Psychological Impact on the Nursing Professionals of the Rioja Health Service (Spain) Due to the SARS-CoV-2 Virus
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population and Scope of the Study
2.3. Study Variables
2.4. Data Collection Instrument and Procedure
2.5. Statistical Procedures and Analysis
2.6. Ethical Considerations
3. Results
3.1. Descriptive Results
3.2. Descriptive Data
3.3. Comparative Analysis of the Variables
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_ (accessed on 14 November 2020).
- Moreira, W.C.; de Sousa, A.R.; de Sousa Nóbrega, M.D.P.S. Mental illness in the general population and health professionals during COVID-19: A scoping review. Texto Contexto Enferm. 2020, 29, 1–17. [Google Scholar] [CrossRef]
- Instituto de Salud Carlos III. Situación de COVID-19 en España n° 54. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/Informe%20COVID-19.%20N%C2%BA%2054_25%20de%20noviembre%20de%202020.pdf (accessed on 28 November 2020).
- Huarcaya-Victoria, J. Consideraciones sobre la salud mental en la pandemia de COVID-19. Rev. Peru. Med. Exp. Salud Pública 2020, 37, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Ortiz, J.; Castro-Quintero, D.; Lerma-Córdoba, C.; Yela-Ceballos, F.; Escobar-Córdoba, F. Consequences of the COVID-19 pandemic in mental health associated with social isolation. SciELO Prepr. 2020, 4, 1–21. [Google Scholar] [CrossRef]
- Paiano, M.; Jaques, A.E.; Nacamura, P.A.B.; Salci, M.A.; Radovanovic, C.A.T.; Carreira, L. Mental health of healthcare professionals in China during the new coronavirus pandemic: An integrative review. Rev. Bras. Enferm. 2020, 73, 1–8. [Google Scholar] [CrossRef]
- Alvarez, A.K.G.; Almaguer, A.Y.C.; Santos, E.D.Z. Management of health personnel’ psychological safety, in emergency situations by COVID-19 in the hospitable or isolation context. Rev. Cuba Enferm. 2020, 36, 1–19. [Google Scholar]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, 1–12. [Google Scholar] [CrossRef]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.J.H.; Yeo, L.L.L.; Ahmad, A.; Khan, F.A.; Shanmugan, G.N.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef]
- Reger, M.A.; Piccirillo, M.L.; Buchman-Schmitt, J.M. COVID-19, Mental Health, and Suicide Risk Among Health Care Workers: Looking Beyond the Crisis. J. Clin. Psychiatry 2020, 81, 5. [Google Scholar] [CrossRef]
- Torales, J.; Higgins, M.O.; Rios-gonzález, C.M.; Barrios, I.; Higgins, M.O.; Rios-gonzález, C.M. Considerations on the mental health impact of the novel coronavirus outbreak (COVID-19). SciELO 2020, 1–6, in press. [Google Scholar]
- Ornell, F.; Halpern, S.C.; Paim Kessler, F.H.; de Magalhães Narvaez, J.C. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. Cad. Saúde Pública 2020, 36, 4. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psyquiatr. 2020, 52, 1–5. [Google Scholar] [CrossRef]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Chan, G.; Xu, X.; Wang, L.; et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain. Behav. Immun. 2020, 88, 916–919. [Google Scholar] [CrossRef]
- Vieta, E.; Pérez, V.; Arango, C. Psychiatry in the aftermath of COVID-19. Rev. Psiquiatr. Salud. Ment. 2020, 13, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Wand, A.P.F.; Zhong, B.L.; Chiu, H.F.K.; Draper, B.; De Leo, D. COVID-19: The implications for suicide in older adults. Int. Psychogeriatr. 2020, 32, 1225–1230. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. J. Psychiatr. Res. 2020, 288, 1–6. [Google Scholar] [CrossRef]
- Shultz, J.M.; Cooper, J.L.; Baingana, F.; Oquendo, M.A.; Espinel, Z.; Althouse, B.M.; Marcelin, L.H.; Towers, S.; Espinola, M.; McCoy, C.B.; et al. The Role of Fear-Related Behaviors in the 2013–2016 West Africa Ebola Virus Disease Outbreak. Curr. Psychiatry Rep. 2016, 18, 104. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.Y.; Yang, Y.Z.; Zhang, X.M.; Xu, X.; Dou, Q.L.; Zhang, W.W.; Cheng, A.S.K. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Centro de Investigación Biomédica de La Rioja. Comité de Ética de la Investigación con Medicamentos de La Rioja (CEImLAR). Available online: https://www.cibir.es/es/plataformas-tecnologicas-y-servicios/ceimlar (accessed on 14 April 2020).
- Alexandre, N.M.C.; Gallasch, C.H.; Lima, M.H.M.; Rodrigues, R.C.M. Reliability in the development and evaluation of measurement instruments in the health field. Rev. Eletr. Enferm. 2013, 15, 802–809. [Google Scholar]
- Coluci, M.Z.O.; Alexandre, N.M.C.; Milani, D. Construção de instrumentos de medida na área da saúde. Ciênc. Saúde. Colet. 2015, 20, 925–936. [Google Scholar] [CrossRef]
- Cunha, C.M.; de Almeida Neto, O.P.; Stackfleth, R. Main psychometric evaluation methods of measuring instruments reliability. Rev. Aten. Saúde 2016, 14, 98–103. [Google Scholar]
- Chen, Q.; Liang, M.; Li, Y.; Guo, J.; Fei, D.; Wang, L.; He, L.; Sheng, C.; Cai, Y.; Li, X.; et al. Mental healthcare for medical staff in china during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, 15–16. [Google Scholar] [CrossRef]
- Huang, J.Z.; Han, M.F.; Luo, T.D.; Ren, A.K.; Zhou, X.P. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2020, 38, 192–195. [Google Scholar] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.; Ho, R. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Santamaría, M.D.; Etxebarria, N.O.; Rodríguez, I.R.; Alboniga-Mayor, J.J.; Gorrotxategi, M.P. Impacto psicológico de la COVID-19 en una muestra de profesionales sanitarios españoles. Rev. Psiquiatr. Salud Ment. 2020, 2. in press. [Google Scholar]
- Wong, T.W.; Yau, J.K.; Chan, C.L.; Kwong, R.S.; Ho, S.M.; Lau, C.C.; Lau, F.L.; Lit, C.H. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005, 12, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Styra, R.; Hawryluck, L.; Robinson, S.; Kasapinovic, S.; Fones, C.; Gold, W.L. Impact on healthcare workers employed in high-risk areas during the Toronto SARS outbreak. J. Psychosom Res. 2008, 64, 177–183. [Google Scholar] [CrossRef]
- Lee, S.M.; Kang, W.S.; Cho, A.; Kim, T.; Park, J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry 2018, 87, 123–127. [Google Scholar] [CrossRef]

| Characteristics | |
|---|---|
| Age | n (%) |
| <25 years old | 38 (6.28) |
| 26–35 years old | 102 (16.86) |
| 36–45 years old | 159 (26.28) |
| 46–55 years old | 183 (30.25) |
| >55 years old | 123 (20.33) |
| Sex | |
| Men | 49 (8.1) |
| Women | 556 (91.9) |
| Marital status | |
| Single | 179 (29.58) |
| Married | 340 (56.2) |
| Divorced | 59 (9.75) |
| Widower | 5 (0.83) |
| Other | 22 (3.64) |
| Children | |
| None | 220 (36.36) |
| One | 121 (20) |
| Two | 223 (36.86) |
| Three or more | 41 (6.78) |
| Dependents in my charge | |
| Yes | 113 (18.68) |
| No | 492 (81.32) |
| Category | |
| Registered Nurse | 386 (63.80) |
| Nurse Auxiliary | 219 (36.20) |
| Type of employment relationship | |
| Civil servant | 316 (52.23) |
| Not civil servant | 289 (47.77) |
| Laboral Experience | |
| <1 year | 33 (5.46) |
| 1–5 years | 82 (13.55) |
| 6–10 years | 61 (10.1) |
| 11–15 years | 67 (11.07) |
| >15 years | 362 (59.83) |
| Item | a. Never | b. Sometimes | c. Almost Always | d. Always |
|---|---|---|---|---|
| Dimension 1. Stressors (N = 605 Cronbach’s alpha = 0.8828) | ||||
| 14. I felt that I had material in the unit that guaranteed my safety in the care of patients infected or possibly infected by COVID-19. | 10 | 212 | 264 | 119 |
| 15. Did I feel a lack or shortage of knowledge related to COVID-19 infection when providing care to patients? | 38 | 368 | 153 | 46 |
| 16. I was afraid of making mistakes and failures in the care of patients infected with COVID-19. | 31 | 332 | 147 | 95 |
| 17. I felt helpless when I saw a COVID-19 patient who was not progressing satisfactorily. | 31 | 156 | 178 | 240 |
| 18. I felt that I did not pay attention to the psycho-emotional needs of COVID-19 infected patients. | 105 | 300 | 138 | 62 |
| 19. I thought that the care I was providing was not sufficiently humanized. | 116 | 281 | 141 | 67 |
| 20. I have had difficulty with a service with new techniques and procedures that I did not previously control and it affected my personal stability. Check only for people who have been relocated or hired because of the health crisis | 122 | 240 | 60 | 27 |
| 21. Coordination and teamwork were observed during the work shifts. | 13 | 191 | 284 | 117 |
| 22. There was enough staff in the unit where I worked during the pandemic. | 87 | 150 | 207 | 161 |
| 23. I felt that the rest time I had was sufficient during the work shift. | 105 | 266 | 134 | 100 |
| 24. I felt that I had an orderly rotation. | 73 | 122 | 138 | 272 |
| 25. I have thought about the possibility of getting infected by COVID-19 during my shift. | 11 | 233 | 159 | 202 |
| 26. I have thought about the possibility of being a probable asymptomatic carrier. | 25 | 288 | 126 | 166 |
| 27. I tested positive for COVID-19. | Yes: n = 95 | No: n = 510 | ||
| 28. What level of stress was generated by being positive in COVID-19. Answer only people who have been positive. Score 1 to 5 | 3.38 | |||
| 29. In what way has the disease passed? Answer only if you have been given positive in the test. | ||||
| a. Asymptomatic. | n = 34 | |||
| b. Mild symptoms without requiring hospital admission. | n = 58 | |||
| c. Serious symptoms that have required hospital admission | n = 3 | |||
| 30. I have been afraid of infecting the people I live with. Answer only if you live with more people. | 7 | 81 | 95 | 278 |
| 31. The situation I found myself in during the pandemic at work has affected my psychological state. | 38 | 319 | 124 | 124 |
| 32. At the end of the shift I felt physically exhausted | 5 | 154 | 232 | 214 |
| 33. At the end of the shift I felt emotionally overloaded. | 10 | 146 | 197 | 252 |
| 34. I managed to fall asleep easily and my rest was restorative. | 126 | 332 | 115 | 32 |
| Dimension 2. Perceived Emotions (N = 605 Cronbach’s alpha = 0.8379) | ||||
| 35. I often felt that I did not spend enough time on my feelings and emotions. Score 1 to 5 | 3.73 | |||
| 36. I have felt sad and have thought about things too much. Score 1 to 5 | 3.91 | |||
| 37. I did not feel able to think about the positive aspects of things. Score 1 to 5 | 3.35 | |||
| 38. I believe that this crisis has changed me and destabilized me on an emotional level. Score 1 to 5 | 3.22 | |||
| Dimension 3. Coping Strategies (N = 605 Cronbach’s alpha = 0.7917) | ||||
| 39. I have tried to avoid facing certain problems. | 189 | 327 | 69 | 20 |
| 40. I have avoided expressing my emotions with my co-workers. | 183 | 317 | 83 | 22 |
| 41. I have answered or spoken badly to my peers to release my pent-up emotions. | 332 | 254 | 15 | 4 |
| 42. I preferred not to analyze the situation when I was doing something wrong, without performing self-criticism and continuing with my tasks. | 365 | 212 | 25 | 3 |
| Varimax Rotation | Dimension 1 | Dimension 2 | Dimension 3 |
|---|---|---|---|
| p14 | 0.4962 | ||
| p15 | 0.5111 | ||
| p16 | 0.5338 | ||
| p17 | 0.3039 | ||
| p18 | 0.4732 | ||
| p19 | 0.4510 | ||
| p21 | 0.4412 | ||
| p22 | 0.6506 | ||
| p23 | 0.5520 | ||
| p24 | 0.4990 | ||
| p25 | 0.6030 | ||
| p26 | 0.6107 | ||
| p27 | 0.2418 | ||
| p31 | 0.2444 | ||
| p32 | 0.2434 | ||
| p33 | 0.2454 | ||
| p34 | 0.3034 | ||
| p35 | 0.6236 | ||
| p36 | 0.8015 | ||
| p37 | 0.7273 | ||
| p38 | 0.7342 | ||
| p39 | 0.4451 | ||
| p40 | 0.3147 | ||
| p41 | 0.3404 | ||
| p42 | 0.4451 | ||
| Kaiser-Meyer-Olkin Test (KMO) | |||
| Item | Value | ||
| p14 | 0.7715 | ||
| p15 | 0.8097 | ||
| p16 | 0.8829 | ||
| p17 | 0.9073 | ||
| p18 | 0.7837 | ||
| p19 | 0.8004 | ||
| p21 | 0.7471 | ||
| p22 | 0.8049 | ||
| p23 | 0.8221 | ||
| p24 | 0.8283 | ||
| p25 | 0.8403 | ||
| p26 | 0.7798 | ||
| p27 | 0.4910 | ||
| p31 | 0.9431 | ||
| p32 | 0.8555 | ||
| p33 | 0.8639 | ||
| p34 | 0.9423 | ||
| p35 | 0.9244 | ||
| p36 | 0.8950 | ||
| p37 | 0.9163 | ||
| p38 | 0.9220 | ||
| p39 | 0.8823 | ||
| p40 | 0.8640 | ||
| p41 | 0.8683 | ||
| p42 | 0.7160 | ||
| Analysis Value | ||
|---|---|---|
| RMSEA | Root Mean Squared Error of Approximation | 0.098 |
| AIC | Akaike’s Information Criterion | 40,223.5 |
| BIC | Bayesian Information Criterion | 40,611.2 |
| CFI | Comparative Fit Index | 0.969 |
| TLI | Tucker-Lewis Index | 0.935 |
| SRMR | Standardized Root Mean Squared Residual | 0.059 |
| CD | Coefficient of Determination | 0.994 |
| Variable | N | Mean | SD | Min. | Max. |
|---|---|---|---|---|---|
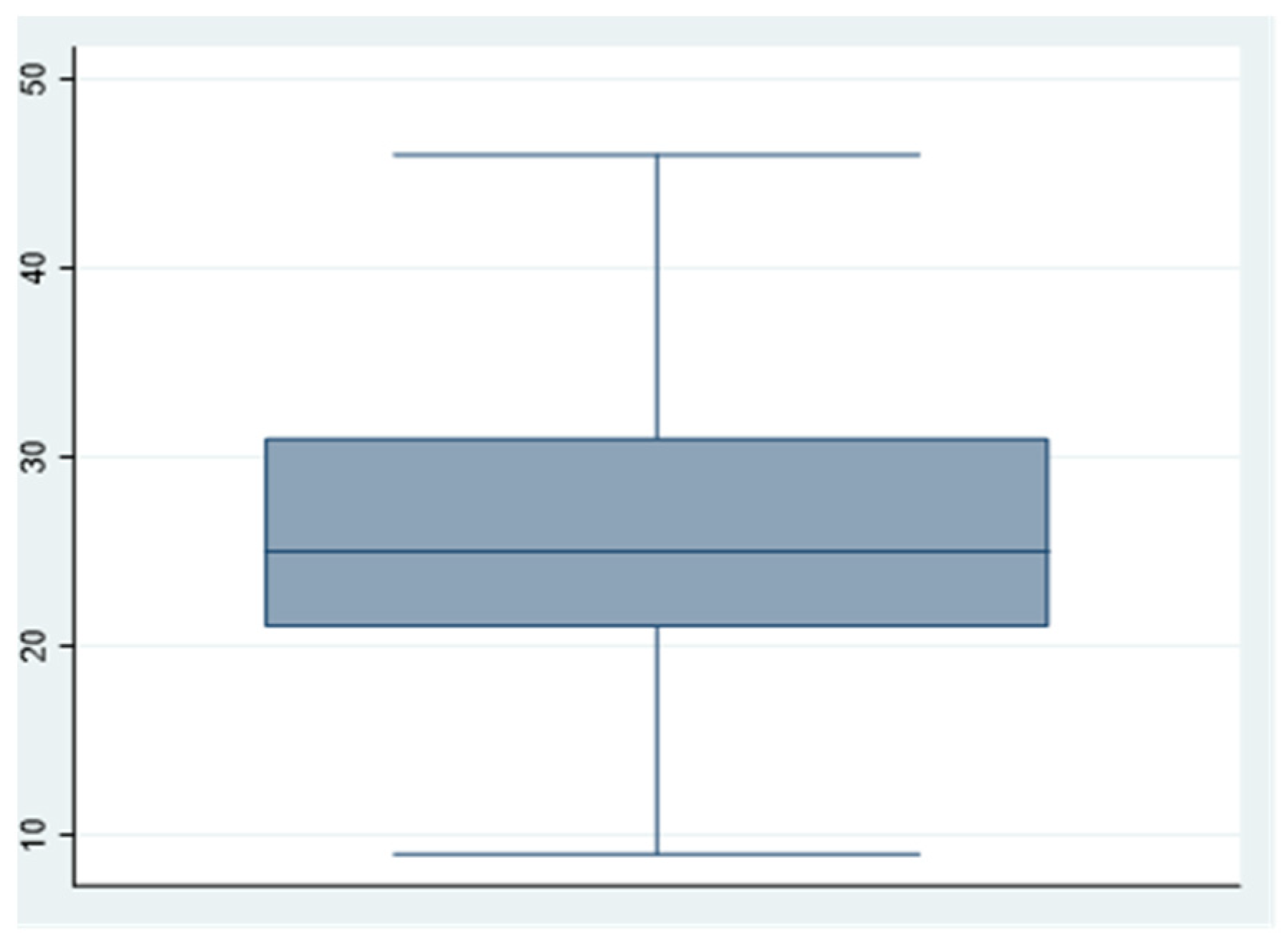
| Dimension 1: Stressors | 605 | 25.7438 | 6.8417 | 9 | 46 |
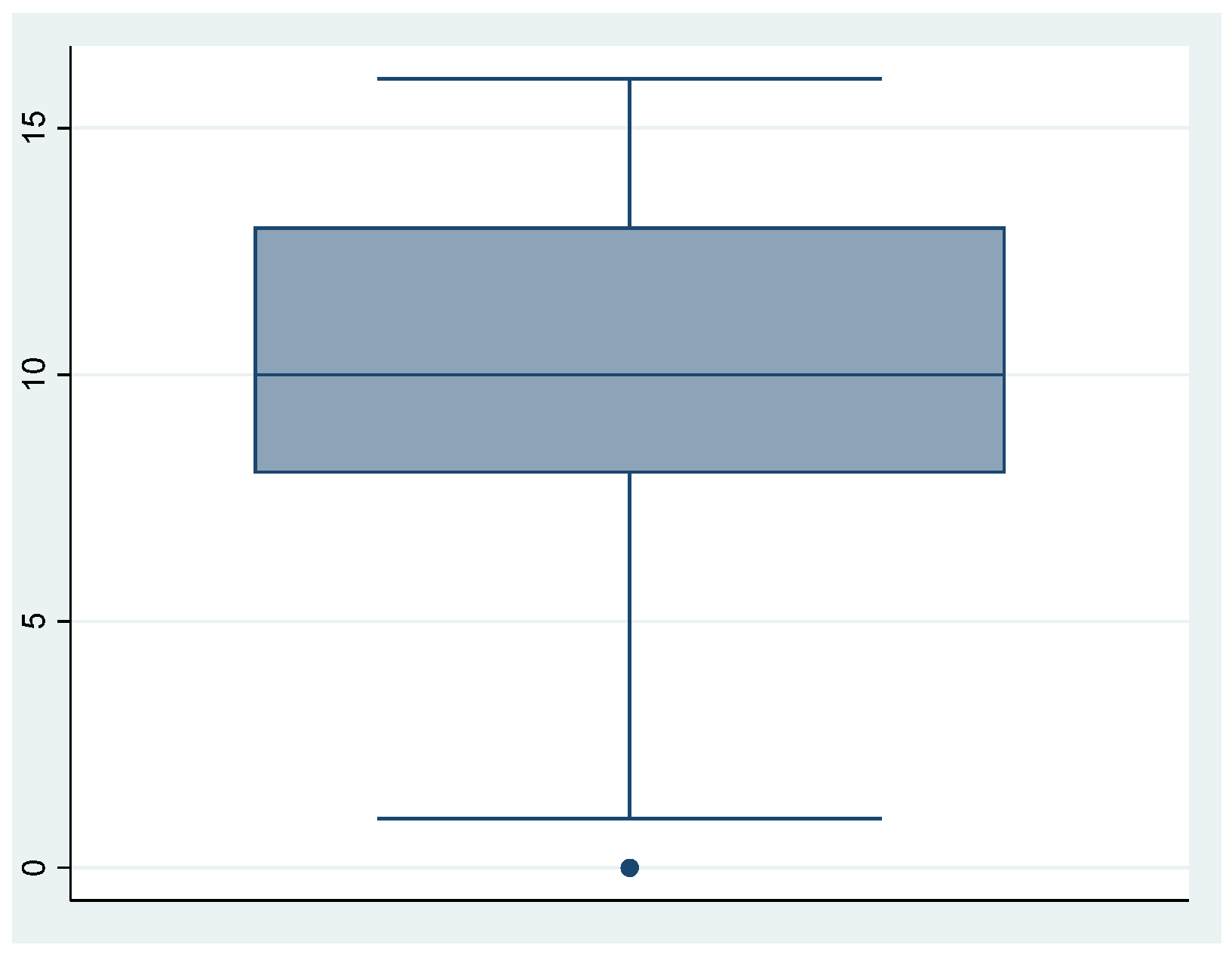
| Dimension 2: Perceived emotions | 605 | 10.20826 | 3.7340 | 0 | 16 |
| Dimension 3: Coping strategies | 605 | 2.712397 | 1.7717 | 0 | 12 |
| Stressors | Perceived Emotions | Coping Strategies. | |||||||
|---|---|---|---|---|---|---|---|---|---|
| C | 95% IC | p-Value | C | 95% IC | p-Value | C | 95%IC | p-Value | |
| Sex | |||||||||
| Woman | 3.02 | 1.08–4.96 | 0.002 | 1.57 | 0.49–2.65 | 0.004 | |||
| Men | |||||||||
| Dependents in my charge | |||||||||
| Not | |||||||||
| Yes | 1.19 | (−0.20)–2.59 | 0.094 | 0.94 | 0.17–1.72 | 0.017 | |||
| Type of employment relationship | |||||||||
| Civil servant | −2.09 | (−3.36)–(−0.81) | 0.001 | −0.45 | (−1.44)–0.54 | 0.374 | −0.18 | (−0.66)–0.29 | 0.455 |
| Not civil servant | 0.17 | (−1.83)–2.17 | 0.868 | 0.95 | 0.16–1.74 | 0.018 | 0.45 | (−0.03)–0.9 | 0.069 |
| Laboral experience | |||||||||
| <1 year | |||||||||
| 1–5 years | 5.79 | 3.13–8.46 | 0.000 | 2.19 | 0.71–3.68 | 0.004 | 0.26 | (−0.50)–1.02 | 0.506 |
| 6–10 years | 4.99 | 2.18–7.79 | 0.001 | 2.18 | 0.62–3.73 | 0.006 | 0.69 | 0.32–1.07 | 0.000 |
| 11–15 years | 4.78 | 1.90–7.66 | 0.001 | 1.60 | 0.06–3.15 | 0.042 | 0.17 | (−0.73)–1.06 | 0.716 |
| >15 years | 4.19 | 1.55–6.83 | 0.002 | 1.75 | 0.43–3.08 | 0.009 | 0.15 | (−0.70)–1.00 | 0.727 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Del Pozo-Herce, P.; Garrido-García, R.; Santolalla-Arnedo, I.; Gea-Caballero, V.; García-Molina, P.; Ruiz de Viñaspre-Hernández, R.; Rodríguez-Velasco, F.J.; Juárez-Vela, R. Psychological Impact on the Nursing Professionals of the Rioja Health Service (Spain) Due to the SARS-CoV-2 Virus. Int. J. Environ. Res. Public Health 2021, 18, 580. https://doi.org/10.3390/ijerph18020580
Del Pozo-Herce P, Garrido-García R, Santolalla-Arnedo I, Gea-Caballero V, García-Molina P, Ruiz de Viñaspre-Hernández R, Rodríguez-Velasco FJ, Juárez-Vela R. Psychological Impact on the Nursing Professionals of the Rioja Health Service (Spain) Due to the SARS-CoV-2 Virus. International Journal of Environmental Research and Public Health. 2021; 18(2):580. https://doi.org/10.3390/ijerph18020580
Chicago/Turabian StyleDel Pozo-Herce, Pablo, Rebeca Garrido-García, Iván Santolalla-Arnedo, Vicente Gea-Caballero, Pablo García-Molina, Regina Ruiz de Viñaspre-Hernández, Francisco José Rodríguez-Velasco, and Raúl Juárez-Vela. 2021. "Psychological Impact on the Nursing Professionals of the Rioja Health Service (Spain) Due to the SARS-CoV-2 Virus" International Journal of Environmental Research and Public Health 18, no. 2: 580. https://doi.org/10.3390/ijerph18020580
APA StyleDel Pozo-Herce, P., Garrido-García, R., Santolalla-Arnedo, I., Gea-Caballero, V., García-Molina, P., Ruiz de Viñaspre-Hernández, R., Rodríguez-Velasco, F. J., & Juárez-Vela, R. (2021). Psychological Impact on the Nursing Professionals of the Rioja Health Service (Spain) Due to the SARS-CoV-2 Virus. International Journal of Environmental Research and Public Health, 18(2), 580. https://doi.org/10.3390/ijerph18020580










