Indicators to Assess Physical Health of Children and Adolescents in Activity Research—A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search
2.3. Study Selection
2.4. Data Collection and Items
2.5. Synthesis of Results
3. Results
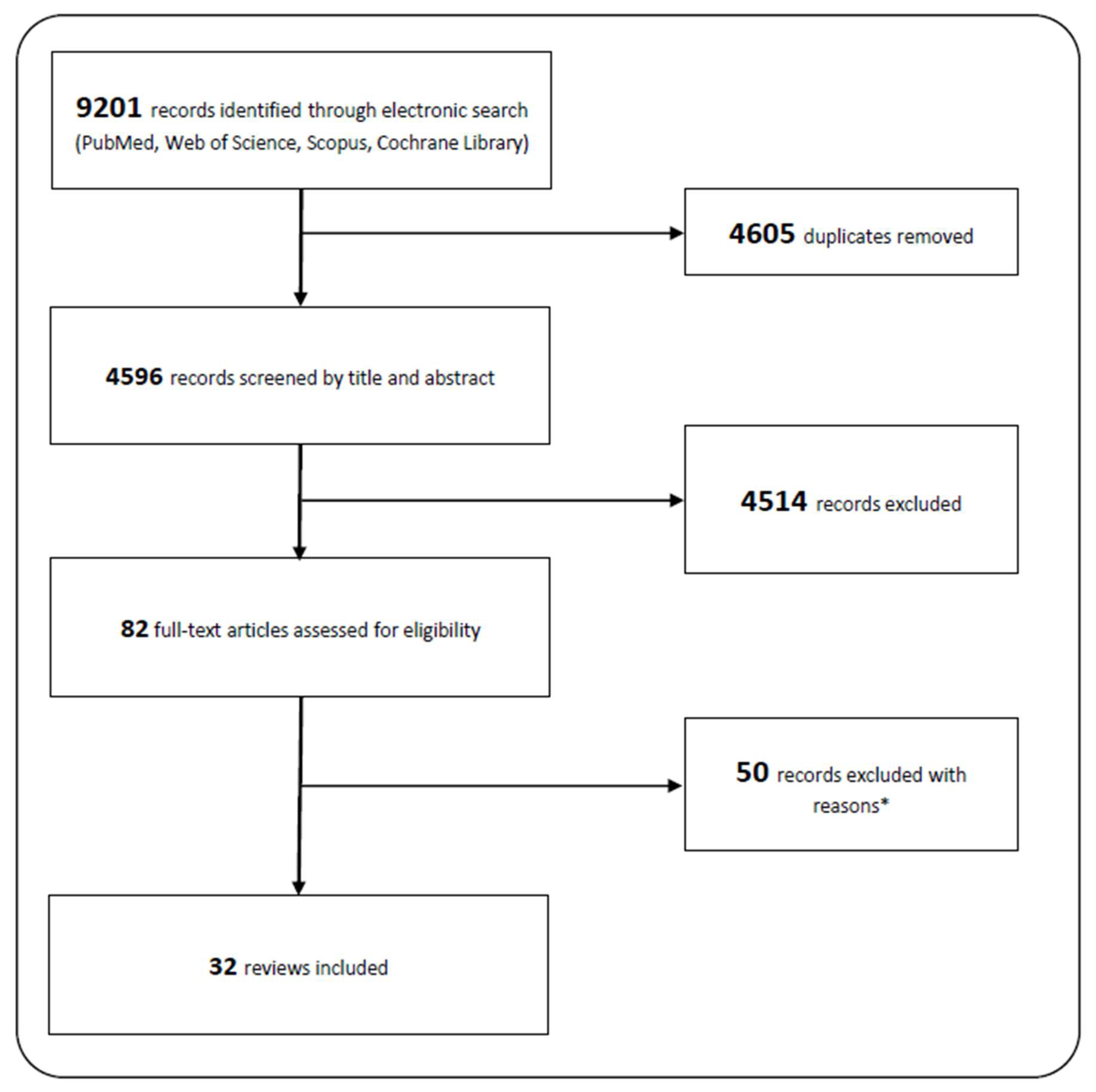
3.1. Electronic Search
3.2. Study Characteristics
3.3. Health Indicators
3.3.1. SR with PA as Exposure
- Body Composition
- Cardiometabolic Biomarkers
- Physical Fitness
- Harms and Injury
- Bone Health
3.3.2. SR with SED as Exposure
- Body Composition
- Cardiometabolic Biomarkers
- Physical Fitness
- Bone Health
3.3.3. SR with PA and SED as Exposure
- Body Composition
- Cardiometabolic Biomarkers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Pescatello, L.S.; Buchner, D.M.; Jakicic, J.M.; Powell, K.E.; Kraus, W.E.; Bloodgood, B.; Campbell, W.W.; Dietz, S.; Dipietro, L.; George, S.M.; et al. Physical Activity to Prevent and Treat Hypertension: A Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1314–1323. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.; Pate, R.R.; Gorber, S.C.; Kho, M.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef] [PubMed]
- Hansen, B.H.; the International Children’s Accelerometry Database (ICAD) Collaborators; Anderssen, S.A.; Andersen, L.B.; Hildebrand, M.; Kolle, E.; Steene-Johannessen, J.; Kriemler, S.; Page, A.S.; Puder, J.; et al. Cross-Sectional Associations of Reallocating Time Between Sedentary and Active Behaviours on Cardiometabolic Risk Factors in Young People: An International Children’s Accelerometry Database (ICAD) Analysis. Sports Med. 2018, 48, 2401–2412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavero-Redondo, I.; Peleteiro, B.; Álvarez-Bueno, C.; Artero, E.G.; Garrido-Miguel, M.; Martinez-Vizcaíno, V. The Effect of Physical Activity Interventions on Glycosylated Haemoglobin (HbA1c) in Non-diabetic Populations: A Systematic Review and Meta-analysis. Sports Med. 2018, 48, 1151–1164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Camhi, S.M.; Katzmarzyk, P. Tracking of cardiometabolic risk factor clustering from childhood to adulthood. Pediatr. Obes. 2010, 5, 122–129. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- MacLean, P.S.; Higgins, J.A.; Giles, E.; Sherk, V.D.; Jackman, M.R. The role for adipose tissue in weight regain after weight loss. Obes. Rev. 2015, 16, 45–54. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, J.A.; Dowda, M.; Pate, R.R.; Kordas, K.; Froberg, K.; Sardinha, L.B.; Kolle, E.; Page, A. Physical Activity and Pediatric Obesity: A Quantile Regression Analysis. Med. Sci. Sports Exerc. 2017, 49, 466–473. [Google Scholar] [CrossRef] [Green Version]
- Herman, K.M.; Craig, C.L.; Gauvin, L.; Katzmarzyk, P.T. Tracking of obesity and physical activity from childhood to adulthood: The Physical Activity Longitudinal Study. Int. J. Pediatr. Obes. 2009, 4, 281–288. [Google Scholar] [CrossRef]
- Janssen, I.; LeBlanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [Green Version]
- Telama, R.; Yang, X.; Viikari, J.; Välimäki, I.; Wanne, O.; Raitakari, O. Physical activity from childhood to adulthood: A 21-year tracking study. Am. J. Prev. Med. 2005, 28, 267–273. [Google Scholar] [CrossRef]
- Telama, R.; Yang, X.; Leskinen, E.; Kankaanpää, A.; Hirvensalo, M.; Tammelin, T.; Viikari, J.S.A.; Raitakari, O.T. Tracking of Physical Activity from Early Childhood through Youth into Adulthood. Med. Sci. Sports Exerc. 2014, 46, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef] [Green Version]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; On Behalf of Sbrn Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, Z.; Chen, S.; Pasco, D.; Pope, Z. A meta-analysis of active video games on health outcomes among children and adolescents. Obes. Rev. 2015, 16, 783–794. [Google Scholar] [CrossRef]
- Gomez-Bruton, A.; Gonzalez-Aguero, A.; Gómez-Cabello, A.; Casajús, J.A.; Vicente-Rodríguez, G. Is Bone Tissue Really Affected by Swimming? A Systematic Review. PLoS ONE 2013, 8, e70119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomez-Bruton, A.; Montero-Marín, J.; González-Agüero, A.; García-Campayo, J.; Moreno, L.A.; Casajús, J.A.; Vicente-Rodríguez, G. The Effect of Swimming During Childhood and Adolescence on Bone Mineral Density: A Systematic Review and Meta-Analysis. Sports Med. 2016, 46, 365–379. [Google Scholar] [CrossRef]
- Guinhouya, B.C.; Samouda, H.; Zitouni, D.; Vilhelm, C.; Hubert, H. Evidence of the influence of physical activity on the metabolic syndrome and/or on insulin resistance in pediatric populations: A systematic review. Pediatr. Obes. 2011, 6, 361–388. [Google Scholar] [CrossRef]
- Henriques-Neto, D.; Peralta, M.; Garradas, S.; Pelegrini, A.; Pinto, A.A.; Sánchez-Miguel, P.A.; Marques, A. Active Commuting and Physical Fitness: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 2721. [Google Scholar] [CrossRef] [Green Version]
- Krahenbühl, T.; Fátima Guimarães, R.D.; Filho, A.D.A.B.; Gonçalves, E.M. Bone geometry and physical activity in children and adolescents: Systematic review. Rev. Paul. Pediatr. 2018, 36, 230–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lubans, D.R.; A Boreham, C.; Kelly, P.; E Foster, C. The relationship between active travel to school and health-related fitness in children and adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 5. [Google Scholar] [CrossRef] [Green Version]
- Miguel-Berges, M.L.; Reilly, J.J.; Aznar, L.A.M.; Jiménez-Pavón, D. Associations Between Pedometer-Determined Physical Activity and Adiposity in Children and Adolescents: Systematic Review. Clin. J. Sport Med. 2018, 28, 64–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramires, V.V.; Dumith, S.C.; Gonçalves, H. Longitudinal Association Between Physical Activity and Body Fat During Adolescence: A Systematic Review. J. Phys. Act. Health 2015, 12, 1344–1358. [Google Scholar] [CrossRef] [PubMed]
- Rauner, A.; Mess, F.; Woll, A. The relationship between physical activity, physical fitness and overweight in adolescents: A systematic review of studies published in or after 2000. BMC Pediatr. 2013, 13, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saunders, L.E.; Green, J.; Petticrew, M.P.; Steinbach, R.; Roberts, H. What Are the Health Benefits of Active Travel? A Systematic Review of Trials and Cohort Studies. PLoS ONE 2013, 8, e69912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sitthipornvorakul, E.; Janwantanakul, P.; Purepong, N.; Pensri, P.; Van Der Beek, A.J. The association between physical activity and neck and low back pain: A systematic review. Eur. Spine J. 2010, 20, 677–689. [Google Scholar] [CrossRef] [Green Version]
- Tan, V.P.S.; Macdonald, H.; Kim, S.; Nettlefold, L.; Gabel, L.; Ashe, M.C.; A McKay, H. Influence of Physical Activity on Bone Strength in Children and Adolescents: A Systematic Review and Narrative Synthesis. J. Bone Miner. Res. 2014, 29, 2161–2181. [Google Scholar] [CrossRef]
- Wilks, D.C.; Besson, H.; Lindroos, A.K.; Ekelund, U. Objectively measured physical activity and obesity prevention in children, adolescents and adults: A systematic review of prospective studies. Obes. Rev. 2010, 12, e119–e129. [Google Scholar] [CrossRef]
- Yang, X.; Zhai, Y.; Zhang, J.; Chen, J.-Y.; Liu, D.; Zhao, W.-H. Combined effects of physical activity and calcium on bone health in children and adolescents: A systematic review of randomized controlled trials. World J. Pediatr. 2020, 16, 356–365. [Google Scholar] [CrossRef]
- Zulfarina, M.S.; Sharkawi, A.M.; Aqilah-S.N., Z.-S.; Mokhtar, S.-A.; Nazrun, S.A.; Naina-Mohamed, I. Influence of Adolescents’ Physical Activity on Bone Mineral Acquisition: A Systematic Review Article. Iran. J. Public Health 2016, 45, 1545–1557. [Google Scholar] [PubMed]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Saunders, T.J.; Katzmarzyk, P.; Okely, A.; Gorber, S.C.; et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef] [PubMed]
- Chinapaw, M.J.M.; Proper, K.I.; Brug, J.; Van Mechelen, W.; Singh, A.S. Relationship between young peoples’ sedentary behaviour and biomedical health indicators: A systematic review of prospective studies. Obes. Rev. 2011, 12, e621–e632. [Google Scholar] [CrossRef]
- Cliff, D.; Hesketh, K.D.; Vella, S.A.; Hinkley, T.; Tsiros, M.; Ridgers, N.; Carver, A.; Veitch, J.; Parrish, A.; Hardy, L.; et al. Objectively measured sedentary behaviour and health and development in children and adolescents: Systematic review and meta-analysis. Obes. Rev. 2016, 17, 330–344. [Google Scholar] [CrossRef] [Green Version]
- Fröberg, A.; Raustorp, A. Objectively measured sedentary behaviour and cardio-metabolic risk in youth: A review of evidence. Eur. J. Nucl. Med. Mol. Imaging 2014, 173, 845–860. [Google Scholar] [CrossRef]
- Koedijk, J.B.; Van Rijswijk, J.; Oranje, W.A.; Bergh, J.P.V.D.; Bours, S.P.; Savelberg, H.H.; Schaper, N.C. Sedentary behaviour and bone health in children, adolescents and young adults: A systematic review. Osteoporos. Int. 2017, 28, 2507–2519. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Wong, F.K.Y. The Association Between Time Spent in Sedentary Behaviors and Blood Pressure: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 867–880. [Google Scholar] [CrossRef]
- Rey-López, J.P.; Vicente-Rodríguez, G.; Biosca, M.; Moreno, L.A. Sedentary behaviour and obesity development in children and adolescents. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 242–251. [Google Scholar] [CrossRef]
- Canabrava, K.L.R.; Amorim, P.R.D.S.; Miranda, V.P.N.; Priore, S.E.; Franceschini, S.D.C.C. Sedentary behavior and cardiovascular risk in children: A systematic review. Rev. Bras. Med. Esporte 2019, 25, 433–441. [Google Scholar] [CrossRef]
- Tanaka, C.; Reilly, J.J.; Huang, W. Longitudinal changes in objectively measured sedentary behaviour and their relationship with adiposity in children and adolescents: Systematic review and evidence appraisal. Obes. Rev. 2014, 15, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; LeBlanc, A.G.; Kho, M.E.; Saunders, T.J.; Larouche, R.; Colley, R.C.; Goldfield, G.; Gorber, S.C. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Ekris, E.; Altenburg, T.; Singh, A.S.; Proper, K.I.; Heymans, M.; Chinapaw, M. An evidence-update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 833–849. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, R.G.; Guedes, D.P. Physical Activity, Sedentary Behavior, Cardiorespiratory Fitness and Metabolic Syndrome in Adolescents: Systematic Review and Meta-Analysis of Observational Evidence. PLoS ONE 2016, 11, e0168503. [Google Scholar] [CrossRef] [PubMed]
- Prentice-Dunn, H.; Prentice-Dunn, S. Physical activity, sedentary behavior, and childhood obesity: A review of cross-sectional studies. Psychol. Health Med. 2012, 17, 255–273. [Google Scholar] [CrossRef] [PubMed]
- Skrede, T.; Steene-Johannessen, J.; Anderssen, S.A.; Resaland, G.K.; Ekelund, U. The prospective association between objectively measured sedentary time, moderate-to-vigorous physical activity and cardiometabolic risk factors in youth: A systematic review and meta-analysis. Obes. Rev. 2018, 20, 55–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verswijveren, S.J.J.M.; Lamb, K.; Bell, L.A.; Timperio, A.; Salmon, J.; Ridgers, N.D. Associations between activity patterns and cardio-metabolic risk factors in children and adolescents: A systematic review. PLoS ONE 2018, 13, e0201947. [Google Scholar] [CrossRef] [Green Version]
- Rothman, K.J. BMI-related errors in the measurement of obesity. Int. J. Obes. 2008, 32, S56–S59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reilly, J.J. Diagnostic accuracy of the BMI for age in paediatrics. Int. J. Obes. 2006, 30, 595–597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Javed, A.; Jumean, M.; Murad, M.H.; Okorodudu, D.; Kumar, S.; Somers, V.K.; Sochor, O.; Lopez-Jimenez, F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: A systematic review and meta-analysis. Pediatr. Obes. 2015, 10, 234–244. [Google Scholar] [CrossRef]
- Ellis, K.J. Selected Body Composition Methods Can Be Used in Field Studies. J. Nutr. 2001, 131, 1589S–1595S. [Google Scholar] [CrossRef]
- Slaughter, M.H.; Lohman, T.G.; Boileau, R.A.; Horswill, C.A.; Stillman, R.J.; van Loan, M.D.; Bemben, D.A. Skinfold Equations for Estimation of Body Fatness in Children and Youth. Hum. Biol. 1988, 60, 709–723. [Google Scholar]
- Freedman, D.S.; Horlick, M.; Berenson, G.S. A comparison of the Slaughter skinfold-thickness equations and BMI in predicting body fatness and cardiovascular disease risk factor levels in children. Am. J. Clin. Nutr. 2013, 98, 1417–1424. [Google Scholar] [CrossRef]
- Kriemler, S.; Puder, J.; Zahner, L.; Roth, R.; Meyer, U.; Bedogni, G. Estimation of percentage body fat in 6-to 13-year-old children by skinfold thickness, body mass index and waist circumference. Br. J. Nutr. 2010, 104, 1565–1572. [Google Scholar] [CrossRef] [Green Version]
- Ulijaszek, S.J.; Kerr, D.A. Anthropometric measurement error and the assessment of nutritional status. Br. J. Nutr. 1999, 82, 165–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stergiou, G.S.; Boubouchairopoulou, N.; Kollias, A. Accuracy of Automated Blood Pressure Measurement in Children: Evidence, Issues, and Perspectives. Hypertension 2017, 69, 1000–1006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopes, L.; Santos, R.; Coelho-E-Silva, M.; Draper, C.; Mota, J.; Jidovtseff, B.; Clark, C.; Schmidt, M.; Morgan, P.; Duncan, M.; et al. A Narrative Review of Motor Competence in Children and Adolescents: What We Know and What We Need to Find Out. Int. J. Environ. Res. Public Health 2020, 18, 18. [Google Scholar] [CrossRef] [PubMed]
- Blair, S.N.; Cheng, Y.; Holder, J.S. Is physical activity or physical fitness more important in defining health benefits? Med. Sci. Sports Exerc. 2001, 33, S379–S399. [Google Scholar] [CrossRef]
- Ekelund, U.; Luan, J.; Sherar, L.B.; Esliger, D.W.; Griew, P.; Cooper, A. Moderate to Vigorous Physical Activity and Sedentary Time and Cardiometabolic Risk Factors in Children and Adolescents. JAMA 2012, 307, 704–712. [Google Scholar] [CrossRef] [Green Version]
| Reference | # Studies | Exposure | Outcome |
|---|---|---|---|
| Gao et al., 2015, [17] | 35 | Active video games | Health outcomes |
| Gomez-Bruton et al., 2013, [18] | 23 | Swimming | Bone tissue |
| Gomez–Bruton et al., 2016, [19] | 14 | Swimming | Bone mineral density |
| Guinhouya et al., 2011, [20] | 37 | PA | Metabolic syndrome, insulin resistance |
| Henriques-Neto et al., 2020, [21] | 11 | Active commuting | Physical fitness |
| Krahnebühl et al., 2018, [22] | 21 | PA | Bone geometry |
| Lubans et al., 2011, [23] | 27 | Active travel | Health-related fitness |
| Miguel-Berges et al., 2017, [24] | 36 | PA | Adiposity |
| Poitras et al., 2016, [3] | 162 | PA | Health indicators |
| Ramires et al., 2015, [25] | 18 | PA, inactivity | Body fat, obesity |
| Rauner et al., 2013, [26] | 14 | PA, PF | Overweight |
| Saunders et al., 2013, [27] | 8 | Active travel | Health benefits |
| Sitthipornvorakul et al., 2010, [28] | 13 | PA | Neck pain, low back pain |
| Tan et al., 2014, [29] | 37 | PA | Bone strength |
| Wilks et al., 2011, [30] | 14 | PA | Obesity |
| Yang et al., 2020, [31] | 9 | PA, calcium | Bone health |
| Zulfarina et al., 2016, [32] | 9 | PA | Bone mineral acquisition |
| Reference | # Studies | Exposure | Outcome |
|---|---|---|---|
| Carson et al., 2016, [33] | 235 | SED | Health indicators |
| Chinapaw et al., 2011, [34] | 31 | SED | Biomedical health indicators |
| Cliff et al., 2016, [35] | 88 | SED | Health and development |
| Fröberg and Raustorp, 2014, [36] | 45 | SED | Cardio-metabolic risk |
| Koedijk et al., 2014, [37] | 17 | SED | Bone health |
| Lee and Wong, 2015, [38] | 24 | SED | Blood pressure |
| Rey-Lopez et al., 2008, [39] | 71 | SED | Obesity |
| Ribeiro Canabrava et al., 2019, [40] | 50 | SED | Cardiovascular risk |
| Tanaka et al., 2014, [41] | 13 | SED | Adiposity |
| Tremblay et al., 2011, [42] | 232 | SED | Health indicators |
| Van Ekris et al., 2016, [43] | 109 | SED | Biomedical health indicators |
| Reference | # Studies | Exposure | Outcome |
|---|---|---|---|
| Oliveira and Guedes, 2016, [44] | 18 | PA, SED | CRF, Metabolic Syndrome |
| Prentice-Dunn et al., 2012, [45] | 17 | PA, SED | Childhood obesity |
| Skrede et al., 2018, [46] | 30 | SED, MVPA | Cardio–metabolic risk factors |
| Verswijveren et al., 2018, [47] | 29 | Activity patterns | Cardio–metabolic risk factors |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolb, S.; Burchartz, A.; Oriwol, D.; Schmidt, S.C.E.; Woll, A.; Niessner, C. Indicators to Assess Physical Health of Children and Adolescents in Activity Research—A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 10711. https://doi.org/10.3390/ijerph182010711
Kolb S, Burchartz A, Oriwol D, Schmidt SCE, Woll A, Niessner C. Indicators to Assess Physical Health of Children and Adolescents in Activity Research—A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(20):10711. https://doi.org/10.3390/ijerph182010711
Chicago/Turabian StyleKolb, Simon, Alexander Burchartz, Doris Oriwol, Steffen C. E. Schmidt, Alexander Woll, and Claudia Niessner. 2021. "Indicators to Assess Physical Health of Children and Adolescents in Activity Research—A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 20: 10711. https://doi.org/10.3390/ijerph182010711
APA StyleKolb, S., Burchartz, A., Oriwol, D., Schmidt, S. C. E., Woll, A., & Niessner, C. (2021). Indicators to Assess Physical Health of Children and Adolescents in Activity Research—A Scoping Review. International Journal of Environmental Research and Public Health, 18(20), 10711. https://doi.org/10.3390/ijerph182010711






