Walking Ability Outcome Measures in Individuals with Spinal Cord Injury: A Systematic Review
Abstract
:1. Introduction
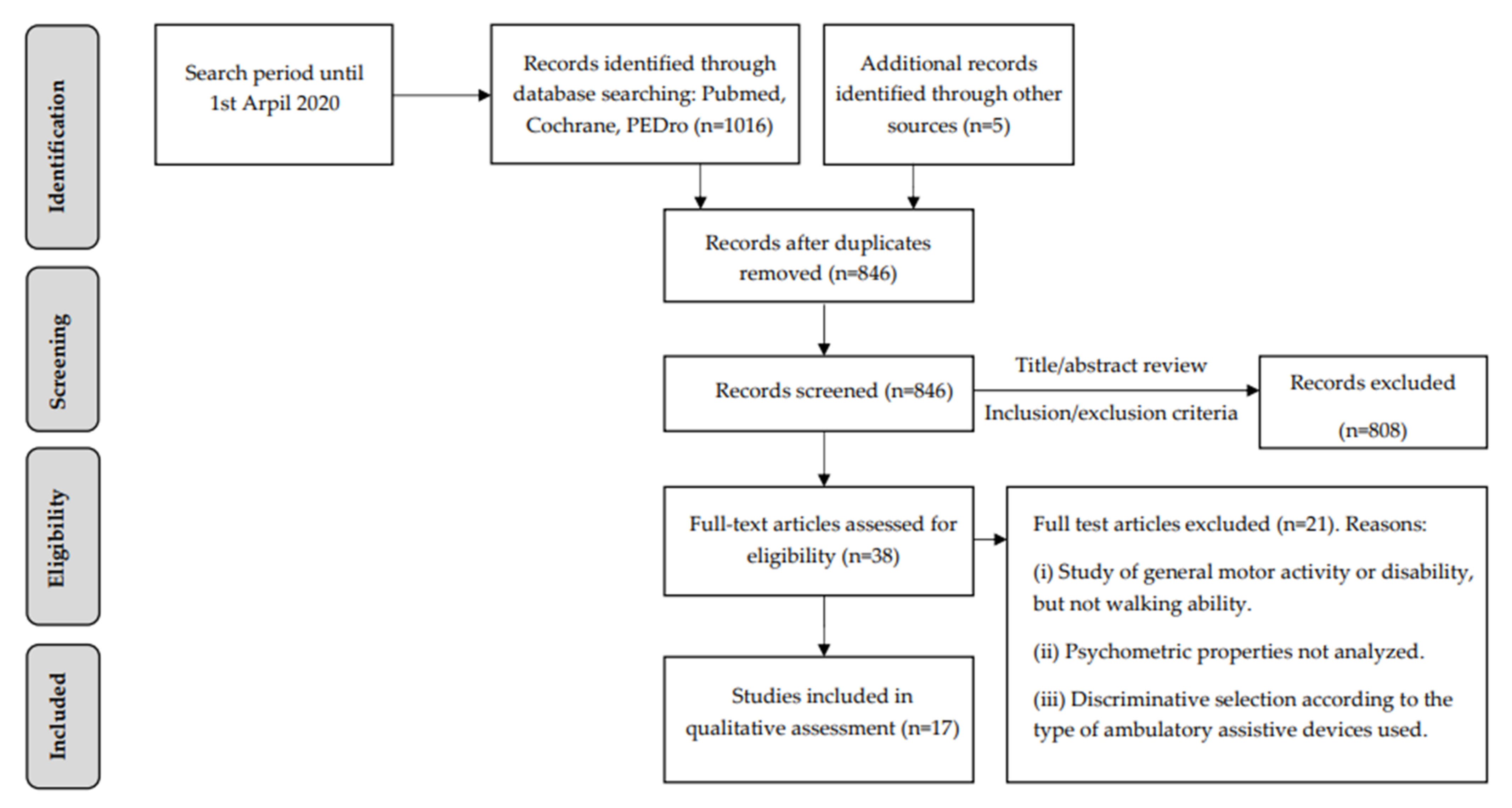
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Collection
3. Results
3.1. Synthesis of the Results
3.1.1. The Gait Profile Score
3.1.2. The 10 Meter Walk Test
3.1.3. The Spinal Cord Injury Functional Ambulation Profile
3.1.4. The Timed up and Go Test
3.1.5. The Five Times Sit-to-Stand Test
3.1.6. The Six-Minute Walk Test
3.1.7. The Walking Index for Spinal Cord Injury (WISCI)
3.1.8. The Spinal Cord Injury Functional Ambulation Inventory
3.1.9. The Spinal Cord Independence Measure mobility items
3.1.10. The Locomotor Stages in Spinal Cord Injury
3.1.11. The Berg Balance Scale
3.1.12. The Community Balance and Mobility Scale
3.1.13. The Activity-based Balance Level Evaluation Scale
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singh, A.; Tetreault, L.; Kalsi-Ryan, S.; Nouri, A.; Fehlings, M.G. Global Prevalence and Incidence of Traumatic Spinal Cord Injury. Clin. Epidemiol. 2014, 6, 309–331. [Google Scholar] [CrossRef] [Green Version]
- Kirshblum, S.C.; Burns, S.P.; Biering-Sorensen, F.; Donovan, W.; Graves, D.E.; Jha, A.; Johansen, M.; Jones, L.; Krassioukov, A.; Mulcahey, M.; et al. International Standards for Neurological Classification of Spinal Cord Injury (Revised 2011). J. Spinal Cord Med. 2011, 34, 535–546. [Google Scholar] [CrossRef] [Green Version]
- Anderson, K.D. Targeting Recovery: Priorities of the Spinal Cord-Injured Population. J. Neurotrauma 2004, 21, 1371–1383. [Google Scholar] [CrossRef]
- Chan, K.; Guy, K.; Shah, G.; Golla, J.; Flett, H.M.; Williams, J.; Musselman, K.E. Retrospective Assessment of the Validity and Use of the Community Balance and Mobility Scale among Individuals with Subacute Spinal Cord Injury. Spinal Cord 2017, 55, 294–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barbeau, H.; Nadeau, S.; Garneau, C. Physical Determinants, Emerging Concepts, and Training Approaches in Gait of Individuals with Spinal Cord Injury. J. Neurotrauma 2006, 23, 571–585. [Google Scholar] [CrossRef]
- Scivoletto, G.; Romanelli, A.; Mariotti, A.; Marinucci, D.; Tamburella, F.; Mammone, A.; Cosentino, E.; Sterzi, S.; Molinari, M. Clinical Factors That Affect Walking Level and Performance in Chronic Spinal Cord Lesion Patients. Spine 2008, 33, 259–264. [Google Scholar] [CrossRef]
- Ditunno, P.L.; Patrick, M.; Stineman, M.; Ditunno, J.F. Who Wants to Walk? Preferences for Recovery after SCI: A Longitudinal and Cross-Sectional Study. Spinal Cord 2008, 46, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Spiess, M.R.; Müller, R.M.; Rupp, R.; Schuld, C.; EM-SCI Study Group; van Hedel, H.J.A. Conversion in ASIA Impairment Scale during the First Year after Traumatic Spinal Cord Injury. J. Neurotrauma 2009, 26, 2027–2036. [Google Scholar] [CrossRef] [PubMed]
- Van Hedel, H.J.A.; Wirz, M.; Dietz, V. Standardized Assessment of Walking Capacity after Spinal Cord Injury: The European Network Approach. Neurol. Res. 2008, 30, 61–73. [Google Scholar] [CrossRef] [Green Version]
- Scivoletto, G.; Tamburella, F.; Laurenza, L.; Foti, C.; Ditunno, J.F.; Molinari, M. Validity and Reliability of the 10-m Walk Test and the 6-Min Walk Test in Spinal Cord Injury Patients. Spinal Cord 2011, 49, 736–740. [Google Scholar] [CrossRef] [PubMed]
- Van Hedel, H.J.A.; Wirz, M.; Curt, A. Improving Walking Assessment in Subjects with an Incomplete Spinal Cord Injury: Responsiveness. Spinal Cord 2006, 44, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.B.; Carnel, C.T.; Ditunno, J.F.; Read, M.S.; Boninger, M.L.; Schmeler, M.R.; Williams, S.R.; Donovan, W.H. Gait and Ambulation Subcommittee Outcome Measures for Gait and Ambulation in the Spinal Cord Injury Population. J. Spinal Cord Med. 2008, 31, 487–499. [Google Scholar] [CrossRef] [Green Version]
- Labruyère, R.; Agarwala, A.; Curt, A. Rehabilitation in Spine and Spinal Cord Trauma. Spine 2010, 35, S259–S262. [Google Scholar] [CrossRef] [PubMed]
- Lam, T.; Noonan, V.K.; Eng, J.J.; SCIRE Research Team. A Systematic Review of Functional Ambulation Outcome Measures in Spinal Cord Injury. Spinal Cord 2008, 46, 246–254. [Google Scholar] [CrossRef] [Green Version]
- Furlan, J.C.; Noonan, V.; Singh, A.; Fehlings, M.G. Assessment of Disability in Patients with Acute Traumatic Spinal Cord Injury: A Systematic Review of the Literature. J. Neurotrauma 2011, 28, 1413–1430. [Google Scholar] [CrossRef] [Green Version]
- Scivoletto, G.; Tamburella, F.; Laurenza, L.; Torre, M.; Molinari, M.; Ditunno, J.F. Walking Index for Spinal Cord Injury Version II in Acute Spinal Cord Injury: Reliability and Reproducibility. Spinal Cord 2014, 52, 65–69. [Google Scholar] [CrossRef] [Green Version]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality Criteria Were Proposed for Measurement Properties of Health Status Questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [Green Version]
- Musselman, K.; Brunton, K.; Lam, T.; Yang, J. Spinal Cord Injury Functional Ambulation Profile: A New Measure of Walking Ability. Neurorehabil. Neural Repair 2011, 25, 285–293. [Google Scholar] [CrossRef]
- Poncumhak, P.; Saengsuwan, J.; Kamruecha, W.; Amatachaya, S. Reliability and Validity of Three Functional Tests in Ambulatory Patients with Spinal Cord Injury. Spinal Cord 2013, 51, 214–217. [Google Scholar] [CrossRef] [PubMed]
- Wirz, M.; Müller, R.; Bastiaenen, C. Falls in Persons with Spinal Cord Injury: Validity and Reliability of the Berg Balance Scale. Neurorehabil. Neural Repair 2010, 24, 70–77. [Google Scholar] [CrossRef]
- Van Hedel, H.J.A.; Dietz, V.; European Multicenter Study on Human Spinal Cord Injury (EM-SCI) Study Group. Walking during Daily Life Can Be Validly and Responsively Assessed in Subjects with a Spinal Cord Injury. Neurorehabil. Neural Repair 2009, 23, 117–124. [Google Scholar] [CrossRef]
- Wedege, P.; Steffen, K.; Strøm, V.; Opheim, A.I. Reliability of Three-Dimensional Kinematic Gait Data in Adults with Spinal Cord Injury. J. Rehabil. Assist. Technol. Eng. 2017, 4, 2055668317729992. [Google Scholar] [CrossRef] [Green Version]
- Van Hedel, H.J.; Wirz, M.; Dietz, V. Assessing Walking Ability in Subjects with Spinal Cord Injury: Validity and Reliability of 3 Walking Tests. Arch. Phys. Med. Rehabil. 2005, 86, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Marino, R.J.; Scivoletto, G.; Patrick, M.; Tamburella, F.; Read, M.S.; Burns, A.S.; Hauck, W.; Ditunno, J. Walking Index for Spinal Cord Injury Version 2 (WISCI-II) with Repeatability of the 10-m Walk Time: Inter- and Intrarater Reliabilities. Am. J. Phys. Med. Rehabil 2010, 89, 7–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morganti, B.; Scivoletto, G.; Ditunno, P.; Ditunno, J.F.; Molinari, M. Walking Index for Spinal Cord Injury (WISCI): Criterion Validation. Spinal Cord 2005, 43, 27–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ditunno, J.F.; Barbeau, H.; Dobkin, B.H.; Elashoff, R.; Harkema, S.; Marino, R.J.; Hauck, W.W.; Apple, D.; Basso, D.M.; Behrman, A.; et al. Validity of the Walking Scale for Spinal Cord Injury and Other Domains of Function in a Multicenter Clinical Trial. Neurorehabil. Neural Repair 2007, 21, 539–550. [Google Scholar] [CrossRef]
- Field-Fote, E.C.; Fluet, G.G.; Schafer, S.D.; Schneider, E.M.; Smith, R.; Downey, P.A.; Ruhl, C.D. The Spinal Cord Injury Functional Ambulation Inventory (SCI-FAI). J. Rehabil. Med. 2001, 33, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Maurer-Burkhard, B.; Smoor, I.; von Reumont, A.; Deckstein, G.; Stierle, I.; Rupp, R.; Schuld, C. Validity and Reliability of a Locomotor Stage-Based Functional Rating Scale in Spinal Cord Injury. Spinal Cord 2016, 54, 619–625. [Google Scholar] [CrossRef] [Green Version]
- Lemay, J.-F.; Nadeau, S. Standing Balance Assessment in ASIA D Paraplegic and Tetraplegic Participants: Concurrent Validity of the Berg Balance Scale. Spinal Cord 2010, 48, 245–250. [Google Scholar] [CrossRef]
- Ardolino, E.M.; Hutchinson, K.J.; Pinto Zipp, G.; Clark, M.; Harkema, S.J. The ABLE Scale: The Development and Psychometric Properties of an Outcome Measure for the Spinal Cord Injury Population. Phys. Ther. 2012, 92, 1046–1054. [Google Scholar] [CrossRef] [PubMed]
- Murphy, A.T.; Kravtsov, S.; Sangeux, M.; Rawicki, B.; New, P.W. Utilizing Three Dimensional Clinical Gait Analysis to Optimize Mobility Outcomes in Incomplete Spinal Cord Damage. Gait Posture 2019, 74, 53–59. [Google Scholar] [CrossRef]
- Baker, R.; McGinley, J.L.; Schwartz, M.H.; Beynon, S.; Rozumalski, A.; Graham, H.K.; Tirosh, O. The Gait Profile Score and Movement Analysis Profile. Gait Posture 2009, 30, 265–269. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Whitney, S.L.; Wrisley, D.M.; Marchetti, G.F.; Gee, M.A.; Redfern, M.S.; Furman, J.M. Clinical Measurement of Sit-to-Stand Performance in People with Balance Disorders: Validity of Data for the Five-Times-Sit-to-Stand Test. Phys. Ther. 2005, 85, 1034–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meretta, B.M.; Whitney, S.L.; Marchetti, G.F.; Sparto, P.J.; Muirhead, R.J. The Five Times Sit to Stand Test: Responsiveness to Change and Concurrent Validity in Adults Undergoing Vestibular Rehabilitation. J. Vestib. Res. 2006, 16, 233–243. [Google Scholar] [PubMed]
- Lord, S.R.; Murray, S.M.; Chapman, K.; Munro, B.; Tiedemann, A. Sit-to-Stand Performance Depends on Sensation, Speed, Balance, and Psychological Status in Addition to Strength in Older People. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, M539–M543. [Google Scholar] [CrossRef]
- Brooks, D.; Solway, S.; Gibbons, W.J. ATS Statement on Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2003, 167, 1287. [Google Scholar] [CrossRef]
- Butland, R.J.; Pang, J.; Gross, E.R.; Woodcock, A.A.; Geddes, D.M. Two-, Six-, and 12-Minute Walking Tests in Respiratory Disease. Br. Med. J. (Clin. Res. Ed.) 1982, 284, 1607–1608. [Google Scholar] [CrossRef] [Green Version]
- Ditunno, J.F.; Ditunno, P.L.; Graziani, V.; Scivoletto, G.; Bernardi, M.; Castellano, V.; Marchetti, M.; Barbeau, H.; Frankel, H.L.; D’Andrea Greve, J.M.; et al. Walking Index for Spinal Cord Injury (WISCI): An International Multicenter Validity and Reliability Study. Spinal Cord 2000, 38, 234–243. [Google Scholar] [CrossRef] [Green Version]
- Dittuno, P.L.; Ditunno, J.F.; Dittuno, J.F. Walking Index for Spinal Cord Injury (WISCI II): Scale Revision. Spinal Cord 2001, 39, 654–656. [Google Scholar] [CrossRef]
- Burns, A.S.; Delparte, J.J.; Patrick, M.; Marino, R.J.; Ditunno, J.F. The Reproducibility and Convergent Validity of the Walking Index for Spinal Cord Injury (WISCI) in Chronic Spinal Cord Injury. Neurorehabil. Neural Repair 2011, 25, 149–157. [Google Scholar] [CrossRef]
- Perry, J.; Garrett, M.; Gronley, J.K.; Mulroy, S.J. Classification of Walking Handicap in the Stroke Population. Stroke 1995, 26, 982–989. [Google Scholar] [CrossRef]
- Catz, A.; Itzkovich, M.; Agranov, E.; Ring, H.; Tamir, A. SCIM--Spinal Cord Independence Measure: A New Disability Scale for Patients with Spinal Cord Lesions. Spinal Cord 1997, 35, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Catz, A.; Itzkovich, M.; Steinberg, F.; Philo, O.; Ring, H.; Ronen, J.; Spasser, R.; Gepstein, R.; Tamir, A. The Catz-Itzkovich SCIM: A Revised Version of the Spinal Cord Independence Measure. Disabil. Rehabil. 2001, 23, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Catz, A.; Itzkovich, M.; Tesio, L.; Biering-Sorensen, F.; Weeks, C.; Laramee, M.T.; Craven, B.C.; Tonack, M.; Hitzig, S.L.; Glaser, E.; et al. A Multicenter International Study on the Spinal Cord Independence Measure, Version III: Rasch Psychometric Validation. Spinal Cord 2007, 45, 275–291. [Google Scholar] [CrossRef]
- Banaszek, G. Vojta’s method as the early neurodevelopmental diagnosis and therapy concept. Przegl Lek 2010, 67, 67–76. [Google Scholar]
- Berg, K. Measuring Balance in the Elderly: Preliminary Development of an Instrument. Physiother. Can. 1989, 41, 304–311. [Google Scholar] [CrossRef]
- Inness, E.L.; Howe, J.-A.; Niechwiej-Szwedo, E.; Jaglal, S.B.; McIlroy, W.E.; Verrier, M.C. Measuring Balance and Mobility after Traumatic Brain Injury: Validation of the Community Balance and Mobility Scale (CB&M). Physiother. Can. 2011, 63, 199–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forrest, G.F.; Hutchinson, K.; Lorenz, D.J.; Buehner, J.J.; Vanhiel, L.R.; Sisto, S.A.; Basso, D.M. Are the 10 Meter and 6 Minute Walk Tests Redundant in Patients with Spinal Cord Injury? PLoS ONE 2014, 9, e94108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guyatt, G.H.; Pugsley, S.O.; Sullivan, M.J.; Thompson, P.J.; Berman, L.; Jones, N.L.; Fallen, E.L.; Taylor, D.W. Effect of Encouragement on Walking Test Performance. Thorax 1984, 39, 818–822. [Google Scholar] [CrossRef] [Green Version]
- Musselman, K.E.; Yang, J.F. Spinal Cord Injury Functional Ambulation Profile: A Preliminary Look at Responsiveness. Phys. Ther. 2014, 94, 240–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ball, C.; Sackett, D.; Phillips, B.; Haynes, B.; Straus, S. Levels of Evidence and Grades of Recommendations. Available online: http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ (accessed on 8 July 2021).
| Property | Definition | Standard Value |
|---|---|---|
| Reliability | Reproducibility: degree to which the score is free from random error (including test re-test reliability, intra- and interrater reliability) [14]. Internal consistency: homogeneity of the items [14]. | Intra- and interrater reliability (Spearman or Pearson coefficients, k coefficient 1, ICC 2): ≥0.75 excellent, 0.40–0.74 moderate, ≤0.39 poor [14]. Test re-test reliability: SRD 3 [16]. Cronbach’s α: ≥0.80 excellent, 0.70–0.79 adequate, ≤0.69 poor [14]. |
| Validity | Assessing if the instrument actually measures what it intends to measure [14]. Criterion validity (concurrent, convergent, predictive) is the extent to which scores on a particular questionnaire relate to a gold standard. For most of the functional scales, there was no criterion standard and, hence, construct validity was used [17]. | Jaspen coefficient of multiserial correlation (M) [18], point biserial correlation coefficient (rpb) [19], Spearman (ρ) or Pearson (r) coefficients: ≥0.70 excellent, 0.50–0.69 moderate, ≤0.49 poor [14]. |
| Responsiveness | The ability of a questionnaire to detect clinically important changes over time [17]. Floor or ceiling effect: the number of respondents who achieved the lowest (floor) or highest (ceiling) possible score [17]. | SRD 3 [14], ROC analysis 4 [20], p−value 5 [11], SRM 6 (0.20 small, 0.50 medium, >0.80 large responsiveness), linear regression analysis [21]. Problematic when >20% of subjects received either minimum or maximum scores [14]. |
| Categories | Outcome Measures |
|---|---|
| Multivariate walking metrics | GPS 1 |
| Spatiotemporal-related walking/balance measures | |
| Timed measures | |
| Speed-related walking tests | 10MWT 2 |
| SCI-FAP 3 | |
| Speed-related balance tests | TUGT 4 |
| FTSST 5 | |
| Distance measures (endurance-related walking tests) | 6MWT 6 |
| Categorical measures of ambulation | |
| Walking assessment measures | WISCI 7 |
| SCI-FAI 8 | |
| Multidimensional measures (locomotor-related subscales) | SCIMIOMob 9 |
| LOSSCI 10 | |
| Balance measures | BBS 11 |
| CB&M 12 scale | |
| ABLE 13 scale |
| Reference | Outcome Measures | Sample Size | Injury Features: Etiology (E) AIS 1 | Population: Age (Mean ± SD) Gender (M/F) 2 | Inclusion/Exclusion Criteria (IC/EC) | Psychometric Properties | Results |
|---|---|---|---|---|---|---|---|
| Wedege et al. [22] | GPS | 15 | E: Traumatic and non-traumatic. AIS 1: D. | Age range: 25–62 11 M/4 F. | IC: ≥ 1 year post-injury, ability to walk 10 m without personal assistance. EC: other diseases affecting gait; BTIs 3 and orthopedic treatment or neurosurgery in the lower limbs within the last 3–6 months. | Inter-and intra-session reliability. | ICC ≥ 0.93 (intersession, except hip rotation), ≥0.96 (intrasession). |
| Van Hedel et al. [23] | 10MWT 6MWT TUGT | 22 75 | E: Traumatic and ischemic. AIS 1: A-D. | Reliability group: 52 ± 20 14 M/8 F. Validity group: 54 ± 20 45 M/30 F. | IC: WISCI II > 0 and no additional gait impairments. | Inter- and intrarater reliability and concurrent validity. | r > 0.97; |r| > 0.88 (10MWT, 6MWT, and TUGT correlated between each other), |ρ| > 0.60 (correlated with WISCI II). |
| Poncumhak et al. [19] | 10MWT TUGT FTSST | 66 16 | E: Traumatic and non-traumatic. AIS 1: C, D. | Validity groups: FIML 4 6: 50.9 ± 13.4 22 M/11 F. FIML 4 7: 50.2 ± 9.5 24 M/9 F. Reliability group: 50.8 ± 10.3 11 M/5 F. | IC: ability to stand up independently and to walk at least 50 m with or without AADs 5 (FIML 4 scores 6–7). | Concurrent validity and interrater reliability. | rpb = 0.78, −0.69, −0.60 (10MWT, TUGT, and FTSST correlated with FIML 4, respectively); ICC = 0.997–1.00 |
| Van Hedel et al. [11] | WISCI II 6MWT 10MWT | 22 | E: Traumatic and non-traumatic. AIS 1: N/A 6. | 45.5 ± 16.7 18 M/4 F. | IC: functional ambulation within the first month after injury (WISCI II ≥ 1). | Responsiveness. | WISCI II (over the first 3 months): p = 0.005; 6MWT and 10MWT (over the first 6 months): p < 0.001–0.01 |
| Scivoletto et al. [10] | 10MWT | 37 | E: Traumatic and non-traumatic. AIS 1: C, D. | Age range: 19–77 28 M/9 F. | IC: functional ambulation at home or community, with or without the use of AADs 5. EC: cognitive deficit, cardiac or lung diseases. | Inter- and intrarater reliability. | ICC = 0.95–0.99; p = 0.09 (in both dynamic and static start conditions). |
| Musselman et al. [18] | SCI-FAP | 32 60 able-bodied. | E: N/A 6. AIS 1: C, D. | 47.6 ± 14.2 24 M/8 F. 42.9 ± 16.0 34 M/26 F. | IC: ≥ 6 months after injury, ability to walk ≥ 5 m with or without physical assistance and/or AADs 5, free of any disease and changes in medications affecting walking ability, not receiving walking training. IC: > 18 years, ≤ 1 fall in the previous month, free of any disease affecting walking ability. | Interrater and test-retest reliability, internal consistency, convergent and discriminative validity. | ICC = 1.00 (interrater), 0.98 (test-retest); α = 0.95; r = −0.59 (correlated with 10MWT and 6MWT), M = 0.68 (correlated with WISCI II), higher scores in injured individuals related to able-bodied ones. |
| Marino et al. [24] | WISCI II | 26 | E: Traumatic and non-traumatic. AIS 1: A, C, and D. | 46.4 ± 19.3 16 M/10 F. | IC: ≥ 6 months after injury, independent lower limb weight bearing once a week. EC: SS 7 WISCI < 6 or equal to 20, any other medical condition which could limit safety ambulation. | Intra- and interrater reliability. | SS 7 WISCI: ICC = 1.00 (intra- and interrater). Maximum WISCI: ICC = 1.00 (intra-), 0.98 (interrater). |
| Morganti et al. [25] | WISCI II | 76 | E: Traumatic and non-traumatic. AIS 1: A-D. | 50.4 ± 19.3 184 M/100 F. | IC: WISCI > 0 and < 20.EC: cognitive impairments that disable to participate in the rehabilitation program. | Concurrent validity. | Correlation with SCIM IMob items (ρ = 0.97) and FIML 4 (ρ =0.70). |
| Ditunno et al. [26] | WISCI II | 146 | E: Traumatic. AIS 1: B-D. | Age range: 16–69 78% M/22% F. | IC: subjects within 8 weeks of onset of injury and within 1 week of admission for rehabilitation. EC: FIML 4 > 3. | Concurrent and predictive validity. | Correlations at 6 months with BBS (ρ = 0.90), FIML 4 (ρ = 0.89), and 6MWT (ρ = 0.79). |
| Scivoletto et al. [16] | WISCI II | 33 | E: Traumatic. AIS 1: C, D. | Median age: 44. 28 M/5 F. | IC: subjects within 3 months of onset of injury, with a motor level of C4-L1 inclusive. | Intra- and interrater reliability, and test re-test reliability. | Maximum WISCI II scores: ICC = 0.975–0.999; SRD = 1.15, 1.68 (tetra- and paraplegics, respectively). |
| Field-Fote et al. [27] | SCI-FAI | 22 19 | E: N/A 6. AIS 1: N/A 6. | Validity/reliability group: 32 ± 13 17 M/5 F. Sensitivity group: 31.7 ± 9.4 13 M/6 F. | IC: ability to maintain stance on the weight-bearing limb independently and to take at least 8 steps using any AADs 5. IC: N/A 6. | Intra- and interrater reliability, convergent validity, and sensitivity. | ICC = 0.70–0.96; r = −0.74, −0.70 (gait score correlated with the 10 feet-walking speed); r = 0.58 (gait score correlated with LEMS 8 to assess sensitivity). |
| Van Hedel et al. [21] | SCIM II IOMob items | 886 | E: Traumatic. AIS 1 A: 413 AIS 1 B: 113 AIS 1 C: 137 AIS 1 D: 223 | 39 ± 18; 19% F. 42 ± 18; 27% F. 48 ± 20; 32% F. 47 ± 17; 22% F. | IC: patients classified with AIS at 1 month after injury and assessed at least at 2 successive time points (at 2 weeks and 1, 3, 6, and 12 months after injury) with SCIM II and either the 10MWT or WISCI II. | Concurrent, validity, internal, and external responsiveness. | IMob items correlated with 10MWT and WISCI II in AIS C-D: ρ = 0.75–0.91; SRM = 0.67–1.24 (IOMob items in AIS C-D); linear regression analysis = 0.79 (IMob items correlated with 10MWT in AIS C). |
| Maurer-Burkhard et al. [28] | LOSSCI | 65 161 | E: N/A 6. AIS 1: C, D. E: N/A 6. AIS 1: A-D. | Reliability group: 44.9 ± 16.0 77% M/23% F. Validity group: 48.3 ± 20.2 65.8% M/34.2% F. | IC: 18–80 years, ≥ 8 weeks after injury, having been assessed by 2 raters in 2 successive assessments within 1–5 days. IC: SCIM databases from the EM-SCI 9 obtained within the first year after injury. | Interrater reliability and construct validity. | WCk 10: 0.98; ρ = 0.77–0.82 (correlated with SCIM IOMob items). |
| Lemay et al. [29] | BBS | 32 | E: Traumatic and non-traumatic. AIS 1: D. | 47.9 ± 12.8 25 M/7 F. | IC: ability to walk 10 m independently with or without AADs 5. EC: other neurological conditions or existence of walking difficulties before the injury. | Concurrent validity and responsiveness. | ρ = 0.71–0.82 (correlated with the SCI-FAI, WISCI II, 10MWT and TUGT); ceiling effect: 44.8% (WISCI II), 68.8% (gait score SCI-FAI), 34.4% (BBS and Walking Mobility and assistive devices section of SCI-FAI). |
| Wirz et al. [20] | BBS | 42 | E: Traumatic and non-traumatic. AIS 1: A-D. | 49.3 ± 11.5 33 M/9 F. | IC: ≥ 1 year after injury prior to enrollment, ability to walk unless 15 m. EC: < 18 or > 65 years, vestibular or visual systems impairments, and others affecting standing or walking function. | Construct validity, interrater reliability, and responsiveness. | ρ = −0.82, −0.89, −0.93 (correlated with WISCI II, SCIM II Mob items, and 10MWT, respectively); ICC = 0.95; ROC = 0.48 (95% confidence interval = 0.29–0.67), ρ = −0.17 (number of falls), ceiling effect: ±1/3 of subjects (BBS, WISCI II, SCIM II). |
| Chan et al. [4] | CB&M scale | 30 | E: Traumatic and non-traumatic. AIS 1: C, D. | 38.3 ± 15.3 23 M/7 F. | IC: < 65 years, FIM 4 ≥ 115 at discharge, ability to complete the CB&M scale and any other balance or walking outcome measures within one week of each other. EC: significant comorbid condition. | Convergent validity, internal consistency. | r = 0.47–0.72 (correlation with the 6MWT, 10MWT and BBS); α = 0.87 |
| Ardolino et al. [30] | ABLE scale | 104 | E: Traumatic. AIS 1: A–D. | 38.6 ± 15.0 79 M/25 F. | IC: ≥ 16 years, traumatic origin of the injury. EC: inability to tolerate upright supported sitting for at least 1 min, need for a spinal stabilization device, limited ability to bend or rotate, inability to follow 2-step commands. | Responsiveness. | Minimal floor and ceiling effects. |
| Reliability | Validity | Responsiveness | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Inter- and Intrasession | Test Re-Test | Intrarater | Interrater | Internal Consistency | Concurrent Convergent | Construct | Predictive | Floor/Ceiling Effects | |
| GPS | +++ | ||||||||
| 10MWT | +++ | +++ | ++/+++ | * | |||||
| SCI-FAP | +++ | +++ | +++ | ++ | Ceiling | ||||
| TUGT | +++ | +++ | ++/+++ | ||||||
| FTSST | +++ | ++ | |||||||
| 6MWT | +++ | +++ | ++/+++ | * | |||||
| WISCI II | ++ | +++ | +++ | +++ | +++ | * Ceiling | |||
| SCI-FAI | +++ | ++/+++ | +++ | ++ Ceiling | |||||
| SCIM IIIOMob | +++ | ++/+++ | |||||||
| LOSSCI | +++ | +++ | |||||||
| BBS | +++ | +++ | +++ | + Ceiling | |||||
| CB&M scale | +++ | +/++/+++ | |||||||
| ABLE scale | Ceiling/Floor | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sinovas-Alonso, I.; Gil-Agudo, Á.; Cano-de-la-Cuerda, R.; del-Ama, A.J. Walking Ability Outcome Measures in Individuals with Spinal Cord Injury: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9517. https://doi.org/10.3390/ijerph18189517
Sinovas-Alonso I, Gil-Agudo Á, Cano-de-la-Cuerda R, del-Ama AJ. Walking Ability Outcome Measures in Individuals with Spinal Cord Injury: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(18):9517. https://doi.org/10.3390/ijerph18189517
Chicago/Turabian StyleSinovas-Alonso, Isabel, Ángel Gil-Agudo, Roberto Cano-de-la-Cuerda, and Antonio J. del-Ama. 2021. "Walking Ability Outcome Measures in Individuals with Spinal Cord Injury: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 18: 9517. https://doi.org/10.3390/ijerph18189517







