Impacts of the Goldmining and Chronic Methylmercury Exposure on the Good-Living and Mental Health of Munduruku Native Communities in the Amazon Basin
Abstract
1. Introduction
For us, the river is the place where we take our food from. We drink the river, we bathe in the river. For us the breast milk, as we say, is the riverbed. The same river also runs in people’s veins. Without the river, there will be no “us”. Without water, nobody can live. Our river is our mother. So it is with the forest. They are sacred because they came from a story in which our ancestors made the Tapajós River with water squeezed from tucumã woodworms.
2. Materials and Methods
2.1. Sampling
2.2. Fieldwork
2.3. Data Collection Instruments
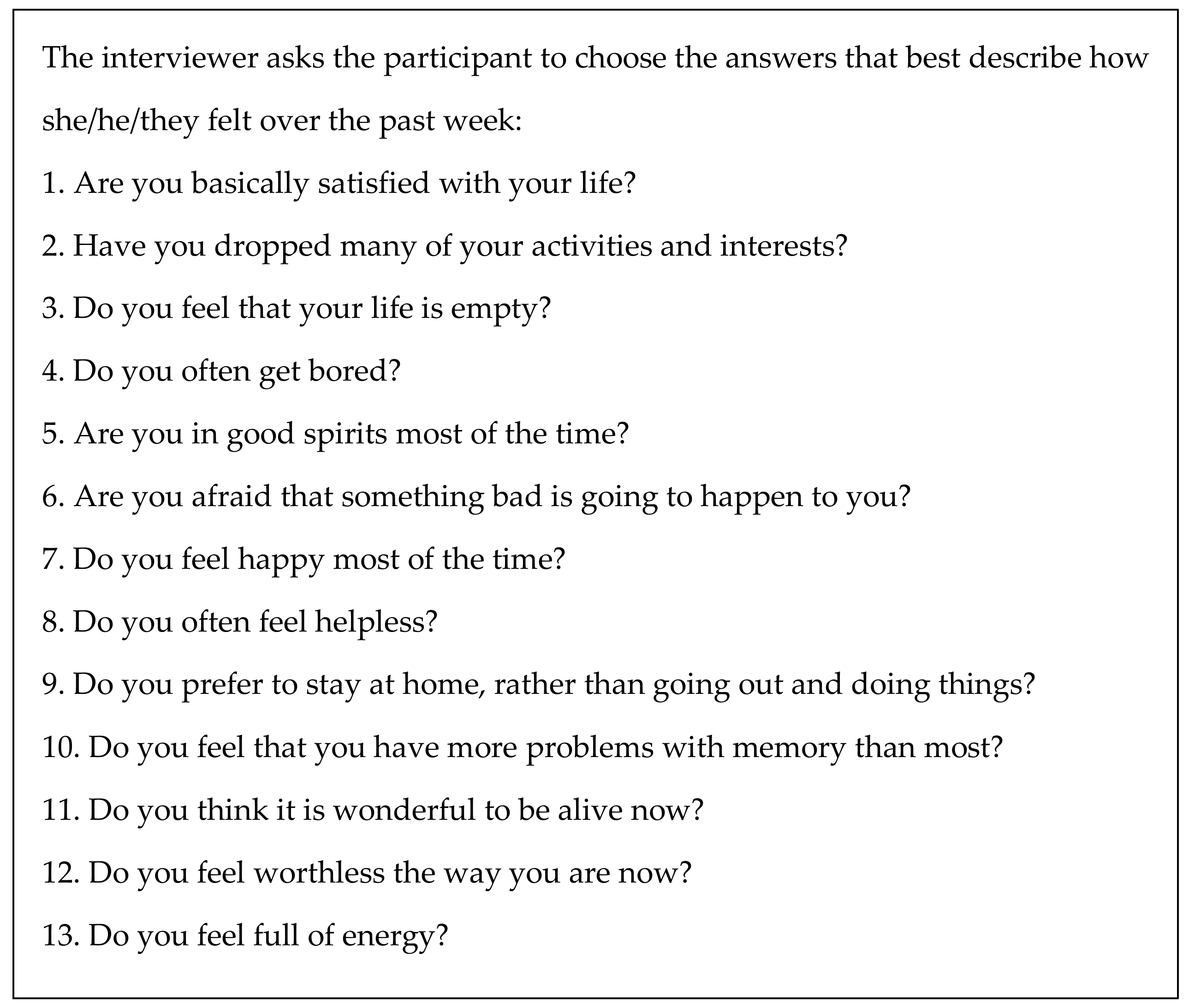
2.3.1. Geriatric Depression Scale—Short Form
2.3.2. Brief Non-Structured Interviews
2.3.3. Mercury Exposure Biomarker
2.4. Statistical Analysis
3. Results
3.1. Mercury Exposure
3.2. GDS-SF
3.3. Brief Non-Structured Interviews
The forest (auadip) is beautiful to me; it makes me joyful and makes me recognize who I am. If I am not in the forest, I feel strange, unfocused, and shattered. And if the forest is being assaulted and hurt, I get hurt. I get sick if the forest gets sick, because my body and my speech are also made of the forest.
4. Discussion
4.1. Methylmercury Exposure and Mental Health Impacts
4.2. Methylmercury Exposure and Mental Health Indicators
4.3. Limitations
4.4. Impacts of Goldmining on Munduruku People Good-Living (Xipan Jewewekukap)
Pajés [traditional healers] learned what they know from snakes. They learned that human diseases come from antiquity, from the first times of the world—times when abysses were open. Many other diseases remained at the bottom of the earth when these abysses closed. Nowadays, since pariwat (non-Amerindian people) are rummaging deep in the earth, these diseases are rising. If pariwat continue to rummage where they shouldn’t, all of us, Munduruku and pariwat, will have serious problems.
I am a pajé, but I don’t know how to cure problems caused by mercury contamination. This is new to me. Nevertheless, I know how to take care of illnesses that are caused by the fact that pariwat are messing with places they shouldn’t. They are messing with other beings’ houses and those beings are getting very angry. That is why we need to combine Munduruku medicines with pariwat medicines. And that is why we have to combine efforts to stop pariwat from messing with the other being’s houses.
Everything in this world has a mother: the fish, the water, the stone... When we mess with the mothers’ offspring, they get angry and attack us, making us ill. Making these mothers mad is very dangerous for the Munduruku. Unfortunately, the destruction of the forest brings even more serious problems than those illnesses. I have learned from the elders that, since the beginning of the world, there is an enormous tree that supports the sky, preventing it from falling to the earth. The miners and loggers are cutting the nails that are at the roots of this tree. If that tree falls, the sky will fall and this world we live in will end.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ramos, A.R.F. Entre a Cruz e a Riscadeira: Catequese e Empresa Extrativista Entre os Munduruku (1910 a 1957). Master’s Thesis, Universidade Federal de Goiás (UFG), Goiânia, Brasil, 2000. [Google Scholar]
- Ramos, A.R.F. Munduruku. In Enciclopédia dos Povos Indígenas No Brasil; Instituto Socioambiental: São Paulo, Brazil, 2003; Available online: http://www.socioambiental.org/pib/epi/munduruku/munduruku.shtm (accessed on 10 October 2020).
- Quijano, A. Colonialidad del poder, eurocentrismo y America Latina. In A Colonialidade do Saber: Eurocentrismo e Ciências Sociais. Perspectivas Latino-Americanas, 1st ed.; Lander, E., Ed.; CLACSO: Buenos Aires, Argentina, 2000; pp. 117–142. [Google Scholar]
- dos Santos, O.A.; Massola, G.M.; da Silva, G.L.G.; Svartman, B.P. Racismo ambiental e lutas por reconhecimento dos povos de floresta da Amazônia. Glob. J. Community Psychol. Pract. 2016, 7, 1–20. [Google Scholar]
- Brabo, E.D.S.; Santos, E.D.O.; Jesus, I.M.D.; Mascarenhas, A.F.; Faial, K.F. Mercury levels in fish consumed by the sai cinza indigenous community, Munduruku reservation, Jacareacanga county, state of Para, Brazil. Cad. Saude Publica 1999, 15, 325–332. [Google Scholar] [CrossRef]
- Barbosa, A.C.; Dórea, J.G. Indices of mercury contamination during breast feeding in the Amazon Basin. Environ. Toxicol. Pharmacol. 1998, 6, 71–79. [Google Scholar] [CrossRef]
- Roulet, M.; Lucotte, M.; Canuel, R.; Rheault, I.; Tran, S.; De Freitos Gog, Y.G.; Farella, N.; do Vale, R.S.; Passos, C.J.S.; da Silva, E.D.J.; et al. Distribution and partition of total mercury in waters of the Tapajos River Basin, Brazilian Amazon. Sci. Total Environ. 1998, 213, 203–211. [Google Scholar] [CrossRef]
- Lacerda, L.; Pfeiffer, W. Mercury from gold mining in the Amazon environment-an overview. Química Nova 1992, 15, 155–160. [Google Scholar]
- Akagi, H.; Malm, O.; Kinjo, Y.; Harada, M.; Branches, F.J.P.; Pfeiffer, W.C.; Kato, H. Methylmercury pollution in the Amazon, Brazil. Sci. Total Environ. 1995, 175, 85–95. [Google Scholar] [CrossRef]
- RAISG. Mapa Inédito Indica Epidemia de Garimpo Ilegal na Panamazônia; Rede Amazônica de Informação Socioambiental Georreferenciada: Manaus, Brasil, 2018; Available online: https://www.amazoniasocioambiental.org/pt-br/radar/mapa-inedito-indica-epidemia-de-garimpo-ilegal-na-panamazonia/ (accessed on 11 October 2020).
- Alvarez-Berríos, N.L.; Aide, T.M. Global demand for gold is another threat for tropical forests. Environ. Res. Lett. 2015, 10, 014006. [Google Scholar] [CrossRef]
- Rahm, M.; Jullian, B.; Lauger, A.; de Carvalho, R.; Vale, L.; Totaram, J.; Cort, K.A.; Djojodikromo, M.; Hardjoprajitno, M.; Neri, S.; et al. Monitoring the Impact of Gold Mining on the Forest Cover and Freshwater in the Guiana Shield. Reference Year 2014; WWF-France: French Guiana, France, 2015; 60p. [Google Scholar]
- Legg, E.D.; Ouboter, P.E.; Wright, M.A.P. Small-Scale Gold Mining Related to Mercury Contamination in the Guianas: A Review; WWF Guianas: Paramaribo, Suriname, 2015. [Google Scholar]
- Brabo, E.; Santos, O.E.C.; Jesus, I.M.; Mascarenhas, A.F.S.; Faial, K.F. Mercury contamination of fish and exposures of an indigenous community in Para state, Brazil. Environ. Res. 2000, 84, 197–203. [Google Scholar] [CrossRef]
- Santos, E.C.; de Jesus, I.M.; Câmara, V.M.; Brabo, E.; Loureiro, E.C.; Mascarenhas, A.; Weirich, J.; Luiz, R.R.; Cleary, D. Mercury exposure in Munduruku Indians from the community of Sai Cinza, State of Pará, Brazil. Environ. Res. 2002, 90, 98–103. [Google Scholar] [CrossRef]
- FAO; WHO. Expert Committee on Food Additives. Sixty-First Meeting. Summary and Conclusions; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- FAO; WHO. Evaluation of Certain Food Additives and Contaminants: Sixty-first Report of the Joint FAO/WHO Expert Committee on Food Additives. In Proceedings of the Joint FAO/WHO Expert Committee on Food Additives (JECFA), Rome, Italy, 10–19 June 2003. [Google Scholar]
- Zahir, F.; Rizwi, S.J.; Haq, S.K.; Khan, R.H. Low dose mercury toxicity and human health. Environ. Toxicol. Pharmacol. 2005, 20, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Ekino, S.; Susa, M.; Ninomiya, T.; Imamura, K.; Kitamura, T. Minamata disease revisited: An update on the acute and chronic manifestations of methyl mercury poisoning. J. Neurol. Sci. 2007, 262, 131–144. [Google Scholar] [CrossRef] [PubMed]
- Chuu, Y.Y.; Liu, S.H.; Lin-Shiau, S. Differential neurotoxic effects of methylmercury and mercuric sulfide in rats. Toxicol. Lett. 2007, 169, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.W.; Pai, M.C.; Chen, H.L.; Guo, H.R.; Su, H.J.; Lee, C.C. Cognitive function and blood methylmercury in adults living near a deserted chloralkali factory. Environ. Res. 2008, 108, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Dolbec, J.; Mergler, D.; Passos, S.C.J.; De Morais, S.S.; Lebel, J. Methylmercury exposure affects motor performance of a riverine population of the Tapajós river, Brazilian Amazon. Int. Arch. Occup. Environ. Health 2000, 73, 195–203. [Google Scholar] [CrossRef]
- Santos-Lima, C.D.; Mourão, D.S.; Carvalho, C.F.; Souza-Marques, B.; Vega, C.M.; Gonçalves, R.A.; Argollo, N.; Mene-zes-Filho, J.A.; Abreu, N.; Hacon, S.S. Neuropsychological effects of mercury exposure in children and adolescents of the Amazon region, Brazil. Neurotoxicology 2020, 79, 48–57. [Google Scholar] [CrossRef]
- Junior, J.M.F.C.; Lima, A.A.S.; Junior, D.R.; Khoury, E.D.T.; Souza, G.S.; Silveira, L.C.L.; Pinheiro, M.C.N. Manifestações emocionais e motoras de ribeirinhos expostos ao mercúrio na Amazônia. Rev. Bras. Epidemiol. 2017, 20, 212–224. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Belaunde, L.E. Viviendo Bien: Género y Fertilidad Entre los Airo-Pai de la Amazonía Peruana; CAAAP: Lima, Peru, 2001. [Google Scholar]
- McCallum, C. Intimidade com estranhos: Uma perspectiva Kaxinawá sobre confiança e a construção de pessoas na Amazônia. Mana 2013, 19, 123–155. [Google Scholar] [CrossRef][Green Version]
- Costa, A. O Bem Viver–Uma Oportunidade Para Imaginar Outros Mundos; Autonomia Literária e Editora Elefante: São Paulo, Brazil, 2015. [Google Scholar]
- Baniwa, A.F. Bem Viver e Viver Bem: Segundo o Povo Baniwa no Noroeste Amazônico Brasileiro; UFPR: Curitiba, Brazil, 2019. [Google Scholar]
- Munduruku, M.L. Vamos continuar guerreando. Interview given to Patricia Bonilha. Rev. Porantim 2016, 390, 6–7. [Google Scholar]
- Basta, P.C.; Viana, P.V.S.; Vasconcellos, A.C.S.; Périssé, A.R.S.; Hofer, C.B.; Paiva, N.S.; Kempton, J.W.; Ciampi de Andrade, D.; Oliveira, R.A.A.; Achatz, R.W.; et al. Mercury exposure in Munduruku indigenous communities from Brazilian Amazon: Methodological background and an overview of the principal results. Int. J. Environ. Res. Public Health 2021, 18. in press. [Google Scholar]
- Sheikh, J.I.; Yesavage, J.A.; Brooks, J.O.; Friedman, L.; Gratzinger, P.; Hill, R.D.; Zadeik, A.; Crook, T. Proposed factor structure of the Geriatric Depression Scale. Int. Psychogeriatr. 1991, 3, 23–28. [Google Scholar] [CrossRef]
- Sheikh, J.I.; Yesavage, J.A.; Scale, G.D. Recent evidence and development of a shorter version. Clin. Gerontol. 1986, 5, 165–172. [Google Scholar]
- Guerin, J.M.; Copersino, M.L.; Schretlen, D.J. Clinical utility of the 15-item geriatric depression scale (GDS-15) for use with young and middle-aged adults. J. Affect Disord. 2018, 241, 59–62. [Google Scholar] [CrossRef]
- Abas, M.; Phillips, C.; Carter, J.; Walter, J.; Banerjee, S.; Levy, R. Culturally sensitive validation of screening questionnaires for depression in older African–Caribbean people living in south London. Br. J. Psychiatry 1998, 173, 249–254. [Google Scholar] [CrossRef]
- Latour, B. Nous N’avons Jamais été Modernes: Essai D’anthropologie Symétrique; La Découverte: Paris, France, 1991. [Google Scholar]
- de Castro, V.E. O nativo relativo. Rev. Mana 2002, 8. [Google Scholar] [CrossRef]
- Silva, D.F. Toward a Global Idea of Race; University of Minnesota Press: Minneapolis, MN, USA, 2007. [Google Scholar]
- de Castro, V.E. Perspectival Anthropology and the Method of Controlled Equivocation. Tipití J. Soc. Anthropol. Lowl. South Am. 2004, 2. Available online: https://digitalcommons.trinity.edu/tipiti/vol2/iss1/1 (accessed on 30 June 2021).
- World Health Organization (WHO). Guidance for Identifying Populations at Risk from Mercury Exposure; WHO: Geneva, Switerzeland, 2008; Available online: https://wedocs.unep.org/bitstream/handle/20.500.11822/11786/IdentifyingPopnatRiskExposuretoMercury_2008Web.pdf?sequence=1&isAllowed=y (accessed on 30 June 2021).
- Marinho, J.S.; Lima, M.O.; de Oliveira Santos, E.C.; de Jesus, I.M.; da Conceição, N.; Pinheiro, M.; Alves, C.N.; Muller, R.C. Mercury speciation in hair of children in three communities of the Amazon, Brazil. Biomed. Res. Int. 2014, 945963. [Google Scholar] [CrossRef] [PubMed]
- de Castro, S.S.N.; de Oliveira Lima, M. Hair as a biomarker of long term mercury exposure in Brazilian Amazon: A systematic review. Int. J. Environ. Res. Public Health 2018, 15, 500. [Google Scholar] [CrossRef] [PubMed]
- Vega, C.M.; Orellana, J.D.; Oliveira, M.W.; Hacon, S.S.; Basta, P.C. Human mercury exposure in Yanomami indigenous villages from the Brazilian Amazon. Int. J. Environ. Res. Public Health 2018, 15, 1051. [Google Scholar] [CrossRef]
- Lebel, J.; Mergler, D.; Lucotte, M.; Amorim, M.; Dolbec, J.; Miranda, D.; Pichet, P. Evidence of early nervous system dysfunction in Amazonian populations exposed to low-levels of methylmercury. Neurotoxicology 1996, 17, 157–167. [Google Scholar]
- Lebel, J.; Mergler, D.; Branches, F.; Lucotte, M.; Amorim, M.; Larribe, F.; Dolbec, J. Neurotoxic effects of low-level methylmercury contamination in the Amazonian Basin. Environ. Res. 1998, 79, 20–32. [Google Scholar] [CrossRef]
- Harada, M.; Nakanishi, J.; Yasoda, E.; da Conceicâo, M.N.P.; Oikawa, T.; de Assis Guimarâes, G.; Ohno, H. Mercury pollution in the Tapajos river basin, Amazon: Mercury level of head hair and health effects. Environ. Int. 2001, 27, 285–290. [Google Scholar] [CrossRef]
- Lacerda, E.M.D.C.B.; Souza, G.D.S.; Cortes, M.I.T.; Rodrigues, A.R.; Pinheiro, M.C.N.; Silveira, L.C.D.L.; Ventura, D.F. Comparison of visual functions of two Amazonian populations: Possible consequences of different mercury exposure. Front. Neurosci. 2020, 13, 1428. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.A.A.; Pinto, B.D.; Rebouças, B.H.; Ciami de Andrade, D.; Vasconcellos, A.C.S.; Basta, P.C. Neurological impacts of chronic methylmercury exposure in Munduruku indigenous adults: Somatosensory, motor and cognitive abnormalities. Int. J. Environ. Res. Public Health. (under review).
- Benefice, E.; Luna-Monrroy, S.; Lopez-Rodriguez, R. Fishing activity, health characteristics and mercury exposure of Amerindian women living alongside the Beni River (Amazonian Bolivia). Int. J. Hyg. Environ. Health 2010, 213, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Peplow, D.; Augustine, S. Neurological abnormalities in a mercury exposed population among indigenous Wayana in Southeast Suriname. Environ. Sci. Process. Impacts 2014, 16, 2415–2422. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gochfeld, M. Cases of mercury exposure, bioavailability and absorption. Ecotoxicol. Environ. Saf. 2003, 56, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Bernhoft, R.A. Mercury toxicity and treatment: A review of the literature. J. Environ. Public Health 2012, 2012, 460508. [Google Scholar] [CrossRef]
- Park, J.D.; Zheng, W. Human exposure and health effects of inorganic and elemental mercury. J. Prev. Med. Public Health 2012, 45, 344–352. [Google Scholar] [CrossRef]
- O’Carroll, R.; Masterton, G.; Dougall, N.; Ebmeier, K.; Goodwin, G. The neuropsychiatric sequelae of mercury poisoning: The mad hatter’s disease revisited. Br. J. Psychiatry 1995, 167, 95–98. [Google Scholar] [CrossRef]
- Wojcik, D.P.; Godfrey, M.E.; Christie, D.; Haley, B.E. Mercury toxicity presenting as chronic fatigue, memory impairment and depression: Diagnosis, treatment, susceptibility, and outcomes in a New Zealand general practice setting (1994–2006). Neuroendocrinol. Endocrinol. Lett. 2006, 27, 415–423. [Google Scholar]
- Uzzell, B.P.; Oler, J. Chronic low-level mercury exposure and neuropsychological functioning. J. Clin. Experim. Neuropsychol. 1986, 8, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Siblerud, R.L. The relationship between mercury from dental amalgam and mental health. Am. J. Psychother. 1989, 43, 575–587. [Google Scholar] [CrossRef]
- World Health Organization. Environmental Health Criteria 1. Mercury; WHO: Geneva, Switerzeland, 1976. [Google Scholar]
- Bakir, F.; Damluji, S.F.; Amin-Zaki, L.; Murtadha, M.; Khalidi, A.; Al-Rawi, N.Y.; Tikriti, S.; Dahahir, H.I.; Clarkson, T.W.; Smith, J.C.; et al. Methylmercury poisoning in Iraq. Science 1973, 181, 230–241. [Google Scholar] [CrossRef]
- Maghazaji, H.I. Psychiatric aspects of methyl mercury poisoning. J. Neurol. Neurosurg. Psychiatry 1974, 37, 954–958. [Google Scholar] [CrossRef] [PubMed]
- Grant, C.A. Pathology of experimental methylmercury intoxication: Some problems of exposure and response. In Mercury, Mercurials and Mercaptans; Miller, M.W., Clarkson, T.W., Eds.; Charles C Thomas Publisher, Ltd.: Springfield, IL, USA, 1973; Volume 111, pp. 294–310. [Google Scholar]
- Batista, Q.M.; Zanello, V. Saúde mental em contextos indígenas: Escassez de pesquisas brasileiras, invisibilidade das diferenças. Estud. Psicol. 2016, 21, 403–414. [Google Scholar] [CrossRef]
- Pedraza, O.; Dotson, V.M.; Willis, F.B.; Graff-Radford, N.R.; Lucas, J.A. Internal consistency and test-retest stability of the geriatric depression scale-short form in African American older adults. J. Psychopathol. Behav. Assess. 2009, 31, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Mui, A.C.; Kang, S.-Y.; Chen, L.M.; Domanski, M.D. Reliability of the geriatric depression scale for use among elderly Asian immigrants in the USA. Int. Psychogeriatr. 2003, 15, 253–271. [Google Scholar] [CrossRef]
- Almeida, O.P.; Almeida, S.A. Confiabilidade da versão brasileira da escala de depressão em geriatria (GDS) versão reduzida. Arq. Neuro-Psiquiatr. 1999, 57, 421–426. [Google Scholar] [CrossRef]
- Jang, Y.; Kim, J.; Chiriboga, D. Acculturation and manifestation of depressive symptoms among Korean-American older adults. Aging Ment. Health 2005, 9, 500–507. [Google Scholar] [CrossRef]
- Flacker, J.M.; Spiro, L. Does question comprehension limit the utility of the Geriatric Depression Scale in older African Americans? J. Am. Geriatr. Soc. 2003, 51, 1511–1512. [Google Scholar] [CrossRef]
- Kirmayer, L.J. Cultural variations in the clinical presentation of depression and anxiety: Implications for diagnosis and treatment. J. Clin. Psychiatry 2001, 62, 22–30. [Google Scholar]
- Jang, Y.; Small, B.J.; Haley, W.E. Cross-cultural comparability of the Geriatric Depression Scale: Comparison between older Koreans and older Americans. Aging Ment. Health 2001, 5, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Hallal, P.C.; Dumith, S.C.; Bertoldi, A.D.; Scalco, D.L.; Menezes, A.M.; Araújo, C.L. Well-being in adolescents: The 11-year follow-up of the 1993 Pelotas (Brazil) birth cohort study. Cad. Saude Publica 2010, 26, 1887–1894. [Google Scholar] [CrossRef] [PubMed]
- Stengers, I. Cosmopolitics; University of Minnesota Press: Minneapolis, MN, USA, 2010; Volume I. [Google Scholar]
- Tosold, L. Por uma vida sem barragens: Corpos, território e o papel da autodeterminação na desnaturalização da violência. Rev. Antropol. 2020, 63, e178182. [Google Scholar] [CrossRef]
- Weir, J.A.Q. Del ‘Giro Ontológico’ al Tiempo de Vuelta del Nosotrxs. Amaz. Latit. 2021, 26. Available online: https://amazonialatitude.com/2021/04/08/del-giro-ontologico-al-tiempo-de-vuelta-del-nosotrxs/ (accessed on 30 June 2021).
- Krenak, A. Ideias Para Adiar o Fim do Mundo; Companhia das Letras: São Paulo, Brazil, 2019. [Google Scholar]
- Kopenawa, D.; Albert, B. La Chute du Ciel. Paroles d’un Chaman Yanomami; Terre Humain, Plon: Paris, France, 2014. [Google Scholar]
| GDS-SF | |||||||
|---|---|---|---|---|---|---|---|
| <4 | ≥4 | Total | |||||
| Sociodemographic Features | |||||||
| Sex | n | % | n | % | n | % | p-value |
| Male | 39 | 69.6 | 17 | 30.4 | 56 | 51.4 | 0.416 |
| Female | 33 | 62.3 | 20 | 37.7 | 53 | 48.6 | |
| Total | 72 | 37 | 109 | ||||
| Age range | |||||||
| ≥30 years | 23 | 67.6 | 11 | 32.4 | 34 | 31.2 | 0.376 |
| 20 to 29 years | 22 | 57.9 | 16 | 42.1 | 38 | 34.9 | |
| 12 to 19 years | 27 | 73.0 | 10 | 27.0 | 37 | 33.9 | |
| Total | 72 | 37 | 109 | ||||
| Schooling | |||||||
| >9 years | 17 | 68.0 | 8 | 32.0 | 25 | 22.9 | 0.339 |
| 5 to 9 years | 47 | 69.1 | 21 | 30.9 | 68 | 62.4 | |
| 0 to 4 years | 8 | 50.0 | 8 | 50.0 | 16 | 14.7 | |
| Total | 72 | 37 | 109 | ||||
| Marital Status | |||||||
| Married | 49 | 64.5 | 27 | 35.5 | 76 | 69.7 | 0.597 |
| Single/Widow | 23 | 69.7 | 10 | 30.3 | 33 | 30.3 | |
| Total | 72 | 37 | 109 | ||||
| Villages | |||||||
| Sawré Muybu | 24 | 52.2 | 22 | 47.8 | 46 | 42.2 | 0.002 |
| Poxo Muybu | 34 | 87.2 | 5 | 12.8 | 39 | 35.8 | |
| Sawré Aboy | 14 | 58.3 | 10 | 41.7 | 24 | 22.0 | |
| Total | 72 | 37 | 109 | ||||
| Regular Income | |||||||
| Yes | 27 | 67.5 | 13 | 32.5 | 40 | 36.7 | 0.808 |
| No | 45 | 65.2 | 24 | 34.8 | 69 | 63.3 | |
| Total | 72 | 37 | 109 | ||||
| Clinical Features | |||||||
| Nervousness | n | % | n | % | n | % | p-value |
| No | 61 | 74.4 | 21 | 25.6 | 82 | 75.2 | 0.001 |
| Yes | 11 | 40.7 | 16 | 59.3 | 27 | 24.8 | |
| Total | 72 | 37 | 109 | ||||
| School failure | |||||||
| No | 41 | 74.5 | 14 | 25.5 | 55 | 51.9 | 0.055 |
| Yes | 29 | 56.9 | 22 | 43.1 | 51 | 48.1 | |
| Total | 70 | 36 | 106 | ||||
| Irritability | |||||||
| No | 69 | 71.9 | 27 | 28.1 | 96 | 88.1 | 0.001 |
| Yes | 3 | 23.1 | 10 | 76.9 | 13 | 11.9 | |
| Total | 72 | 37 | 109 | ||||
| Physical Activity restriction | |||||||
| No | 68 | 68.0 | 32 | 32.0 | 100 | 91.7 | 0.153 |
| Yes | 4 | 44.4 | 5 | 55.6 | 9 | 8.3 | |
| Total | 72 | 37 | 109 | ||||
| Previous Malaria | |||||||
| No | 38 | 73.1 | 14 | 26.9 | 52 | 47.7 | 0.139 |
| Yes | 34 | 59.6 | 23 | 40.4 | 57 | 52.3 | |
| Total | 72 | 37 | 109 | ||||
| Previous hospitalization | |||||||
| No | 44 | 68.8 | 20 | 31.3 | 64 | 58.7 | 0.479 |
| Yes | 28 | 62.2 | 17 | 37.8 | 45 | 41.3 | |
| Total | 72 | 37 | 109 | ||||
| GDS-SF ≥ 4 | ||
|---|---|---|
| Variables | PR Crude (CI 90%) | p-Value |
| Hg Level | ||
| Hg < 10 µg/g | 1.0 | |
| Hg ≥ 10 µg/g | 1.6 (1.0–2.5) | 0.072 |
| Nervousness | ||
| No | 1.0 | |
| Yes | 2.3 (1.5–3.5) | 0.001 |
| Irritability | ||
| No | 1.0 | |
| Yes | 2.7 (1.9–3.9) | 0.001 |
| Regular Income | ||
| Yes | 1.0 | |
| No | 1.1 (0.7–1.7) | 0.809 |
| Villages | ||
| Sawré Muybu | 1.0 | |
| Poxo Muybu | 0.3 (0.1–0.6) | 0.003 |
| Sawré Aboy | 0.9 (0.5–1.4) | 0.630 |
| Age range | ||
| ≥30 years | 1.0 | |
| 20 to 29 years | 1.3 (0.8–2.2) | 0.399 |
| 12 to 19 years | 0.8 (0.5–1.5) | 0.624 |
| Gender | ||
| Male | 1.0 | |
| Female | 1.2 (0.8–1.9) | 0.418 |
| Schooling | ||
| >9 years | 1.0 | |
| 5 to 9 years | 1.0 (0.6–1.7) | 0.918 |
| 0 to 4 years | 1.6 (0.8–2.9) | 0.245 |
| School Failure | ||
| No | 1.0 | |
| Yes | 1.7 (1.1–2.7) | 0.061 |
| Marital Status | ||
| Married | 1.0 | |
| Single/Widow | 0.9 (0.5–1.4) | 0.603 |
| GDS-SF ≥ 4 | ||
|---|---|---|
| Variables | PR-Adjusted (CI 95%) | p-Value |
| Hg Level | ||
| Hg < 10 µg/g | 1.0 | |
| Hg ≥ 10 µg/g | 1.8 (1.1–3.0) | 0.024 |
| Nervousness | ||
| No | 1.0 | |
| Yes | 2.1 (1.3–3.3) | 0.003 |
| Irritability | ||
| No | 1.0 | |
| Yes | 3.0 (1.9–4.9) | 0.001 |
| Regular Income | ||
| Yes | 1.0 | |
| No | 1.1 (0.6–1.9) | 0.766 |
| Age range | ||
| ≥30 years | 1.0 | |
| 20 to 29 years | 1.4 (0.8–2.5) | 0.219 |
| 12 to 19 years | 0.7 (0.4–1.5) | 0.400 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Achatz, R.W.; de Vasconcellos, A.C.S.; Pereira, L.; Viana, P.V.d.S.; Basta, P.C. Impacts of the Goldmining and Chronic Methylmercury Exposure on the Good-Living and Mental Health of Munduruku Native Communities in the Amazon Basin. Int. J. Environ. Res. Public Health 2021, 18, 8994. https://doi.org/10.3390/ijerph18178994
Achatz RW, de Vasconcellos ACS, Pereira L, Viana PVdS, Basta PC. Impacts of the Goldmining and Chronic Methylmercury Exposure on the Good-Living and Mental Health of Munduruku Native Communities in the Amazon Basin. International Journal of Environmental Research and Public Health. 2021; 18(17):8994. https://doi.org/10.3390/ijerph18178994
Chicago/Turabian StyleAchatz, Rafaela Waddington, Ana Claudia Santiago de Vasconcellos, Lucia Pereira, Paulo Victor de Sousa Viana, and Paulo Cesar Basta. 2021. "Impacts of the Goldmining and Chronic Methylmercury Exposure on the Good-Living and Mental Health of Munduruku Native Communities in the Amazon Basin" International Journal of Environmental Research and Public Health 18, no. 17: 8994. https://doi.org/10.3390/ijerph18178994
APA StyleAchatz, R. W., de Vasconcellos, A. C. S., Pereira, L., Viana, P. V. d. S., & Basta, P. C. (2021). Impacts of the Goldmining and Chronic Methylmercury Exposure on the Good-Living and Mental Health of Munduruku Native Communities in the Amazon Basin. International Journal of Environmental Research and Public Health, 18(17), 8994. https://doi.org/10.3390/ijerph18178994








