Assessment of Severe COVID-19 Outcomes Using Measures of Smoking Status and Smoking Intensity
Abstract
:1. Introduction
2. Methods
Participants and Procedures
3. Measures
3.1. Tobacco Use
3.2. Severe COVID-19 Outcomes
3.3. Covariates
3.4. Statistical Analysis
4. Results
4.1. Description of Study Population
4.2. Characteristics of Study Participants by Smoking Status
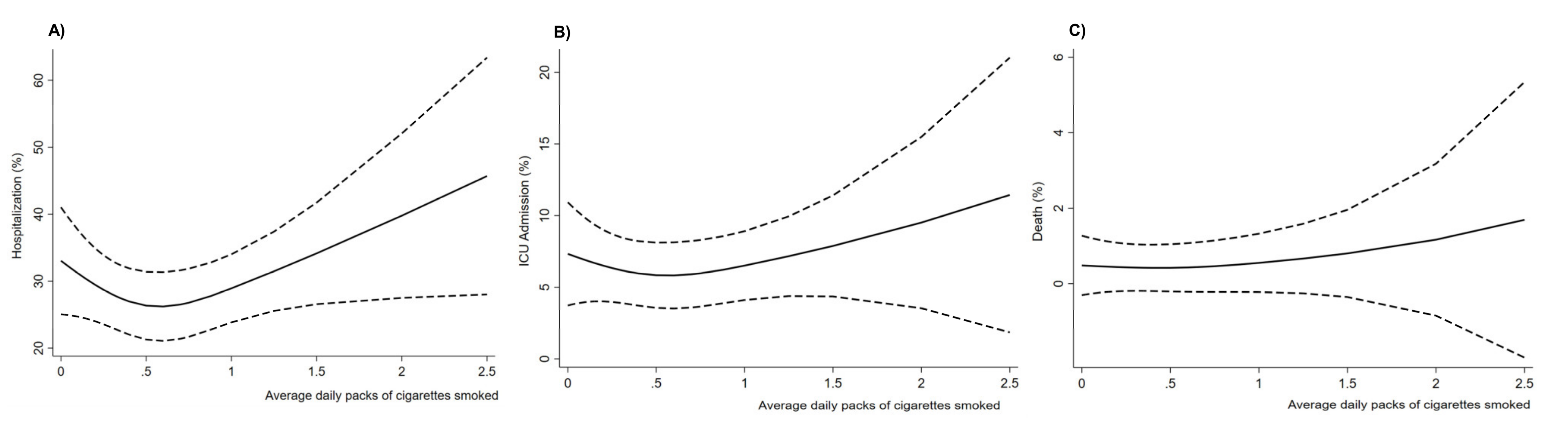
4.3. Smoking Status and Severe COVID-19 Outcomes
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- WHO Statement: Tobacco Use and COVID-19. Available online: https://www.who.int/news/item/11-05-2020-who-statement-tobacco-use-and-covid-19 (accessed on 22 April 2021).
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2014.
- Lawrence, H.; Hunter, A.; Murray, R.; Lim, W.S.; McKeever, T. Cigarette smoking and the occurrence of influenza-Systematic review. J. Infect. 2019, 79, 401–406. [Google Scholar] [CrossRef]
- Baskaran, V.; Murray, R.L.; Hunter, A.; Lim, W.S.; McKeever, T.M. Effect of tobacco smoking on the risk of developing community acquired pneumonia: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0220204. [Google Scholar] [CrossRef] [Green Version]
- Strzelak, A.; Ratajczak, A.; Adamiec, A.; Feleszko, W. Tobacco Smoke Induces and Alters Immune Responses in the Lung Triggering Inflammation, Allergy, Asthma and Other Lung Diseases: A Mechanistic Review. Int. J. Environ. Res. Public Health 2018, 15, 1033. [Google Scholar] [CrossRef] [Green Version]
- Umnuaypornlert, A.; Kanchanasurakit, S.; Lucero-Prisno, D.E.I.; Saokaew, S. Smoking and risk of negative outcomes among COVID-19 patients: A systematic review and meta-analysis. Tob. Induc. Dis. 2021, 19, 9. [Google Scholar] [CrossRef]
- Brake, S.J.; Barnsley, K.; Lu, W.; McAlinden, K.D.; Eapen, M.S.; Sohal, S.S. Smoking Upregulates Angiotensin-Converting Enzyme-2 Receptor: A Potential Adhesion Site for Novel Coronavirus SARS-CoV-2 (Covid-19). J. Clin. Med. 2020, 9, 841. [Google Scholar] [CrossRef] [Green Version]
- COVID-19: People with Certain Medical Conditions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html#smoking (accessed on 22 April 2021).
- Case, J.B.; Winkler, E.S.; Errico, J.M.; Diamond, M.S. On the road to ending the COVID-19 pandemic: Are we there yet? Virology 2021, 557, 70–85. [Google Scholar] [CrossRef]
- Phillips, N. The coronavirus is here to stay-here’s what that means. Nature 2021, 590, 382–384. [Google Scholar] [CrossRef]
- Grundy, E.J.; Suddek, T.; Filippidis, F.T.; Majeed, A.; Coronini-Cronberg, S. Smoking, SARS-CoV-2 and COVID-19: A review of reviews considering implications for public health policy and practice. Tob. Induc. Dis. 2020, 18, 58. [Google Scholar] [CrossRef]
- Patanavanich, R.; Glantz, S.A. Smoking Is Associated With COVID-19 Progression: A Meta-analysis. Nicotine Tob. Res. 2020, 22, 1653–1656. [Google Scholar] [CrossRef]
- Lowe, K.E.; Zein, J.; Hatipoglu, U.; Attaway, A. Association of Smoking and Cumulative Pack-Year Exposure With COVID-19 Outcomes in the Cleveland Clinic COVID-19 Registry. JAMA Intern. Med. 2021, 181, 709–711. [Google Scholar] [CrossRef]
- Mendy, A.; Apewokin, S.; Wells, A.A.; Morrow, A.L. Factors Associated with Hospitalization and Disease Severity in a Racially and Ethnically Diverse Population of COVID-19 Patients. medRxiv 2020. [Google Scholar] [CrossRef]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems, 5th ed.; WHO Press: Geneva, Switzerland, 2016; Volume 3. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 17; StataCorp LLC.: College Station, TX, USA, 2021. [Google Scholar]
- SAS Institute Inc. SAS Software Version 9.4; SAS Institute Inc.: Cary, NC, USA, 2013. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Epidemiology 2007, 18, 800–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haddad, C.; Bou Malhab, S.; Sacre, H.; Salameh, P. Smoking and COVID-19: A Scoping Review. Tob. Use Insights 2021, 14, 1179173X21994612. [Google Scholar] [CrossRef]
- Caruso, M.; Distefano, A.; Emma, R.; Di Rosa, M.; Carota, G.; Rust, S.; Polosa, R.; Zuccarello, P.; Ferrante, M.; Raciti, G.; et al. Role of Cigarette Smoke on Angiotensin-Converting Enzyme-2 Protein Membrane Expression in Bronchial Epithelial Cells Using an Air-Liquid Interface Model. Front. Pharm. 2021, 12, 652102. [Google Scholar] [CrossRef] [PubMed]
- Walls, A.C.; Park, Y.J.; Tortorici, M.A.; Wall, A.; McGuire, A.T.; Veesler, D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 2020, 181, 281–292.e6. [Google Scholar] [CrossRef]
- Duncan, M.S.; Freiberg, M.S.; Greevy, R.A., Jr.; Kundu, S.; Vasan, R.S.; Tindle, H.A. Association of Smoking Cessation With Subsequent Risk of Cardiovascular Disease. JAMA 2019, 322, 642–650. [Google Scholar] [CrossRef] [Green Version]
- Park, S.; Han, K.; Lee, S.; Kim, Y.; Lee, Y.; Kang, M.W.; Park, S.; Kim, Y.C.; Han, S.S.; Lee, H.; et al. Smoking, development of or recovery from metabolic syndrome, and major adverse cardiovascular events: A nationwide population-based cohort study including 6 million people. PLoS ONE 2021, 16, e0241623. [Google Scholar]
- Tindle, H.A.; Stevenson Duncan, M.; Greevy, R.A.; Vasan, R.S.; Kundu, S.; Massion, P.P.; Freiberg, M.S. Lifetime Smoking History and Risk of Lung Cancer: Results From the Framingham Heart Study. J. Natl. Cancer Inst. 2018, 110, 1201–1207. [Google Scholar] [CrossRef]
- Gulsen, A.; Yigitbas, B.A.; Uslu, B.; Dromann, D.; Kilinc, O. The Effect of Smoking on COVID-19 Symptom Severity: Systematic Review and Meta-Analysis. Pulm. Med. 2020, 2020, 7590207. [Google Scholar] [CrossRef]
- Polubriaginof, F.; Salmasian, H.; Albert, D.A.; Vawdrey, D.K. Challenges with Collecting Smoking Status in Electronic Health Records. AMIA Annu. Symp. Proc. 2017, 2017, 1392–1400. [Google Scholar] [PubMed]
- Mahabee-Gittens, E.M.; Merianos, A.L.; Gordon, J.S.; Stone, L.; Semenova, O.; Matt, G.E. Electronic Health Record Classification of Tobacco Smoke Exposure and Cotinine Levels in Hospitalized Pediatric Patients. Hosp. Pediatrics 2019, 9, 659–664. [Google Scholar] [CrossRef]
| Characteristics | N (%) |
|---|---|
| Older adults (65 + years old) | 1119 (24.7) |
| Female sex | 2911 (63.1) |
| Race/ethnicity | |
| Non-Hispanic White | 2557 (55.5) |
| Non-Hispanic Black | 1526 (33.1) |
| Hispanic | 269 (5.8) |
| Other | 259 (5.6) |
| Smoking | |
| Never | 2815 (61.0) |
| Current | 841 (18.2) |
| Former | 955 (20.7) |
| Comorbidities | |
| Obesity | 1010 (21.9) |
| Type 2 diabetes | 942 (20.4) |
| Asthma | 666 (14.4) |
| COPD | 437 (9.5) |
| Hypertension | 1913 (41.5) |
| CKD | 492 (10.7) |
| CVD | 1724 (37.4) |
| Cancer history | 1187 (25.7) |
| COVID-19 outcomes | |
| Hospitalization | 1333 (28.9) |
| ICU admission | 450 (9.8) |
| Death | 66 (1.4) |
| Never | Ever Smokers | p-Value † | Current Smokers | p-Value ‡ | Former Smokers | p-Value ⸸ | |
|---|---|---|---|---|---|---|---|
| Older adults (65 or older) | 582 (20.7) | 537 (29.9) | 0.001 | 142 (16.9) | 0.02 | 395 (41.4) | <0.001 |
| Female sex | 1871 (66.5) | 1040 (57.9) | <0.001 | 480 (57.1) | <0.001 | 560 (58.6) | <0.001 |
| Race/ethnicity | <0.001 | <0.001 | <0.001 | ||||
| Non-Hispanic White | 1558 (55.3) | 999 (55.6) | 442 (52.6) | 557 (58.3) | |||
| Non-Hispanic Black | 830 (29.5) | 696 (38.8) | 349 (41.5) | 347 (36.3) | |||
| Hispanic | 228 (8.1) | 41 (2.3) | 20 (2.4) | 21 (2.2) | |||
| Other | 199 (7.1) | 60 (3.3) | 30 (3.6) | 30 (3.1) | |||
| Comorbidities | |||||||
| Obesity | 552 (19.6) | 458 (25.5) | <0.001 | 156 (18.5) | 0.49 | 302 (31.6) | <0.001 |
| Type 2 diabetes | 452 (16.1) | 490 (27.7) | <0.001 | 174 (20.7) | 0.002 | 316 (33.1) | <0.001 |
| Asthma | 346 (12.3) | 320 (17.8) | <0.001 | 137 (16.3) | 0.003 | 183 (19.2) | <0.001 |
| COPD | 81 (2.9) | 356 (19.8) | <0.001 | 155(18.4) | <0.001 | 201 (21.0) | <0.001 |
| Hypertension | 910 (32.3) | 1003 (55.8) | <0.001 | 388 (46.1) | <0.001 | 615 (64.4) | <0.001 |
| CKD | 213 (7.6) | 279 (15.5) | <0.001 | 81 (9.6) | 0.05 | 198 (20.7) | <0.001 |
| CVD | 836 (29.7) | 888 (49.4) | <0.001 | 332 (39.5) | <0.001 | 556 (58.2) | <0.001 |
| Cancer history | 606 (21.5) | 581 (32.3) | <0.001 | 202 (24.0) | 0.13 | 379 (39.7) | <0.001 |
| Severe COVID-19 outcomes | |||||||
| Hospitalization | 677 (24.0) | 656 (36.5) | <0.001 | 268 (31.9) | <0.001 | 388 (40.6) | <0.001 |
| ICU admission | 234 (8.3) | 216 (12.0) | <0.001 | 95 (11.3) | 0.008 | 121 (12.7) | <0.001 |
| Death | 26 (0.9) | 40 (2.2) | <0.001 | 10 (1.2) | 0.49 | 30 (3.1) | <0.001 |
| Hospitalization AOR (95% CI) | ICU Admission AOR (95% CI) | Death AOR (95% CI) | |
|---|---|---|---|
| Obesity | 0.99 (0.83, 1.19) | 0.85 (0.66, 1.11) | 0.56 (0.31, 1.05) |
| Diabetes | 1.57 (1.30, 1.89) | 1.51 (1.16, 1.97) | 1.39 (0.80, 2.42) |
| Asthma | 0.94 (0.76, 1.16) | 0.82 (0.61, 1.12) | 1.25 (0.65, 2.39) |
| COPD | 1.76 (1.38, 2.4) | 1.59 (1.17, 2.17) | 1.57 (0.86, 2.89) |
| Hypertension | 1.32 (1.08, 1.60) | 1.02 (0.75, 1.38) | 1.72 (0.73, 4.07) |
| CKD | 2.05 (1.63, 2.58) | 1.74 (1.30, 2.33) | 1.87 (1.07, 3.27) |
| CVD | 2.78 (2.33, 3.31) | 3.52 (2.68, 4.63) | 8.35 (2.99, 23.34) |
| Cancer | 0.80 (0.68, 0.95) | 0.79 (0.62, 1.01) | 0.92 (0.55, 1.56) |
| Hospitalization AOR (95% CI) | ICU Admission AOR (95% CI) | Death AOR (95% CI) | |
|---|---|---|---|
| Ever smoker status | |||
| Never | Reference | Reference | Reference |
| Ever | 1.26 (1.08, 1.46) | 1.20 (0.96, 1.49) | 1.15 (0.65, 2.00) |
| Former and current smoking status | |||
| Never | Reference | Reference | Reference |
| Current | 1.23 (1.02, 1.49) | 1.24 (0.94, 1.64) | 0.77 (0.34, 1.71) |
| Former | 1.28 (1.07, 1.54) ¶ | 1.16 (0.89, 1.51) | 1.34 (0.75, 2.40) |
| Packs smoked per day | 1.30 (1.10, 1.53) | 1.23 (1.04, 1.44) | 0.99 (0.56, 1.73) |
| Years of smoking | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 1.01 (0.99, 1.03) |
| Pack-years of smoking | |||
| Per 10 pack-years | 1.09 (1.02, 1.17) | 1.07 (0.99, 1.15) | 1.00 (0.86, 1.16) |
| Never smokers | Reference | Reference | Reference |
| 1 to 10 pack-years | 0.87 (0.64, 1.18) | 0.87 (0.56, 1.34) | N/A |
| 11 to 20 pack-years | 1.07 (0.73, 1.56) | 0.92 (0.53, 1.58) | N/A |
| 21 to 30 pack-years | 1.21 (0.80, 1.85) | 0.81 (0.42, 1.53) | N/A |
| >31 pack-years | 1.44 (0.97, 2.15) | 1.22 (0.71, 2.09) | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahabee-Gittens, E.M.; Mendy, A.; Merianos, A.L. Assessment of Severe COVID-19 Outcomes Using Measures of Smoking Status and Smoking Intensity. Int. J. Environ. Res. Public Health 2021, 18, 8939. https://doi.org/10.3390/ijerph18178939
Mahabee-Gittens EM, Mendy A, Merianos AL. Assessment of Severe COVID-19 Outcomes Using Measures of Smoking Status and Smoking Intensity. International Journal of Environmental Research and Public Health. 2021; 18(17):8939. https://doi.org/10.3390/ijerph18178939
Chicago/Turabian StyleMahabee-Gittens, E. Melinda, Angelico Mendy, and Ashley L. Merianos. 2021. "Assessment of Severe COVID-19 Outcomes Using Measures of Smoking Status and Smoking Intensity" International Journal of Environmental Research and Public Health 18, no. 17: 8939. https://doi.org/10.3390/ijerph18178939
APA StyleMahabee-Gittens, E. M., Mendy, A., & Merianos, A. L. (2021). Assessment of Severe COVID-19 Outcomes Using Measures of Smoking Status and Smoking Intensity. International Journal of Environmental Research and Public Health, 18(17), 8939. https://doi.org/10.3390/ijerph18178939







