Associations between Temperature and Influenza Activity: A National Time Series Study in China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Influenza Epidemiological and Virological Data
2.2. Meteorological Data
2.3. Generalized Additive Models (GAMs)
3. Results
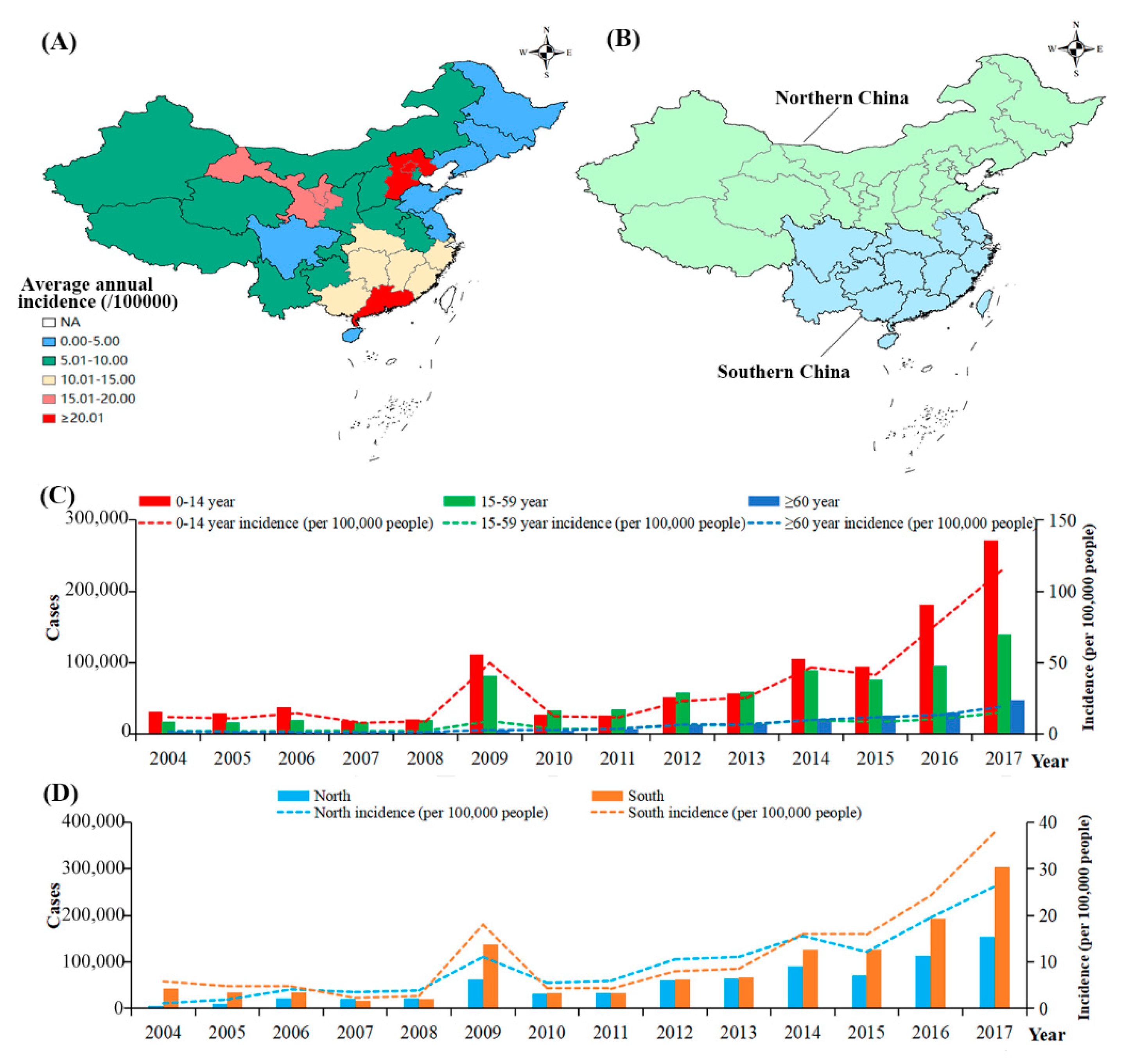
3.1. The Incidences of Influenza in China
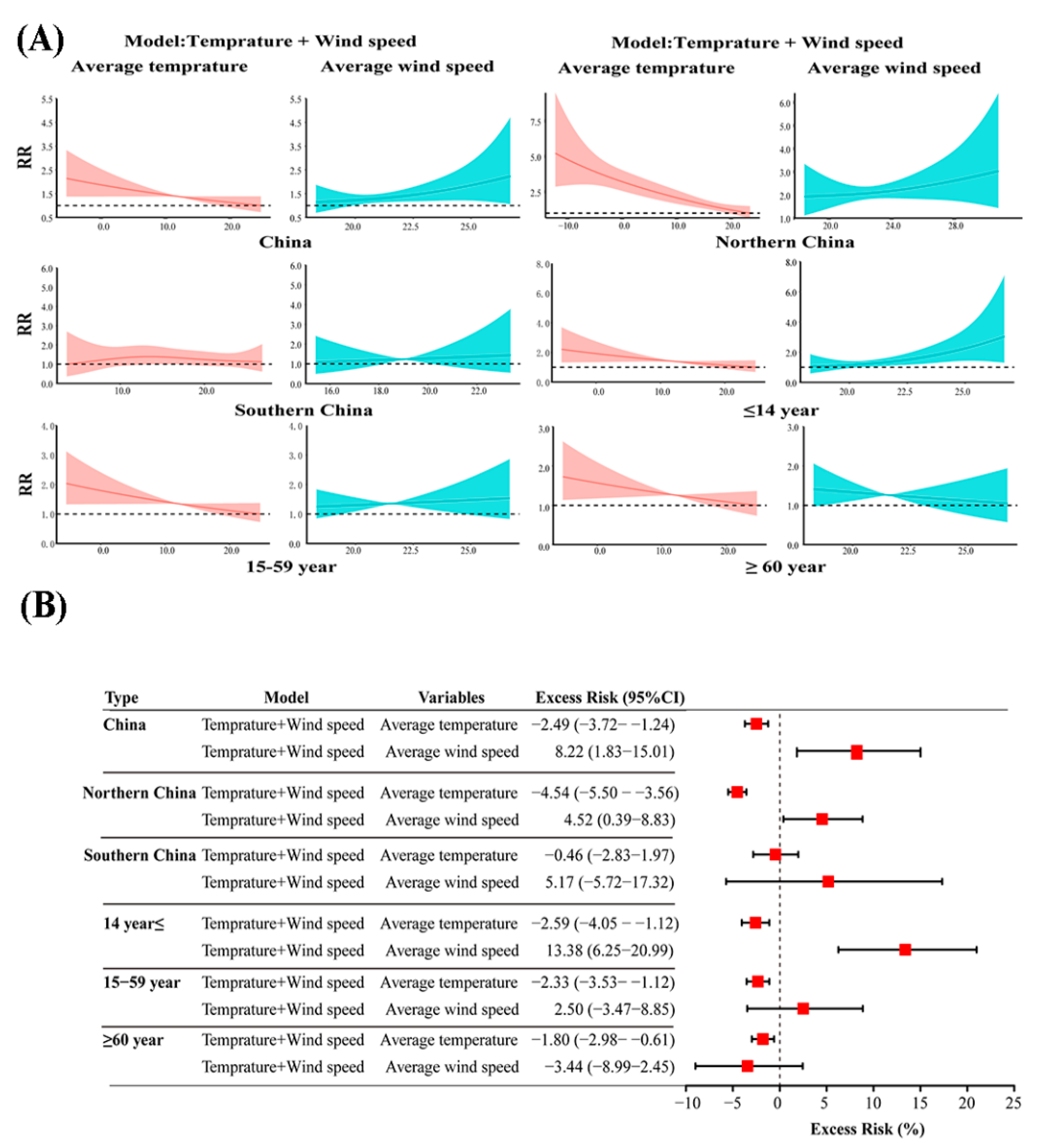
3.2. The Exposure–Response and Excess Risk of Monthly AT to the Incidence of Influenza
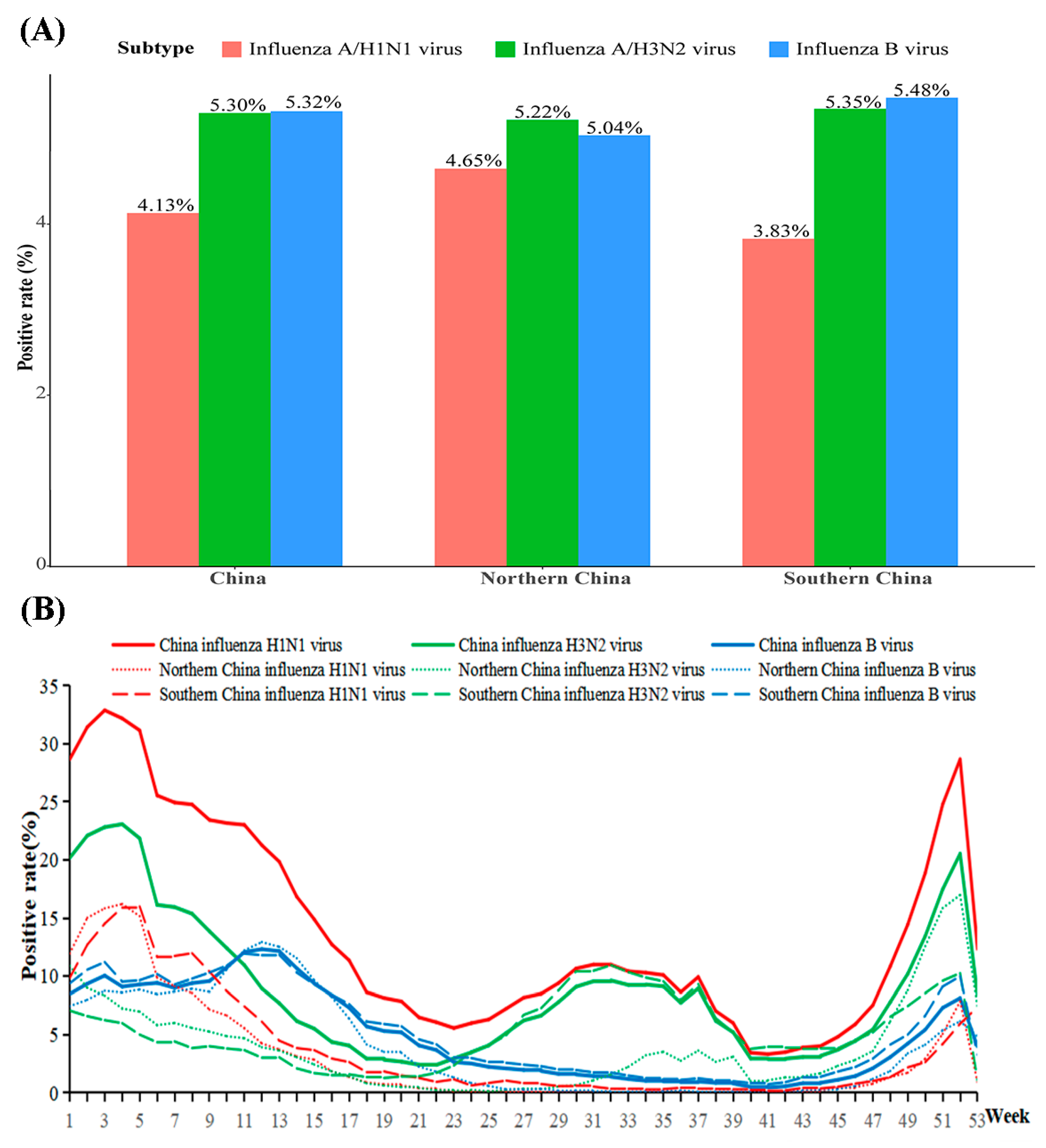
3.3. The Activity of Influenza Virus in China
3.4. The Exposure–Response and Excess Risk of Weekly AT to the Positive Rate of Influenza Virus
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, X.; Zhang, B.; Wang, Y.; Haymour, H.S.; Zhang, F.; Xu, L.C.; Srinivasarao, M.; Low, P.S. A universal dual mechanism immunotherapy for the treatment of influenza virus infections. Nat. Commun. 2020, 11, 5597. [Google Scholar] [CrossRef]
- World Health Organization. Up to 650,000 People Die of Respiratory Diseases Linked to Seasonal Flu Each Year. 2018. Available online: https://www.who.int/news/item/13-12-2017-up-to-650-000-people-die-of-respiratory-diseases-linked-to-seasonal-flu-each-year (accessed on 1 July 2021).
- von Klot, S.; Zanobetti, A.; Schwartz, J. Influenza epidemics, seasonality, and the effects of cold weather on cardiac mortality. Environ. Health 2012, 11, 74. [Google Scholar] [CrossRef] [Green Version]
- Soebiyanto, R.P.; Gross, D.; Jorgensen, P.; Buda, S.; Bromberg, M.; Kaufman, Z.; Prosenc, K.; Socan, M.; Vega Alonso, T.; Widdowson, M.A.; et al. Associations between Meteorological Parameters and Influenza Activity in Berlin (Germany), Ljubljana (Slovenia), Castile and León (Spain) and Israeli Districts. PLoS ONE 2015, 10, e0134701. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Rao, Y.; Sun, Q.; Wu, X.; Jin, J.; Bi, Y.; Chen, J.; Lei, F.; Liu, Q.; Duan, Z.; et al. Identification of climate factors related to human infection with avian influenza A H7N9 and H5N1 viruses in China. Sci. Rep. 2015, 5, 18094. [Google Scholar] [CrossRef] [Green Version]
- Shaman, J.; Pitzer, V.E.; Viboud, C.; Grenfell, B.T.; Lipsitch, M. Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol. 2010, 8, e1000316. [Google Scholar] [CrossRef]
- Cox, N.J.; Subbarao, K. Global epidemiology of influenza: Past and present. Annu. Rev. Med. 2000, 51, 407–421. [Google Scholar] [CrossRef]
- Tamerius, J.; Nelson, M.I.; Zhou, S.Z.; Viboud, C.; Miller, M.A.; Alonso, W.J. Global influenza seasonality: Reconciling patterns across temperate and tropical regions. Environ. Health Perspect. 2011, 119, 439–445. [Google Scholar] [CrossRef] [Green Version]
- Finkelman, B.S.; Viboud, C.; Koelle, K.; Ferrari, M.J.; Bharti, N.; Grenfell, B.T. Global patterns in seasonal activity of influenza A/H3N2, A/H1N1, and B from 1997 to 2005: Viral coexistence and latitudinal gradients. PLoS ONE 2007, 2, e1296. [Google Scholar] [CrossRef]
- Azziz Baumgartner, E.; Dao, C.N.; Nasreen, S.; Bhuiyan, M.U.; Mah, E.M.S.; Al Mamun, A.; Sharker, M.A.; Zaman, R.U.; Cheng, P.Y.; Klimov, A.I.; et al. Seasonality, timing, and climate drivers of influenza activity worldwide. J. Infect. Dis. 2012, 206, 838–846. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Ye, X.; Zhou, J.; Zhai, F.; Chen, J. The association between the seasonality of pediatric pandemic influenza virus outbreak and ambient meteorological factors in Shanghai. Environ. Health 2020, 19, 71. [Google Scholar] [CrossRef]
- Park, J.E.; Son, W.S.; Ryu, Y.; Choi, S.B.; Kwon, O.; Ahn, I. Effects of temperature, humidity, and diurnal temperature range on influenza incidence in a temperate region. Influenza Other Respir Viruses 2020, 14, 11–18. [Google Scholar] [CrossRef] [Green Version]
- Yamaya, M.; Nishimura, H.; Lusamba Kalonji, N.; Deng, X.; Momma, H.; Shimotai, Y.; Nagatomi, R. Effects of high temperature on pandemic and seasonal human influenza viral replication and infection-induced damage in primary human tracheal epithelial cell cultures. Heliyon 2019, 5, e01149. [Google Scholar] [CrossRef] [Green Version]
- Lowen, A.C.; Mubareka, S.; Steel, J.; Palese, P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007, 3, 1470–1476. [Google Scholar] [CrossRef]
- Yang, W.; Cummings, M.J.; Bakamutumaho, B.; Kayiwa, J.; Owor, N.; Namagambo, B.; Byaruhanga, T.; Lutwama, J.J.; O’Donnell, M.R.; Shaman, J. Dynamics of influenza in tropical Africa: Temperature, humidity, and co-circulating (sub)types. Influenza Other Respir. Viruses 2018, 12, 446–456. [Google Scholar] [CrossRef] [Green Version]
- Soebiyanto, R.P.; Adimi, F.; Kiang, R.K. Modeling and predicting seasonal influenza transmission in warm regions using climatological parameters. PLoS ONE 2010, 5, e9450. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Wang, Y.; Jin, S.; Wu, Z.; Chin, D.P.; Koplan, J.P.; Wilson, M.E. Emergence and control of infectious diseases in China. Lancet 2008, 372, 1598–1605. [Google Scholar] [CrossRef]
- China Center for Disease Control and Prevention. The Public Health Science Data Center. Available online: http://www.phsciencedata.cn/Share/index.jsp (accessed on 20 June 2021).
- China Center for Disease Control and Prevention. Epidemic Situation of Notifiable Infectious Diseases in China in 2017. Available online: http://www.nhc.gov.cn/jkj/s3578/201802/de926bdb046749abb7b0a8e23d929104.shtml (accessed on 20 June 2021).
- Liu, Z.; Zhang, J.; Zhang, Y.; Lao, J.; Liu, Y.; Wang, H.; Jiang, B. Effects and interaction of meteorological factors on influenza: Based on the surveillance data in Shaoyang, China. Environ. Res. 2019, 172, 326–332. [Google Scholar] [CrossRef]
- Jaakkola, K.; Saukkoriipi, A.; Jokelainen, J.; Juvonen, R.; Kauppila, J.; Vainio, O.; Ziegler, T.; Rönkkö, E.; Jaakkola, J.J.; Ikäheimo, T.M. Decline in temperature and humidity increases the occurrence of influenza in cold climate. Environ. Health 2014, 13, 22. [Google Scholar] [CrossRef] [Green Version]
- du Prel, J.B.; Puppe, W.; Gröndahl, B.; Knuf, M.; Weigl, J.A.; Schaaff, F.; Schmitt, H.J. Are meteorological parameters associated with acute respiratory tract infections? Clin. Infect. Dis. 2009, 49, 861–868. [Google Scholar] [CrossRef] [Green Version]
- Tang, J.W.; Lai, F.Y.; Wong, F.; Hon, K.L. Incidence of common respiratory viral infections related to climate factors in hospitalized children in Hong Kong. Epidemiol. Infect. 2010, 138, 226–235. [Google Scholar] [CrossRef] [Green Version]
- Bouvier, N.M.; Palese, P. The biology of influenza viruses. Vaccine 2008, 26, D49–D53. [Google Scholar] [CrossRef] [Green Version]
- Jiang, D.; Wang, Q.; Bai, Z.; Qi, H.; Ma, J.; Liu, W.; Ding, F.; Li, J. Could Environment Affect the Mutation of H1N1 Influenza Virus? Int. J. Environ. Res. Public Health 2020, 17, 3092. [Google Scholar] [CrossRef]
- Zhang, Y.; Ye, C.; Yu, J.; Zhu, W.; Wang, Y.; Li, Z.; Xu, Z.; Cheng, J.; Wang, N.; Hao, L.; et al. The complex associations of climate variability with seasonal influenza A and B virus transmission in subtropical Shanghai, China. Sci. Total Environ. 2020, 701, 134607. [Google Scholar] [CrossRef]
- Luan, G.; Zhou, M.G. Correlation between low air temperature and influenza incidence in winter in China, 2004–2016. Chin. J. Epidemiol. 2020, 41, 368–372. [Google Scholar]
- Firestone, S.M.; Cogger, N.; Ward, M.P.; Toribio, J.A.; Moloney, B.J.; Dhand, N.K. The influence of meteorology on the spread of influenza: Survival analysis of an equine influenza (A/H3N8) outbreak. PLoS ONE 2012, 7, e35284. [Google Scholar] [CrossRef] [Green Version]
- Feng, C.; Li, J.; Sun, W.; Zhang, Y.; Wang, Q. Impact of ambient fine particulate matter (PM2.5) exposure on the risk of influenza-like-illness: A time-series analysis in Beijing, China. Environ. Health 2016, 15, 17. [Google Scholar] [CrossRef] [Green Version]
- Hammond, G.W.; Raddatz, R.L.; Gelskey, D.E. Impact of atmospheric dispersion and transport of viral aerosols on the epidemiology of influenza. Rev. Infect. Dis. 1989, 11, 494–497. [Google Scholar] [CrossRef]
- Ssematimba, A.; Hagenaars, T.J.; de Jong, M.C. Modelling the wind-borne spread of highly pathogenic avian influenza virus between farms. PLoS ONE 2012, 7, e31114. [Google Scholar] [CrossRef] [Green Version]

| Monthly Influenza Cases and Meteorological Data | ||||||||
| Regions | Factors | Data Source | Number of Months | Min. | P (25th) | Median | P (75th) | Max. |
| China | Influenza cases | Notifiable infectious disease report database | 168 | 1179 | 3567 | 7210.5 | 13,953 | 135,398 |
| AT, °C | CMDSSS | 168 | −5.35 | 3.82 | 13.19 | 20.12 | 24.77 | |
| ARH, % | CMDSSS | 168 | 53.57 | 59.86 | 64.64 | 69.92 | 74.22 | |
| AWS, cm/s | CMDSSS | 168 | 18.3 | 19.68 | 20.9 | 23.05 | 26.7 | |
| ACP, mm | CMDSSS | 168 | 6.22 | 28.4 | 58.32 | 113.63 | 168.44 | |
| AAP, hPa | CMDSSS | 168 | 911.26 | 915.25 | 920.82 | 924.84 | 936.15 | |
| Northern China | Influenza cases | Notifiable infectious disease report database | 168 | 153 | 1208 | 3106 | 5374 | 58,371 |
| AT, °C | CMDSSS | 168 | −12.22 | −2.02 | 9.3 | 17.43 | 23.46 | |
| ARH, % | CMDSSS | 168 | 43.44 | 51.82 | 58.03 | 64.54 | 71.08 | |
| AWS, cm/s | CMDSSS | 168 | 18.43 | 20.97 | 22.55 | 25.2 | 30.82 | |
| ACP, mm | CMDSSS | 168 | 1.89 | 8.72 | 26.54 | 62.39 | 173.42 | |
| AAP, hPa | CMDSSS | 168 | 892 | 896.92 | 902.06 | 906.21 | 924.91 | |
| Southern China | Influenza cases | Notifiable infectious disease report database | 168 | 551 | 1936 | 3689 | 8360 | 77,027 |
| AT, °C | CMDSSS | 168 | 3.67 | 11.45 | 18.25 | 23.56 | 26.85 | |
| ARH, % | CMDSSS | 168 | 64.39 | 71 | 73.89 | 76.61 | 81.54 | |
| AWS, cm/s | CMDSSS | 168 | 15.42 | 17.97 | 18.88 | 20.07 | 23.37 | |
| ACP, mm | CMDSSS | 168 | 11.28 | 51.61 | 98.11 | 170.13 | 278.8 | |
| AAP, hPa | CMDSSS | 168 | 935.58 | 939.64 | 946.03 | 949.67 | 954.66 | |
| Weekly Influenza Virological and Meteorological Data | ||||||||
| Regions | Factors | Data Source | Number of Weeks | Min. | P (25th) | Median | P (75th) | Max. |
| China | Influenza H1N1 virus (%) | China National Influenza Center | 522 | 0 | 0.09 | 0.49 | 2.63 | 35.29 |
| Influenza H3N2 virus (%) | China National Influenza Center | 522 | 0 | 0.6 | 2.44 | 6.88 | 32.67 | |
| Influenza B virus (%) | China National Influenza Center | 522 | 0 | 0.59 | 1.71 | 6.35 | 38.91 | |
| AT, °C | CMDSSS | 522 | −5.62 | 3.62 | 13.74 | 21.17 | 26.08 | |
| ARH, % | CMDSSS | 522 | 49.39 | 61.48 | 66.1 | 70.68 | 77.93 | |
| AWS, cm/s | CMDSSS | 522 | 16.29 | 19.76 | 21.19 | 23.13 | 29.46 | |
| ACP, mm | CMDSSS | 522 | 0.24 | 6.79 | 15.63 | 26.87 | 55.65 | |
| AAP, hPa | CMDSSS | 522 | 913.24 | 919.86 | 925.39 | 929.2 | 941.14 | |
| Northern China | Influenza H1N1 virus (%) | China National Influenza Center | 522 | 0 | 0 | 0.15 | 2.03 | 37.68 |
| Influenza H3N2 virus (%) | China National Influenza Center | 522 | 0 | 0.15 | 1.17 | 4.47 | 38.48 | |
| Influenza B virus (%) | China National Influenza Center | 522 | 0 | 0.09 | 0.45 | 3.75 | 41.16 | |
| AT, °C | CMDSSS | 522 | −13.65 | −2.87 | 9.61 | 18.46 | 24.52 | |
| ARH, % | CMDSSS | 522 | 36.93 | 51.03 | 57.34 | 64.15 | 74.61 | |
| AWS, cm/s | CMDSSS | 522 | 16.32 | 21.01 | 23.04 | 25.76 | 34.76 | |
| ACP, mm | CMDSSS | 522 | 0.09 | 1.77 | 5.52 | 14.27 | 50.26 | |
| AAP, hPa | CMDSSS | 522 | 884.55 | 892.72 | 898.73 | 902.09 | 917.93 | |
| Southern China | Influenza H1N1 virus (%) | China National Influenza Center | 522 | 0 | 0.09 | 0.5 | 2.73 | 40.53 |
| Influenza H3N2 virus (%) | China National Influenza Center | 522 | 0 | 0.59 | 2.07 | 6.96 | 34.16 | |
| Influenza B virus (%) | China National Influenza Center | 522 | 0 | 0.73 | 2.08 | 7.13 | 39.7 | |
| AT, °C | CMDSSS | 522 | 2.65 | 11.17 | 18.68 | 24.16 | 28.6 | |
| ARH, % | CMDSSS | 522 | 57.38 | 72.78 | 76.12 | 79.16 | 85.9 | |
| AWS, cm/s | CMDSSS | 522 | 14.17 | 17.71 | 18.93 | 20.39 | 26.38 | |
| ACP, mm | CMDSSS | 522 | 0.03 | 11.25 | 24.41 | 39.4 | 94.63 | |
| AAP, hPa | CMDSSS | 522 | 942.17 | 949.93 | 955.91 | 960.46 | 968.93 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.; Zhang, X.; Jiang, D.; Yan, D.; Guan, Z.; Zhou, Y.; Liu, X.; Huang, C.; Ding, C.; Lan, L.; et al. Associations between Temperature and Influenza Activity: A National Time Series Study in China. Int. J. Environ. Res. Public Health 2021, 18, 10846. https://doi.org/10.3390/ijerph182010846
Chen C, Zhang X, Jiang D, Yan D, Guan Z, Zhou Y, Liu X, Huang C, Ding C, Lan L, et al. Associations between Temperature and Influenza Activity: A National Time Series Study in China. International Journal of Environmental Research and Public Health. 2021; 18(20):10846. https://doi.org/10.3390/ijerph182010846
Chicago/Turabian StyleChen, Can, Xiaobao Zhang, Daixi Jiang, Danying Yan, Zhou Guan, Yuqing Zhou, Xiaoxiao Liu, Chenyang Huang, Cheng Ding, Lei Lan, and et al. 2021. "Associations between Temperature and Influenza Activity: A National Time Series Study in China" International Journal of Environmental Research and Public Health 18, no. 20: 10846. https://doi.org/10.3390/ijerph182010846
APA StyleChen, C., Zhang, X., Jiang, D., Yan, D., Guan, Z., Zhou, Y., Liu, X., Huang, C., Ding, C., Lan, L., Huang, X., Li, L., & Yang, S. (2021). Associations between Temperature and Influenza Activity: A National Time Series Study in China. International Journal of Environmental Research and Public Health, 18(20), 10846. https://doi.org/10.3390/ijerph182010846






