clustering of diet, physical activity and sedentary behavior among Brazilian adolescents in the national school-based health survey (PeNSE 2015). BMC Public Health 2018, 18, 1283. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.M.; Ozer, E.M.; Denny, S.; Marmot, M.; Resnick, M.; Fatusi, A.; Currie, C. Adolescence and the social determinants of health. Lancet 2012, 379, 1641–1652. [Google Scholar] [CrossRef]
- Collese, T.S.; De Moraes, A.C.F.; Fernández-Alvira, J.M.; Michels, N.; De Henauw, S.; Manios, Y.; Androutsos, O.; Kafatos, A.; Widhalm, K.; Galfo, M.; et al. How do energy balance-related behaviors cluster in adolescents? Int. J. Public Health 2019, 64, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Seabra, A.F.; Mendonça, D.M.; Thomis, M.A.; Anjos, L.A.; Maia, J.A. Biological and socio-cultural determinants of physical activity in adolescents. Cad. Saúde Pública 2008, 24, 721–736. [Google Scholar] [CrossRef]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- O’Donoghue, G.; Kennedy, A.; Puggina, A.; Aleksovska, K.; Buck, C.; Burns, C.; Cardon, G.; Carlin, A.; Ciarapica, D.; Colotto, M.; et al. Socio-economic determinants of physical activity across the life course: A “DEterminants of DIet and Physical ACtivity” (DEDIPAC) umbrella literature review. PLoS ONE 2018, 13, e0190737. [Google Scholar] [CrossRef]
- Parker, K.E.; Salmon, J.; Costigan, S.A.; Villanueva, K.; Brown, H.L.; Timperio, A. Activity-related behavior typologies in youth: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 44. [Google Scholar] [CrossRef]
- Elgar, F.J.; Pförtner, T.-K.; Moor, I.; De Clercq, B.; Stevens, G.W.J.M.; Currie, C. Socioeconomic inequalities in adolescent health 2002–2010: A time-series analysis of 34 countries participating in the Health Behaviour in School-aged Children study. Lancet 2015, 385, 2088–2095. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.H.; Ciliska, D.; Dobbins, M.; Micucci, S. A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid.-Based Nurs. 2004, 1, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, G.; Panatto, D.; Domnich, A.; Arata, L.; Pammolli, A.; Simi, R.; Giacchi, M.V.; Amicizia, D.; Gasparini, R. Clustering of health-related behaviors among early and mid-adolescents in Tuscany: Results from a representative cross-sectional study. J. Public Health 2018, 40, e25–e33. [Google Scholar] [CrossRef]
- Nuutinen, T.; Lehto, E.; Ray, C.; Roos, E.; Villberg, J.; Tynjälä, J. Clustering of energy balance-related behaviours, sleep, and overweight among Finnish adolescents. Int. J. Public Health 2017, 62, 929–938. [Google Scholar] [CrossRef]
- Veloso, S.M.; Matos, M.G.; Carvalho, M.; Diniz, J.A. Psychosocial factors of different health behaviour patterns in adolescents: Association with overweight and weight control behaviours. J. Obes. 2012, 2012, 852672. [Google Scholar] [CrossRef]
- Platat, C.; Perrin, A.-E.; Oujaa, M.; Wagner, A.; Haan, M.-C.; Schlienger, J.-L.; Simon, C. Diet and physical activity profiles in French preadolescents. Br. J. Nutr. 2006, 8, 501–507. [Google Scholar]
- Yen, L.-L.; Chiu, C.-J.; Wu, W.-C.; Pan, L.-Y. Aggregation of health behaviors among fourth graders in Northern Taiwan. J. Adolesc. Health 2006, 39, 435–442. [Google Scholar] [CrossRef]
- Marttila-Tornio, K.; Ruotsalainen, H.; Miettunen, J.; Männikkö, N.; Kääriäinen, M. Clusters of health behaviours and their relation to body mass index among adolescents in Northern Finland. Scand. J. Caring Sci. 2019, 34, 666–674. [Google Scholar] [CrossRef]
- Kontogianni, M.D.; Farmaki, A.-E.; Vidra, N.; Sofrona, S.; Magkanari, F.; Yannakoulia, M. Associations between lifestyle patterns and body mass index in a sample of Greek children and adolescents. J. Am. Diet. Assoc. 2010, 110, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Androutsos, O.; Moschonis, G.; Mavrogianni, C.; Roma-Giannikou, E.; Chrousos, G.P.; Kanaka-Gantenbein, C.; Manios, Y. Identification of lifestyle patterns, including sleep deprivation, associated with insulin resistance in children: The healthy growth study. Eur. J. Clin. Nutr. 2014, 68, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Azeredo, C.M.; Levy, R.B.; Peres, M.F.T.; Menezes, P.R.; Araya, R. Patterns of health-related behaviours among adolescents: A cross-sectional study based on the National Survey of School Health Brazil 2012. BMJ Open 2016, 6, e011571. [Google Scholar] [CrossRef] [PubMed]
- Busch, V.; Van Stel, H.F.; Schrijvers, A.J.; de Leeuw, J.R. Clustering of health-related behaviors, health outcomes and demographics in Dutch adolescents: A cross-sectional study. BMC Public Health 2013, 13, 1118. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.J.; Crawford, D.A.; Salmon, J.; Campbell, K.; McNaughton, S.A.; Mishra, G.D.; Ball, K. Clustering of obesity-related risk behaviors in children and their mothers. Ann. Epidemiol. 2011, 21, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Cuenca-García, M.; Huybrechts, I.; Ruiz, J.R.; Ortega, F.B.; Ottevaere, C.; González-Gross, M.; Moreno, L.A.; Vicente-Rodríguez, G.; Molnár, D.; Polito, A.; et al. Clustering of multiple lifestyle behaviors and health-related fitness in European adolescents. J. Nutr. Educ. Behav. 2013, 45, 549–557. [Google Scholar] [CrossRef]
- Fernández-Alvira, J.M.; De Bourdeaudhuij, I.; Singh, A.S.; Vik, F.N.; Manios, Y.; Kovacs, E.; Jan, N.; Brug, J.; Moreno, L.A. Clustering of energy balance-related behaviors and parental education in European children: The ENERGY-project. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 5. [Google Scholar] [CrossRef]
- Fleary, S.A. Combined patterns of risk for problem and obesogenic behaviors in adolescents: A latent class analysis approach. J. Sch. Health 2017, 87, 182–193. [Google Scholar] [CrossRef]
- Iannotti, R.J.; Wang, J. Patterns of physical activity, sedentary behavior, and diet in U.S. adolescents. J. Adolesc. Health 2013, 53, 280–286. [Google Scholar] [CrossRef]
- Lioret, S.; Touvier, M.; Lafay, L.; Volatier, J.-L.; Maire, B. Dietary and physical activity patterns in french children are related to overweight and socioeconomic status. J. Nutr. 2008, 138, 101–107. [Google Scholar] [CrossRef]
- Maia, E.G.; Mendes, L.L.; Pimenta, A.M.; Levy, R.B.; Claro, R.M. Cluster of risk and protective factors for obesity among Brazilian adolescents. Int. J. Public Health 2018, 63, 481–490. [Google Scholar] [CrossRef]
- Mandic, S.; Bengoechea, E.G.; Coppell Kirsten, J.; Spence John, C. Clustering of (un)healthy behaviors in adolescents from Dunedin, New Zealand. Am. J. Health Behav. 2017, 41, 266–275. [Google Scholar] [CrossRef]
- De Moraes, A.C.F.; Fernández-Alvira, J.M.; Rendo-Urteaga, T.; Julián-Almárcegui, C.; Beghin, L.; Kafatos, A.; Molnar, D.; De Henauw, S.; Manios, Y.; Widhalm, K.; et al. Effects of clustering of multiple lifestyle-related behaviors on blood pressure in adolescents from two observational studies. Prev. Med. 2016, 82, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Moreira, N.F.; da Veiga, G.V.; Santaliestra-Pasías, A.M.; Androutsos, O.; Cuenca-García, M.; de Oliveira, A.S.D.; Pereira, R.A.; de Moraes, A.B.D.V.; Van den Bussche, K.; Censi, L.; et al. Clustering of multiple energy balance related behaviors is associated with body fat composition indicators in adolescents: Results from the HELENA and ELANA studies. Appetite 2018, 120, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Rodrigo, C.; Gil, Á.; González-Gross, M.; Ortega, R.; Serra-Majem, L.; Varela-Moreiras, G.; Aranceta-Bartrina, J. Clustering of dietary patterns, lifestyles, and overweight among Spanish children and adolescents in the ANIBES study. Nutrients 2016, 8, 11. [Google Scholar] [CrossRef]
- Rodrigues, P.R.M.; Pereira, R.A.; Santana, A.M.S.; Gama, A.; Carvalhal, I.M.; Nogueira, H.; Rosado-Marques, V.; Padez, C. Patterns of lifestyle-related behaviors and parents’ overweight are associated with increased body adiposity in schoolchildren: A cross-sectional study in Portugal. Nutrire 2017, 42, 23. [Google Scholar] [CrossRef]
- Seghers, J.; Rutten, C. Clustering of multiple lifestyle behaviours and its relationship with weight status and cardiorespiratory fitness in a sample of Flemish 11- to 12-year-olds. Public Health Nutr. 2010, 13, 1838–1846. [Google Scholar] [CrossRef]
- Sena, E.D.M.S.; Muraro, A.P.; Rodrigues, P.R.M.; de Paula Fiuza, R.F.; Ferreira, M.G. Risk behaviour patterns for chronic diseases and associated factors among adolescents. Nutr. Hosp. 2017, 34, 914–922. [Google Scholar]
- Spengler, S.; Mess, F.; Mewes, N.; Mensink, G.B.; Woll, A. A cluster-analytic approach towards multidimensional health-related behaviors in adolescents: The MoMo-Study. BMC Public Health 2012, 12, 1128. [Google Scholar] [CrossRef]
- Turner, K.; Dwyer, J.J.M.; Edwards, A.M.; Allison, K.R. Clustering of Specific Health-related Behaviours: Among Toronto Adolescents. Can. J. Diet. Pract. Res. 2011, 72, e155–e160. [Google Scholar] [CrossRef]
- Ferrar, K.; Golley, R. Adolescent diet and time use clusters and associations with overweight and obesity and socioeconomic position. Health Educ. Behav. 2015, 42, 361–369. [Google Scholar] [CrossRef]
- Santaliestra-Pasías, A.M.; Mouratidou, T.; Reisch, L.; Pigeot, I.; Ahrens, W.; Mårild, S.; Molnár, D.; Siani, A.; Sieri, S.; Tornatiris, M.; et al. Clustering of lifestyle behaviours and relation to body composition in European children. The IDEFICS study. Eur. J. Clin. Nutr. 2015, 69, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. Clustering of children’s obesity-related behaviours: Associations with sociodemographic indicators. Eur. J. Clin. Nutr. 2014, 68, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Gubbels, J.S.; Kremers, S.P.; Goldbohm, R.A.; Stafleu, A.; Thijs, C. Energy balance-related behavioural patterns in 5-year-old children and the longitudinal association with weight status development in early childhood. Public Health Nutr. 2012, 15, 1402–1410. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.; Riggs, N.R.; Spruijt-Metz, D.; Chou, C.-P.; Huang, Z.; Pentz, M. Identifying patterns of eating and physical activity in children: A latent class analysis of obesity risk. Obesity 2011, 19, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Laxer, R.E.; Brownson, R.C.; Dubin, J.A.; Cooke, M.; Chaurasia, A.; Leatherdale, S.T. Clustering of risk-related modifiable behaviours and their association with overweight and obesity among a large sample of youth in the COMPASS study. BMC Public Health 2017, 17, 102. [Google Scholar] [CrossRef]
- Berlin, K.S.; Kamody, R.C.; Thurston, I.B.; Banks, G.G.; Rybak, T.M.; Ferry, R.J. Physical activity, sedentary behaviors, and nutritional risk profiles and relations to body mass index, obesity, and overweight in eighth grade. Behav. Med. 2017, 43, 31–39. [Google Scholar] [CrossRef]
- Van der Sluis, M.E.; Lien, N.; Twisk, J.W.; Steenhuis, I.H.; Bere, E.; Klepp, K.I.; Wind, M. Longitudinal associations of energy balance-related behaviours and cross-sectional associations of clusters and body mass index in Norwegian adolescents. Public Health Nutr. 2010, 13, 1716–1721. [Google Scholar] [CrossRef]
- Landsberg, B.; Plachta-Danielzik, S.; Lange, D.; Johannsen, M.; Seiberl, J.; Müller, M.J. Clustering of lifestyle factors and association with overweight in adolescents of the Kiel Obesity Prevention Study. Public Health Nutr. 2010, 13, 1708–1715. [Google Scholar] [CrossRef]
- Magee, C.A.; Caputi, P.; Iverson, D.C. Patterns of health behaviours predict obesity in Australian children: Health profiles and obesity. J. Paediatr. Child Health 2013, 49, 291–296. [Google Scholar] [CrossRef]
- Boone-Heinonen, J.; Gordon-Larsen, P.; Adair, L.S. Obesogenic clusters: Multidimensional adolescent obesity-related behaviors in the U.S. Ann. Behav. Med. 2008, 36, 217–230. [Google Scholar] [CrossRef]
- Hartz, J.; Yingling, L.; Ayers, C.; Adu-Brimpong, J.; Rivers, J.; Ahuja, C.; Powell-Wiley, T.M. Clustering of health behaviors and cardiorespiratory fitness among U.S. Adolescents. J. Adolesc. Health 2018, 62, 583–590. [Google Scholar] [CrossRef]
- Jureša, V.; Musil, V.; Majer, M.; Ivanković, D.; Petrović, D. Behavioral pattern of overweight and obese school children. Coll. Antropol. 2012, 36, 139. [Google Scholar] [CrossRef][Green Version]
- De Souza Dantas, M.; Dos Santos, M.C.; Lopes, L.A.F.; Guedes, D.P.; Guedes, M.R.A.; Oesterreich, S.A. Clustering of excess body weight-related behaviors in a sample of Brazilian adolescents. Nutrients 2018, 10, 1505. [Google Scholar] [CrossRef] [PubMed]
- Bel-Serrat, S.; Mouratidou, T.; Santaliestra-Pasías, A.M.; Iacoviello, L.; Kourides, Y.A.; Marild, S.; Molnár, D.; Reisch, L.; Siani, A.; Stomfai, S.; et al. Clustering of multiple lifestyle behaviours and its association to cardiovascular risk factors in children: The IDEFICS study. Eur. J. Clin. Nutr. 2013, 67, 848–854. [Google Scholar] [CrossRef]
- Gubbels, J.S.; Kremers, S.P.; Stafleu, A.; Goldbohm, R.; de Vries, N.K.; Thijs, C. Clustering of energy balance-related behaviors in 5-year-old children: Lifestyle patterns and their longitudinal association with weight status development in early childhood. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 77. [Google Scholar] [CrossRef] [PubMed]
- Laxer, R.E.; Cooke, M.; Dubin, J.A.; Brownson, R.C.; Chaurasia, A.; Leatherdale, S.T. Behavioural patterns only predict concurrent BMI status and not BMI trajectories in a sample of youth in Ontario, Canada. PLoS ONE 2018, 13, e0190405. [Google Scholar] [CrossRef] [PubMed]
- Spengler, S.; Mess, F.; Schmocker, E.; Woll, A. Longitudinal associations of health-related behavior patterns in adolescence with change of weight status and self-rated health over a period of 6 years: Results of the MoMo longitudinal study. BMC Pediatr. 2014, 14, 242. [Google Scholar] [CrossRef] [PubMed]
- Dumuid, D.; Olds, T.; Lewis, L.K.; Martin-Fernández, J.A.; Barreira, T.; Broyles, S.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Kuriyan, R.; et al. The adiposity of children is associated with their lifestyle behaviours: A cluster analysis of school-aged children from 12 nations: Children’s adiposity relates to their lifestyle behaviours. Pediatr. Obes. 2018, 13, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Pereira, S.; Katzmarzyk, P.; Gomes, T.; Borges, A.; Santos, D.; Souza, M.; Dos Santos, F.K.; Chaves, R.N.; Champagne, C.M.; Barreira, T.V.; et al. Profiling physical activity, diet, screen and sleep habits in portuguese children. Nutrients 2015, 7, 4345–4362. [Google Scholar] [CrossRef]
- Riggs, N.R.; Huh, J.; Chou, C.-P.; Spruijt-Metz, D.; Pentz, M.A. Executive function and latent classes of childhood obesity risk. J. Behav. Med. 2012, 35, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Moschonis, G.; Mavrogianni, C.; Karatzi, K.; Iatridi, V.; Chrousos, G.P.; Lionis, C.; Manios, Y. Increased physical activity combined with more eating occasions is beneficial against dyslipidemias in children. The Healthy Growth Study. Eur. J. Nutr. 2013, 52, 1135–1144. [Google Scholar] [CrossRef]
- Moschonis, G.; Kalliora, A.C.; Costarelli, V.; Papandreou, C.; Koutoukidis, D.; Lionis, C.; Chrousos, G.P.; Manios, Y. Identification of lifestyle patterns associated with obesity and fat mass in children: The Healthy Growth Study. Public Health Nutr. 2014, 17, 614–624. [Google Scholar] [CrossRef]
- Craigie, A.M.; Lake, A.A.; Kelly, S.A.; Adamson, A.J.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef]
- Blass, E.; Anderson, D.; Kirkorian, H.; Pempek, T.; Price, I.; Koleini, M. On the road to obesity: Television viewing increases intake of high-density foods. Physiol. Behav. 2006, 88, 597–604. [Google Scholar] [CrossRef]
- Bellissimo, N.; Pencharz, P.B.; Thomas, S.G.; Anderson, G.H. Effect of television viewing at mealtime on food intake after a glucose preload in boys. Pediatr. Res. 2007, 61, 745–749. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L.; Giacomelli, A.M.; Kent, K.M.; Roemmich, J.N.; Epstein, L.H. Television watching increases motivated responding for food and energy intake in children. Am. J. Clin. Nutr. 2007, 85, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Marsh, S.; Ni Mhurchu, C.; Maddison, R. The non-advertising effects of screen-based sedentary activities on acute eating behaviours in children, adolescents, and young adults. A systematic review. Appetite 2013, 71, 259–273. [Google Scholar] [CrossRef]
- Dennison, B.A.; Edmunds, L.S. The role of television in childhood obesity. Prog. Pediatr. Cardiol. 2008, 25, 191–197. [Google Scholar] [CrossRef]
- Avery, A.; Anderson, C.; McCullough, F. Associations between children’s diet quality and watching television during meal or snack consumption: A systematic review. Matern. Child Nutr. 2017, 13, e12428. [Google Scholar] [CrossRef]
- Parsons, T.J.; Power, C.; Manor, O. Longitudinal physical activity and diet patterns in the 1958 British Birth Cohort. Med. Sci. Sports Exerc. 2006, 38, 547–554. [Google Scholar] [CrossRef]
- Kelishadi, R. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN Study. Bull World Health Organ. 2007, 85, 19–26. [Google Scholar] [CrossRef]
- Pate, R.R.; Heath, G.W.; Dowda, M.; Trost, S.G. Associations between physical activity and other health behaviors in a representative sample of US adolescents. Am. J. Public Health 1996, 86, 1577–1581. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mello, G.T.d.; Lopes, M.V.V.; Minatto, G.; Costa, R.M.d.; Matias, T.S.; Guerra, P.H.; Filho, V.C.B.; Silva, K.S. Clustering of Physical Activity, Diet and Sedentary Behavior among Youth from Low-, Middle-, and High-Income Countries: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 10924. https://doi.org/10.3390/ijerph182010924
Mello GTd, Lopes MVV, Minatto G, Costa RMd, Matias TS, Guerra PH, Filho VCB, Silva KS. Clustering of Physical Activity, Diet and Sedentary Behavior among Youth from Low-, Middle-, and High-Income Countries: A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(20):10924. https://doi.org/10.3390/ijerph182010924
Chicago/Turabian StyleMello, Gabrielli Thais de, Marcus Vinicius Veber Lopes, Giseli Minatto, Rafael Martins da Costa, Thiago Sousa Matias, Paulo Henrique Guerra, Valter Cordeiro Barbosa Filho, and Kelly Samara Silva. 2021. "Clustering of Physical Activity, Diet and Sedentary Behavior among Youth from Low-, Middle-, and High-Income Countries: A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 20: 10924. https://doi.org/10.3390/ijerph182010924
APA StyleMello, G. T. d., Lopes, M. V. V., Minatto, G., Costa, R. M. d., Matias, T. S., Guerra, P. H., Filho, V. C. B., & Silva, K. S. (2021). Clustering of Physical Activity, Diet and Sedentary Behavior among Youth from Low-, Middle-, and High-Income Countries: A Scoping Review. International Journal of Environmental Research and Public Health, 18(20), 10924. https://doi.org/10.3390/ijerph182010924






