A Spatial Analysis of COVID-19 in African Countries: Evaluating the Effects of Socio-Economic Vulnerabilities and Neighbouring
Abstract
:1. Introduction
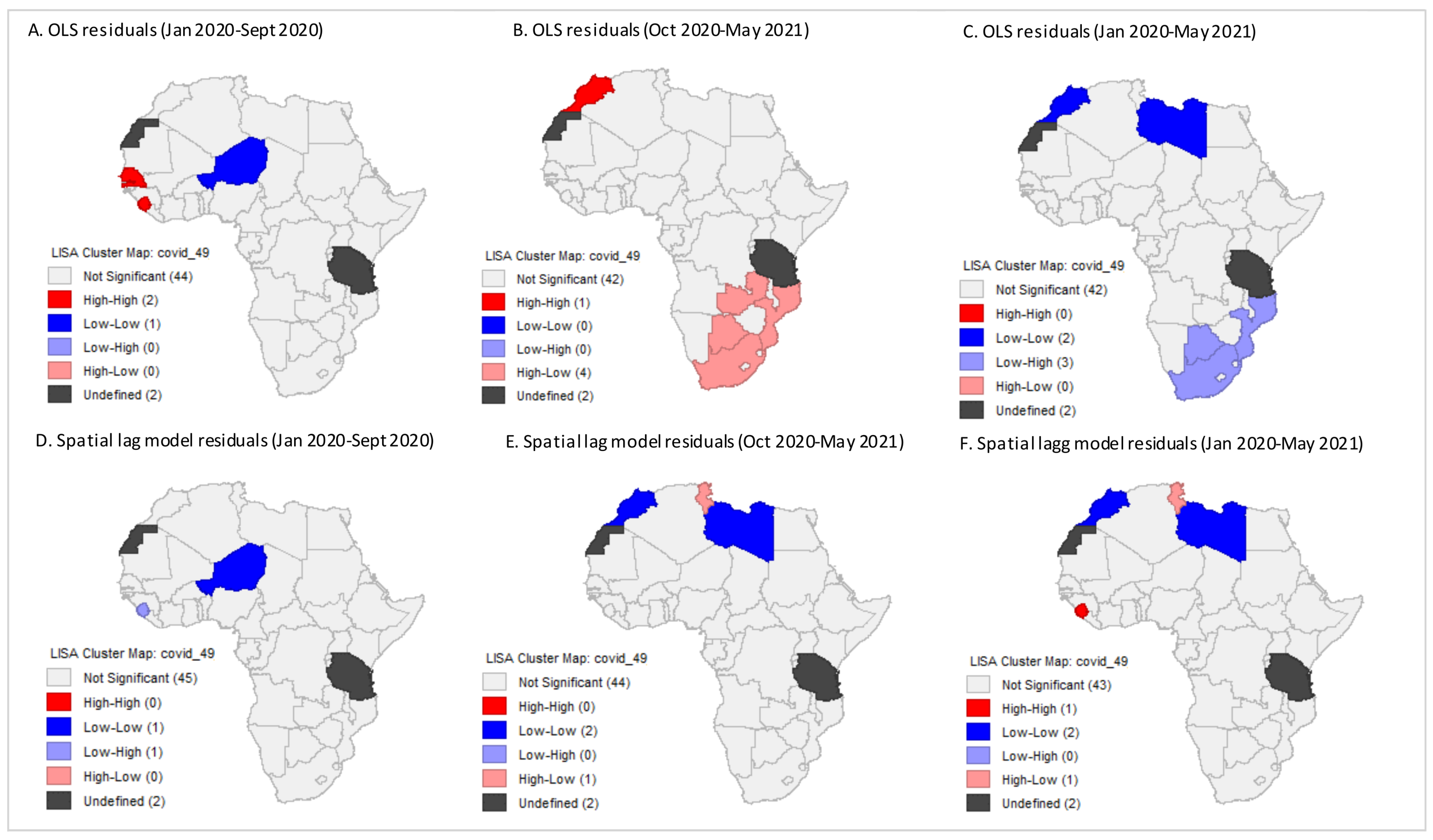
2. Methods
2.1. Data Sources
2.2. Spatial Regression Models
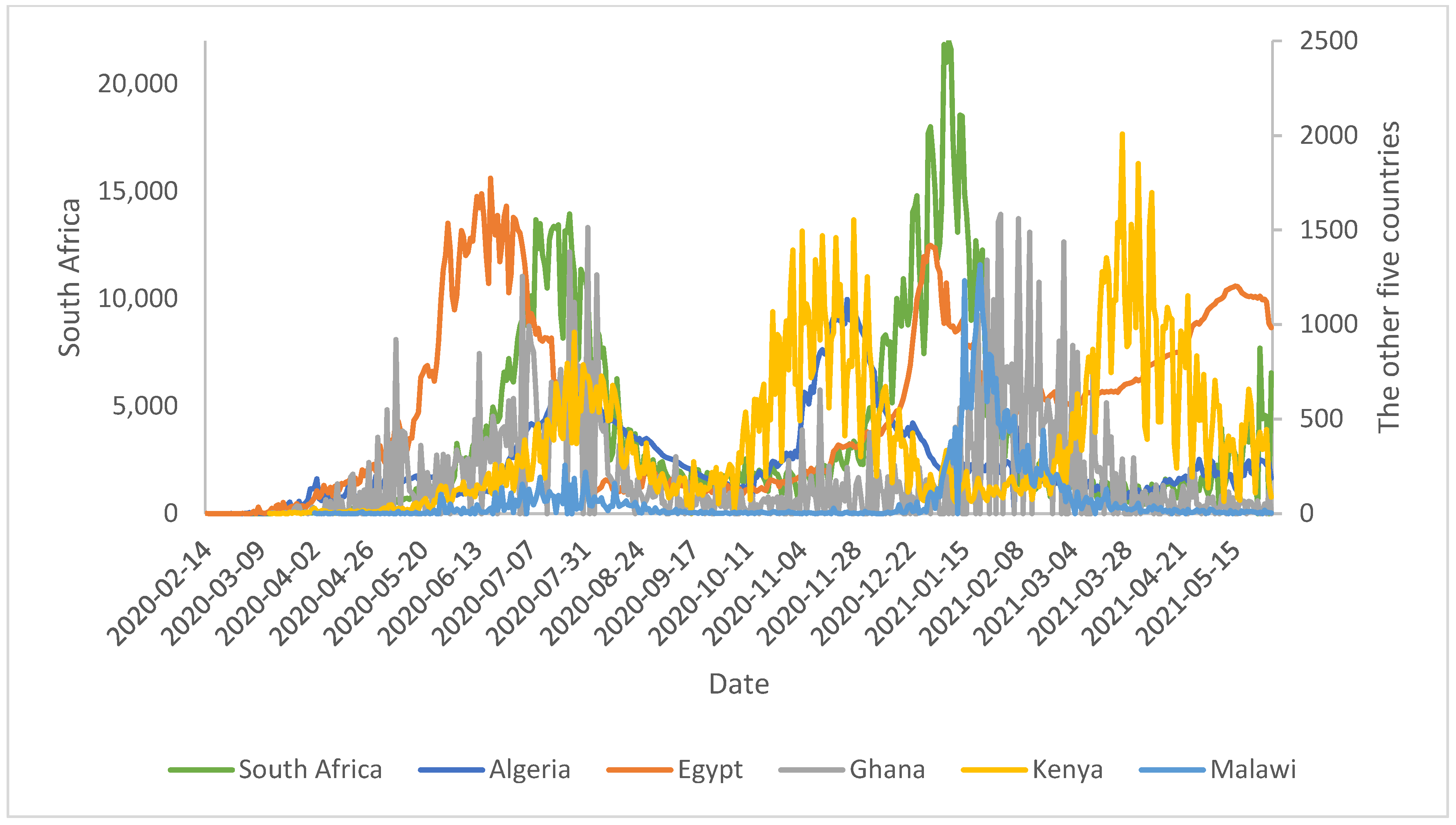
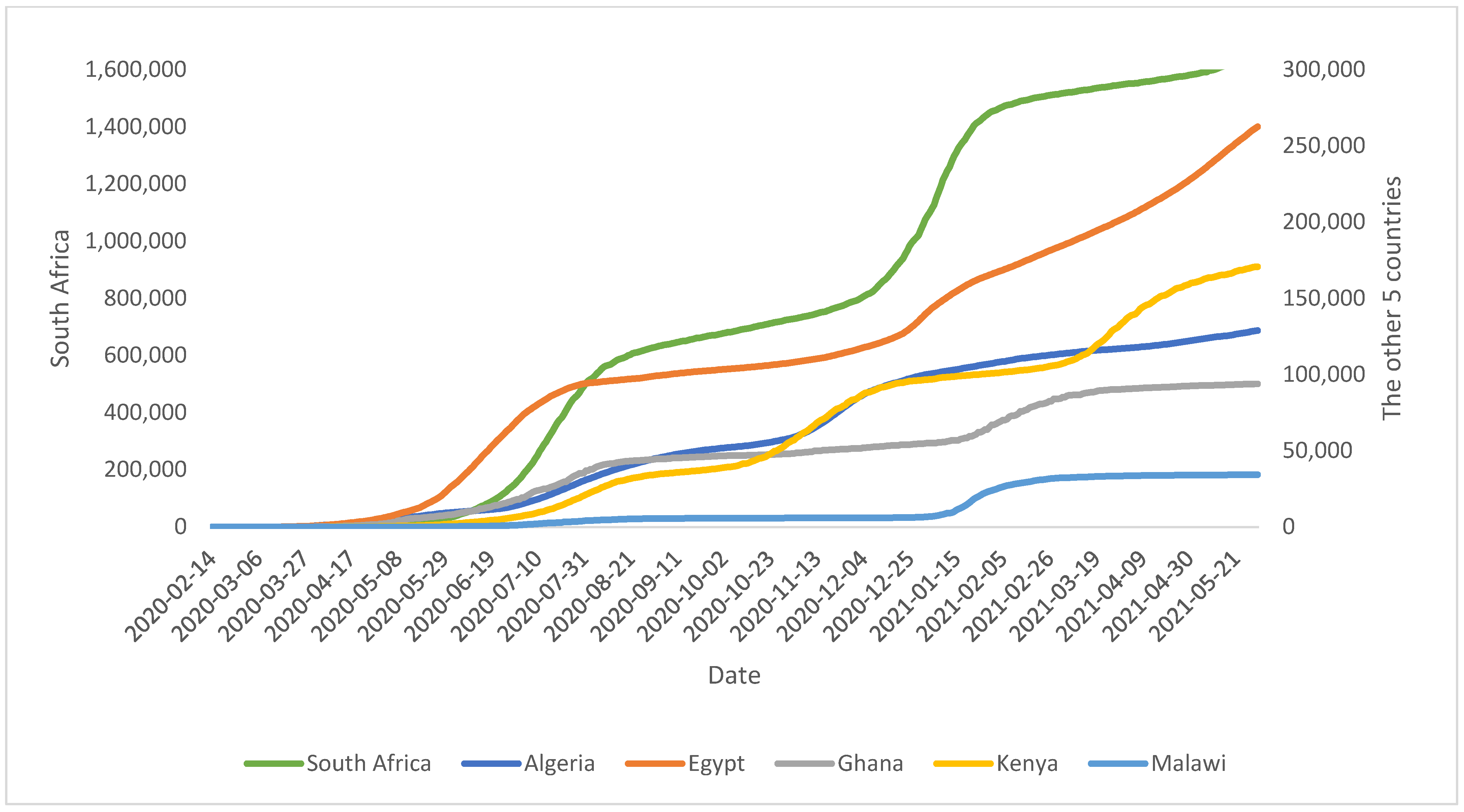
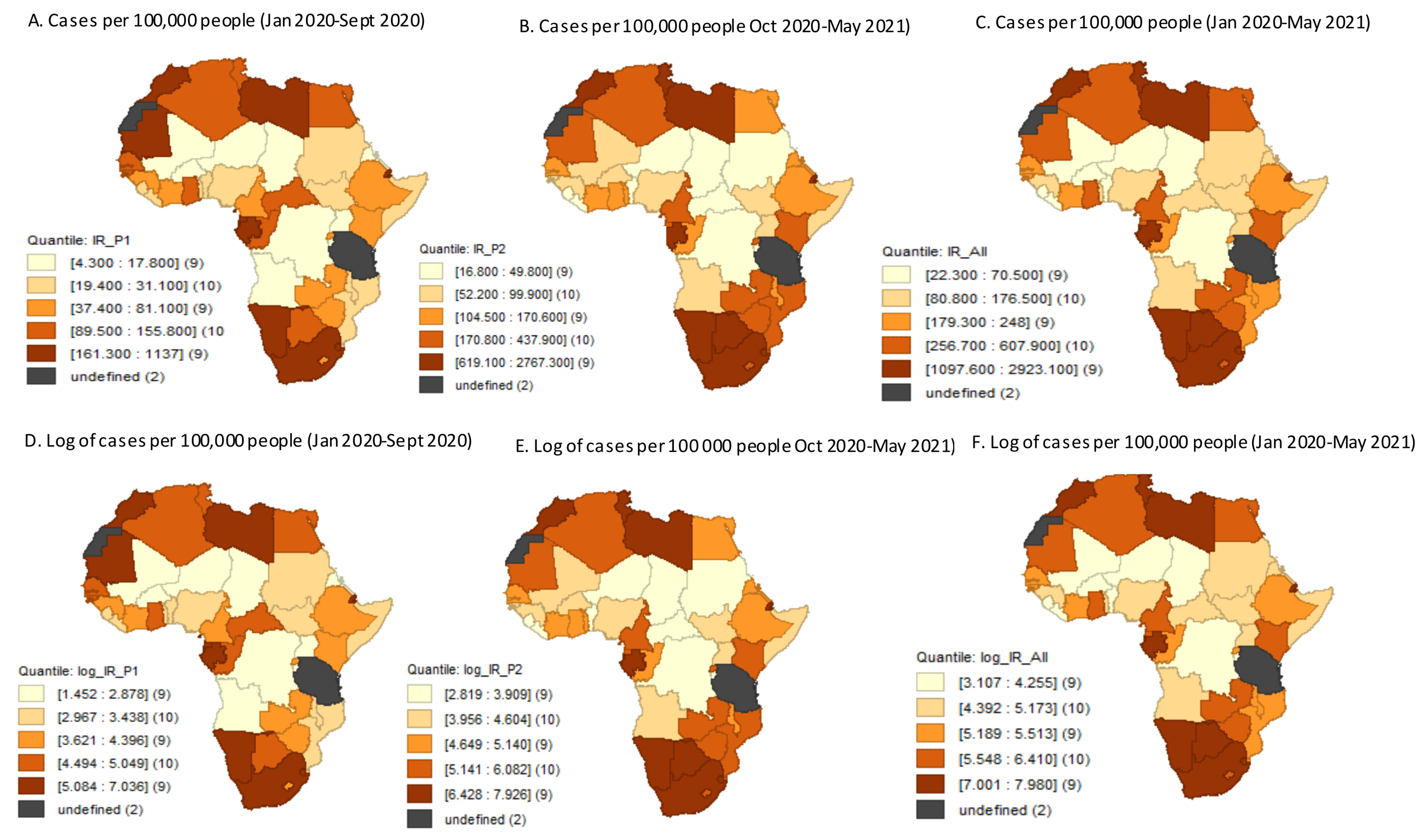
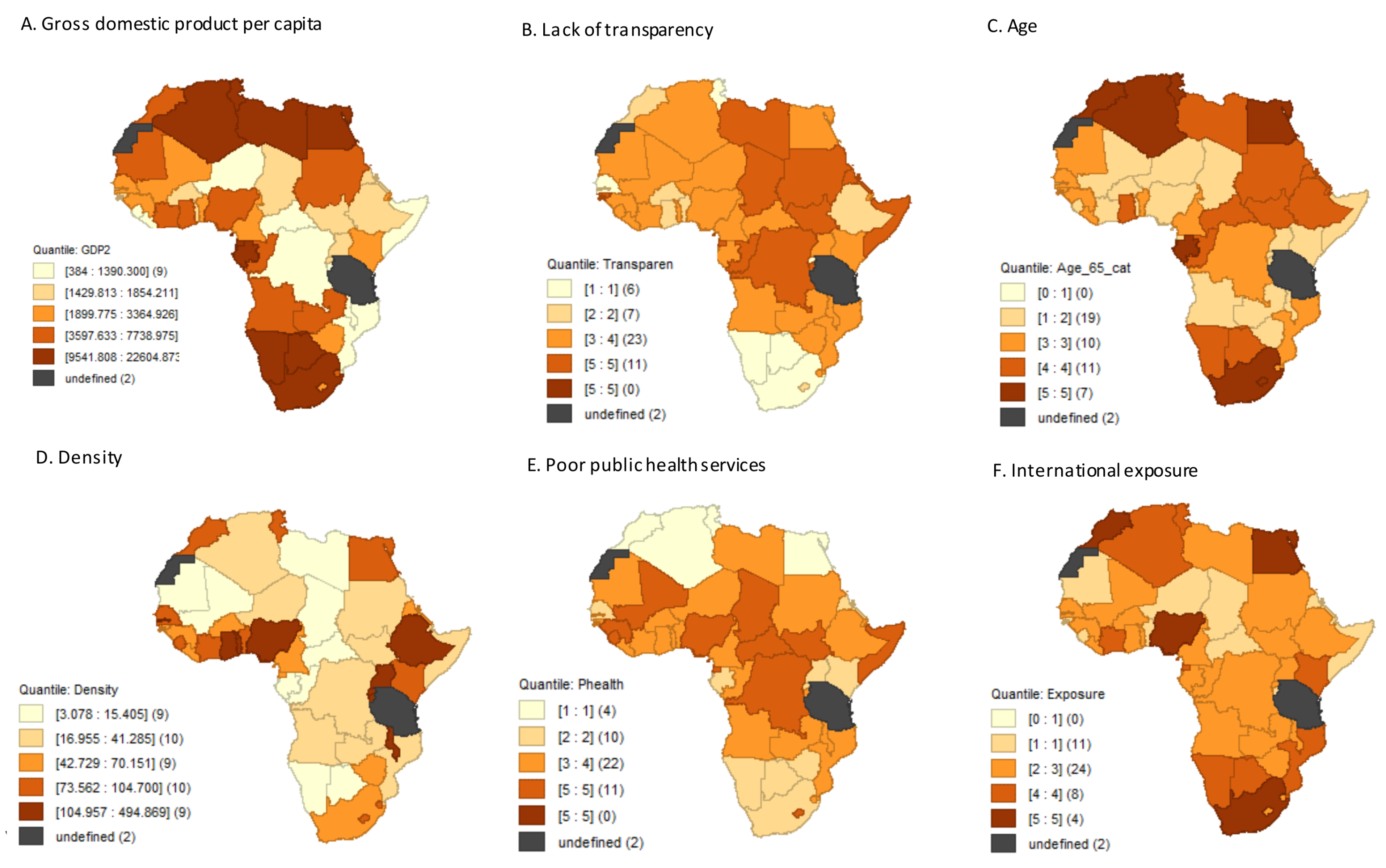
3. Results
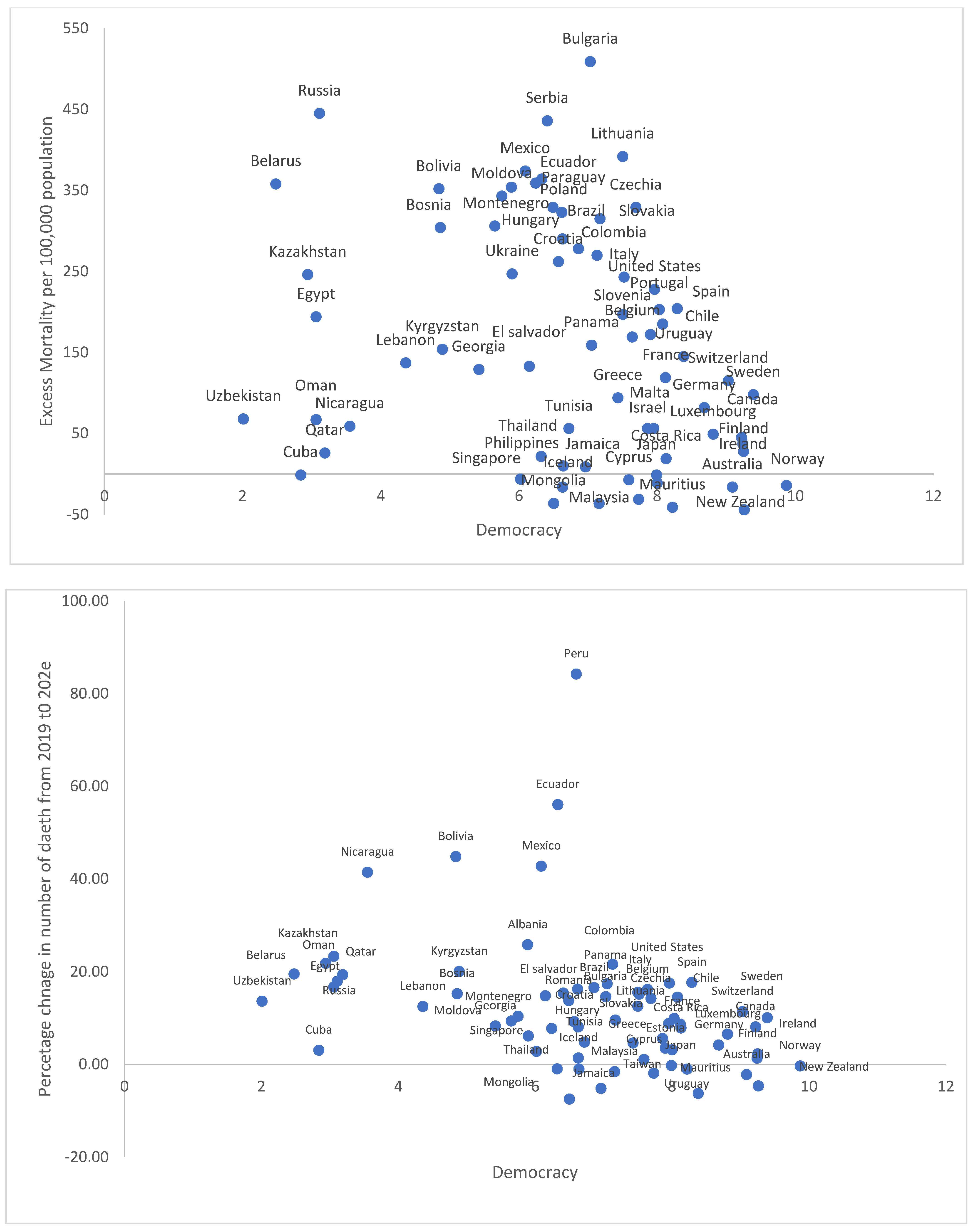
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Li, Q. An outbreak of NCIP (2019-nCoV) infection in China—Wuhan, Hubei province, 2019–2020. China CDC Wkly. 2020, 2, 79–80. [Google Scholar] [CrossRef]
- Lu, H.; Stratton, C.W.; Tang, Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J. Med. Virol. 2020, 92, 401–402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Pat, A.; Adegboye, O.A.; Adekunle, A.I.; Rahman, K.M.; McBryde, E.S.; Eisen, D.P. Economic Consequences of the COVID-19 Outbreak: The Need for Epidemic Preparedness. Front. Public Health 2020, 8, 241. [Google Scholar] [CrossRef]
- Villani, L.; Pastorino, R.; Molinari, E.; Anelli, F.; Ricciardi, W.; Graffigna, G.; Boccia, S. Impact of the COVID-19 pandemic on the psychological well-being of students in an Italian university: A web-based cross-sectional survey. Glob. Health 2021, 17, 39. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, A.A. Impact of the COVID-19 pandemic on the social and educational aspects of Saudi university students’ lives. PLoS ONE 2021, 16, e0250026. [Google Scholar] [CrossRef]
- Ritchie, H.; Ortiz-Ospina, E.; Beltekian, D.; Mathieu, E.; Hasell, J.; Macdonald, B.; Giattino, C.; Appel, C.; Rodés-Guirao, L.; Roser, M. Coronavirus Pandemic (COVID-19). 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 15 June 2021).
- Mehtar, S.; Preiser, W.; Lakhe, N.A.; Bousso, A.; TamFum, J.-J.M.; Kallay, O.; Seydi, M.; Zumla, P.S.A.; Nachega, J.B. Limiting the spread of COVID-19 in Africa: One size mitigation strategies do not fit all countries. Lancet Glob. Health 2020, 8, e881–e883. [Google Scholar] [CrossRef]
- Gilbert, M.; Pullano, G.; Pinotti, F.; Valdano, E.; Poletto, C.; Boëlle, P.Y.; D’Ortenzio, E.; Yazdanpanah, Y.; Eholie, S.P.; Altmann, M.; et al. Preparedness and vulnerability of African countries against importations of COVID-19: A modelling study. Lancet 2020, 395, 871–877. [Google Scholar] [CrossRef] [Green Version]
- Lone, S.A.; Ahmad, A. COVID-19 pandemic—an African perspective. Emerg. Microbes Infect. 2020, 9, 1300–1308. [Google Scholar] [CrossRef]
- Umviligihozo, G.; Mupfumi, L.; Sonela, N.; Naicker, D.; Obuku, E.A.; Koofhethile, C.; Mogashoa, T.; Kapaata, A.; Ombati, G.; Michelo, C.M. Sub-Saharan Africa preparedness and response to the COVID-19 pandemic: A perspective of early career African scientists. Wellcome Open Res. 2020, 5, 163. [Google Scholar] [CrossRef]
- Africa Center for Strategic Studies. Mapping Risk Factors for the Spread of COVID-19 in Africa. 2020. Available online: Africacenter.org/spotlight/mapping-risk-factors-spread-covid-19-africa/ (accessed on 1 March 2021).
- Sigler, T.; Mahmuda, S.; Kimpton, A.; Loginova, J.; Wohland, P.; Charles-Edwards, E.; Corcoran, J. The socio-spatial determinants of COVID-19 diffusion: The impact of globalisation, settlement characteristics and population. Glob. Health 2021, 17, 56. [Google Scholar] [CrossRef]
- Fatima, M.; O’Keefe, K.J.; Wei, W.; Arshad, S.; Gruebner, O. Geospatial Analysis of COVID-19: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 2336. [Google Scholar] [CrossRef]
- Shen, C.Y. Logistic growth modelling of COVID-19 proliferation in China and its international implications. Int. J. Infect. Dis. 2020, 96, 582–589. [Google Scholar] [CrossRef]
- Roosa, K.; Lee, Y.; Luo, R.; Kirpich, A.; Rothenberg, R.; Hyman, J.; Yan, P.; Chowell, G. Real-time forecasts of the COVID-19 epidemic in China from February 5th to February 24th, 2020. Infect. Dis. Model. 2020, 5, 256–263. [Google Scholar] [CrossRef]
- Almeshal, A.M.; Almazrouee, A.I.; Alenizi, M.R.; Alhajeri, S.N. Forecasting the Spread of COVID-19 in Kuwait Using Compartmental and Logistic Regression Models. Appl. Sci. 2020, 10, 3402. [Google Scholar] [CrossRef]
- Reddy, T.; Shkedy, Z.; Janse van Rensburg, C.; Mwambi, H.; Debba, P.; Zuma, K.; Manda, S. Short-term real-time prediction of total number of reported COVID-19 cases and deaths in South Africa: A data driven approach. BMC Med. Res. Methodol. 2021, 21, 15. [Google Scholar] [CrossRef]
- Cooper, I.; Mondal, A.; Antonopoulos, C.G. A SIR model assumption for the spread of COVID-19 in different communities. Chaos Solitons Fractals 2020, 139, 110057. [Google Scholar] [CrossRef]
- Sun, F.; Matthews, S.A.; Yang, T.C.; Hu, M.H. A spatial analysis of COVID-19 period prevalence in US counties through June 28, 2020: Where geography matters? Ann. Epidemiol. 2020. [Google Scholar] [CrossRef]
- Cuadros, D.F.; Xiao, Y.; Mukandavire, Z.; Correa-Agudelo, E.; Hernández, A.; Kim, H.; MacKinnon, N.J. Spatiotemporal transmission dynamics of the COVID-19 pandemic and its impact on critical healthcare capacity. Health Place 2020, 64, 102404. [Google Scholar] [CrossRef]
- Raymundo, C.E.; Oliveira, M.C.; Eleuterio, T.D.A.; André, S.R.; da Silva, M.G.; Queiroz, E.R.D.S.; Medronho, R.D.A. Spatial analysis of COVID-19 incidence and the sociodemographic context in Brazil. PLoS ONE 2021, 16, e0247794. [Google Scholar] [CrossRef]
- Saffary, T.; Adegboye, O.A.; Gayawan, E.; Elfaki, F.; Kuddus, M.A.; Saffary, R. Analysis of COVID-19 Cases’ Spatial Dependence in US Counties Reveals Health Inequalities. Front. Public Health 2020, 8, 579190. [Google Scholar] [CrossRef]
- Wang, Y.; Di, Q. Modifiable areal unit problem and environmental factors of COVID-19 outbreak. Sci. Total Environ. 2020, 740, 139984. [Google Scholar] [CrossRef]
- Lin, Y.; Zhong, P.; Chen, T. Association Between Socioeconomic Factors and the COVID-19 Outbreak in the 39 Well-Developed Cities of China. Front. Public Health 2020, 8, 546637. [Google Scholar] [CrossRef]
- Nyasulu, J.C.Y.; Munthali, R.J.; Nyondo-Mipando, A.L.; Pandya, H.; Nyirenda, L.; Nyasulu, P.S.; Manda, S. COVID-19 pandemic in Malawi: Did public sociopolitical events gatherings contribute to its first-wave local transmission? Int. J. Infect. Dis. 2021, 106, 269–275. [Google Scholar] [CrossRef]
- Cambaza, E.M.; Viegas, G.C. COVID-19: Correlation between gross domestic product, number of tests, and confirmed cases in 13 African countries. J. Public Health Epidemiol. 2021, 13, 14–19. [Google Scholar]
- Nit, B.; Samy, A.L.; Tan, S.L.; Vory, S.; Lim, Y.; Nugraha, R.R.; Lin, X.; Ahmadi, A.; Lucero-Prisno, D.E., 3rd. Understanding the Slow COVID-19 Trajectory of Cambodia. Public Health Pract. 2021, 2, 100073. [Google Scholar] [CrossRef]
- Nguyen Thi Yen, C.; Hermoso, C.; Laguilles, E.M.; De Castro, L.E.; Camposano, S.M.; Jalmasco, N.; Cua, K.A.; Isa, M.A.; Akpan, E.F.; Ly, T.P.; et al. Vietnam’s success story against COVID-19. Public Health Pract. 2021, 2, 100132. [Google Scholar] [CrossRef]
- Anselin, L. Spatial Econometrics: Methods and Models; Kluwer Academic Publishers: Dordrecht, The Netherlands, 1988. [Google Scholar]
- LeSage, J.P. An Introduction to Spatial Econometrics, Revue D’économie Industrielle [Online], 123 | 3e Trimestre 2008, Document 4, Online since 15 September 2010, Connection on 19 April 2019. Available online: http://journals.openedition.org/rei/3887 (accessed on 20 September 2021). [CrossRef] [Green Version]
- Bivand, R.S.; Pebesma, E.; Gomez-Rubio, V. Applied Spatial Data Analysis with R, 2nd ed.; Springer: New York, NY, USA, 2013; Available online: https://asdar-book.org/ (accessed on 20 September 2021).
- Anselin, L.; Bera, A.K.; Florax, R.; Yoon, M.J. Simple Diagnostic Tests for Spatial Dependence. Reg. Sci. Urban Econ. 1996, 27, 77–104. [Google Scholar] [CrossRef]
- Sankoh, O.; Dickson, K.E.; Faniran, S.; Lahai, J.I.; Forna, F.; Liyosi, E.; Kamara, M.K.; Jabbi, S.B.; Johnny, A.B.; Conteh-Khali, N.; et al. Births and deaths must be registered in Africa. Lancet Glob. Health 2020, 8, e33–e34. [Google Scholar] [CrossRef] [Green Version]
- Karlinsky, A.; Kobak, D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. eLife 2021, 10, e69336. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, M.; Malani, A.; Ravi, S.; Agrawal, A. Authoritarian governments appear to manipulate COVID data. arXiv 2020, arXiv:2007.09566. [Google Scholar]
- Liang, L.-L.; Tseng, C.-H.; Ho, H.J.; Wu, C.-Y. Covid-19 mortality is negatively associated with test number and government effectiveness. Sci. Rep. 2020, 10, 12567. [Google Scholar] [CrossRef] [PubMed]
- Annaka, S. Political regime, data transparency, and COVID-19 death cases. SSM Popul. Health 2021, 15, 100832. [Google Scholar] [CrossRef]
- Wang, Q.; Dong, W.; Yang, K.; Ren, Z.; Huang, D.; Zhang, P.; Wang, J. Temporal, and spatial analysis of COVID-19 transmission in China and its influencing factors. Int. J. Infect. Dis. 2021, 105, 675–685. [Google Scholar] [CrossRef]
| COVID-19 Burdern Indicator | Mean | SD | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| Number of days since 1st case | 440.4 | 13.7 | 441 | 383 | 479 |
| Confirmed number of cases | 101,041 | 254,776 | 26,963 | 2191 | 1,665,617 |
| Confirmed number of cases/100,000 | 543.8 | 799.4 | 211.3 | 22.3 | 2923.1 |
| Confirmed number of cases/100,000 * | 2.4 | 0.6 | 2.3 | 1.3 | 3.5 |
| Confirmed number of deaths | 2750 | 8577 | 517 | 6 | 56,506 |
| CFR | 2.2 | 1.5 | 1.7 | 0.13 | 7.4 |
| COVID-19 vulnerability indicator | |||||
| Age 65 or older (%) | 3.7 | 1.7 | 3.1 | 2.2 | 10.9 |
| Extreme poverty (%) | 34.1 | 23.6 | 36.8 | 0.5 | 77.6 |
| GDP per capita | 5443.8 | 68 | 6182.7 | 2705.4 | 26,382.3 |
| Country | Confirmed Cases (No.) | Confirmed Deaths (No.) | CFR (%) |
|---|---|---|---|
| Most affected | |||
| South Africa | 1,665,617 | 56,506 | 3.39 |
| Morocco | 519,216 | 9147 | 1.76 |
| Tunisia | 345,474 | 12,654 | 3.66 |
| Ethiopia | 271,541 | 4165 | 1.53 |
| Egypt | 262,650 | 15,096 | 5.75 |
| Least affected | |||
| Burundi | 4790 | 6 | 0.13 |
| Eritrea | 4094 | 14 | 0.34 |
| Liberia | 2191 | 86 | 3.93 |
| COVID-19 Vulnerability | OLS Model | SAR Model | Spatial Error Model | SAC Model | ||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Constant | 1.57 | 2.72 | 0.67 | 3.05 | −0.28 | 2.49 | −0.47 | 2.85 |
| Weak Public Health System | 0.06 | 0.16 | 0.08 | 0.15 | 0.11 | 0.14 | 0.13 | 0.14 |
| High International Exposure | −0.03 | 0.15 | −0.04 | 0.14 | −0.07 | 0.13 | −0.08 | 0.13 |
| Age 65 or older | 0.30 | 0.12 * | 0.30 | 0.11 * | 0.30 | 0.11 * | 0.31 | 0.12 * |
| Population Density | −0.0008 | 0.002 | −0.005 | 0.002 | 0.00008 | 0.002 | −0.0001 | 0.002 |
| Low Transparency | −0.25 | 0.12 * | −0.25 | 0.11 * | −0.24 | 0.11 | −0.24 | 0.11 * |
| Low GDP Capita | −0.0001 | 0.00003 * | −0.0001 | 0.00003 * | −0.0001 | 0.00003 * | −0.0001 | 0.00003 * |
| Number of days | 0.010 | 0.01 | 0.01 | 0.01 | 0.02 | 0.01 | 0.02 | 0.01 |
| Spatial lag parameter | 0.084 | −0.097 | ||||||
| Spatial error parameter | 0.207 | 0.337 | ||||||
| AIC | 136.99 | 138.75 | 138.5 | 140.42 | ||||
| COVID-19 Vulnerability | OLS Model | SAR Model | Spatial Error Model | SAC Model | ||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Constant | 11.38 | 5.19 | 4.67 | 5.10 | 10.81 | 4.74 | 5.22 | 4.28 |
| Weak Public Health System | −0.30 | 0.15 * | −0.19 | 0.13 | −0.28 | 0.13 * | −0.24 | 0.11 * |
| High International Exposure | 0.04 | 0.13 | 0.0005 | 0.03 | 0.04 | 0.12 | 0.008 | 0.11 |
| Age 65 or older | 0.15 | 0.11 | 0.14 | 0.10 | 0.15 | 0.10 | 0.12 | 0.08 |
| Population Density | −0.001 | 0.002 | −0.003 | 0.001 | −0.001 | 0.001 | −0.002 | 0.001 |
| Low Transparency | −0.26 | 0.11 * | −0.25 | 0.09 * | −0.26 | 0.10 * | −0.19 | 0.08 * |
| Low GDP Per Capita | −0.0001 | 0.00003 * | 0.00009 | 0.00003 * | −0.0001 | 0.00003 * | 0.00008 | 0.00002 * |
| Number of days | −0.01 | 0.01 | −0.002 | 0.01 | −0.01 | 0.01 | −0.005 | 0.009 |
| Spatial lag parameter | 0.342 * | 0.535 * | ||||||
| Spatial error parameter | 0.041 | −0.564 * | ||||||
| AIC | 129.25 | 126.05 | 131.22 | 123.42 | ||||
| COVID-19 Vulnerability | OLS Model | SAR Model | Spatial Error Model | SAC Model | ||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Constant | 8.83 | 4.85 | 3.17 | 5.11 | 8.56 | 4.42 | 5.22 | 4.29 |
| Weak Public Health System | −0.20 | 0.14 | −0.11 | 0.12 | −0.19 | 0.12 | −0.18 | 0.11 |
| High International Exposure | 0.002 | 0.13 | 0.03 | 0.11 | −0.0003 | 0.12 | −0.006 | 0.11 |
| Age 65 or older | 0.20 | 0.11 | 0.18 | 0.09 | 0.20 | 0.10 * | 0.17 | 0.08 * |
| Population Density | −0.001 | 0.001 | −0.002 | 0.001 | −0.001 | 0.001 | −0.0004 | 0.001 |
| Low Transparency | −0.26 | 0.11 * | −0.25 | 0.09 * | −0.26 | 0.09 | −0.21 | 0.08 |
| Low GDP Per Capita | −0.001 | 0.00003 * | −0.0001 | 0.00003 * | −0.0001 | 0.00003 * | −0.00008 | 0.00002 * |
| Number of days | −0.007 | 0.01 | 0.002 | 0.01 | −0.006 | 0.010 * | −0.004 | 0.009 * |
| Spatial lag parameter | 0.282 | 0.448 * | ||||||
| Spatial error parameter | 0.0171 | −0.505 | ||||||
| AIC | 122.89 | 121.4 | 124.89 | 120.46 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manda, S.O.M.; Darikwa, T.; Nkwenika, T.; Bergquist, R. A Spatial Analysis of COVID-19 in African Countries: Evaluating the Effects of Socio-Economic Vulnerabilities and Neighbouring. Int. J. Environ. Res. Public Health 2021, 18, 10783. https://doi.org/10.3390/ijerph182010783
Manda SOM, Darikwa T, Nkwenika T, Bergquist R. A Spatial Analysis of COVID-19 in African Countries: Evaluating the Effects of Socio-Economic Vulnerabilities and Neighbouring. International Journal of Environmental Research and Public Health. 2021; 18(20):10783. https://doi.org/10.3390/ijerph182010783
Chicago/Turabian StyleManda, Samuel O. M., Timotheus Darikwa, Tshifhiwa Nkwenika, and Robert Bergquist. 2021. "A Spatial Analysis of COVID-19 in African Countries: Evaluating the Effects of Socio-Economic Vulnerabilities and Neighbouring" International Journal of Environmental Research and Public Health 18, no. 20: 10783. https://doi.org/10.3390/ijerph182010783
APA StyleManda, S. O. M., Darikwa, T., Nkwenika, T., & Bergquist, R. (2021). A Spatial Analysis of COVID-19 in African Countries: Evaluating the Effects of Socio-Economic Vulnerabilities and Neighbouring. International Journal of Environmental Research and Public Health, 18(20), 10783. https://doi.org/10.3390/ijerph182010783







