Psychological Distress and Work Environment Perception by Physical Therapists from Southern Italy during COVID-19 Pandemic: The C.A.L.A.B.R.I.A Study
Abstract
:1. Introduction
2. Materials and Methods
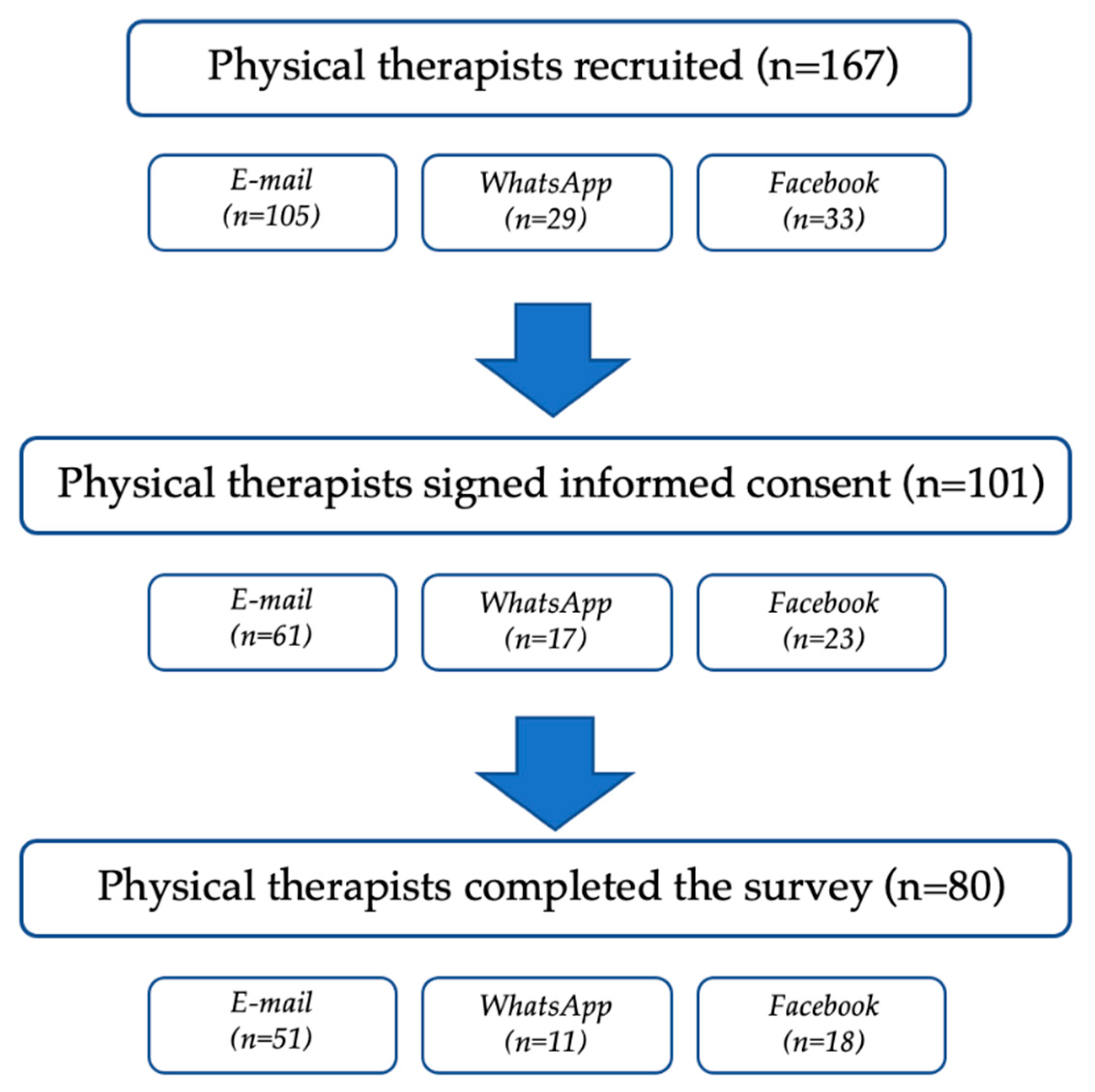
2.1. Participants
2.2. Survey Questionnaire
2.3. Statistical Analysis
3. Results
- -
- Question 4 (Q4—“How much do you feel sure of your working skills during COVID-19 pandemic?”) = 4.3 ± 1.4;
- -
- Question 5 (Q5—“How much does your superior actively work to ensure an optimal organization of the activities?”) = 4.6 ± 1.2;
- -
- Question 6 (Q6—“How much does your superior actively work to ensure good conditions of well-being and employee development?”) = 4.5 ± 1.2;
- -
- Question 7 (Q7—“How much do you feel frustrated in relation to your work?”) = 3.9 ± 1.2;
- -
- Question 8 (Q8—“How much do you feel exposed to the risk of being affected by COVID-19”) = 4.8 ± 1.3;
- -
- Question 9 (Q9—“How much do you fear your colleagues being affected by COVID-19?”) = 4.9 ± 1.1.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Attia, Y.A.; El-Saadony, M.T.; Swelum, A.A.; Qattan, S.Y.; Al-Qurashi, A.D.; Asiry, K.A.; Shafi, M.E.; Elbestawy, A.R.; Gado, A.R.; Khafaga, A.F.; et al. COVID-19: Pathogenesis, advances in treatment and vaccine development and environmental impact—an updated review. Environ. Sci. Pollut. Res. 2021, 28, 22241–22264. [Google Scholar] [CrossRef]
- De Sire, A.; Andrenelli, E.; Negrini, F.; Patrini, M.; Lazzarini, S.G.; Ceravolo, M.G.; Kiekens, C.; Arienti, C.; Ceravolo, M.G.; Côté, P.; et al. Rehabilitation and COVID-19: A rapid living systematic review by cochrane rehabilitation field updated as of December 31st, 2020 and synthesis of the scientific literature of 2020. Eur. J. Phys. Rehabil. Med. 2021, 57, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Demeco, A.; Marotta, N.; Barletta, M.; Pino, I.; Marinaro, C.; Petraroli, A.; Moggio, L.; Ammendolia, A. Rehabilitation of patients post-COVID-19 infection: A literature review. J. Int. Med. Res. 2020, 48. [Google Scholar] [CrossRef] [PubMed]
- Marotta, N.; Demeco, A.; Moggio, L.; Ammendolia, A. Why is telerehabilitation necessary? A pre-post COVID-19 comparative study of ICF activity and participation. J. Enabling Technol. 2021. [Google Scholar] [CrossRef]
- Curci, C.; Negrini, F.; Ferrillo, M.; Bergonzi, R.; Bonacci, E.; Camozzi, D.M.; Ceravolo, C.; De Franceschi, S.; Guarnieri, R.; Moro, P.; et al. Functional outcome after inpatient rehabilitation in post-intensive care unit COVID-19 patients: Findings and clinical implications from a real-practice retrospective study. Eur. J. Phys. Rehabil. Med. 2021. [Google Scholar] [CrossRef]
- Carda, S.; Invernizzi, M.; Bavikatte, G.; Bensmaïl, D.; Bianchi, F.; Deltombe, T.; Draulans, N.; Esquenazi, A.; Francisco, G.E.; Gross, R.; et al. COVID-19 pandemic. What should Physical and Rehabilitation Medicine specialists do? A clinician’s perspective. Eur. J. Phys. Rehabilitation Med. 2020, 56, 515–524. [Google Scholar] [CrossRef]
- Negrini, F.; Ferrario, I.; Mazziotti, D.; Berchicci, M.; Bonazzi, M.; de Sire, A.; Negrini, S.; Zapparoli, L. Neuropsychological Features of Severe Hospitalized Coronavirus Disease 2019 Patients at Clinical Stability and Clues for Postacute Rehabilitation. Arch. Phys. Med. Rehabil. 2021, 102, 155–158. [Google Scholar] [CrossRef]
- Ferraro, F.; Calafiore, D.; Dambruoso, F.; Guidarini, S.; de Sire, A. COVID-19 related fatigue: Which role for rehabilitation in post-COVID-19 patients? A case series. J. Med. Virol. 2021, 93, 1896–1899. [Google Scholar] [CrossRef]
- Vitacca, M.; Carone, M.; Clini, E.M.; Paneroni, M.; Lazzeri, M.; Lanza, A.; Privitera, E.; Pasqua, F.; Gigliotti, F.; Castellana, G.; et al. Joint Statement on the Role of Respiratory Rehabilitation in the COVID-19 Crisis: The Italian Position Paper. Respiration 2020, 99, 493–499. [Google Scholar] [CrossRef]
- Margetić, B.; Peraica, T.; Stojanović, K.; Ivanec, D. Predictors of emotional distress during the COVID-19 pandemic; a Croatian study. Pers. Individ. Dif. 2021, 175, 110691. [Google Scholar] [CrossRef]
- Minahan, J.; Falzarano, F.; Yazdani, N.; Siedlecki, K.L. The COVID-19 Pandemic and Psychosocial Outcomes Across Age Through the Stress and Coping Framework. Gerontologist 2021, 61, 228–239. [Google Scholar] [CrossRef]
- Bettger, J.P.; Thoumi, A.; Marquevich, V.; De Groote, W.; Rizzo Battistella, L.; Imamura, M.; Delgado Ramos, V.; Wang, N.; Dreinhoefer, K.E.; Mangar, A.; et al. COVID-19: Maintaining essential rehabilitation services across the care continuum. BMJ Glob. Heal. 2020, 5, e002670. [Google Scholar] [CrossRef]
- Penati, R.; Begenisic, T.; Zeni, F.; DE Sire, A.; Bernetti, A.; Fiore, P.; Nardone, A. Impact of COVID-19 pandemic on Physical Medicine and Rehabilitation residency: An Italian nationwide epidemiologic survey. Eur. J. Phys. Rehabil. Med. 2021. [Google Scholar] [CrossRef]
- Koffman, J.; Gross, J.; Etkind, S.N.; Selman, L. Uncertainty and COVID-19: How are we to respond? J. R. Soc. Med. 2020, 113, 211–216. [Google Scholar] [CrossRef]
- Ditwiler, R.E.; Swisher, L.L.; Hardwick, D.D. Professional and Ethical Issues in United States Acute Care Physical Therapists Treating Patients With COVID-19: Stress, Walls, and Uncertainty. Phys. Ther. 2021, 101. [Google Scholar] [CrossRef]
- Shechter, A.; Diaz, F.; Moise, N.; Anstey, D.E.; Ye, S.; Agarwal, S.; Birk, J.L.; Brodie, D.; Cannone, D.E.; Chang, B.; et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry 2020, 66, 1–8. [Google Scholar] [CrossRef]
- Trépanier, S.-G.; Fernet, C.; Austin, S. Longitudinal relationships between workplace bullying, basic psychological needs, and employee functioning: A simultaneous investigation of psychological need satisfaction and frustration. Eur. J. Work. Organ. Psychol. 2016, 25, 690–706. [Google Scholar] [CrossRef]
- Collantoni, E.; Saieva, A.; Meregalli, V.; Girotto, C.; Carretta, G.; Boemo, D.; Bordignon, G.; Capizzi, A.; Contessa, C.; Nesoti, M.; et al. Psychological Distress, Fear of COVID-19, and Resilient Coping Abilities among Healthcare Workers in a Tertiary First-Line Hospital during the Coronavirus Pandemic. J. Clin. Med. 2021, 10, 1465. [Google Scholar] [CrossRef] [PubMed]
- Benfante, A.; Di Tella, M.; Romeo, A.; Castelli, L. Traumatic Stress in Healthcare Workers During COVID-19 Pandemic: A Review of the Immediate Impact. Front. Psychol. 2020, 11, 569935. [Google Scholar] [CrossRef] [PubMed]
- Spoorthy, M.S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatr. 2020, 51. [Google Scholar] [CrossRef] [PubMed]
- Panzeri, A.; Rossi Ferrario, S.; Cerutti, P. Psychological Differences Among Healthcare Workers of a Rehabilitation Institute During the COVID-19 Pandemic: A Two-Step Study. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Rieckert, A.; Schuit, E.; Bleijenberg, N.; Ten Cate, D.; De Lange, W.; De Man-Van Ginkel, J.M.; Mathijssen, E.; Smit, L.C.; Stalpers, D.; Schoonhoven, L.; et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open 2021, 11. [Google Scholar] [CrossRef]
- Gómez-Salgado, J.; Domínguez-Salas, S.; Romero-Martín, M.; Ortega-Moreno, M.; García-Iglesias, J.J.; Ruiz-Frutos, C. Sense of coherence and psychological distress among healthcare workers during the COVID-19 pandemic in Spain. Sustainability 2020, 12, 6855. [Google Scholar] [CrossRef]
- Weaver, M.S.; Rosenberg, A.R.; Fry, A.; Shostrom, V.; Wiener, L. The Impact of the Coronavirus Pandemic on Pediatric Palliative Care Team Structures, Services, and Care Delivery. J. Palliat. Med. 2020, 24, 1213–1220. [Google Scholar] [CrossRef]
- Nikčević, A.V.; Marino, C.; Kolubinski, D.C.; Leach, D.; Spada, M.M. Modelling the contribution of the Big Five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. J. Affect. Disord. 2021, 279, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Bennett, P.; Noble, S.; Johnston, S.; Jones, D.; Hunter, R. COVID-19 confessions: A qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open 2020, 10, e043949. [Google Scholar] [CrossRef] [PubMed]
- Duarte, H.; Daros Vieira, R.; Cardozo Rocon, P.; Andrade, A.C.D.S.; Wittmer, V.L.; Capellini, V.K.; Soares, S.C.S.; Paro, F.M. Factors associated with Brazilian physical therapists’ perception of stress during the COVID-19 pandemic: A cross-sectional survey. Psychol. Heal. Med. 2021, 25, 1–12. [Google Scholar] [CrossRef]
- Baert, S.; Lippens, L.; Moens, E.; Sterkens, P.; Weytjens, J. The COVID-19 Crisis and Telework: A Research Survey on Experiences, Expectations and Hopes. IZA Discuss. Pap. 2005. Available online: https://www.iza.org/publications/dp/13229/the-covid-19-crisis-and-telework-a-research-survey-on-experiences-expectations-and-hopes (accessed on 23 July 2021).
- Likert, R. A technique for the measurement of attitudes. Arch. Psychol. 1932, 140, 55. [Google Scholar]
- Choi, J.; Peters, M.; Mueller, R.O. Correlational analysis of ordinal data: From Pearson’s r to Bayesian polychoric correlation. Asia Pacific Educ. Rev. 2010, 11, 459–466. [Google Scholar] [CrossRef]
- Croux, C.; Dehon, C. Influence functions of the Spearman and Kendall correlation measures. Stat. Methods Appl. 2010, 19, 497–515. [Google Scholar] [CrossRef] [Green Version]
- Plonsky, L.; Ghanbar, H. Multiple Regression in L2 Research: A Methodological Synthesis and Guide to Interpreting R2 Values. Mod. Lang. J. 2018, 102, 713–731. [Google Scholar] [CrossRef]
- Jeong, Y.; Jung, M.J. Application and interpretation of hierarchical multiple regression. Orthop. Nurs. 2016, 35, 338–341. [Google Scholar] [CrossRef] [PubMed]
- Serrão, C.; Duarte, I.; Castro, L.; Teixeira, A. Burnout and depression in portuguese healthcare workers during the covid-19 pandemic—the mediating role of psychological resilience. Int. J. Environ. Res. Public Health 2021, 18, 636. [Google Scholar] [CrossRef] [PubMed]
- Farì, G.; de Sire, A.; Giorgio, V.; Rizzo, L.; Bruni, A.; Bianchi, F.P.; Zonno, A.; Pierucci, P.; Ranieri, M.; Megna, M. Impact of COVID-19 on the mental health in a cohort of Italian rehabilitation healthcare workers. J Med. Virol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Pniak, B.; Leszczak, J.; Adamczyk, M.; Rusek, W.; Matosz, P.; Guzik, A. Occupational burnout among active physiotherapists working in clinical hospitals during the COVID-19 pandemic in south-eastern Poland. Work 2021, 68, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Alemanno, F.; Houdayer, E.; Parma, A.; Spina, A.; Del Forno, A.; Scatolini, A.; Angelone, S.; Brugliera, L.; Tettamanti, A.; Beretta, L.; et al. COVID-19 cognitive deficits after respiratory assistance in the subacute phase: A COVID rehabilitation unit experience. PLoS ONE 2021, 16, e0246590. [Google Scholar] [CrossRef]
- Puchner, B.; Sahanic, S.; Kirchmair, R.; Pizzini, A.; Sonnweber, B.; Wöll, E.; Mühlbacher, A.; Garimorth, K.; Dareb, B.; Ehling, R.; et al. Beneficial effects of multi-disciplinary rehabilitation in postacute COVID-19: An observational cohort study. Eur. J. Phys. Rehabil. Med. 2021, 57. [Google Scholar] [CrossRef]
- Yang, S.; Kwak, S.G.; Ko, E.J.; Chang, M.C. The mental health burden of the covid-19 pandemic on physical therapists. Int. J. Environ. Res. Public Health 2020, 17, 3723. [Google Scholar] [CrossRef]
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Min, B.Q.; Tian, Q.; Leng, H.X.; Du, J.L.; et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, D.G.; Musa, J.S. Impact of the corona virus disease 2019 pandemic on physiotherapy services in Nigeria. J. Heal. Res. 2021, 35, 369–373. [Google Scholar] [CrossRef]
- Fava, G.A.; McEwen, B.S.; Guidi, J.; Gostoli, S.; Offidani, E.; Sonino, N. Clinical characterization of allostatic overload. Psychoneuroendocrinology 2019, 108, 94–101. [Google Scholar] [CrossRef]
- Simonelli, C.; Paneroni, M.; Fokom, A.G.; Saleri, M.; Speltoni, I.; Favero, I.; Garofali, F.; Scalvini, S.; Vitacca, M. How the COVID-19 infection tsunami revolutionized the work of respiratory physiotherapists: An experience from Northern Italy. Monaldi Arch. Chest Dis. 2020, 90, 292–298. [Google Scholar] [CrossRef]
- Snowdon, D.A.; Cooke, S.; Lawler, K.; Scroggie, G.; Williams, K.; Taylor, N.F. Physiotherapists prefer clinical supervision to focus on professional skill development: A qualitative study. Physiother. Canada 2020, 72, 249–257. [Google Scholar] [CrossRef]
- Snowdon, D.A.; Leggat, S.G.; Harding, K.E.; Scroggie, G.; Hau, R.; Darzins, P.; Taylor, N.F. Direct supervision of physiotherapists improves compliance with clinical practice guidelines for patients with hip fracture: A controlled before-and-after study. Disabil. Rehabil. 2020, 42, 3825–3832. [Google Scholar] [CrossRef]
- Gianola, S.; Bargeri, S.; Campanini, I.; Corbetta, D.; Gambazza, S.; Innocenti, T.; Meroni, R.; Castellini, G.; Turolla, A. The Spread of COVID-19 Among 15,000 Physical Therapists in Italy: A Cross-Sectional Study. Phys. Ther. 2021, 101. [Google Scholar] [CrossRef] [PubMed]
- Varona, J.F.; Madurga, R.; Peñalver, F.; Abarca, E.; Almirall, C.; Cruz, M.; Ramos, E.; Castellano Vázquez, J.M. Seroprevalence of SARS-CoV-2 antibodies in over 6000 healthcare workers in Spain. Int. J. Epidemiol. 2021, 50, 400–409. [Google Scholar] [CrossRef]
- Theorell, T. COVID-19 and Working Conditions in Health Care. Psychother. Psychosom. 2020, 89, 193–194. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Wei, J.; Zhu, H.; Duan, Y.; Geng, W.; Hong, X.; Jiang, J.; Zhao, X.; Zhu, B. A Study of Basic Needs and Psychological Wellbeing of Medical Workers in the Fever Clinic of a Tertiary General Hospital in Beijing during the COVID-19 Outbreak. Psychother. Psychosom. 2020, 89, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Alkassabi, O.Y.; Al-Sobayel, H.; Al-Eisa, E.S.; Buragadda, S.; Alghadir, A.H.; Iqbal, A. Job satisfaction among physiotherapists in Saudi Arabia: Does the leadership style matter? BMC Health Serv. Res. 2018, 18, 422. [Google Scholar] [CrossRef] [Green Version]
- Hou, T.; Zhang, T.; Cai, W.; Song, X.; Chen, A.; Deng, G.; Ni, C. Social support and mental health among health care workers during Coronavirus Disease 2019 outbreak: A moderated mediation model. PLoS ONE 2020, 15, e0233831. [Google Scholar] [CrossRef] [PubMed]

| Domain A: Epidemiologic questions |
| (Q1) How long have you been working in this Region and in which sector do you work? |
| (Q2) What has significantly changed in your work duties during COVID-19 pandemic? |
| (Q3) Have you performed a specific course/training to manage COVID-19 issues in your workplace? |
| Domain B: Questions on psychological distress and work environment (7-point Likert scale) |
| (Q4) How much do you feel sure of your working skills during COVID-19 pandemic? |
| (Q5) How much does your superior actively work to ensure an optimal organization of the activities? |
| (Q6) How much does your superior actively work to ensure good conditions of well-being and employee development? |
| (Q7) How much do you feel frustrated in relation to your work? |
| (Q8) How much do you feel exposed to the risk of being affected by COVID-19? |
| (Q9) How much do you fear your colleagues being affected by COVID-19? |
| Total (n = 80) | |
|---|---|
| Male/female | 29/51 |
| Age (years) | 32.5 ± 10.1 |
| Physical therapists working in the private sector (%) | 49 (61.3) |
| Physical therapists working in the National Health System (%) | 31 (38.7) |
| Variable | In Which Sector Do You Work? | Age | Gender |
|---|---|---|---|
| In which sector do you work? | — | ||
| Age | 0.04 | — | |
| Gender | 0.14 | 0.03 | — |
| Q4 | −0.32 * | 0.13 | −0.04 |
| Q5 | −0.02 | −0.06 | −0.06 |
| Q6 | −0.48 ** | 0.01 | −0.16 |
| Q7 | 0.16 | 0.18 | −0.09 |
| Q8 | 0.06 | −0.03 | 0.09 |
| Q9 | 0.16 | 0.08 | 0.05 |
| Variable | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
|---|---|---|---|---|---|---|
| 1. Q4 | — | |||||
| 2. Q5 | 0.52 *** | — | ||||
| 3. Q6 | 0.36 * | 0.50 *** | — | |||
| 4. Q7 | −0.24 | −0.30 * | −0.27 | — | ||
| 5. Q8 | −0.03 | −0.26 | 0.01 | 0.31 | — | |
| 6. Q9 | −0.04 | −0.06 | −0.24 * | 0.50 ** | 0.69 *** | — |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Sire, A.; Marotta, N.; Raimo, S.; Lippi, L.; Inzitari, M.T.; Tasselli, A.; Gimigliano, A.; Palermo, L.; Invernizzi, M.; Ammendolia, A. Psychological Distress and Work Environment Perception by Physical Therapists from Southern Italy during COVID-19 Pandemic: The C.A.L.A.B.R.I.A Study. Int. J. Environ. Res. Public Health 2021, 18, 9676. https://doi.org/10.3390/ijerph18189676
de Sire A, Marotta N, Raimo S, Lippi L, Inzitari MT, Tasselli A, Gimigliano A, Palermo L, Invernizzi M, Ammendolia A. Psychological Distress and Work Environment Perception by Physical Therapists from Southern Italy during COVID-19 Pandemic: The C.A.L.A.B.R.I.A Study. International Journal of Environmental Research and Public Health. 2021; 18(18):9676. https://doi.org/10.3390/ijerph18189676
Chicago/Turabian Stylede Sire, Alessandro, Nicola Marotta, Simona Raimo, Lorenzo Lippi, Maria Teresa Inzitari, Anna Tasselli, Alessandra Gimigliano, Liana Palermo, Marco Invernizzi, and Antonio Ammendolia. 2021. "Psychological Distress and Work Environment Perception by Physical Therapists from Southern Italy during COVID-19 Pandemic: The C.A.L.A.B.R.I.A Study" International Journal of Environmental Research and Public Health 18, no. 18: 9676. https://doi.org/10.3390/ijerph18189676






