Disparities in Healthcare Services and Spatial Assessments of Mobile Health Clinics in the Border Regions of Thailand
Abstract
1. Introduction
2. Materials and Methods
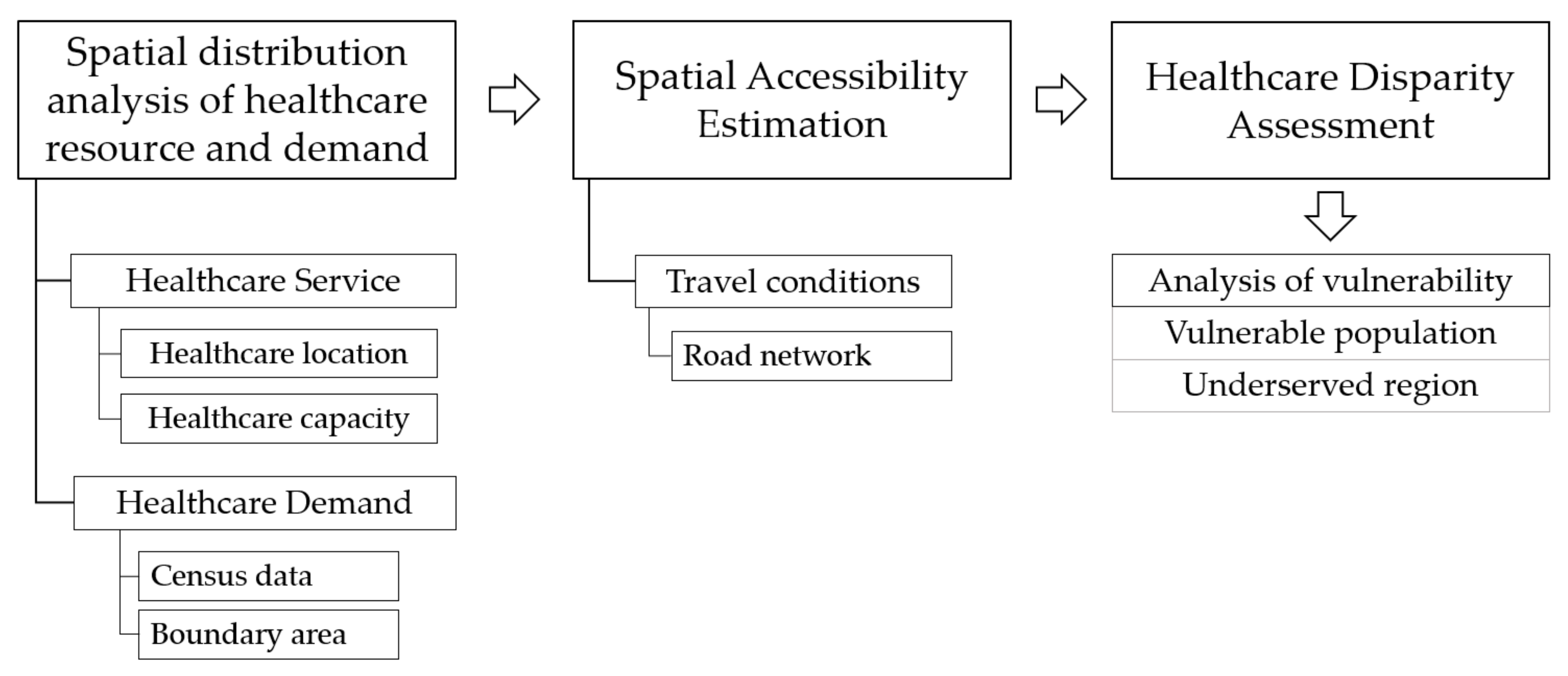
2.1. Methodology
2.1.1. Spatial Distribution of Healthcare Resources and Population Demand
2.1.2. Spatial Accessibility Estimation
2.1.3. Healthcare Disparity Assessment
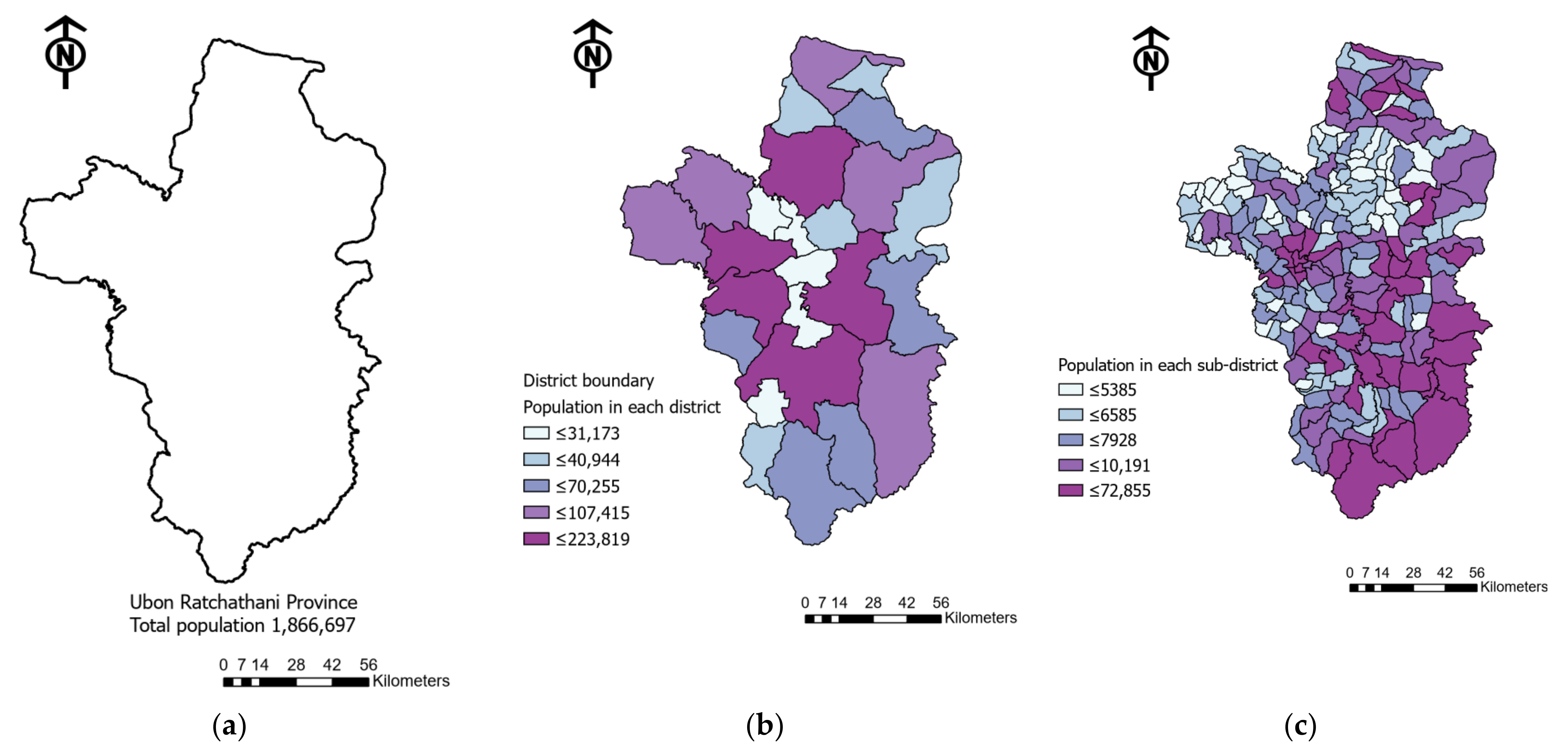
2.2. Study Area
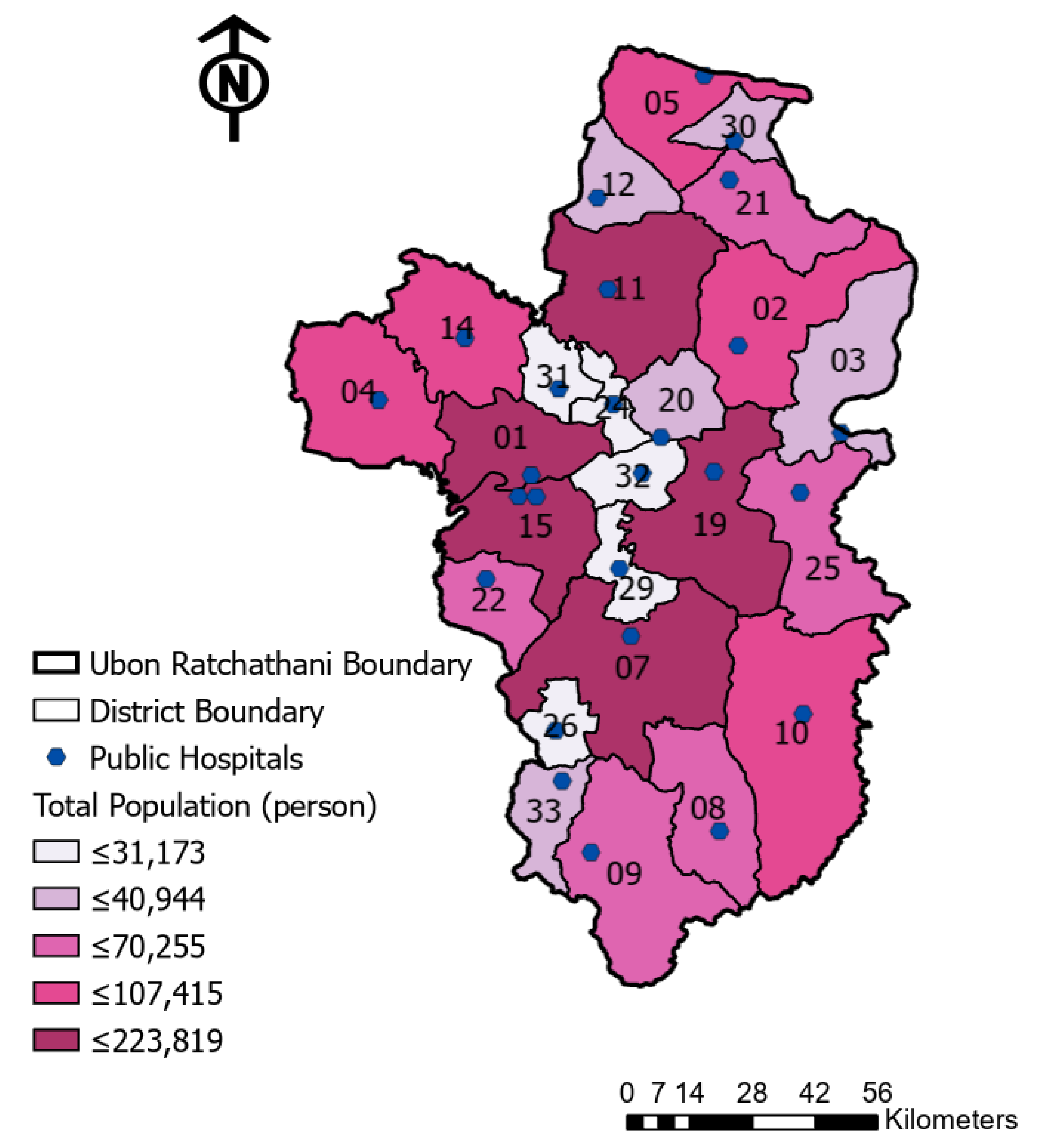
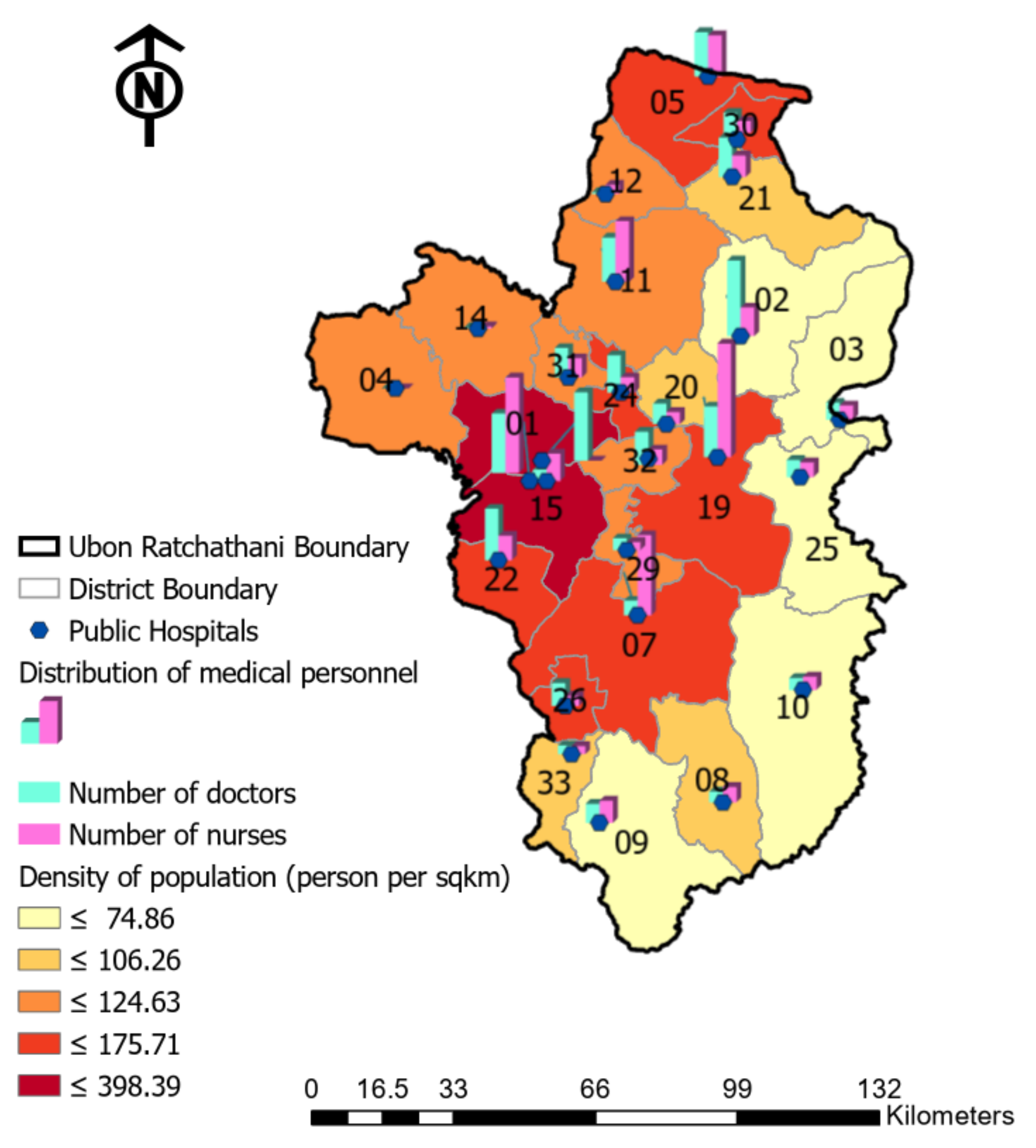
2.3. Collected Data
3. Results
3.1. Spatial Distribution Analysis of Healthcare
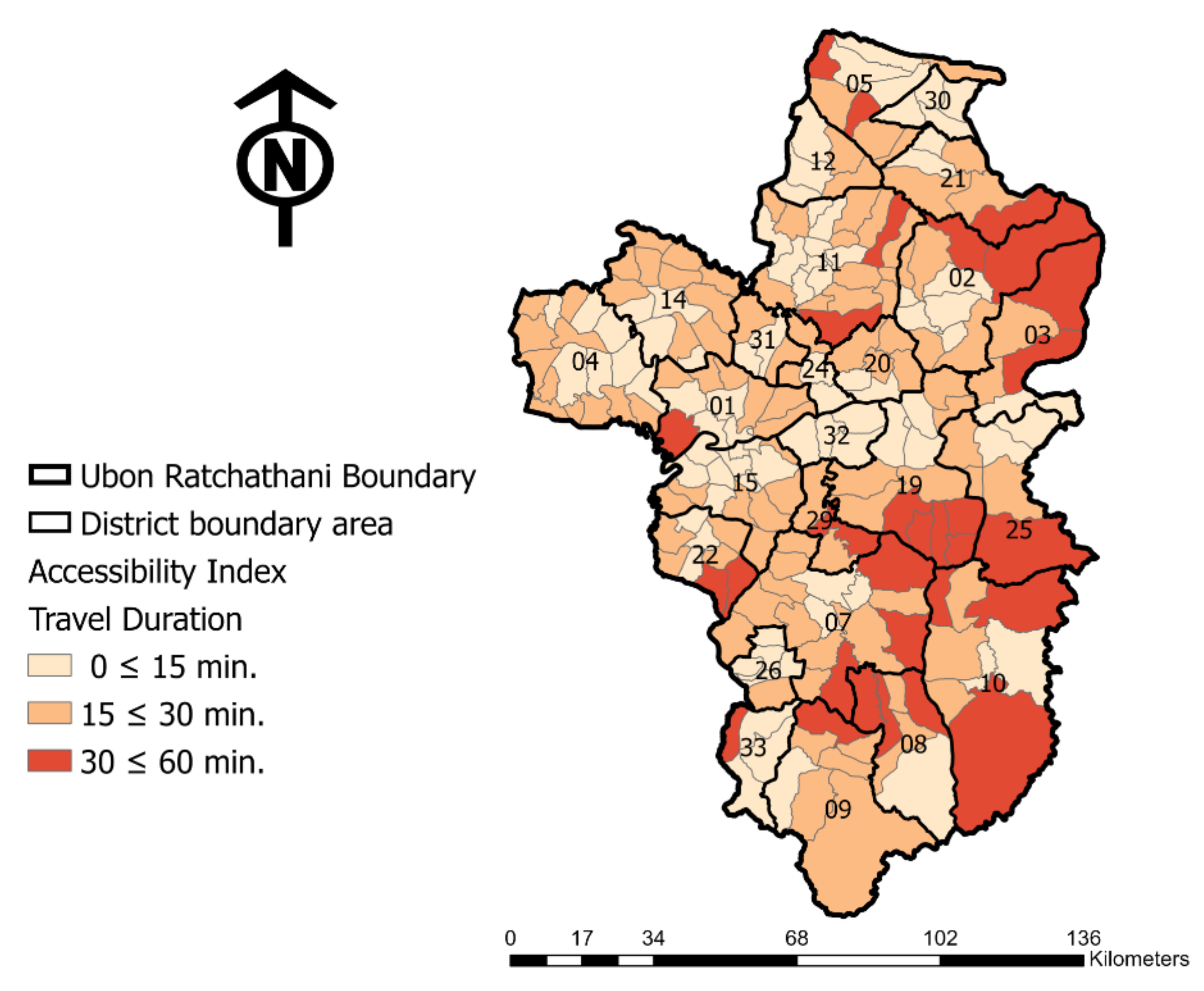
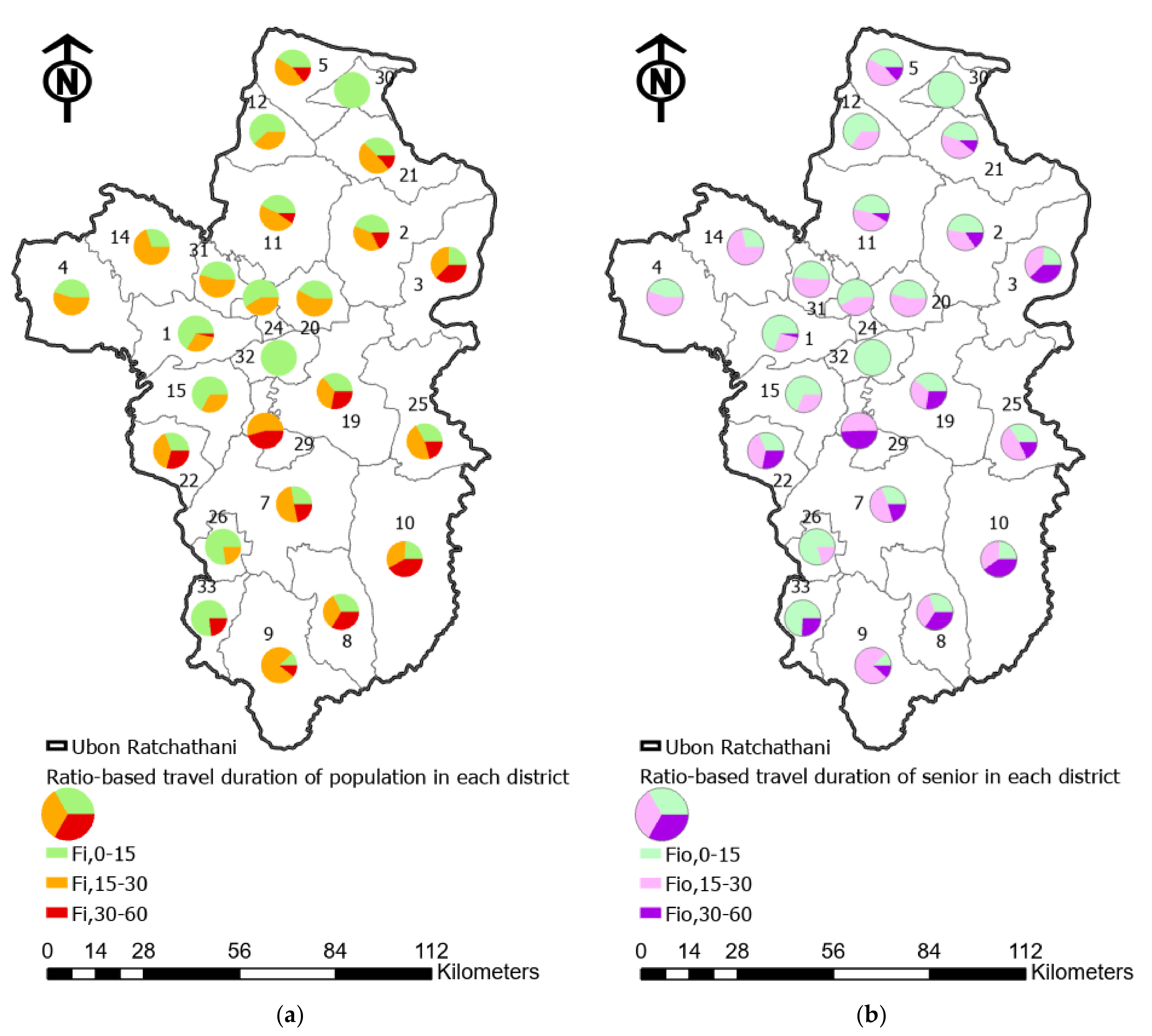
3.2. Spatial Accessibility Analysis
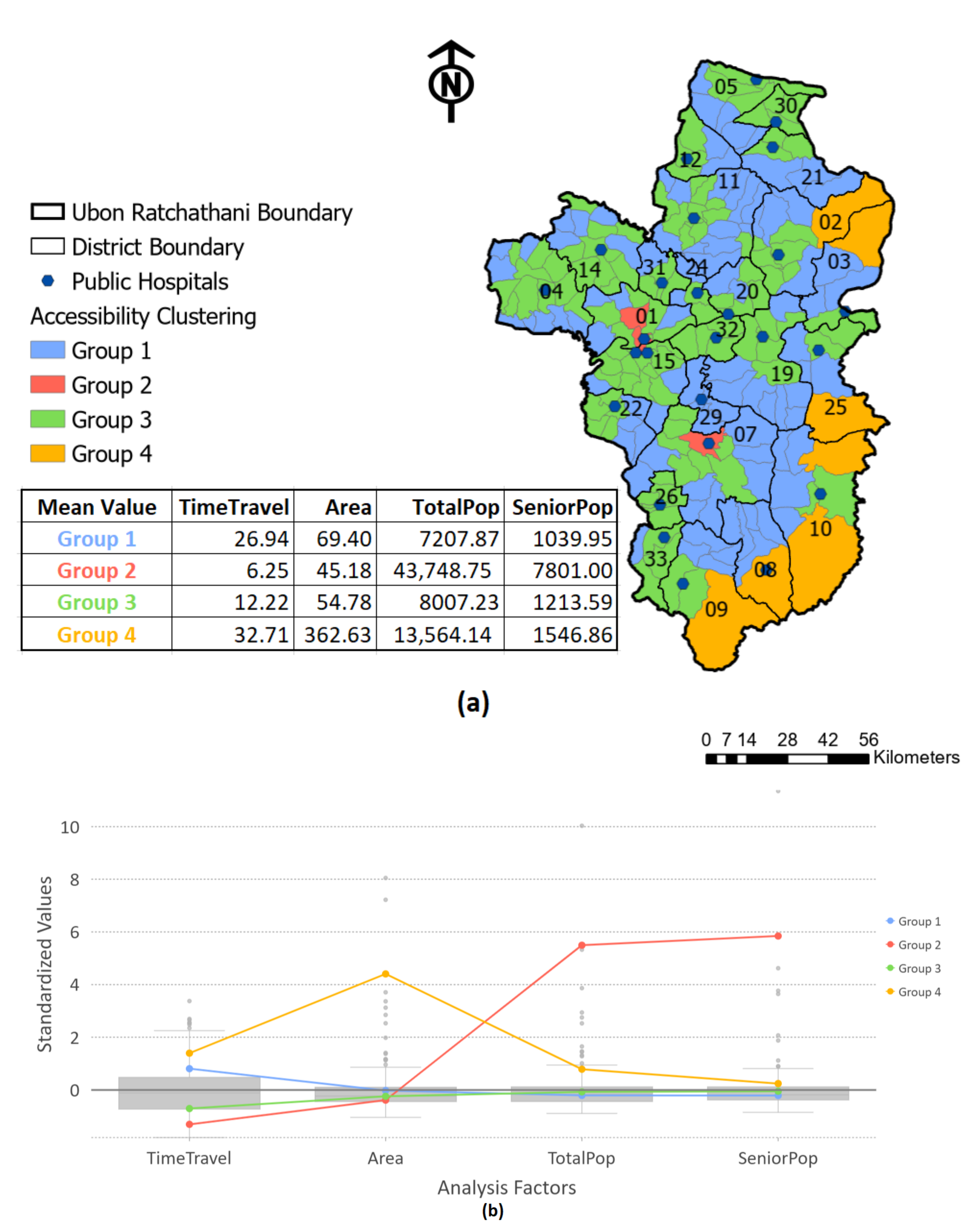
3.3. Healthcare Disparity Assessment
4. Discussion
4.1. Overall Assessment of Spatial Accessibility of Healthcare Facilities
4.2. Disparity Assessment of Healthcare Service Distribution
4.3. Limitations of This Study
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schuller, K.A.; Cronin, C.E.; Nicks, S.E.; Jing, X.; Kingori, C.; Morrone, M. Development and application of a rubric to compare strategies for improving access to health care in rural communities in the United States. Eval. Program Plan. 2019, 74, 61–68. [Google Scholar] [CrossRef]
- Peters, D.H.; Garg, A.; Bloom, G.; Walker, D.G.; Brieger, W.R.; Hafizur Rahman, M. Poverty and access to health care in developing countries. Ann. N. Y. Acad. Sci. 2008, 1136, 161–171. [Google Scholar] [CrossRef]
- Sekhri, N.; Feachem, R.; Ni, A. Public-Private Integrated Partnerships Demonstrate The Potential To Improve Health Care Access, Quality, And Efficiency. Health Aff. 2011, 30, 1498–1507. [Google Scholar] [CrossRef]
- Voss, M.; Marten, R.; Gulati, D. Accelerating the SDG3 Global Action Plan. BMJ Glob. Health 2019, 4, e001930. [Google Scholar] [CrossRef] [PubMed]
- European Commision. Delivering the Sustainable Development Goals at Local and Regional Level; European Commission: Brussels, Belgium, 2018. [Google Scholar]
- Walt, G.; Gilson, L. Reforming the health sector in developing countries: The central role of policy analysis. Health Policy Plan 1994, 9, 353–370. [Google Scholar] [CrossRef] [PubMed]
- Hennink, M.; Stephenson, R. Using research to inform health policy: Barriers and strategies in developing countries. J. Health Commun. 2005, 10, 163–180. [Google Scholar] [CrossRef]
- Duong, D.V.; Binns, C.W.; Lee, A.H. Utilization of delivery services at the primary health care level in rural Vietnam. Soc. Sci. Med. 2004, 59, 2585–2595. [Google Scholar] [CrossRef] [PubMed]
- Lane, J.; Andrews, G.; Orange, E.; Brezak, A.; Tanna, G.; Lebese, L.; Carter, T.; Naidoo, E.; Levendal, E.; Katz, A. Strengthening health policy development and management systems in low- and middle- income countries: South Africa’s approach. Health Policy OPEN 2020, 1, 100010. [Google Scholar] [CrossRef]
- Stierman, E.K.; Kalbarczyk, A.; Oo, H.N.L.; Koller, T.S.; Peters, D.H. Assessing Barriers to Effective Coverage of Health Services for Adolescents in Low- and Middle-Income Countries: A Scoping Review. J. Adolesc. Health 2021, 69, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Campos, M.M.; Olmstead-Rose, L. Mobile Health Clinics: Increasing Access to Care in Central and Eastern Contra Costa County; La Piana Consulting: Emeryville, CA, USA, 2012. [Google Scholar]
- Carmack, H.J.; Bouchelle, Z.; Rawlins, Y.; Bennet, J.; Hill, C.; Oriol, N.E. Mobilizing a Narrative of Generosity: Patient Experiences on an Urban Mobile Health Clinic. Commun. Q. 2017, 65, 419–435. [Google Scholar] [CrossRef]
- Geoffroy, E.; Harries, A.D.; Bissell, K.; Schell, E.; Bvumbwe, A.; Tayler-Smith, K.; Kizito, W. Bringing care to the community: Expanding access to health care in rural Malawi through mobile health clinics. Public Health Action 2014, 4, 252–258. [Google Scholar] [CrossRef]
- US Department of Health and Human Services; Office of Minority Health. Mobile Health Clinics in the United States: Reducing Disparities: Improving Care, Improving Health, Controlling Costs; US Department of Health and Human Services: Washington, DC, USA, 2013.
- Mobilehealthmap.org. Mobile Health Map: Impact Report. Available online: https://www.mobilehealthmap.org/impact-report (accessed on 28 September 2021).
- Hill, C.F.; Powers, B.W.; Jain, S.H.; Bennet, J.; Vavasis, A.; Oriol, N.E. Mobile health clinics in the era of reform. Am. J. Manag Care 2014, 20, 261–264. [Google Scholar]
- Swabri, J.; Uzor, C.; Laird, E.; O’Carroll, A. Health status of the homeless in Dublin: Does the mobile health clinic improve access to primary healthcare for its users? Ir. J. Med. Sci. 2019, 188, 545–554. [Google Scholar] [CrossRef]
- Rafferty, R. Creating a Sustainable Model for Improved Utilization of a Mobile Health Clinic in Nashville, TN; PCLP: Nashville, TN, USA, 2016. [Google Scholar]
- Malone, N.C.; Williams, M.M.; Fawzi, M.C.S.; Bennet, J.; Hill, C.; Katz, J.N.; Oriol, N.E. Mobile health clinics in the United States. Int. J. Equity Health 2020, 19, 40. [Google Scholar] [CrossRef] [PubMed]
- Stephanie, W.; Hill, C.; Ricks, M.L.; Bennet, J.; Oriol, N.E. The scope and impact of mobile health clinics in the United States: A literature review. Int. J. Equity Health 2017, 16, 178. [Google Scholar]
- Penchansky, R.; Thomas, J.W. The concept of access: Definition and relationship to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Whippo, T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place 2012, 18, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Hawthorne, T.L.; Kwan, M.P. Using GIS and perceived distance to understand the unequal geographies of healthcare in lower-income urban neighbourhoods. Geogr. J. 2012, 178, 18–30. [Google Scholar] [CrossRef] [PubMed]
- McLafferty, S.L. GIS and health care. Annu. Rev. Public Health 2003, 24, 25–42. [Google Scholar] [CrossRef] [PubMed]
- Calovi, M.; Seghieri, C. Using a GIS to support the spatial reorganization of outpatient care services delivery in Italy. BMC Health Serv. Res. 2018, 18, 883. [Google Scholar] [CrossRef]
- Cheng, L.; Yang, M.; De Vos, J.; Witlox, F. Examining geographical accessibility to multi-tier hospital care services for the elderly: A focus on spatial equity. J. Transp. Health 2020, 19, 100926. [Google Scholar] [CrossRef]
- Ashiagbor, G.; Ofori-Asenso, R.; Forkuo, E.K.; Agyei-Frimpong, S. Measures of geographic accessibility to health care in the Ashanti Region of Ghana. Sci. Afr. 2020, 9, e00453. [Google Scholar] [CrossRef]
- Padeiro, M. Geographical accessibility to community pharmacies by the elderly in metropolitan Lisbon. Res. Soc. Adm. Pharm. 2018, 14, 653–662. [Google Scholar] [CrossRef]
- Kelly, C.; Hulme, C.; Farragher, T.; Clarke, G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open 2016, 6, e013059. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, J.C.; Cramb, S.M.; McGree, J.M.; Dunn, N.A.; Baade, P.D.; Mengersen, K.L. Geographic variation in the intended choice of adjuvant treatments for women diagnosed with screen-detected breast cancer in Queensland. BMC Public Health 2015, 15, 1204. [Google Scholar] [CrossRef]
- Gilbert, S.M.; Pow-Sang, J.M.; Xiao, H. Geographical Factors Associated with Health Disparities in Prostate Cancer. Cancer Control. 2016, 23, 401–408. [Google Scholar] [CrossRef]
- Fayet, Y.; Coindre, J.M.; Dalban, C.; Gouin, F.; De Pinieux, G.; Farsi, F.; Ducimetière, F.; Chemin-Airiau, C.; Jean-Denis, M.; Chabaud, S.; et al. Geographical Accessibility of the Referral Networks in France. Intermediate Results from the IGéAS Research Program. Int. J. Environ. Res. Public Health 2018, 15, 2204. [Google Scholar] [CrossRef]
- Huotari, T.; Rusanen, J.; Keistinen, T.; Lähderanta, T.; Ruha, L.; Sillanpää, M.J.; Antikainen, H. Effect of centralization on geographic accessibility of maternity hospitals in Finland. BMC Health Serv. Res. 2020, 20, 337. [Google Scholar] [CrossRef]
- Grineski, S.; Morales, D.X.; Collins, T.; Wilkes, J.; Bonkowsky, J.L. Geographic and Specialty Access Disparities in US Pediatric Leukodystrophy Diagnosis. J. Pediatr. 2020, 220, 193–199. [Google Scholar] [CrossRef]
- McEvoy, C.S.; Ross-Li, D.; Norris, E.A.; Ricca, R.L.; Gow, K.W. From far and wide: Geographic distance to pediatric surgical care across Canada. J. Pediatr. Surg. 2020, 55, 908–912. [Google Scholar] [CrossRef]
- Costa, C.; Tenedório, J.A.; Santana, P. Disparities in Geographical Access to Hospitals in Portugal. ISPRS Int. J. Geo-Inf. 2020, 9, 567. [Google Scholar] [CrossRef]
- Bates, J.E.; Parekh, A.D.; Chowdhary, M.; Amdur, R.J. Geographic Distribution of Radiation Oncologists in the United States. Pract. Radiat. Oncol. 2020, 10, e436–e443. [Google Scholar] [CrossRef]
- Kirch, D.G.; Henderson, M.K.; Dill, M.J. Physician workforce projections in an era of health care reform. Annu. Rev. Med. 2012, 63, 435–445. [Google Scholar] [CrossRef]
- Zhang, X.; Lin, D.; Pforsich, H.; Lin, V.W. Physician workforce in the United States of America: Forecasting nationwide shortages. Hum. Resour. Health 2020, 18, 8. [Google Scholar] [CrossRef] [PubMed]
- Guimarães, T.; Lucas, K.; Timms, P. Understanding how low-income communities gain access to healthcare services: A qualitative study in São Paulo, Brazil. J. Transp. Health 2019, 15, 100658. [Google Scholar] [CrossRef]
- Luo, X.; Zheng, R.; Jin, X.; Sun, Y.; Chen, L.; Peng, J.; Huang, X.; Tian, X.; Mei, L. Barriers to Adolescent Health Care in Maternal and Children’s Healthcare Hospitals: Based on a National Survey in China. J. Adolesc. Health 2020, 67, S32–S37. [Google Scholar] [CrossRef]
- Tuson, M.; Yap, M.; Kok, M.R.; Boruff, B.; Murray, K.; Vickery, A.; Turlach, B.A.; Whyatt, D. Overcoming inefficiencies arising due to the impact of the modifiable areal unit problem on single-aggregation disease maps. Int. J. Health Geogr. 2020, 19, 40. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef]
- Khan, M.M.; Ali, D.; Ferdousy, Z.; Al-Mamun, A. A cost-minimization approach to planning the geographical distribution of health facilities. Health Policy Plan. 2001, 16, 264–272. [Google Scholar] [CrossRef][Green Version]
- Murad, A.A. Using geographical information systems for defining the accessibility to health care facilities in Jeddah City, Saudi Arabia. Geospat. Health 2014, 8, S661–S669. [Google Scholar] [CrossRef]
- Dos Anjos Luis, A.; Cabral, P. Geographic accessibility to primary healthcare centers in Mozambique. Int. J. Equity Health 2016, 15, 173. [Google Scholar] [CrossRef]
- Jones, S.G.; Ashby, A.J.; Momin, S.R.; Naidoo, A. Spatial implications associated with using Euclidean distance measurements and geographic centroid imputation in health care research. Health Serv. Res. 2010, 45, 316–327. [Google Scholar] [CrossRef]
- Kadobera, D.; Sartorius, B.; Masanja, H.; Mathew, A.; Waiswa, P. The effect of distance to formal health facility on childhood mortality in rural Tanzania, 2005–2007. Glob. Health Action 2012, 5, 19099. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Adams, A.M.; Islam, R.; Hasan, S.M.; Panciera, R. Impact of traffic variability on geographic accessibility to 24/7 emergency healthcare for the urban poor: A GIS study in Dhaka, Bangladesh. PLoS ONE 2019, 14, e0222488. [Google Scholar] [CrossRef] [PubMed]
- Evandrou, M.; Falkingham, J.; Le Grand, J.; Winter, D. Equity in health and social care. J. Soc. Policy 1992, 21, 489–523. [Google Scholar] [CrossRef]
- Campbell, S.M.; Roland, M.O.; Buetow, S.A. Defining quality of care. Soc. Sci. Med. 2000, 51, 1611–1625. [Google Scholar] [CrossRef]
- Keeves, J.; Braaf, S.C.; Ekegren, C.L.; Beck, B.; Gabbe, B.J. Access to Healthcare Following Serious Injury: Perspectives of Allied Health Professionals in Urban and Regional Settings. Int. J. Environ. Res. Public Health 2021, 18, 1230. [Google Scholar] [CrossRef] [PubMed]
- Habib, S.S.; Jamal, W.Z.; Zaidi, S.M.A.; Siddiqui, J.-U.-R.; Khan, H.M.; Creswell, J.; Batra, S.; Versfeld, A. Barriers to Access of Healthcare Services for Rural Women—Applying Gender Lens on TB in a Rural District of Sindh, Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 10102. [Google Scholar] [CrossRef]
- Ingram, D.R. The concept of accessibility: A search for an operational form. Reg. Stud. 1971, 5, 101–107. [Google Scholar] [CrossRef]
- Ashik, F.R.; Mim, S.A.; Neema, M.N. Towards vertical spatial equity of urban facilities: An integration of spatial and aspatial accessibility. J. Urban. Manag. 2020, 9, 77–92. [Google Scholar] [CrossRef]
- Deborah, O.M.L.; Chiu, M.Y.L.; Cao, K. Geographical Accessibility of Community Health Assist System General Practitioners for the Elderly Population in Singapore: A Case Study on the Elderly Living in Housing Development Board Flats. Int. J. Environ. Res. Public Health 2018, 15, 1988. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Meyer, P.; Jin, L. Spatial access to health care and elderly ambulatory care sensitive hospitalizations. Public Health 2019, 169, 76–83. [Google Scholar] [CrossRef]
- Wu, H.C.; Tseng, M.H. Evaluating Disparities in Elderly Community Care Resources: Using a Geographic Accessibility and Inequality Index. Int. J. Environ. Res. Public Health 2018, 15, 1353. [Google Scholar] [CrossRef] [PubMed]
- Goodridge, D.; Marciniuk, D. Rural and remote care: Overcoming the challenges of distance. Chronic Respir. Dis. 2016, 13, 192–203. [Google Scholar] [CrossRef]
- Strasser, R.; Kam, S.M.; Regalado, S.M. Rural Health Care Access and Policy in Developing Countries. Annu. Rev. Public Health 2016, 37, 395–412. [Google Scholar] [CrossRef] [PubMed]
- Rostampour, M.; Nosratnejad, S. A Systematic Review of Equity in Healthcare Financing in Low- and Middle-Income Countries. Value Health Reg. Issues 2020, 21, 133–140. [Google Scholar] [CrossRef]
- Tansley, G.; Schuurman, N.; Amram, O.; Yanchar, N. Spatial Access to Emergency Services in Low- and Middle-Income Countries: A GIS-Based Analysis. PLoS ONE 2015, 10, e0141113. [Google Scholar] [CrossRef]
- Nemet, G.F.; Bailey, A.J. Distance and health care utilization among the rural elderly. Soc. Sci. Med. 2000, 50, 1197–1208. [Google Scholar] [CrossRef]
- Williams, J.S.; Walker, R.J.; Egede, L.E. Achieving Equity in an Evolving Healthcare System: Opportunities and Challenges. Am. J. Med. Sci. 2016, 351, 33–43. [Google Scholar] [CrossRef]
- Dijkstra, E.W. A note on two problems in connexion with graphs. Numer. Math. 1959, 1, 269–271. [Google Scholar] [CrossRef]
- Witchayaphong, P.; Pravinvongvuth, S.; Kanitpong, K.; Sano, K.; Horpibulsuk, S. Influential Factors Affecting Travelers’ Mode Choice Behavior on Mass Transit in Bangkok, Thailand. Sustainability 2020, 12, 9522. [Google Scholar] [CrossRef]
- Limanond, T.; Butsingkorn, T.; Chermkhunthod, C. Travel behavior of university students who live on campus: A case study of a rural university in Asia. Transp. Policy 2011, 18, 163–171. [Google Scholar] [CrossRef]
- Royal Thai Government Gazette. Ministerial Rule: Set Vehicle Speed on National or Rural Roads. Available online: http://www.ratchakitcha.soc.go.th/DATA/PDF/2564/A/017/T_0003.PDF?fbclid=IwAR0QNmRRiZCGg6AWx9XaZmFCWlD2LSIaP8gKqvsDOi3SyGppkbIISjZ-pLg (accessed on 7 October 2021).
- Vanderschuren, M.; McKune, D. Emergency care facility access in rural areas within the golden hour?: Western Cape case study. Int. J. Health Geogr. 2015, 14, 5. [Google Scholar] [CrossRef] [PubMed]
- Bosanac, E.M.; Parkinson, R.C.; Hall, D.S. Geographic access to hospital care: A 30-minute travel time standard. Med. Care 1976, 14, 616–624. [Google Scholar] [CrossRef]
- McCarthy, S.; Moore, D.; Smedley, W.A.; Crowley, B.M.; Stephens, S.W.; Griffin, R.L.; Tanner, L.C.; Jansen, J.O. Impact of Rural Hospital Closures on Health-Care Access. J. Surg. Res. 2021, 258, 170–178. [Google Scholar] [CrossRef]
- Ubon Ratchathani Provincial Statistical Office. Ubon Ratchathani Provincial Statistical Report: 2017; Ubon Ratchathani Provincial Statistical Office: Ubon Ratchathani, Thailand, 2017.
- National Statistic Office. Report on the 2017 Survey of the Older Persons in Thailand; National Statistic Office: Laksi Bangkok, Thailand, 2017; p. 266.
- Luevisadpaibul, S.; Tanundet, N.; Warisarn, P.; Kamsan, R.; Teeraleekul, W.; Charoenwai, W. The Effect of Communities Based Rehabilitation for Disabled Persons in Ubon Ratchathani Province. J. Health Sci. 2017, 22, 82–89. [Google Scholar]
- Singhard, S.; Kittiworavej, S.; Meenakate, P.; Suriya, A. Cognitive Function and Functional Ability of Older People, Elderly School, Faculty of Nursing, Ubon Ratchathani University. J. Health Sci. 2021, 30, 242–250. [Google Scholar]
- Woratanarat, T.; Woratanarat, P.; Lekthip, C. Primary Health Care Systems: Case Study of Thailand; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Yingtaweesak, T.; Yoshida, Y.; Hemhongsa, P.; Hamajima, N.; Chaiyakae, S. Accessibility of health care service in Thasongyang, Tak Province, Thailand. Nagoya J. Med. Sci. 2013, 75, 243–250. [Google Scholar] [PubMed]
- Ministry of Public Health. Thailand Health Profile 2016–2017; Ministry of Public Health: Bangkok, Thailand, 2019.
- Janssen, P. Thailand’s Expanding State ‘Threatens Future Growth’. Available online: https://asia.nikkei.com/Politics-Economy/Economy/Thailand-s-expanding-state-threatens-future-growth (accessed on 29 September 2021).
- Head, J. Life and Death on Thailand’s Lethal Roads. Available online: https://www.bbc.com/news/world-asia-38660283 (accessed on 30 September 2021).
- Manakitsomboon, H. Share of Respondents That Own a Car in Thailand in 2019. Available online: https://www.statista.com/statistics/1027960/thailand-car-ownership-among-consumers/#statisticContainer (accessed on 29 September 2021).
- Department of Land Transport. Department of Land Transport Revealing the Statistics of New Car Registrations. Available online: https://www.dlt.go.th/th/public-news/view.php?_did=2806 (accessed on 29 September 2021).
- Tangcharoensathien, V.; Witthayapipopsakul, W.; Panichkriangkrai, W.; Patcharanarumol, W.; Mills, A. Health systems development in Thailand: A solid platform for successful implementation of universal health coverage. Lancet 2018, 391, 1205–1223. [Google Scholar] [CrossRef]
- Suraratdecha, C.; Saithanu, S.; Tangcharoensathien, V. Is universal coverage a solution for disparities in health care?: Findings from three low-income provinces of Thailand. Health Policy 2005, 73, 272–284. [Google Scholar] [CrossRef] [PubMed]
- Dilokthornsakul, P.; Lee, T.A.; Dhippayom, T.; Jeanpeerapong, N.; Chaiyakunapruk, N. Comparison of Health Care Utilization and Costs for Patients with Asthma by Severity and Health Insurance in Thailand. Value Health Reg. Issues 2016, 9, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Chandoevwit, W.; Phatchana, P. Inpatient care expenditure of the elderly with chronic diseases who use public health insurance: Disparity in their last year of life. Soc. Sci. Med. 2018, 207, 64–70. [Google Scholar] [CrossRef]
- Quashie, N.T.; Pothisiri, W. Rural-urban gaps in health care utilization among older Thais: The role of family support. Arch. Gerontol. Geriatr. 2019, 81, 201–208. [Google Scholar] [CrossRef]
- Ghezzi, E.M.; Kobayashi, K.; Park, D.-Y.; Srisilapanan, P. Oral healthcare systems for an ageing population: Concepts and challenges. Int. Dent. J. 2017, 67, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Official Statistics Registration Systems. Population Data 2020. Available online: https://stat.bora.dopa.go.th/stat/xstat/new/6312/6312cc34.txt (accessed on 5 May 2021).
- Pailoplee, S. mitrearth.org. Available online: http://www.mitrearth.org/ (accessed on 5 December 2020).
- Ministry of Public Health. Information of Health Service in Ubon Ratchathani Province; Ministry of Public Health: Bangkok, Thailand, 2020.
- Health Data Center. Number of Health Personnel; Health Data Center: Bangkok, Thailand, 2020. [Google Scholar]
- Condeço-Melhorado, A.; Christidis, P. Road Accessibility in Border Regions: A JoInt. Approach. Netw. Spat. Econ. 2018, 18, 363–383. [Google Scholar] [CrossRef]
- Buchmueller, T.C.; Jacobson, M.; Wold, C. How far to the hospital?: The effect of hospital closures on access to care. J. Health Econ. 2006, 25, 740–761. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Jeong, M.H.; Park, K.-H.; Lee, M.G.; Ko, J.S.; Sim, D.S.; Yoon, N.S.; Yoon, H.J.; Hong, Y.J.; Park, H.W.; et al. AS-107: Clinical Effects of Distance Between Home and Hospital on Mortality in Patients with Acute Myocardial Infarction. Am. J. Cardiol. 2010, 105, 45A. [Google Scholar] [CrossRef]
- Burkey, M.L.; Bhadury, J.; Eiselt, H.A.; Toyoglu, H. The impact of hospital closures on geographical access: Evidence from four southeastern states of the United States. Oper. Res. Perspect. 2017, 4, 56–66. [Google Scholar] [CrossRef]
- Jomnonkwao, S.; Sangphong, O.; Khampirat, B.; Siridhara, S.; Ratanavaraha, V. Public transport promotion policy on campus: Evidence from Suranaree University in Thailand. Public Transp. 2016, 8, 185–203. [Google Scholar] [CrossRef]
- Johnson, A.; Booker, S.Q. Population-Focused Approaches for Proactive Chronic Pain Management in Older Adults. Pain Manag. Nurs. 2021. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Dwivedi, P.; Singh Rawat, A.K.; Dwivedi, A.K. 3—Nutrition nutraceuticals: A proactive approach for healthcare. In Nutraceuticals; Grumezescu, A.M., Ed.; Academic Press: Cambridge, MA, USA, 2016; pp. 79–116. [Google Scholar]
- Tanaka, K.; Iwasawa, M. Aging in rural Japan—Limitations in the current social care policy. J. Aging Soc. Policy 2010, 22, 394–406. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Yang, K.; Chu, S.H.; Youm, Y.; Kim, H.C.; Park, Y.-R.; Son, Y.-J. Social Activities and Health-Related Quality of Life in Rural Older Adults in South Korea: A 4-Year Longitudinal Analysis. Int. J. Environ. Res. Public Health 2020, 17, 5553. [Google Scholar] [CrossRef] [PubMed]

| Data Information | Geographical Level | Year | Source | Data Type | Application |
|---|---|---|---|---|---|
| Population data | Province | 2020 | The official statistics of Thailand | Text file | Spatial distribution analysis |
| District | |||||
| Sub-district | |||||
| GIS-boundary data | Province boundary | 2020 | mitrearth.org | Shape file | Boundary of study area |
| District boundary | |||||
| Sub-district boundary | |||||
| Healthcare data | Province | 2020 | The Open Government Data of Thailand | CSV file | Spatial distribution analysis |
| Health personnel data | Province | 2020 | Health Data Center | CSV file | Spatial distribution analysis |
| Information of Study Area | Amount | |
|---|---|---|
| Ubon Ratchathani information | Area (km2) | 15,487 |
| Population density (people/km2) | 120.53 | |
| Number of district areas | 25 | |
| Number of sub-district areas | 219 | |
| Population information | Total population | 1,866,697 |
| Male | 930,904 | |
| Female | 934,297 | |
| Senior population | 278,901 | |
| Male | 156,208 | |
| Female | 122,693 | |
| The lowest administrative level: sub-district | Min.–max. area (km2) | 1.91–604.09 |
| Average area (km2) | 70.72 | |
| Min.–max. population | 2816–72,855 | |
| Average population | 8524 | |
| Healthcare Information | Number of public hospitals | 26 |
| Number of physicians | 2327 | |
| Number of nurses | 2206 | |
| Access Duration (min) (t) | Number of Sub- district | Area (km2) | % Area | Estimated Population | % Population | Estimated Senior | % Senior Population |
|---|---|---|---|---|---|---|---|
| 0 ≤ 15 | 85 | 4827 | 31.2% | 844,393 | 45.2% | 132,967 | 15.75% |
| 15 ≤ 30 | 104 | 6964 | 45.0% | 768,502 | 41.2% | 112,400 | 14.63% |
| 30 ≤ 60 | 30 | 3696 | 23.9% | 253,802 | 13.6% | 33,534 | 13.21% |
| District no. | Total District Area (km2) | Number of Sub- Districts | The District Population-Weighted Time to Reach Healthcare Facilities | Area Ratio of Each District Area (Si,t) | ||
|---|---|---|---|---|---|---|
| (min.) | ||||||
| 1 | 561.8 | 12 | 18.74 | 34.1% | 51.6% | 14.3% |
| 2 | 947.9 | 11 | 28.54 | 26.7% | 33.3% | 40.0% |
| 3 | 718.4 | 5 | 33.22 | 16.3% | 29.8% | 53.9% |
| 4 | 861.9 | 18 | 18.82 | 46.8% | 53.2% | 0.0% |
| 5 | 603.0 | 9 | 23.11 | 40.4% | 43.4% | 16.2% |
| 7 | 1260.7 | 16 | 26.85 | 12.9% | 57.7% | 29.3% |
| 8 | 650.2 | 6 | 29.00 | 45.2% | 19.3% | 35.5% |
| 9 | 1038.0 | 7 | 26.46 | 11.3% | 79.8% | 8.9% |
| 10 | 1485.1 | 8 | 29.25 | 16.3% | 22.8% | 60.9% |
| 11 | 1020.4 | 23 | 23.09 | 30.9% | 53.1% | 16.1% |
| 12 | 346.9 | 5 | 18.98 | 61.5% | 38.5% | 0.0% |
| 14 | 727.5 | 14 | 19.33 | 29.0% | 71.0% | 0.0% |
| 15 | 613.5 | 16 | 16.12 | 47.2% | 52.8% | 0.0% |
| 19 | 950.5 | 14 | 27.11 | 22.7% | 46.1% | 31.1% |
| 20 | 311.6 | 6 | 16.86 | 27.2% | 72.8% | 0.0% |
| 21 | 554.0 | 6 | 26.21 | 17.6% | 58.2% | 24.2% |
| 22 | 388.4 | 9 | 25.15 | 24.8% | 46.9% | 28.3% |
| 24 | 184.8 | 4 | 20.75 | 55.2% | 44.8% | 0.0% |
| 25 | 766.7 | 6 | 25.05 | 23.1% | 35.6% | 41.2% |
| 26 | 215.6 | 5 | 12.25 | 68.3% | 31.7% | 0.0% |
| 29 | 248.1 | 3 | 29.15 | 0.0% | 66.2% | 33.8% |
| 30 | 218.7 | 4 | 10.03 | 100.0% | 0.0% | 0.0% |
| 31 | 230.5 | 4 | 15.98 | 43.7% | 56.3% | 0.0% |
| 32 | 264.8 | 4 | 13.05 | 100.0% | 0.0% | 0.0% |
| 33 | 318.2 | 4 | 21.43 | 84.4% | 0.0% | 15.6% |
| District no. | Ratio of Estimated Population in Each District | Ratio of Estimated Senior in Each District | ||||
|---|---|---|---|---|---|---|
| 1 | 66.6% | 30.0% | 3.4% | 69.3% | 27.0% | 3.7% |
| 2 | 44.0% | 38.4% | 17.6% | 47.7% | 36.7% | 15.6% |
| 3 | 24.8% | 37.8% | 37.3% | 24.0% | 38.2% | 37.7% |
| 4 | 45.5% | 54.5% | 0.0% | 44.3% | 55.7% | 0.0% |
| 5 | 41.0% | 44.2% | 14.8% | 42.3% | 44.5% | 13.2% |
| 7 | 27.8% | 50.6% | 21.6% | 30.8% | 48.8% | 20.4% |
| 8 | 32.5% | 33.9% | 33.6% | 30.5% | 35.2% | 34.3% |
| 9 | 12.0% | 77.4% | 10.6% | 11.9% | 76.6% | 11.6% |
| 10 | 24.2% | 34.0% | 41.7% | 24.5% | 35.4% | 40.1% |
| 11 | 43.1% | 47.2% | 9.7% | 46.6% | 45.1% | 8.3% |
| 12 | 61.9% | 38.1% | 0.0% | 65.5% | 34.5% | 0.0% |
| 14 | 30.0% | 70.0% | 0.0% | 27.8% | 72.2% | 0.0% |
| 15 | 67.4% | 32.6% | 0.0% | 68.5% | 31.5% | 0.0% |
| 19 | 36.2% | 35.8% | 28.1% | 38.9% | 34.0% | 27.1% |
| 20 | 42.8% | 57.2% | 0.0% | 45.6% | 54.4% | 0.0% |
| 21 | 37.6% | 48.8% | 13.5% | 44.9% | 44.0% | 11.1% |
| 22 | 30.8% | 39.8% | 29.3% | 31.2% | 40.6% | 28.2% |
| 24 | 58.6% | 41.4% | 0.0% | 57.9% | 42.1% | 0.0% |
| 25 | 33.0% | 46.4% | 20.6% | 34.1% | 47.8% | 18.2% |
| 26 | 77.4% | 22.6% | 0.0% | 79.8% | 20.2% | 0.0% |
| 29 | 0.0% | 54.5% | 45.5% | 0.0% | 50.8% | 49.2% |
| 30 | 100.0% | 0.0% | 0.0% | 100.0% | 0.0% | 0.0% |
| 31 | 45.9% | 54.1% | 0.0% | 47.6% | 52.4% | 0.0% |
| 32 | 100.0% | 0.0% | 0.0% | 100.0% | 0.0% | 0.0% |
| 33 | 77.0% | 0.0% | 23.0% | 74.3% | 0.0% | 25.7% |
| Analysis Factor | Mean | Standard Deviation | Min. | Max. | R2 |
|---|---|---|---|---|---|
| Travel time | 19.03 | 9.78 | 1.35 | 52.10 | 0.6338 |
| Area | 70.72 | 66.11 | 1.91 | 604.09 | 0.6563 |
| Total population | 8523.73 | 6398.12 | 2816 | 72,855 | 0.5943 |
| Senior population | 1273.52 | 1113.94 | 324 | 13,950 | 0.6492 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sritart, H.; Tuntiwong, K.; Miyazaki, H.; Taertulakarn, S. Disparities in Healthcare Services and Spatial Assessments of Mobile Health Clinics in the Border Regions of Thailand. Int. J. Environ. Res. Public Health 2021, 18, 10782. https://doi.org/10.3390/ijerph182010782
Sritart H, Tuntiwong K, Miyazaki H, Taertulakarn S. Disparities in Healthcare Services and Spatial Assessments of Mobile Health Clinics in the Border Regions of Thailand. International Journal of Environmental Research and Public Health. 2021; 18(20):10782. https://doi.org/10.3390/ijerph182010782
Chicago/Turabian StyleSritart, Hiranya, Kuson Tuntiwong, Hiroyuki Miyazaki, and Somchat Taertulakarn. 2021. "Disparities in Healthcare Services and Spatial Assessments of Mobile Health Clinics in the Border Regions of Thailand" International Journal of Environmental Research and Public Health 18, no. 20: 10782. https://doi.org/10.3390/ijerph182010782
APA StyleSritart, H., Tuntiwong, K., Miyazaki, H., & Taertulakarn, S. (2021). Disparities in Healthcare Services and Spatial Assessments of Mobile Health Clinics in the Border Regions of Thailand. International Journal of Environmental Research and Public Health, 18(20), 10782. https://doi.org/10.3390/ijerph182010782








