The Appointment System Influences Uptake of Cataract Surgical Services in Rwanda
Abstract
1. Introduction
2. Materials and Methods
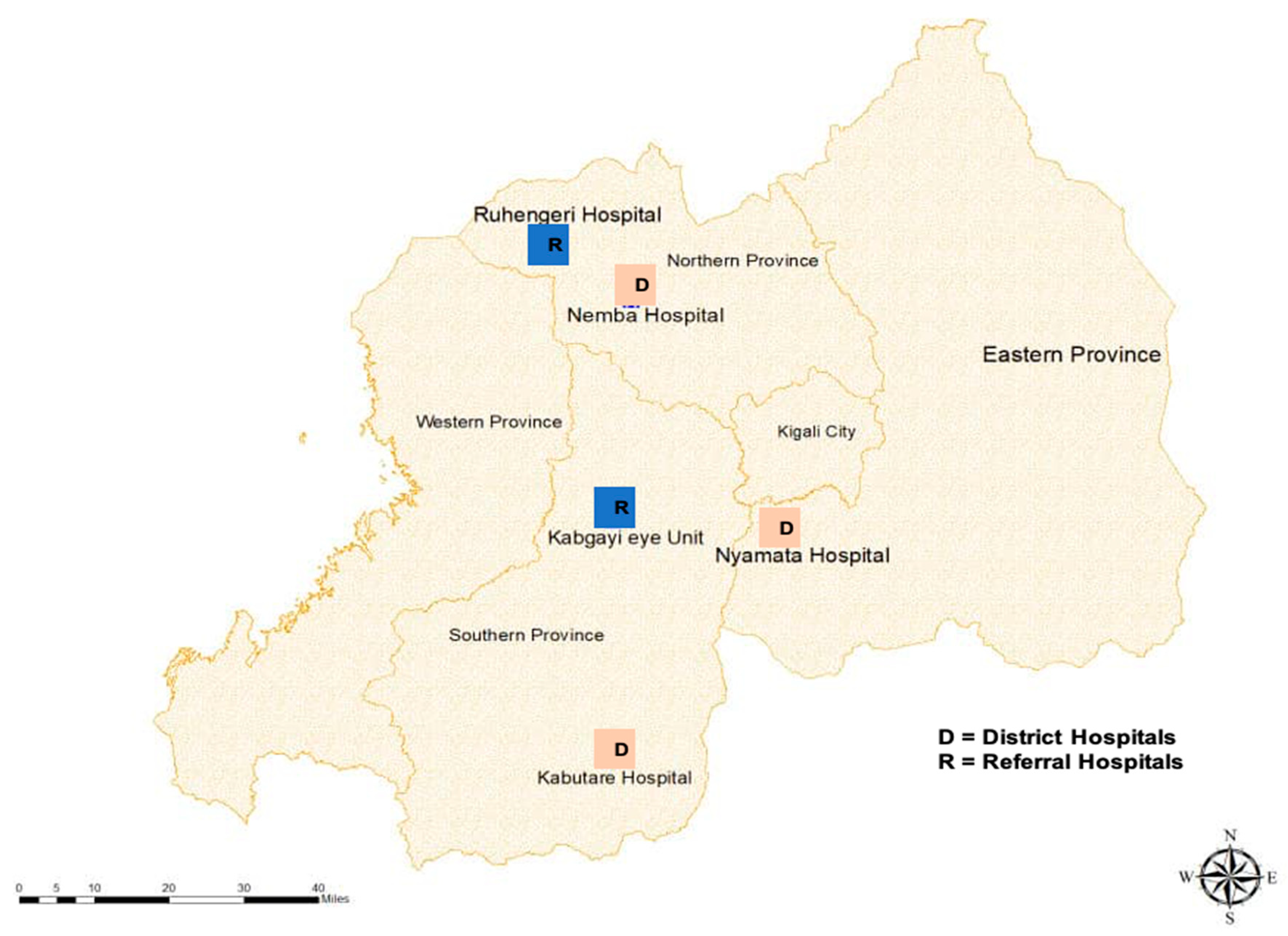
2.1. Sample Selection
2.2. Ethics
2.3. Data Collection
- Sociodemographic characteristics: Literacy status (literate vs. illiterate), socioeconomic status (Ubudehe Level 1 (poorest) to 4 (wealthiest)), family support status (number of children, escorted to appointment, decision-making), travel time to the eye clinic (hours), cost of transport (US$);
- Whether counselling about surgery was delivered by the ophthalmic clinic officer (counselling received vs. not received);
- Appointment-related factors such as ownership of a mobile telephone in the family, whether a specific date was provided for the surgical appointment, method of receiving appointment information, whether a reminder was provided, the number of days between the diagnosis and surgical appointment;
- General health status (e.g., diabetes, hypertension, HIV and AIDS, rheumatoid arthritis, chronic heart problems);
- Self-reported disability using the Washington group short set of questions on disability [11].
2.4. Analysis
3. Results
3.1. Uptake of Appointment
3.2. Factors Associated with Uptake of Appointments
3.3. Barriers to Uptake of Appointment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ackland, P.; Resnikoff, S.; Bourne, R. World blindness and visual impairment: Despite many successes, the problem is growing. Community Eye Health J. 2018, 30, 71–73. [Google Scholar]
- International Agency for the Prevention of Blindness. Vision Atlas [Internet]; IAPB: London, UK, 2018. [Google Scholar]
- Riaz, Y.; de Silva, S.R.; Evans, J.R. Manual Small Incision Cataract Surgery (MSICS) with Posterior Chamber Intraocular Lens Versus Phacoemulsification with Posterior Chamber Intraocular Lens for Age-Related Cataract; Cochrane Database of Systematic Reviews; John Wiley and Sons Ltd.: Hoboken, NJ, USA, 2013; Volume 2013. [Google Scholar]
- National Institute of Statistics of Rwanda. Population and Housing Surveys; National Institute of Statistics of Rwanda: Kigali, Rwanda, 2012.
- Nkurikiye, J.; Mathenge, W. Rapid Assessment of Avoidable Blindness in Rwanda [Internet]; Ministry of Health Rwanda: Kigali, Rwanda, 2015.
- Mathenge, W.; Nkurikiye, J.; Limburg, H.; Kuper, H. Rapid assessment of avoidable blindness in western Rwanda: Blindness in a postconflict setting. PLoS Med. 2007, 4, 1187–1194. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Rwanda. Republic of Rwanda National Eye Health Strategic Plan; Ministry of Health: Kigali, Rwanda, 2018.
- Rwanda Ministry of Health Fourth Health Sector Strategic Plan; Ministry of Health: Kigali, Rwanda, 2018; pp. 1–104.
- Nyandekwe, M.; Nzayirambaho, M.; Kakoma, J.B. Universal health coverage in Rwanda: Dream or reality. Pan Afr. Med. J. 2014, 17, 232. [Google Scholar] [CrossRef] [PubMed]
- Rwanda Social Security Board. Community Based Health Insurance; Rwanda Social Security Board: Kigali, Rwanda, 2016.
- Washington Group. Washington Group Short Set of Disability Questions; US National Center for Health Statistics: Hyattsville, MD, USA.
- Aboobaker, S.; Courtright, P. Barriers to cataract surgery in Africa: A systematic review. Middle East Afr. J. Ophthalmol. 2016, 23, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Syed, A.; Polack, S.; Eusebio, C.; Mathenge, W.; Wadud, Z.; Mamunur, A.K.; Foster, A.; Kuper, H. Predictors of attendance and barriers to cataract surgery in Kenya, Bangladesh and the Philippines. Disabil. Rehabil. 2013, 35, 1660–1667. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Statistics of Rwanda. The Fifth Integrated Household Living Conditions Survey; EICV5 2016/17: Rwanda Poverty Profile Report; National Institute of Statistics of Rwanda: Kigali, Rwanda, 2018; p. 82.
- Lin, H.; Lin, D.; Long, E.; Jiang, H.; Qu, B.; Tang, J.; Lin, Y.; Chen, J.; Wu, X.; Lin, Z.; et al. Patient participation in free cataract surgery: A cross-sectional study of the low-income elderly in urban China. BMJ Open 2016, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Rono, H.K.; Bastawrous, A.; Macleod, D.; Wanjala, E.; DiTanna, G.L.; Weiss, H.A.; Burton, M.J. Smartphone-based screening for visual impairment in Kenyan school children: A cluster randomised controlled trial. Lancet Glob. Health 2018, 6, e924–e932. [Google Scholar] [CrossRef]
- Karra, M.; Canning, D.; Foster, S.; Shah, I.H.; Senanayake, H.; Ratnasiri, U.D.P.; Pathiraja, R.P. Location and content of counselling and acceptance of postpartum IUD in Sri Lanka. Reprod Health 2017, 14, 42. [Google Scholar] [CrossRef] [PubMed]
- Kaakinen, P.; Ervasti, H.; Kääriäinen, M. Quality of counselling for knee and shoulder arthroscopy patients during day surgery. Int. J. Orthop. Trauma Nurs. 2017, 24, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Finger, R.P.; Kupitz, D.G.; Holz, F.G.; Chandrasekhar, S.; Balasubramaniam, B.; Ramani, R.V.; Gilbert, C.E. Regular provision of outreach increases acceptance of cataract surgery in South India. Trop. Med. Int. Health 2011, 16, 1268–1275. [Google Scholar] [CrossRef] [PubMed]
- Bright, T.; Kuper, H. A systematic review of access to general healthcare services for people with disabilities in low and middle income countries. Int. J. Environ. Res. Public Health 2018, 15, 1879. [Google Scholar] [CrossRef] [PubMed]
- NHS. Plan, Do, Study, Act (PDSA) Cycles and the Model for Improvement; NHS: London, UK, 2019.
- Gilbert, C.; Shukla, R.; Murthy, G.V.S.; Santosha, B.V.M.; Gudlavalleti, A.G.; Mukpalkar, S.; Yamarthi, P.; Pendyala, S.; Pendyala, S.; Edla, S.; et al. Retinopathy of prematurity: Overview and highlights of an initiative to integrate prevention, screening, and management into the public health system in India. Indian J. Ophthalmol. 2019, 68, S103–S107. [Google Scholar] [CrossRef] [PubMed]
| Sample Frame n = 297 | Participants n = 221 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Facility | Attended Surgical Appointment | Did not Attend Surgical Appointment | Attended Surgical Appointment | Did not Attend Surgical Appointment | ||||||||
| M | F | T | M | F | T | M | F | T | M | F | T | |
| Referral Hospital | ||||||||||||
| Kabgayi | 19 | 31 | 50 (66.6) | 10 | 15 | 25 (33.3) | 12 | 16 | 28 (57.1) | 8 | 13 | 21 (42.9) |
| Ruhengeri | 7 | 14 | 21 (60.0) | 5 | 9 | 14 (40.0) | 5 | 11 | 16 (72.7) | 2 | 4 | 6 (27.3) |
| District Hospital | ||||||||||||
| Nemba | 13 | 27 | 40 (42.1) | 19 | 36 | 55 (57.9) | 13 | 27 | 40 (50.6) | 13 | 26 | 39 (49.3) |
| Nyamata | 6 | 11 | 16 (55.2) | 5 | 8 | 13 (44.8) | 6 | 11 | 17 (68.0) | 3 | 5 | 8 (32.0) |
| Kabutare | 15 | 17 | 32 (51.6) | 11 | 19 | 30 (48.4) | 12 | 13 | 25 (54.3) | 8 | 13 | 21 (45.6) |
| Total | 60 | 100 | 160 (53.9) | 50 | 87 | 137 (46.1) | 48 | 78 | 126 (57.0) | 34 | 61 | 95 (43.0) |
| Total | Attended | OR (95%CI) | p-Value * | |||
|---|---|---|---|---|---|---|
| n | % | |||||
| Literate | No | 157 | 80 | (51.0) | Ref | |
| Yes, with difficulty | 24 | 17 | (70.8) | 2.3 (0.9–5.9) | 0.07 | |
| Yes, easily | 40 | 29 | (72.5) | 2.5 (1.2–5.4) | 0.02 | |
| Number of children | 8+ | 63 | 24 | (38.1) | Ref | |
| 4 to 7 | 123 | 79 | (64.2) | 2.3 (1.2–4.3) | 0.008 | |
| <4 | 35 | 24 | (68.6) | 3.1 (1.3–7.4) | 0.01 | |
| Vision impairment (VI) | Not VI | 38 | 25 | (65.8) | Ref | |
| Mild | 41 | 22 | (58.5) | 0.7 (0.1–2.0) | 0.5 | |
| Moderate | 82 | 28 | (34.2) | 0.3 (0.1–0.6) | 0.002 | |
| Severe | 29 | 23 | (79.3) | 2.0 (0.6–6.1) | 0.2 | |
| Blind | 31 | 26 | (84.0) | 2.7 (1.1–10.0) | 0.03 | |
| Mobile telephone in the family | No | 120 | 45 | (37.5) | Ref | |
| Yes | 101 | 66 | (65.4) | 3.6 (2.0–6.3) | <0.0001 | |
| Counselling received | Yes | 187 | 100 | (54.3) | Ref | |
| No | 37 | 26 | (70.3) | 0.5 (0.2–1.1) | 0.08 | |
| Specific appointment date provided | No | 74 | 26 | (31.4) | Ref | |
| Yes | 133 | 100 | (75.2) | 2.3 (1.3–5.2) | 0.004 | |
| Appointment reminder provided | No | 105 | 54 | (51.5) | Ref | |
| Yes | 26 | 23 | (88.5) | 6.4 (1.8–22.9) | 0.004 | |
| Number of days between diagnosis and surgical appointment | 30+ | 39 | 22 | (56.4) | Ref | |
| 10 to 29 | 38 | 22 | (57.9) | 1.4 (0.8–4.1) | 0.1 | |
| <10 | 66 | 44 | (66.6) | 1.6 (1.1–4.3) | 0.05 | |
| Walking difficulties | None | 161 | 99 | (61.5) | Ref | |
| Some/a lot | 60 | 27 | (45.0) | 0.5 (0.3–0.9) | 0.03 | |
| Barriers | Referral Hospital—Permanent Services (n = 27) | District Hospital—Outreach Services (n = 68) | ||||
|---|---|---|---|---|---|---|
| Male | Female | Total (n, %) | Male | Female | Total (n, %) | |
| Cost | 6 | 12 | 18 (66.6) | 7 | 22 | 29 (42.6) |
| Insufficient/unclear information | 2 | 2 | 4 (14.8) | 13 | 27 | 40 (58.8) |
| Lack of escort | 2 | 4 | 6 (22.2) | 0 | 7 | 7 (10.3) |
| Sickness/other disability | 1 | 2 | 3 (11.1) | 6 | 4 | 10 (14.7) |
| Fear of surgery | 2 | 2 | 4 (14.8) | 1 | 3 | 4 (5.9) |
| Lack of transport | 0 | 0 | 0 (0.0) | 4 | 5 | 9 (13.2) |
| Other | 1 | 0 | 1 (3.7) | 6 | 7 | 13 (19.1) |
| Enablers | Referral Hospital—Permanent Services (n = 20) | District Hospital—Outreach Services (n = 14) | ||||
|---|---|---|---|---|---|---|
| Male | Female | Total (n, %) | Male | Female | Total (n, %) | |
| Received information | 4 | 10 | 14 (70.0) | 5 | 2 | 7 (50.0) |
| Family support | 2 | 9 | 11 (55.0) | 4 | 4 | 8 (57.1) |
| Transport provided | 3 | 1 | 4 (20.0) | 2 | 2 | 4 (28.6) |
| Severity of vision loss | 1 | 4 | 5 (25.0) | 0 | 2 | 2 (14.3) |
| Other | 0 | 0 | 0 (0.0) | 2 | 3 | 5 (35.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kitema, G.F.; Morjaria, P.; Mathenge, W.; Ramke, J. The Appointment System Influences Uptake of Cataract Surgical Services in Rwanda. Int. J. Environ. Res. Public Health 2021, 18, 743. https://doi.org/10.3390/ijerph18020743
Kitema GF, Morjaria P, Mathenge W, Ramke J. The Appointment System Influences Uptake of Cataract Surgical Services in Rwanda. International Journal of Environmental Research and Public Health. 2021; 18(2):743. https://doi.org/10.3390/ijerph18020743
Chicago/Turabian StyleKitema, Gatera Fiston, Priya Morjaria, Wanjiku Mathenge, and Jacqueline Ramke. 2021. "The Appointment System Influences Uptake of Cataract Surgical Services in Rwanda" International Journal of Environmental Research and Public Health 18, no. 2: 743. https://doi.org/10.3390/ijerph18020743
APA StyleKitema, G. F., Morjaria, P., Mathenge, W., & Ramke, J. (2021). The Appointment System Influences Uptake of Cataract Surgical Services in Rwanda. International Journal of Environmental Research and Public Health, 18(2), 743. https://doi.org/10.3390/ijerph18020743






