Are Public Oral Care Services Evenly Distributed?—Nation-Wide Assessment of the Provision of Oral Care in Japan Using the National Database of Health Insurance Claims
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Acquisition
2.2. Data Analysis
2.2.1. Description for Dental Claim Data
2.2.2. Calculation of the Standardized Claims Data Ratio (SCR)
2.2.3. Geographic Analysis Using Z-Score for Distribution of Oral and Dental Care Services in Secondary Medical Care Area
2.2.4. Associations with the Prefectural Characteristics of Human Resources and Economic Indicator
3. Results
3.1. Distribution of Dental Receipts by Age and Gender
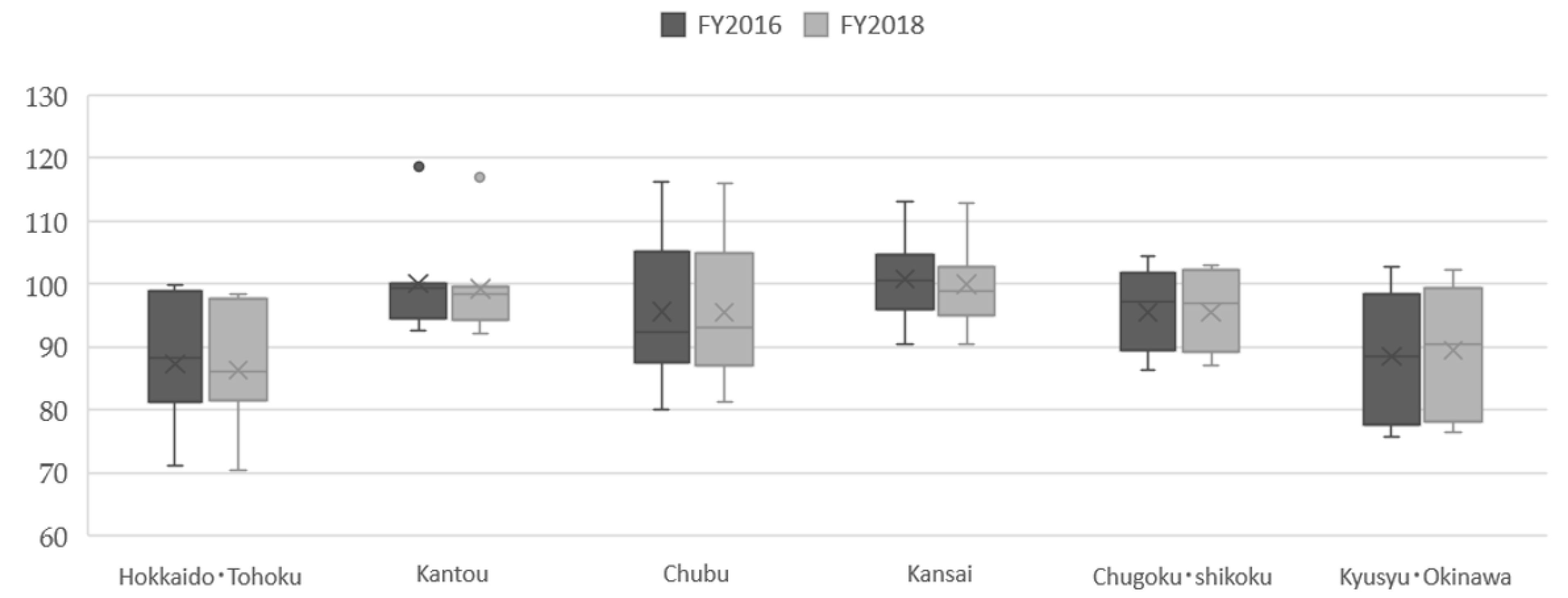
3.2. Standardized Claim Data Ratio (SCR) in Oral and Dental Care Provision
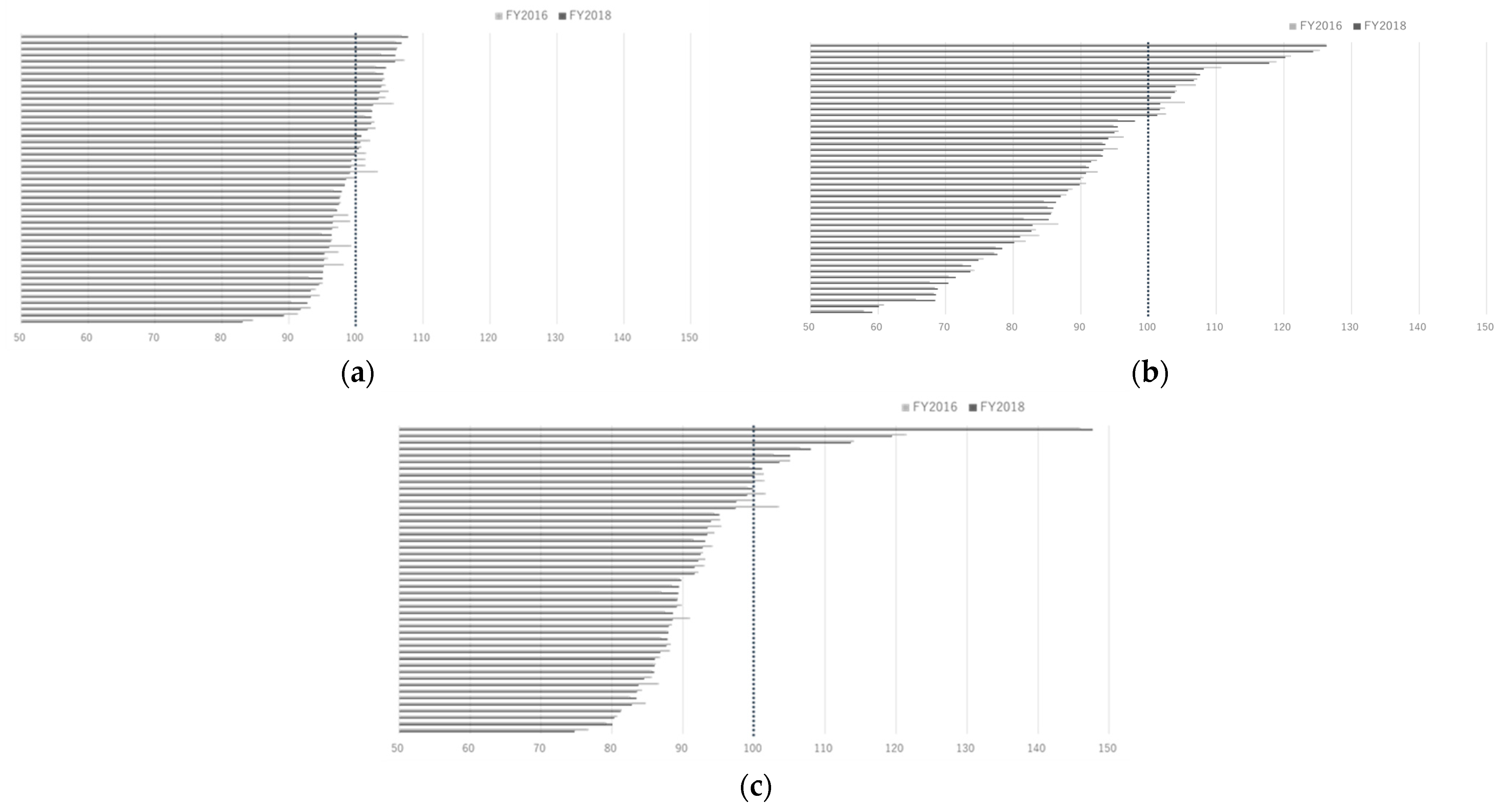
3.3. The SCRs by Disease Codes (Dental Caries, Periodontal Disease and Tooth Loss)
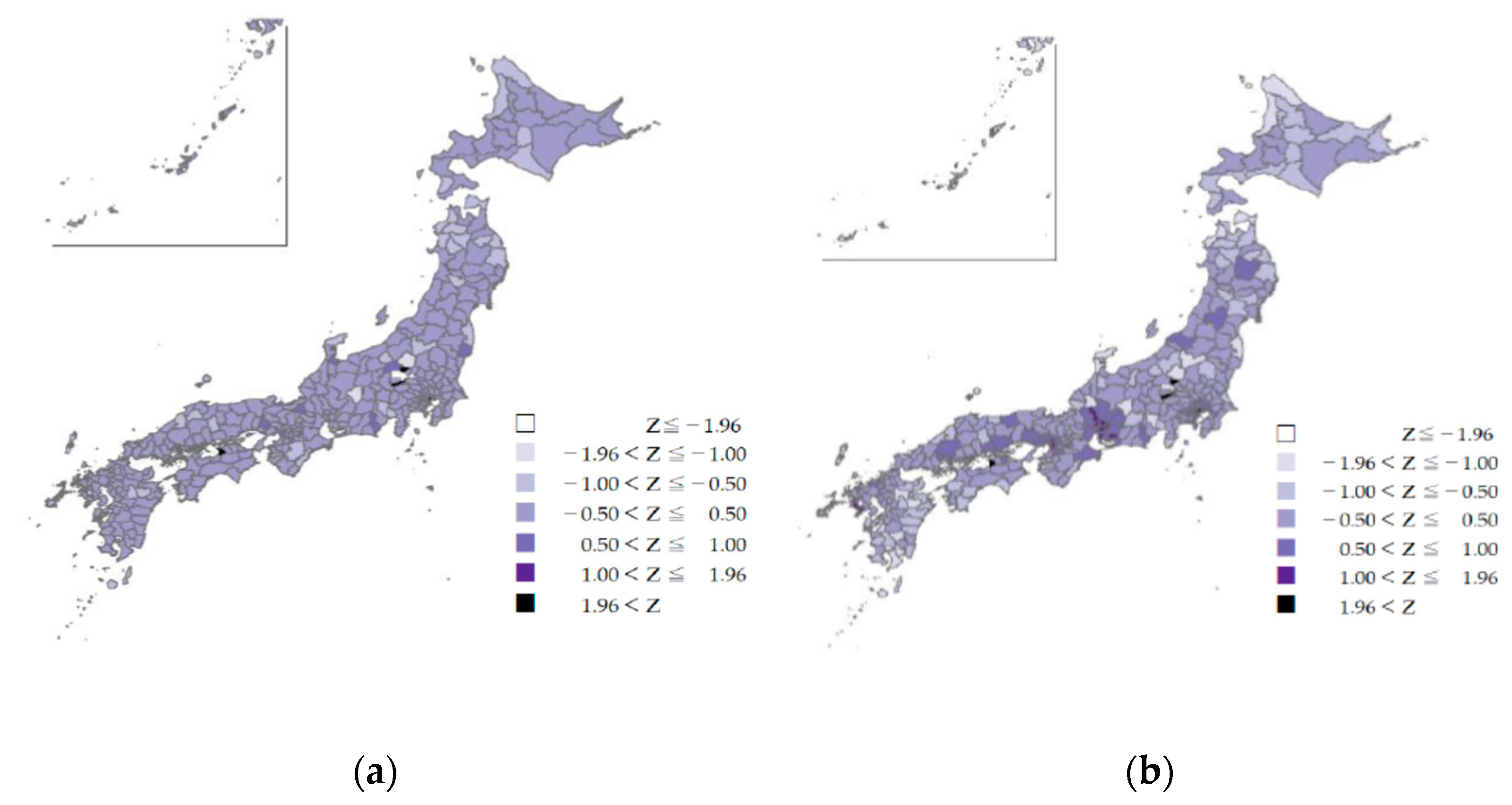
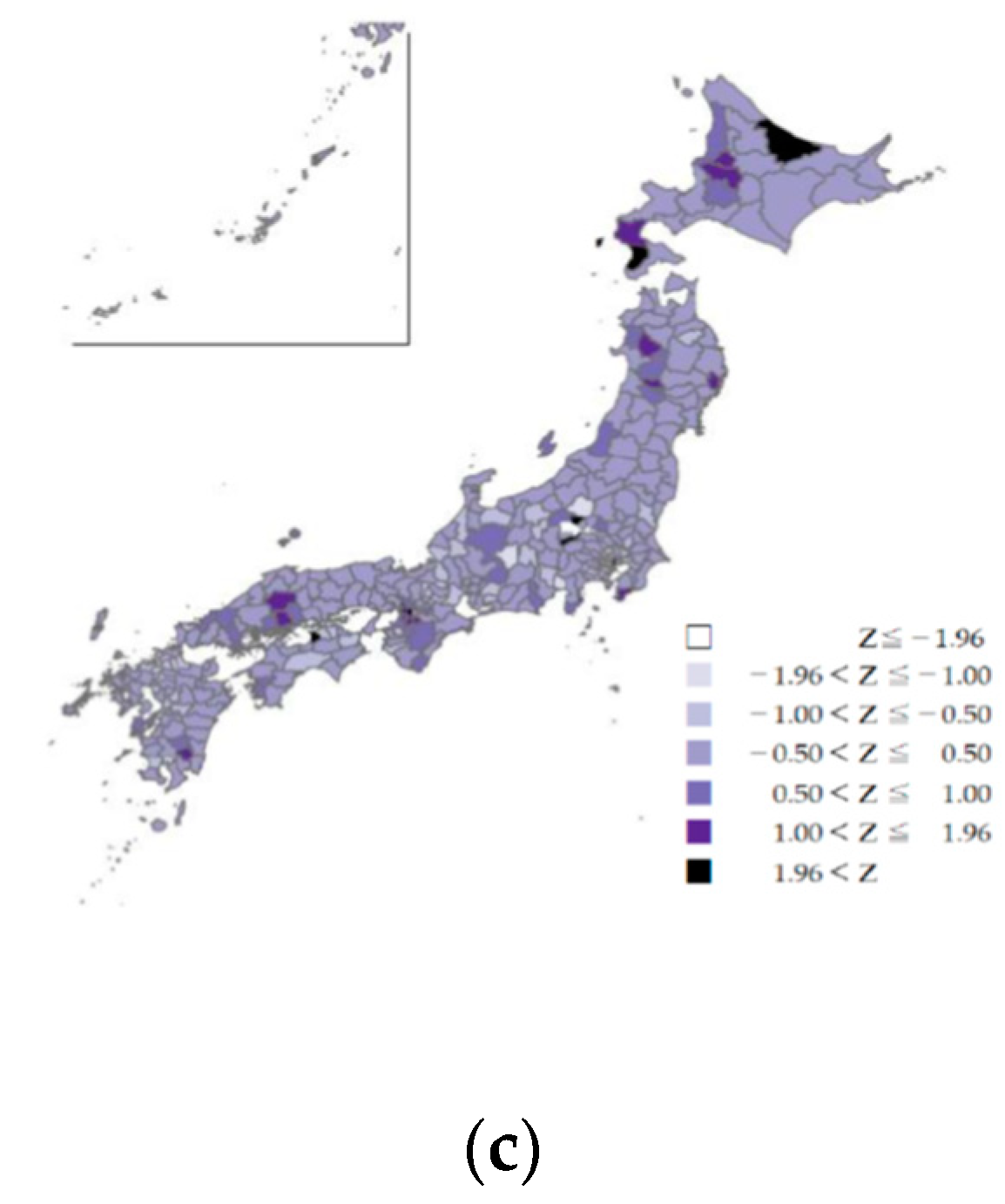
3.4. Z-Scores of Issued Dental Receipts in Secondary Medical Care Areas
3.5. Human Resources of Oral and Dental Care Services and Economic Indicator in Prefectures—Analysis for the SCR of Total Dental Receipt in Regression Model
3.6. Provided Oral Care at Hospitals and Clinics
4. Discussion
4.1. Standardized Claims Data Ratio (SCR) as an Indicator of Oral and Dental Care Provision
4.2. Equitable Access to Oral and Dental Care
4.3. Oral and Dental Care Covered by Health Insurance
4.4. Oral and Dental Care in Aging Societies
4.5. Disparities in Oral Health Care—Global Issues
4.6. Limitation of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Oral Health. Achieving Better Oral Health as Part of The Universal Health Coverage and Noncommunicable Disease Agendas Towards 2030.EB148/8.WHO. Available online: https://apps.who.int/gb/e/e_eb148.html (accessed on 27 July 2021).
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Badewy, R.; Singh, H.; Quiñonez, C.; Singhal, S. Impact of poor oral health on community-dwelling seniors: A scoping review. Health Serv. Insights 2021, 14, 1178632921989734. [Google Scholar] [PubMed]
- Jansson, L.; Lavstedt, S.; Frithiof, L.; Theobald, H. Relationship between oral health and mortality in cardiovascular diseases. J. Clin. Periodontol. 2001, 28, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Lu, B. Prospective association of periodontal disease with cardiovascular and all-cause mortality: NHANES III follow-up study. Atherosclerosis 2011, 218, 536–542. [Google Scholar] [CrossRef]
- Schwahn, C.; Polzer, I.; Haring, R.; Dörr, M.; Wallaschofski, H.; Kocher, T.; Mundt, T.; Holtfreter, B.; Samietz, S.; Völzke, H.; et al. Missing, unreplaced teeth and risk of all-cause and cardiovascular mortality. Int. J. Cardiol. 2013, 167, 1430–1437. [Google Scholar] [CrossRef]
- Ajwani, S.; Mattila, K.J.; Närhi, T.O.; Tilvis, R.S.; Ainamo, A. Oral health status, C-reactive protein and mortality—A 10 year follow-up study. Gerodontology 2003, 20, 32–40. [Google Scholar] [CrossRef]
- Saremi, A.; Nelson, R.G.; Tulloch-Reid, M.; Hanson, R.L.; Sievers, M.L.; Taylor, G.W.; Shlossman, M.; Bennett, P.H.; Genco, R.; Knowler, W.C. Periodontal disease and mortality in type 2 diabetes. Diabetes Care 2005, 28, 27–32. [Google Scholar] [CrossRef]
- Aida, J.; Kondo, K.; Yamamoto, T.; Hirai, H.; Nakade, M.; Osaka, K.; Sheiham, A.; Tsakos, G.; Watt, R.G. Oral health and cancer, cardiovascular, and respiratory mortality of Japanese. J. Dent. Res. 2011, 90, 1129–1135. [Google Scholar] [CrossRef]
- Manabe, K.; Tanji, F.; Tomata, Y.; Zhang, S.; Tsuji, I. Preventive effect of oral self-care on pneumonia death among the elderly with tooth loss: The ohsaki cohort 2006 study. Tohoku J. Exp. Med. 2019, 247, 251–257. [Google Scholar] [CrossRef]
- Iwasaki, M.; Taylor, G.W.; Awano, S.; Yoshida, A.; Kataoka, S.; Ansai, T.; Nakamura, H. Periodontal disease and pneumonia mortality in haemodialysis patients: A 7-year cohort study. J. Clin. Periodontol. 2018, 45, 38–45. [Google Scholar] [CrossRef]
- Ansai, T.; Takata, Y.; Yoshida, A.; Soh, I.; Awano, S.; Hamasaki, T.; Sogame, A.; Shimada, N. Association between tooth loss and orodigestive cancer mortality in an 80-year-old community-dwelling Japanese population: A 12-year prospective study. BMC Public Health 2013, 13, 814. [Google Scholar] [CrossRef]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights (ST/ESA/SER.A/430). 2019. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf (accessed on 10 July 2021).
- Austin, R.S.; Olley, R.C.; Ray-Chaudhuri, A.; Gallagher, J.E. Oral disease prevention for older people. Prim. Dent. Care J. Fac. Gen. Dent. Pract. (UK) 2011, 18, 101–106. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Healthcare System for the Older People. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/iryouhoken/koukikourei/index.html (accessed on 15 August 2021).
- Oral or Dental Care and Treatments Covered by Health Insurance. Available online: https://www.kenpo.gr.jp/opckenpo/contents/shikumi/kyufu/sagaku/teeth.html (accessed on 10 July 2021).
- Ministry of Health, Labour and Welfare. Website for the Provision of the National Database of Health Insurance Claims and Specific Health Checkups. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/iryouhoken/reseputo/index.html (accessed on 10 July 2021).
- Kato, G. History of the secondary use of national database of health insurance claims and specific health checkups of Japan(NDB). Trans. Jpn. Soc. Med. Biol. Eng. 2017, 55, 143–150. [Google Scholar]
- Matsuda, S.; Fujimori, K. The claim database in Japan. Asian Pac. J. Dis. Manag. 2014, 6, 55–59. [Google Scholar] [CrossRef]
- Tsuneishi, M.; Yamamoto, T.; Ishii, T.; Sato, T.; Yamaguchi, T.; Makino, T. Association between number of teeth and medical visit due to aspiration pneumonia in older people using the receipt and health checkup information database. Jpn. J. Geriatr. 2017, 32, 349–356. [Google Scholar]
- Takeuchi, K.; Sato, Y.; Suma, S.; Furuta, M.; Okabe, Y.; Tanaka, A.; Osaka, K.; Yamashita, Y. Associations of oral health status and dental health service utilization with dental and medical expenditures. J. Dent. Health 2017, 67, 160–171. [Google Scholar]
- Kodama, T.; Ida, Y.; Miura, H. A Nationwide survey on working hours and working environment among hospital dentists in Japan. Int. J. Environ. Res. Public Health 2020, 17, 9048. [Google Scholar] [CrossRef]
- Miura, H.; Tano, R.; Oshima, K.; Usui, Y. Analysis of factors related to working status of dental hygienists in Japan. Int. J. Environ. Res. Public Health 2021, 18, 1025. [Google Scholar] [CrossRef] [PubMed]
- Oshima, K. Current status of supply of and demand for dental technicians in Japan: Evaluation and countermeasures against the decrease in the number of dental technicians. Jpn. Dent. Sci. Rev. 2021, 57, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Guidelines for the Provision of Information on Medical Receipts and Specified Medical Examinations. Ministry of Health, Labour and Welfare. Available online: https://www.mhlw.go.jp/stf/shingi2/0000135204.html (accessed on 10 July 2021).
- Ministry of Health, Labours and Welfare. Coding Names of Dental Diseases (Shika-Syoubyou). The Third NDB Open Data. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177221_00002.html (accessed on 10 July 2021).
- Matsuda, S.; Fujimori, K.; Fushimi, K.; Ishikawa, K.B.; Ikeda, S. An analysis of the current state of home care in Japan using the Standardized Claim Ratio (SCR). Rev. Jpn. Soc. Health Support Sci. 2018, 3, 1–10. (In Japanese) [Google Scholar]
- Chapter V Ensuring the Medical Care Delivery System. Medical Care Act. Amendment of Act No. 79 of 2018. Available online: http://www.japaneselawtranslation.go.jp/law/detail/?ft=1&re=01&dn=1&x=36&y=10&co=01&ia=03&ja=04&ky=%E5%8C%BB%E7%99%82%E6%B3%95&page=6 (accessed on 10 July 2021).
- Ministry of Health, Labours and Welfare. Statistics of Physicians, Dentists and Pharmacists. Available online: https://www.mhlw.go.jp/english/database/db-hss/spdp.html (accessed on 10 July 2021).
- Ministry of Health, Labours and Welfare. Report on Public Health Administration and Services. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/eisei/18/ (accessed on 10 July 2021).
- Ministry of Health, Labours and Welfare. Survey of Medical Institutions. Available online: https://www.mhlw.go.jp/toukei/list/79-1a.html (accessed on 10 July 2021).
- Cabinet Office. Prefectural Accounts. Prefectural income per capita. Available online: https://www.esri.cao.go.jp/jp/sna/data/data_list/kenmin/files/contents/main_2018.html (accessed on 10 July 2021).
- Ministry of Health, Labour and Welfare. The Role of NDB and Long-Term Care DB and Their Analysis Infrastructure. In Proceedings of the 1st Expert Meeting on Analysis Infrastructure for Medical and Long-term Care Data, Tokyo, Japan, 16 May 2018. [Google Scholar]
- Folayan, M.O.; Tantawi, M.E.; Virtanen, J.I.; Feldens, C.A.; Rashwan, M.; Kemoli, A.M.; Villena, R.; Al-Batayneh, O.B.; Amalia, R.; Gaffar, B.; et al. An ecological study on the association between universal health service coverage index, health expenditures, and early childhood caries. BMC Oral Health 2021, 21, 126. [Google Scholar]
- Akhmedova, Z.R.; Butova, V.G.; Umarova, K.V.; Zherebtsov, A.Y.; Shevchenko, O.V. Monitoring the implementation of the compulsory health insurance program for the prevention of dental diseases. Stomatologiia 2021, 100, 25–29. [Google Scholar] [CrossRef]
- Choi, J.S. Has the health insurance coverage of scaling contributed positively to periodontal health in korea? Int. J. Environ. Res. Public Health 2020, 17, 8537. [Google Scholar] [CrossRef]
- Idon, P.I.; Sotunde, O.A.; Ogundare, T.O.; Yusuf, J.; Makanjuola, J.O.; Mohammed, A.; Igweagu, C.E.; Alalade, O. Access to root canal treatment in a Nigerian sub-population: Assessment of the effect of dental health insurance. Afr. Health Sci. 2021, 21, 470–477. [Google Scholar] [CrossRef]
- Kieffer, E.C.; Goold, S.D.; Buchmueller, T.; Nalliah, R.; Beathard, E.; Kirch, M.A.; Solway, E.; Tipirneni, R.; Clark, S.J.; Haggins, A.N.; et al. Beneficiaries’ perspectives on improved oral health and its mediators after medicaid expansion in Michigan: A mixed methods study. J. Public Health Dent. 2021, 1–11. [Google Scholar] [CrossRef]
- Kim, N.H.; Jung, S.H.; Kawachi, I. Did expanded dental insurance reduce out-of-pocket expenditures on dental care among older adults in Korea? Interrupted Time-Series Analysis. Int. J. Environ. Res. Public Health 2021, 18, 3003. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Yao, N.A. socio-economic disparities in dental health and dental care utilisation among older Chinese. Int. Dent. J. 2021, 71, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Japanese Society for Oral Health. Oral Health Association of Japan edit. Report on the survey of dental diseases FY 2016 (Japanese). Available online: https://www.mhlw.go.jp/toukei/list/62-28.html (accessed on 10 July 2021).
- John, V.; Alqallaf, H.; De Bedout, T. Periodontal disease and systemic diseases: An update for the clinician. J. (Indiana Dent. Assoc.) 2016, 95, 16–23. [Google Scholar]
- Carrizales-Sepúlveda, E.F.; Ordaz-Farías, A.; Vera-Pineda, R.; Flores-Ramírez, R. Periodontal disease, systemic inflammation and the risk of cardiovascular disease. Heart Lung Circ. 2018, 27, 1327–1334. [Google Scholar] [CrossRef] [PubMed]
- Liccardo, D.; Cannavo, A.; Spagnuolo, G.; Ferrara, N.; Cittadini, A.; Rengo, C.; Rengo, G. Periodontal disease: A risk factor for diabetes and cardiovascular disease. Int. J. Mol. Sci. 2019, 20, 1414. [Google Scholar] [CrossRef] [PubMed]
- Priyamvara, A.; Dey, A.K.; Bandyopadhyay, D.; Katikineni, V.; Zaghlol, R.; Basyal, B.; Barssoum, K.; Amarin, R.; Bhatt, D.L.; Lavie, C.J. Periodontal inflammation and the risk of cardiovascular disease. Curr. Atheroscler. Rep. 2020, 22, 28. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, M.; Graziani, F.; D’Aiuto, F. Periodontal therapy and cardiovascular risk. Periodontol. 2000 2020, 83, 107–124. [Google Scholar] [CrossRef]
- Roca-Millan, E.; González-Navarro, B.; Sabater-Recolons, M.M.; Marí-Roig, A.; Jané-Salas, E.; López-López, J. Periodontal treatment on patients with cardiovascular disease: Systematic review and meta-analysis. Med. Oral Patol. Oral Y Cir. Bucal 2018, 23, e681–e690. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Marco Del Castillo, A.; Jepsen, S.; Gonzalez-Juanatey, J.R.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef]
- Cho, M.J.; Kim, Y.S.; Park, E.Y.; Kim, E.K. Association between periodontal health and stroke: Results from the 2013–2015 korea national health and nutrition examination survey (KNHANES). J. Dent. Sci. 2021, 16, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Al-Nasser, L.; Lamster, I.B. Prevention and management of periodontal diseases and dental caries in the older adults. Periodontol. 2000 2020, 84, 69–83. [Google Scholar] [CrossRef]
- Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [CrossRef]
- Hosseinpoor, A.R.; Itani, L.; Petersen, P.E. Socio-economic inequality in oral healthcare coverage: Results from the World Health Survey. J. Dent. Res. 2012, 91, 275–281. [Google Scholar] [CrossRef]
- OECD. Health at a Glance; OECD: Paris, France, 2017. [Google Scholar]
- van der Wouden, P.; den Dekker, J.; van der Heijden, G. Costs and financing of oral healthcare in the Netherlands. Ned. Tijdschr. Voor Tandheelkd. 2019, 126, 335–340. [Google Scholar] [CrossRef]
- Mouradian, W.E.; Wehr, E.; Crall, J.J. Disparities in children’s oral health and access to dental care. JAMA 2000, 284, 2625–2631. [Google Scholar] [CrossRef]
- Kim, J.; Choi, Y.; Park, S.; Kim, J.L.; Lee, T.H.; Cho, K.H.; Park, E.C. Disparities in the experience and treatment of dental caries among children aged 9–18 years: The cross-sectional study of Korean National Health and Nutrition Examination Survey (2012–2013). Int. J. Equity Health 2016, 15, 88. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ito, K.; Cable, N.; Yamamoto, T.; Suzuki, K.; Kondo, K.; Osaka, K.; Tsakos, G.; Watt, R.G.; Aida, J. Wider dental care coverage associated with lower oral health inequalities: A comparison study between Japan and England. Int. J. Environ. Res. Public Health 2020, 17, 5539. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Wu, Q.; Bell, R.A.; Wright, W.G.; Garcia, R.I.; Quandt, S.A. Trends in use of dental care provider types and services in the United States in 2000–2016: Rural-urban comparisons. J. Am. Dent. Assoc. (1939) 2020, 151, 596–606. [Google Scholar] [CrossRef] [PubMed]

| Fiscal Year | FY 2016 | FY 2018 | ||||||
|---|---|---|---|---|---|---|---|---|
| Prefectural Characteristics | Mean | Std. Dev. | Min | Max | Mean | Std. Dev. | Min | Max |
| SCR of total number of receipts | 94.53 | 10.28 | 71.24 | 118.52 | 94.30 | 9.98 | 70.49 | 116.87 |
| Number of dentists § | 2160.7 | 2756.4 | 340 | 16,107 | 2165.5 | 2757.0 | 341 | 16,023 |
| Number of dental hygienist | 2634.7 | 2453.7 | 698 | 12,952 | 2821.9 | 2638.7 | 734 | 13,720 |
| Number of dental technician | 737.0 | 581.0 | 236 | 3013 | 733.4 | 594.7 | 230 | 3130 |
| Number of dental laboratory | 444.8 | 408.9 | 73 | 1846 | 446.9 | 407.1 | 78 | 1808 |
| Number of dental clinics | 1467.0 | 1855.0 | 257 | 10,658 | 1460.0 | 1854.0 | 260 | 10,672 |
| Prefectural income (JY) | 9,043,117 | 12,300,000 | 1,350,373 | 73,600,000 | 9,295,932 | 12,600,000 | 1,409,584 | 74,800,000 |
| Prefectural population | 2,700,697 | 2,742,348 | 569,554 | 13,600,000 | 2,690,280 | 2,766,906 | 560,397 | 13,800,000 |
| (Per 1000 people) | ||||||||
| Dentists | 0.73 | 0.13 | 0.55 | 1.18 | 0.74 | 0.13 | 0.55 | 1.16 |
| Dental hygienist | 1.06 | 0.22 | 0.67 | 1.60 | 1.13 | 0.23 | 0.73 | 1.68 |
| Dental technician | 0.32 | 0.10 | 0.16 | 0.61 | 0.3 | 0.10 | 0.15 | 0.62 |
| Dental laboratory | 0.17 | 0.03 | 0.10 | 0.25 | 0.17 | 0.03 | 0.10 | 0.25 |
| Dental clinics | 0.50 | 0.07 | 0.38 | 0.77 | 0.50 | 0.07 | 0.39 | 0.77 |
| Prefectural income per capita Ψ | 2.92 | 0.48 | 2.37 | 5.40 | 3.03 | 0.47 | 2.47 | 5.41 |
| (Numbers Per 1000 People) | Dentists | Dental Hygienist | Dental Technician | Dental Clinics | Dental Laboratory | Income Per Capita Ψ |
|---|---|---|---|---|---|---|
| SCR | 0.522 *** | 0.111 | −0.419 * | 0.501 *** | 0.054 | 0.399 ** |
| Dentists | 1.0 | 0.241 | −0.140 | 0.799 *** | 0.376 ** | 0.104 |
| Dental hygienist | 1.0 | 0.399 * | 0.2683 (p = 0.068) | 0.242 | −0.360 * | |
| Dental technician | 1.0 | −0.267 (p = 0.069) | 0.206 | −0.281 (p = 0.056) | ||
| Dental clinics | 1.0 | 0.357 * | 0.138 |
| Model 1 | (R2 = 0.4658, adj-R2 = 0.4285) | 95% CI | |||||
| Coef. | Std. Err. | t | p | low | high | vif | |
| Dentists | 32.82 | 9.30 | 3.53 | 0.001 | 14.07 | 51.57 | 1.28 |
| Dental technician | −21.86 | 11.33 | −1.93 | 0.06 | −44.72 | 0.99 | 1.21 |
| Prefectural income per capita | 6.48 | 2.69 | 2.41 | 0.020 | 1.07 | 11.90 | 1.07 |
| const. | 57.75 | 9.53 | 6.06 | <0.001 | 38.52 | 76.97 | |
| Model 1_a | (R2 = 0.5107, adj-R2 = 0.4641) | 95% CI | |||||
| Coef. | Std. Err. | t | p | low | high | vif | |
| Dentists | 36.85 | 9.23 | 3.99 | <0.001 | 18.22 | 55.49 | 1.27 |
| Dental technician | −20.68 | 10.99 | −1.88 | 0.067 | −42.86 | 1.50 | 1.07 |
| Prefectural income per capita | 10.40 | 3.28 | 3.17 | 0.003 | 3.78 | 17.01 | 1.97 |
| Dentist × Prefectural income per capita § | −19.52 | 9.94 | −1.96 | 0.056 | −39.59 | 0.54 | 2.03 |
| const. | 101.46 | 3.71 | 27.38 | <0.001 | 93.98 | 108.94 | |
| Model 2 | (R2 = 0.3939, adj-R2 = 0.3516) | 95% CI | |||||
| Coef. | Std. Err. | t | p | low | high | vif | |
| Dental clinics | 57.03 | 21.36 | 2.67 | 0.011 | 13.97 | 100.10 | 1.43 |
| Dental laboratory | 13.12 | 39.32 | 0.33 | 0.74 | −66.19 | 92.42 | 1.06 |
| Prefectural income per capita | 7.21 | 2.99 | 2.41 | 0.02 | 1.19 | 13.24 | 1.39 |
| const. | 41.94 | 11.28 | 3.72 | 0.001 | 19.18 | 64.69 | |
| Model 2_a | (R2 = 0.4736, adj-R2 = 0.4234) | 95% CI | |||||
| Coef. | Std. Err. | t | p | low | high | vif | |
| Dental clinics | 85.91 | 23.17 | 3.71 | 0.001 | 39.16 | 132.67 | 1.89 |
| Dental laboratory | −31.92 | 41.16 | −0.78 | 0.442 | −114.98 | 51.15 | 1.30 |
| Prefectural income per capita | 12.41 | 3.49 | 3.56 | 0.001 | 5.37 | 19.45 | 2.13 |
| Clinics × Prefectural income per capita § | −50.09 | 19.87 | 3.56 | 0.016 | −90.18 | −9.99 | 2.98 |
| const. | 100.57 | 7.31 | 13.76 | <0.001 | 85.82 | 76.97 | |
| Model 3 | (R2 = 0.5296, adj-R2 = 0.4813) | 95% CI | |||||
| Coef. | Std. Err. | p | low | high | vif | ||
| Dentists | 21.89 | 9.99 | 2.19 | 0.034 | 1.74 | 42.04 | 1.54 |
| Dental hygienist | 14.26 | 6.06 | 2.35 | 0.023 | 2.03 | 26.49 | 1.69 |
| Dental technician | −34.77 | 12.09 | −2.88 | 0.006 | −59.17 | −10.38 | 1.31 |
| Prefectural income per capita | 8.96 | 2.78 | 3.22 | 0.002 | 3.35 | 14.56 | 1.52 |
| const. | 46.43 | 10.41 | 4.46 | <0.001 | 25.43 | 67.44 | |
| Model 3_a | (R2 = 0.5799, adj-R2 = 0.5287) | 95% CI | |||||
| Coef. | Std. Err. | p | low | high | vif | ||
| Dentists | 25.28 | 9.74 | 2.60 | 0.013 | 5.62 | 44.95 | 1.60 |
| Dental hygienist | 15.29 | 5.88 | 2.60 | 0.013 | 3.41 | 27.16 | 1.74 |
| Dental technician | −34.21 | 11.55 | −2.96 | 0.005 | −57.53 | −10.89 | 1.35 |
| Prefectural income per capita | 13.26 | 3.27 | 4.06 | <0.001 | 6.67 | 19.86 | 2.29 |
| Dentists × Prefectural income per capita § | −20.22 | 9.33 | −2.17 | 0.036 | −39.06 | −1.38 | 1.97 |
| const. | 88.57 | 6.05 | 14.63 | <0.001 | 76.34 | 100.80 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kodama, T.; Ida, Y.; Oshima, K.; Miura, H. Are Public Oral Care Services Evenly Distributed?—Nation-Wide Assessment of the Provision of Oral Care in Japan Using the National Database of Health Insurance Claims. Int. J. Environ. Res. Public Health 2021, 18, 10850. https://doi.org/10.3390/ijerph182010850
Kodama T, Ida Y, Oshima K, Miura H. Are Public Oral Care Services Evenly Distributed?—Nation-Wide Assessment of the Provision of Oral Care in Japan Using the National Database of Health Insurance Claims. International Journal of Environmental Research and Public Health. 2021; 18(20):10850. https://doi.org/10.3390/ijerph182010850
Chicago/Turabian StyleKodama, Tomoko, Yusuke Ida, Katsuo Oshima, and Hiroko Miura. 2021. "Are Public Oral Care Services Evenly Distributed?—Nation-Wide Assessment of the Provision of Oral Care in Japan Using the National Database of Health Insurance Claims" International Journal of Environmental Research and Public Health 18, no. 20: 10850. https://doi.org/10.3390/ijerph182010850
APA StyleKodama, T., Ida, Y., Oshima, K., & Miura, H. (2021). Are Public Oral Care Services Evenly Distributed?—Nation-Wide Assessment of the Provision of Oral Care in Japan Using the National Database of Health Insurance Claims. International Journal of Environmental Research and Public Health, 18(20), 10850. https://doi.org/10.3390/ijerph182010850








