Perceived Social Support Attenuates the Association between Stress and Health-Related Quality of Life among Adults Experiencing Homelessness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measures
2.3.1. Participant Characteristics
2.3.2. Social Support
2.3.3. Perceived Stress
2.3.4. Health-Related Quality of Life
2.4. Data Analysis
3. Results
3.1. Sample Descriptives
3.2. Moderation Analyses
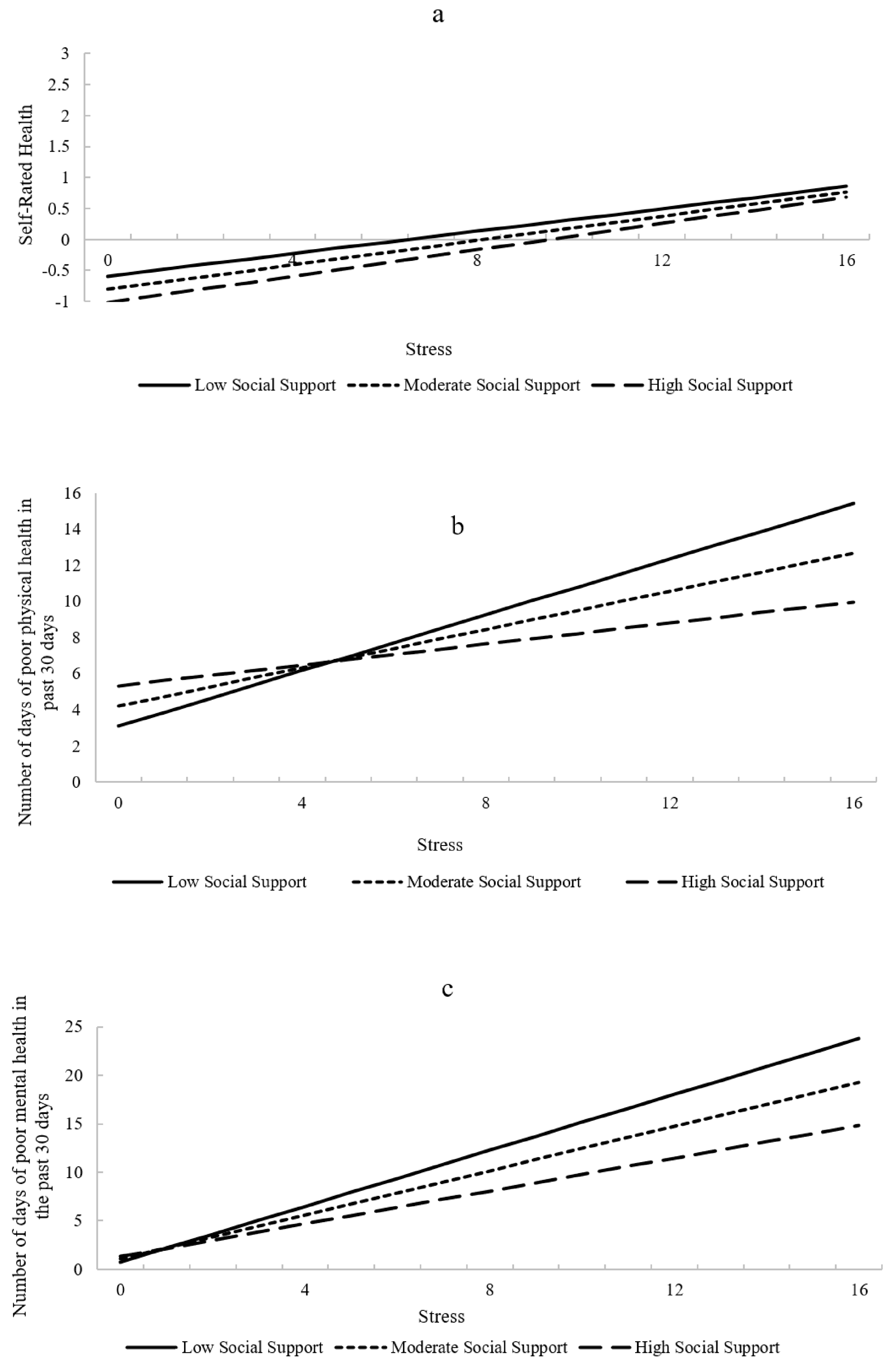
3.2.1. Self-Rated Health
3.2.2. Poor Physical Health Days
3.2.3. Poor Mental Health Days
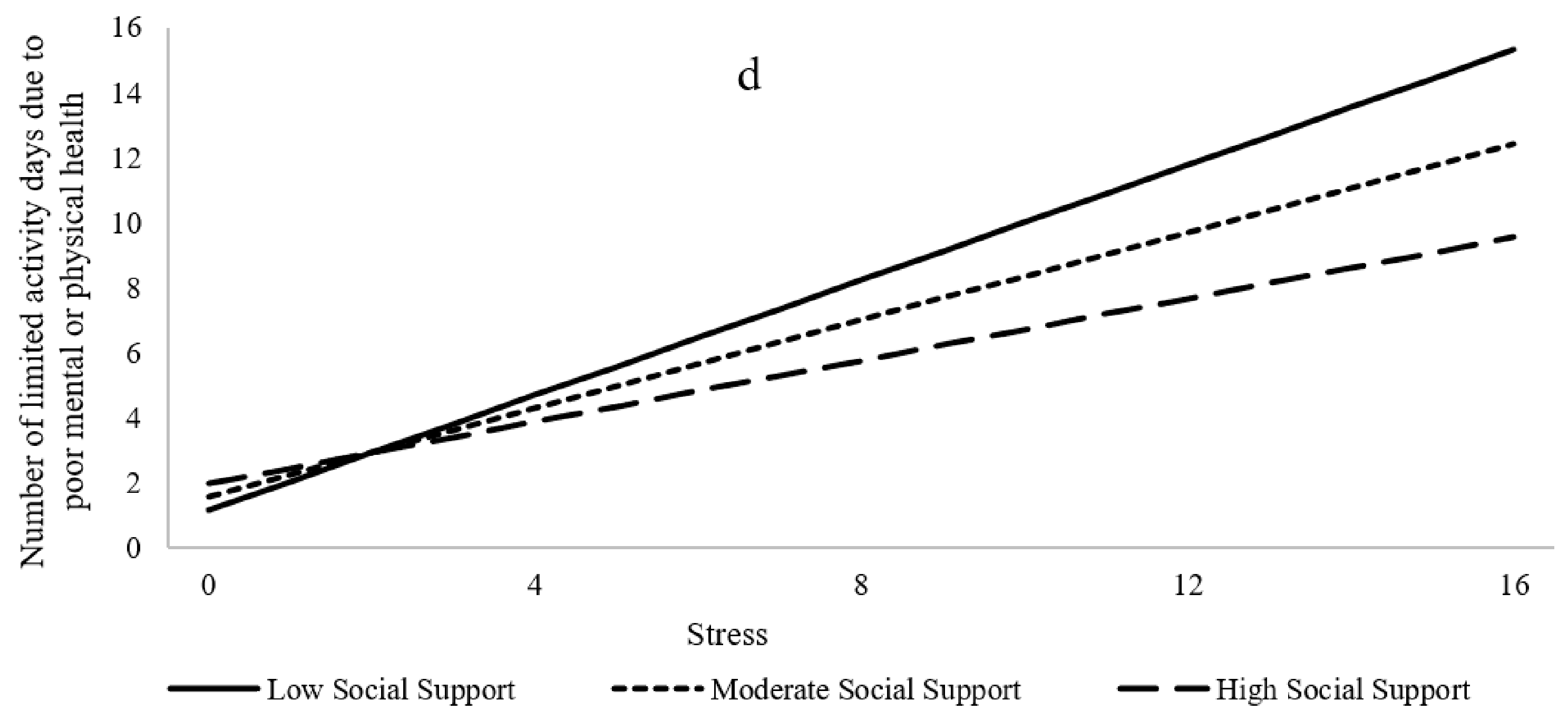
3.2.4. Activity-Limited Days Due to Poor Physical or Mental Health
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The, U.S. Department of Housing and Urban Development, Office of Community Planning and Development. The 2020 Annual Homeless Assessment Report (AHAR) to Congress; The U.S. Department of Housing and Urban Development, Office of Community Planning and Development: Washington, DC, USA, 2020.
- Baggett, T.P.; O’Connell, J.J.; Singer, D.E.; Rigotti, N.A. The unmet health care needs of homeless adults: A national study. Am. J. Public Health 2010, 100, 1326–1333. Available online: https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2009.180109 (accessed on 21 August 2021). [CrossRef] [PubMed]
- Hwang, S.W. Homelessness and health. CMAJ Can. Med. Assoc. J. 2001, 164, 229–233. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC80688/ (accessed on 31 July 2021).
- Childress, S.; Reitzel, L.R.; Maria, D.S.; Kendzor, D.E.; Moisiuc, A.; Businelle, M.S. Mental illness and substance use problems in relation to homelessness onset. Am. J. Health Behav. 2015, 39, 549–555. [Google Scholar] [CrossRef]
- Maness, S.B.; Reitzel, L.R.; Hernandez, D.C.; Santa Maria, D.M.; Batson, M.A.; Zingg, T.; Kendzor, D.E.; Businelle, M.S. Modifiable health risk factors and readiness to change among homeless adults. Am. J. Health Behav. 2019, 43, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Reitzel, L.R.; Chinamuthevi, S.; Daundasekara, S.S.; Hernandez, D.C.; Chen, T.-A.; Harkara, Y.; Obasi, E.M.; Kendzor, D.E.; Businelle, M.S. Association of problematic alcohol use and food insecurity among homeless men and women. Int. J. Environ. Res. Public Health 2020, 17, 3631. [Google Scholar] [CrossRef] [PubMed]
- Neisler, J.; Shree, S.; Reitzel, L.R.; Chen, T.A.; Kendzor, D.E.; Obasi, E.M.; Wrighting, Q.; Businelle, M.S. Characterizing alcohol use behaviors among homeless men and women. Am. J. Health Behav. 2019, 43, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Baggett, T.P.; Hwang, S.W.; O’Connell, J.J.; Porneala, P.C.; Stringfellow, E.J.; Orav, E.J.; Singer, D.E.; Rigotti, N.A. Mortality Among Homeless Adults in Boston—Shift in Cases of Death Over 15 Year Period. JAMA Intern. Med. 2013, 173, 189–195. Available online: https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/1556797 (accessed on 21 August 2021). [CrossRef]
- Taylor, E.M.; Kendzor, D.E.; Reitzel, L.R.; Businelle, M.S. Health risk factors and desire to change among homeless adults. Am. J. Health Behav. 2016, 40, 455–460. [Google Scholar] [CrossRef]
- Agrawal, P.; Neisler, J.; Businelle, M.S.; Kendzor, D.E.; Hernandez, D.C.; Odoh, C.; Reitzel, L.R. Exposure to Violence and Sleep Inadequacies among Men and Women Living in a Shelter Setting. Health Behav. Res. 2019, 2, 19. [Google Scholar] [CrossRef] [Green Version]
- Hernandez, D.C.; Daundasekara, S.S.; Arlinghaus, K.R.; Tobar, N.; Reitzel, L.R.; Kendzor, D.E.; Businelle, M.S. Cumulative risk factors associated with food insecurity among adults who experience homelessness. Health Behav. Res. 2019, 2, 7. [Google Scholar] [CrossRef] [Green Version]
- Odoh, C.; Businelle, M.S.; Chen, T.-A.; Kendzor, D.E.; Obasi, E.M.; Reitzel, L.R. Association of fear and mistrust with stress among sheltered homeless adults, and the moderating effects of race and sex. J. Racial Ethnic Health Disp. 2020, 7, 458–467. [Google Scholar] [CrossRef]
- Iwundu, C.N.; Agrawal, P.; Businelle, M.S.; Kendzor, D.E.; Reitzel, L.R. Predictors of Overnight and Emergency Treatment among Homeless Adults. Int. J. Environ. Res. Public Health 2020, 17, 4271. [Google Scholar] [CrossRef]
- Gonzalez, J.R.; Jetelina, K.K.; Roberts, M.; Reitzel, L.R.; Kendzor, D.E.; Walters, S.; Businelle, M.S. Criminal justice system involvement among homeless adults. Am. J. Crim. Justice 2018, 43, 158–166. [Google Scholar] [CrossRef]
- Chang, H.-L.; Fisher, F.D.; Reitzel, L.R.; Kendzor, D.E.; Nguyen, M.A.H.; Businelle, M.S. Subjective sleep inadequacy and self-rated health among homeless adults. Am. J. Health Behav. 2015, 39, 14–21. [Google Scholar] [CrossRef]
- Reitzel, L.R.; Short, N.A.; Schmidt, N.B.; Garey, L.; Zvolensky, M.J.; Moisiuc, A.; Reddick, C.; Kendzor, D.E.; Businelle, M.S. Distress tolerance links sleep problems with stress & health in homeless. Am. J. Health Behav. 2017, 41, 760–774. [Google Scholar] [CrossRef]
- Wrighting, Q.; Reitzel, L.R.; Chen, T.-A.; Kendzor, D.E.; Hernandez, D.C.; Obasi, E.M.; Shree, S.; Businelle, M.S. Characterizing discrimination experiences by race among homeless adults. Am. J. Health Behav. 2019, 43, 531–542. [Google Scholar] [CrossRef]
- Kendzor, D.E.; Reitzel, L.R.; Businelle, M.S. Characterizing Stressors and Modifiable Health Risk Factors Among Homeless Smokers: An Exploratory Pilot Study. Health Edu. Behav. Off. Pub. Soc. Public Health Edu. 2015, 42, 642–647. [Google Scholar] [CrossRef]
- National Alliance to End Homelessness. Exploring the State of Homelessness: 2020 Edition. 2020. Available online: https://endhomelessness.org/exploring-the-state-of-homelessness-in-2020/ (accessed on 20 August 2021).
- Currie, L.B.; Patterson, M.L.; Moniruzzaman, A.; McCandless, L.C.; Somers, J.M. Examining the relationship between health-related need and the receipt of care by participants experiencing homelessness and mental illness. BMC Health Serv. Res. 2014, 14, 404. [Google Scholar] [CrossRef] [Green Version]
- Sun, S.; Irestig, R.; Burström, B.; Beijer, U.; Burström, K. Health-related quality of life (EQ-5D) among homeless persons compared to a general population sample in Stockholm County, 2006. Scand. J. Public Health 2012, 40, 115–125. [Google Scholar] [CrossRef]
- Lewer, D.; Aldridge, R.W.; Menezes, D.; Sawyer, C.; Zaninotto, P.; Dedicoat, M.; Ahmed, I.; Luchenski, S.; Hayward, A.; Story, A. Health-related quality of life and prevalence of six chronic diseases in homeless and housed people: A cross-sectional study in London and Birmingham, England. BMJ Open 2019, 9, e025192. [Google Scholar] [CrossRef] [Green Version]
- Odafe, M.O.; Salami, T.K.; Walker, R.L. Race-related stress and hopelessness in community-based African American adults: Moderating role of social support. Cult. Divers. Ethn. Minority Psych. 2017, 23, 561–569. [Google Scholar] [CrossRef]
- Neisler, J.; Reitzel, L.R.; Garey, L.; Kenzdor, D.E.; Hébert, E.T.; Vijayaraghavan, M.; Businelle, M.S. Concurrent nicotine and tobacco product use among homeless smokers and associations with cigarette dependence and other factors related to quitting. Drug Alcohol Depend. 2018, 185, 133–140. [Google Scholar] [CrossRef] [Green Version]
- Matsumura, K.; Morozumi, R.; Hamazaki, K.; Tsuchida, A.; Inadera, H.; Japan Environment and Children’s Study (JECS) Group. Effect estimate of time-varying social support and trust on the physical and mental health of mothers at 2.5 years postpartum: The Japan Environment and Children’s Study (JECS). J. Epidemiol 2021. advance online publication. [Google Scholar] [CrossRef]
- Durbin, A.; Nisenbaun, R.; Kopp, B.; O’Campo, P.; Hwang, S.W.; Stergiopoulos, V. Are resilience and perceived stress related to social support and housing stability among homeless adults with mental illness? Health Soc. Care Community 2019, 27, 1053–1062. [Google Scholar] [CrossRef]
- Zugazaga, C.B. Pathways to homelessness and social support among homeless single men, single women, and women with children. Proquest Disser. Pub. 2002. Available online: http://search.proquest.com.ezproxy.lib.uh.edu/dissertations-theses/pathways-homelessness-social-support-among/docview/305438941/se-2?accountid=7107 (accessed on 31 July 2021).
- Fargo, J.D.; Munley, E.A.; Byrne, T.H.; Montgomery, A.E.; Culhane, D.P. Community-Level Characteristics Associated with Variation in Rates of Homelessness Among Families and Single Adults. Am. J. Public Health 2013, 103, S340–S347. Available online: https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2013.301619 (accessed on 31 July 2021). [CrossRef]
- Garey, L.; Reitzel, L.R.; Neisler, J.; Kendzor, D.E.; Zvolensky, M.J.; Neighbors, C.; Hernandez, D.C.; Businelle, M.S. Health-Related Quality of Life Among Homeless Smokers: Risk and Protective Factors of Latent Class Membership. Behav. Med. 2019, 45, 40–51. [Google Scholar] [CrossRef]
- Cohen, L.H.; Burt, C.E.; Bjorck, J.P. Life stress and adjustment: Effects of life events experienced by young adolescents and their parents. Dev. Psych. 1987, 23, 583–592. [Google Scholar] [CrossRef]
- Unger, J.B.; Kipke, M.D.; Thomas, S.R.; Johnson, C.J.; Montgomery, S.B.; Iverson, E. Stress, Coping, and Social Support among Homeless Youth. J. Adolesc. Youth 1998, 85, 343–374. [Google Scholar] [CrossRef]
- Waring, J.; Hébert, E.T.; Alexander, A.C.; Kendzor, D.E.; Businelle, M.S. Evaluating the influences of social support and smoking cues on daily smoking abstinence among socioeconomically disadvantaged adults. Addict. Behav. 2020, 100, 106107. Available online: https://doi-org.ezproxy.lib.uh.edu/10.1016/j.addbeh.2019.106107 (accessed on 31 July 2021). [CrossRef]
- Letiecq, B.L.; Anderson, E.A.; Koblinsky, S.A. Social Support of Homeless and Housed Mothers: A Comparison of Temporary and Permanent Housing Arrangements. Fam. Relat. 1998, 47, 415–421. [Google Scholar] [CrossRef]
- Arozullah, A.M.; Yarnold, P.R.; Bennett, C.L.; Soltysik, R.C.; Wolf, M.S.; Ferreira, R.M.; Lee, S.-Y.D.; Costello, S.; Shakir, A.; Denwood, C.; et al. Development and Validation of a Short-Form, Rapid Estimate of Adult Literacy in Medicine. Med. Care 2007, 45, 1026–1033. Available online: http://www.jstor.org/stable/40221577 (accessed on 31 July 2021). [CrossRef]
- Cohen, S.; Hoberman, H. Positive Events and Social Supports as Buffers of Life Change Stress. J. Appl. Perceived Soc. Psychol. 1983, 13, 99–125. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control. Behavioral Risk Factor Surveillance System 2009 Survey Data and Documentation; CDC: Atlanta, GA, USA, 2019. Available online: https://www.cdc.gov/brfss/annual_data/annual_2009.htm (accessed on 7 August 2021).
- Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public’s Health in the 21st Century; Nat. Press (US), The Healthcare Delivery System: Washington, DC, USA, 2002. Available online: https://www.ncbi.nlm.nih.gov/books/NBK221227/ (accessed on 31 July 2021).
- Center for Disease Control and Prevention. Measuring Healthy Days; CDC: Atlanta, GA, USA, 2000. Available online: https://stacks.cdc.gov/view/cdc/6406 (accessed on 8 August 2021).
- Idler, E.L.; Benyamini, Y. Self-rated health and mortality: A review of twenty-seven community studies. J. Health Soc. Behav. 1997, 38, 21–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, P.O.; Neyman, J. Tests of certain linear hypotheses and their application to some educational problems. Stat. Res. Mem. 1936, 1, 57–93. Available online: https://psycnet.apa.org/record/1936-05538-001 (accessed on 20 August 2021).
- Leung, D.Y.P.; Chan, H.Y.L.; Chiu, P.K.C.; Lo, R.S.K.; Lee, L.L.Y. Source of Social Support and Caregiving Self-Efficacy on Caregiver Burden and Patient’s Quality of Life: A Path Analysis on Patients with Palliative Care Needs and Their Caregivers. Int. J. Environ. Res. Public Health 2020, 17, 5457. [Google Scholar] [CrossRef]
- Watson, J.; Crawley, J.; Kane, D. Social exclusion, health and hidden homelessness. Public Health 2016, 139, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Anderson, M.-C.; Hazel, A.; Perkins, J.M.; Almquist, Z.W. The Ecology of Unsheltered Homelessness: Environmental and Social-Network Predictors of Well-Being among an Unsheltered Homeless Population. Int. J. Environ. Res. Public Health 2021, 18, 7328. [Google Scholar] [CrossRef]
- Businelle, M.S.; Cuate, E.L.; Kesh, A.; Poonawalla, I.B.; Kendzor, D.E. Comparing homeless smokers to economically disadvantaged domiciled smokers. Am. J. Public Health 2013, 103, S218–S220. Available online: http://dx.doi.org.ezproxy.lib.uh.edu/10.2105/AJPH.2013.301336 (accessed on 7 August 2021). [CrossRef]
- Van Everdingen, C.; Bob Peerenboom, P.; Van Der Velden, K.; Delespaul, P.A.E.G. A Comprehensive Assessment to Enable Recovery of the Homeless: The HOP-TR Study. Front. Public Health 2021, 9, 661517. [Google Scholar] [CrossRef]
- Barker, S.L.; Maguire, N. Experts by Experience: Peer Support and its Use with the Homeless. Community Ment. Health J. 2017, 53, 598–612. Available online: https://link.springer.com/article/10.1007/s10597-017-0102-2 (accessed on 7 August 2021). [CrossRef] [Green Version]
- Addo, R.; Yuma, P.; Barrera, I.; Layton, D. Social networks and subjective wellbeing of adults in a Housing First program. J. Community Psychol. 2021, 24, 1–12. [Google Scholar] [CrossRef]
- Golembiewski, E.; Watson, D.P.; Robison, L.; Coberg, J.W., II. Social Network Decay as Potential Recovery from Homelessness: A Mixed Methods Study in Housing First Programming. Soc. Sci. 2017, 6, 96. [Google Scholar] [CrossRef] [Green Version]
- Meadows, O.M. Social Support Among Homeless and Housed Mothers: An Integrative Review. J. Psychol. Nurs. Ment. Health Serv. 2005, 43, 40–47. [Google Scholar] [CrossRef]
- Rhoades, H.; Hsu, H.; Rice, E.; Harris, T.; Motte-Kerr, W.L.; Winetrobe, H.; Henwood, B.; Wenzel, S. Social network change after moving into permanent supportive housing: Who stays and who goes? Net. Sci. 2021, 9, 18–34. [Google Scholar] [CrossRef]
- Mercado, M.; Marroquín, J.M.; Ferguson, K.M.; Bender, K.; Shelton, J.; Prock, K.A.; Maria, D.S.; Hsu, H.-T.; Narendorf, S.C.; Petering, R.; et al. The intersection of housing and mental well-being: Examining the needs of formerly homeless young adults transitioning to stable housing. SSM–Pop. Health 2021, 14, 100775. [Google Scholar] [CrossRef]
- Cantwell, J.; Muldoon, O.T.; Gallagher, S. Social support and mastery influence the association between stress and poor physical health in parents caring for children with developmental disabilities. Res. Dev. Disabil. 2014, 35, 2215–2223. [Google Scholar] [CrossRef] [Green Version]
- Toro, P.A.; Oko-Riebau, M. Social Support and Stress Among Homeless Adults in Southern Poland. J. Community Psychol. 2015, 43, 430–446. [Google Scholar] [CrossRef]
- Chemaitelly, H.; Kanaan, C.; Beydoun, H.; Chaaya, M.; Kanaan, M.; Sibai, A.M. The role of gender in the association of social capital, social support, and economic security with self-rated health among older adults in deprived communities in Beirut. Qual. Life Res. 2013, 22, 1371–1379. [Google Scholar] [CrossRef]
- Oklahoma City Planning Department-Housing & Community Development Division. 2016 Point-In-Time a Snapshot of Homelessness in Oklahoma City; Oklahoma City Planning Department: Oklahoma City, OK, USA, 2016. Available online: https://www.okc.gov/home/showpublisheddocument/5680/636104892047270000 (accessed on 20 August 2021).
- Solarz, A.; Bogat, G.A. When social support fails: The homeless. J. Community Psychol. 1990, 18, 79–96. Available online: https://doi.org/10.1002/1520-6629(199001)18:1<79::AID-JCOP2290180112>3.0.CO;2-B (accessed on 20 August 2021). [CrossRef]
| Characteristics | n (SD)/% [n] |
|---|---|
| Sex | |
| Female | 36.32 [211] |
| Age | 43.64 (12.16) |
| Race | |
| White | 53.65 [309] |
| Black or African American | 19.62 [113] |
| Asian | 0.35 [2] |
| Native American/Alaska Native | 12.33 [71] |
| Multi-racial/Other | 14.06 [81] |
| Years of Education | 11.94 (2.04) |
| Insurance Status | |
| Insured | 30 [174] |
| Serious Mental Illness | |
| Yes | 65.69 [381] |
| Data Collection Site | |
| Site 1 | 41.31 [240] |
| Site 2 | 8.61 [50] |
| Site 3 | 30.29 [176] |
| Site 4 | 10.15 [59] |
| Site 5 | 7.23 [42] |
| Site 6 | 2.41 [14] |
| Lifetime Homeless (in months) | 42.36 (51.25) |
| Social Support | 32.91 (8.72) |
| Perceived Stress | 7.67 (3.58) |
| Self-rated Health (Continuous) | 3.04 (1.12) |
| Self-rated Health (Binary) | |
| Fair or Poor | 36.38 [211] |
| Excellent, Very Good, or Good | 63.62 [369] |
| Poor Physical Health Days (past 30 days) | 7.95 (10.69) |
| Poor Physical Health Days (past 30 days) | |
| 0 | 37.54 [217] |
| 1–13 | 38.75 [224] |
| ≥14 | 23.7 [137] |
| Poor Mental Health Days (past 30 days) | 10.78 (11.80) |
| Poor Mental Health Days (past 30 days) | |
| 0 | 32.18 [186] |
| 1–13 | 31.66 [183] |
| ≥14 | 36.16 [209] |
| Limited Activity Days (past 30 days) | 6.36 (9.59) |
| Limited Activity Days (past 30 days) | |
| 0 | 48.62 [281] |
| 1–13 | 31.49 [182] |
| ≥14 | 19.90 [115] |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex (ref: Male) | 1 | ||||||||||
| 2. Age | −0.107 * | 1 | |||||||||
| 3. Years of Education | 0.041 | 0.084 * | 1 | ||||||||
| 4. Any Insurance (Ref: No) | 0.188 *** | 0.040 | 0.039 | 1 | |||||||
| 5. Serious Mental Illness (Ref: No) | 0.159 *** | 0.075 | 0.024 | 0.101 * | 1 | ||||||
| 6. Lifetime Homeless (in months) | −0.116 ** | 0.246 *** | −0.039 | 0.026 | −0.004 | 1 | |||||
| 7. Social Support | 0.069 | −0.093 * | 0.069 | −0.066 | −0.118 ** | −0.085 * | 1 | ||||
| 8. Perceived Stress | 0.089 * | −0.035 | −0.042 | −0.054 | 0.200 *** | −0.047 | −0.432 *** | 1 | |||
| 9. Poor Self-rated Health | 0.113 ** | 0.208 *** | −0.002 | 0.012 | 0.166 *** | 0.039 | −0.290 *** | 0.382 *** | 1 | ||
| 10. Poor Physical Health Days (past 30 days) | 0.009 | 0.237 *** | 0.055 | −0.005 | 0.227 *** | 0.093 * | −0.189 *** | 0.229 *** | 0.447 *** | 1 | |
| 11. Poor Mental Health Days (past 30 days) | 0.125 ** | 0.055 | 0.024 | −0.029 | 0.345 *** | −0.001 | −0.345 *** | 0.479 *** | 0.358 *** | 0.538 *** | 1 |
| 12. Limited Activity Days (past 30 days) | 0.022 | 0.185 *** | 0.0269 | 0.060 | 0.224 *** | 0.060 | −0.282 *** | 0.330 *** | 0.345 *** | 0.563 *** | 0.597 *** |
| Outcomes of Interest | Key Variables for Interaction | Estimate | SE | p-Value |
|---|---|---|---|---|
| Self-rated Health | Social Support | −0.017 | 0.005 | 0.001 |
| Perceived Stress | 0.099 | 0.014 | <0.0001 | |
| Social Support*Perceived Stress | 0.001 | 0.001 | 0.466 | |
| Poor Physical Health Days | Social Support | −0.083 | 0.055 | 0.131 |
| Perceived Stress | 0.529 | 0.137 | <0.0001 | |
| Social Support*Perceived Stress | −0.028 | 0.013 | 0.030 | |
| Poor Mental Health Days | Social Support | −0.228 | 0.054 | <0.0001 |
| Perceived Stress | 1.140 | 0.135 | <0.0001 | |
| Social Support*Perceived Stress | −0.034 | 0.012 | 0.007 | |
| Activity-Limited Days Due to Poor Physical or Mental Health | Social Support | −0.134 | 0.048 | 0.006 |
| Perceived Stress | 0.679 | 0.120 | <0.0001 | |
| Social Support*Perceived Stress | −0.024 | 0.011 | 0.033 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jafry, M.Z.; Martinez, J.; Chen, T.A.; Businelle, M.S.; Kendzor, D.E.; Reitzel, L.R. Perceived Social Support Attenuates the Association between Stress and Health-Related Quality of Life among Adults Experiencing Homelessness. Int. J. Environ. Res. Public Health 2021, 18, 10713. https://doi.org/10.3390/ijerph182010713
Jafry MZ, Martinez J, Chen TA, Businelle MS, Kendzor DE, Reitzel LR. Perceived Social Support Attenuates the Association between Stress and Health-Related Quality of Life among Adults Experiencing Homelessness. International Journal of Environmental Research and Public Health. 2021; 18(20):10713. https://doi.org/10.3390/ijerph182010713
Chicago/Turabian StyleJafry, Midhat Z., Jayda Martinez, Tzuan A. Chen, Michael S. Businelle, Darla E. Kendzor, and Lorraine R. Reitzel. 2021. "Perceived Social Support Attenuates the Association between Stress and Health-Related Quality of Life among Adults Experiencing Homelessness" International Journal of Environmental Research and Public Health 18, no. 20: 10713. https://doi.org/10.3390/ijerph182010713
APA StyleJafry, M. Z., Martinez, J., Chen, T. A., Businelle, M. S., Kendzor, D. E., & Reitzel, L. R. (2021). Perceived Social Support Attenuates the Association between Stress and Health-Related Quality of Life among Adults Experiencing Homelessness. International Journal of Environmental Research and Public Health, 18(20), 10713. https://doi.org/10.3390/ijerph182010713








