Adherence to a Lifestyle Exercise and Nutrition Intervention in University Employees during the COVID-19 Pandemic: A Randomized Controlled Trial
Abstract
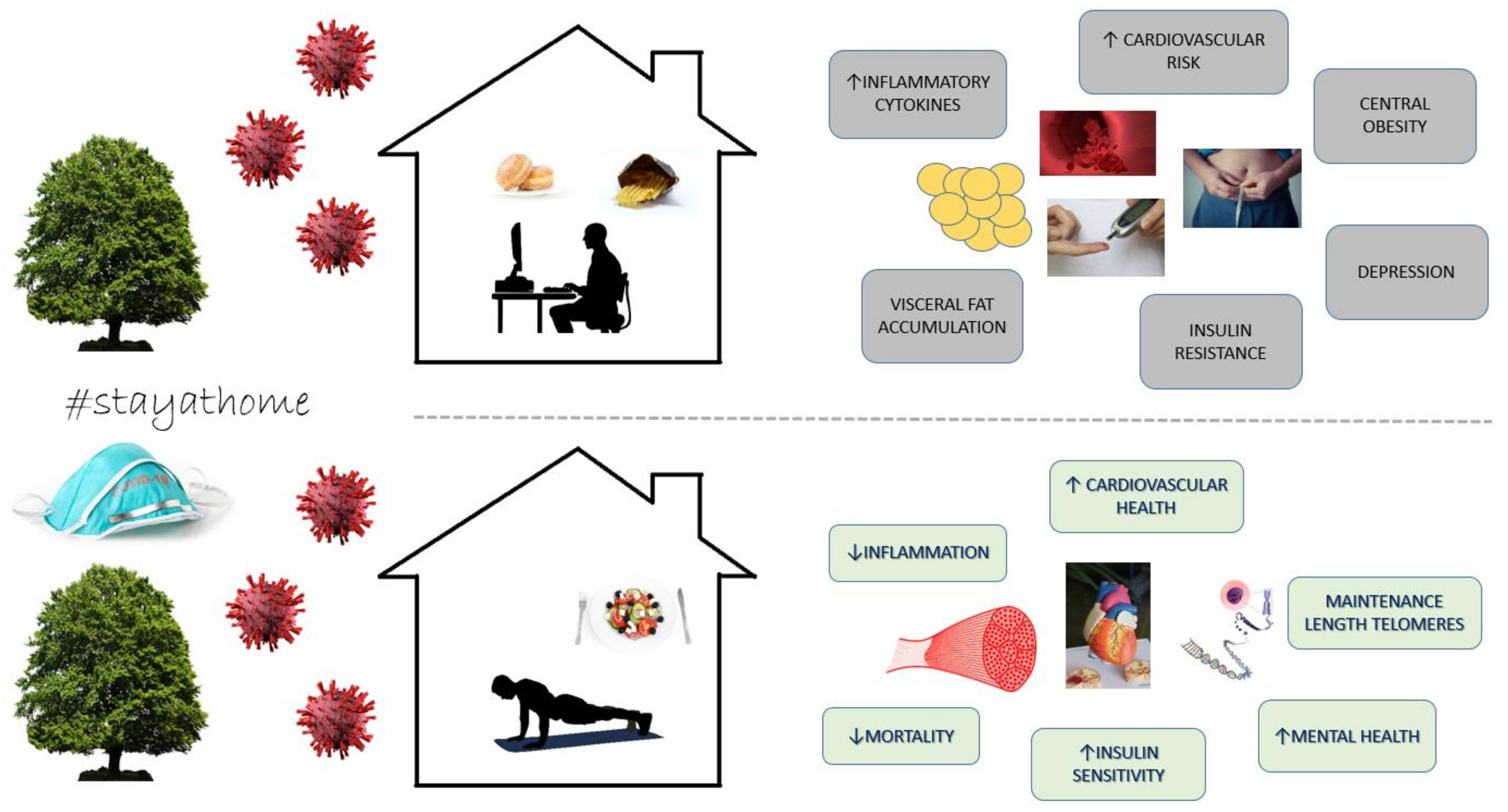
:1. Introduction
2. Methods
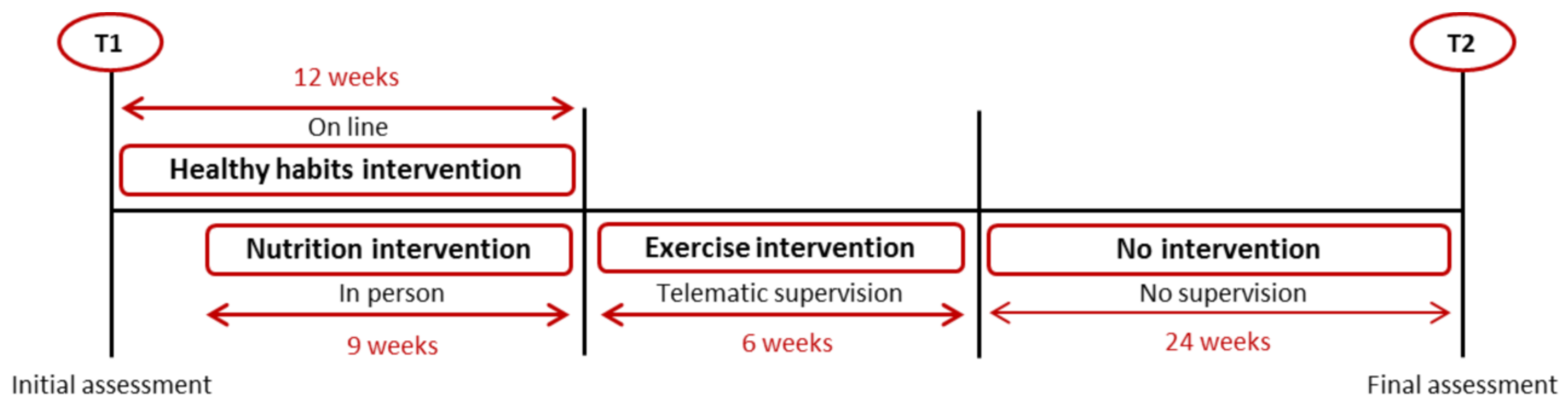
2.1. Study Design
2.2. Participants
2.3. Sample Size
2.4. Randomization
2.5. Variables
2.5.1. Lifestyle
2.5.2. Health-Related Quality of Life
2.5.3. Anthropometric Variables
2.6. Lifestyle Intervention
2.7. Place of the Intervention and Times of Assessments
2.8. Statistical Analysis
3. Results
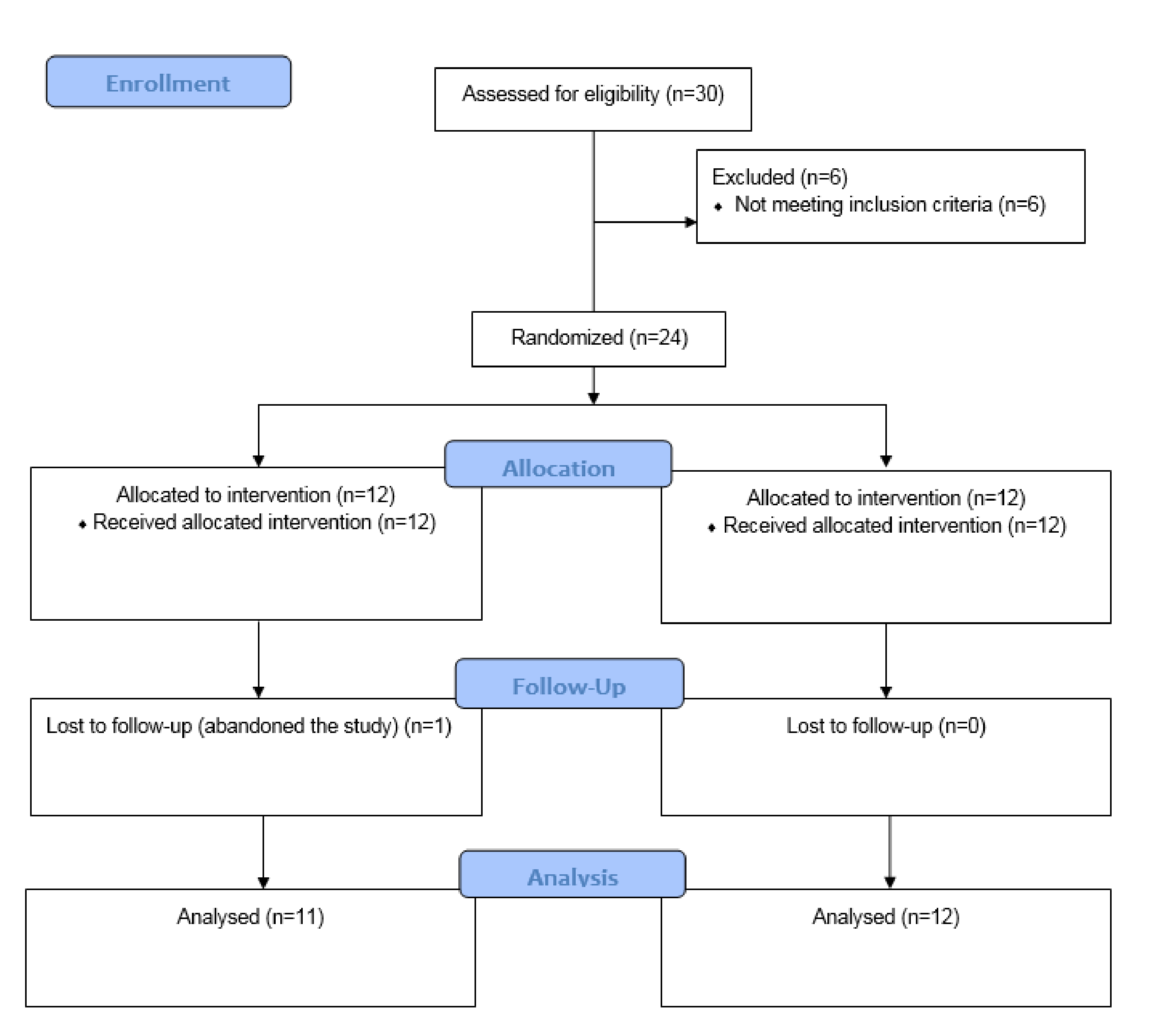
3.1. Recruitement
3.2. Description of the Sample
3.3. Lifestyle
3.4. Health-Related Quality of Life
3.5. Anthropometric Variables
Compliance with the Exercise and Nutrition Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ciotti, M.; Ciccozzi, M.; Terrinoni, A.; Jiang, W.C.; Wang, C.B.; Bernardini, S. The COVID-19 pandemic. Crit. Rev. Clin. Lab. Sci. 2020, 57, 365–388. [Google Scholar] [CrossRef]
- Genin, P.M.; Lambert, C.; Larras, B.; Pereira, B.; Toussaint, J.-F.; Baker, J.S.; Tremblay, A.; Thivel, D.; Duclos, M. How Did the COVID-19 Confinement Period Affect Our Physical Activity Level and Sedentary Behaviors? Methodology and First Results From the French National ONAPS Survey. J. Phys. Act. Health 2021, 18, 1–8. [Google Scholar] [CrossRef]
- López-Bueno, R.; Calatayud, J.; Casaña, J.; Casajús, J.A.; Smith, L.; Tully, M.A.; Andersen, L.L.; López-Sánchez, G.F. COVID-19 Confinement and Health Risk Behaviors in Spain. Front. Psychol. 2020, 11, 1–10. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef] [PubMed]
- Castañeda-Babarro, A.; Coca, A.; Arbillaga-Etxarri, A.; Gutiérrez-Santamaría, B. Physical activity change during COVID-19 confinement. Int. J. Environ. Res. Public Health 2020, 17, 6878. [Google Scholar] [CrossRef] [PubMed]
- Franco, E.; Urosa, J.; Barakat, R.; Refoyo, I. Physical activity and adherence to the mediterranean diet among spanish employees in a health-promotion program before and during the COVID-19 pandemic: The sanitas-healthy cities challenge. Int. J. Environ. Res. Public Health 2021, 18, 2735. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Sánchez, E.; Ramírez-Vargas, G.; Avellaneda-López, Y.; Orellana-Pecino, J.I.; García-Marín, E.; Díaz-Jimenez, J. Eating habits and physical activity of the spanish population during the COVID-19 pandemic period. Nutrients 2020, 12, 2826. [Google Scholar] [CrossRef]
- Tárraga López, P.J.; Panisello Royo, J.M.; Carbayo Herencia, J.; Carro, A.; Rosich, N.; Panisello, M.; Presas, J.A.; Albero, J.S. Changes in adherence to the Mediterranean diet observed in a Spanish population during confinement for the SARS-CoV-2 pandemic. Nutr. Hosp. 2020, 38, 109–120. [Google Scholar] [CrossRef]
- Arocha Rodulfo, J.I. Sedentarism, a disease from xxi century. Clínica e Investigación en Arteriosclerosis 2019, 31, 233–240. [Google Scholar] [CrossRef]
- Motta, V.; Bonzini, M.; Grevendonk, L.; Iodice, S.; Bollati, V. Epigenetics applied to epidemiology: Investigating environmental factors and lifestyle influence on human health. Med. Lav. 2017, 108, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Keadle, S.K.; Troiano, R.P.; Kahle, L.; Koster, A.; Brychta, R.; Van Domelen, D.; Caserotti, P.; Chen, K.Y.; Harris, T.B.; et al. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in US adults. Am. J. Clin. Nutr. 2016, 104, 1424–1432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Booth, F.W.; Roberts, C.K.; Thyfault, J.P.; Ruegsegger, G.N.; Toedebusch, R.G. Role of inactivity in chronic diseases: Evolutionary insight and pathophysiological mechanisms. Physiol. Rev. 2017, 97, 1351–1402. [Google Scholar] [CrossRef] [PubMed]
- González, K.; Fuentes, J.; Márquez, J.L. Physical inactivity, sedentary behavior and chronic diseases. Korean J. Fam. Med. 2017, 38, 111–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patterson, R.; McNamara, E.; Tainio, M.; de Sá, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018, 33, 811–829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Strain, T.; Wijndaele, K.; Garcia, L.; Cowan, M.; Guthold, R.; Brage, S.; Bull, F.C. Levels of domain-specific physical activity at work, in the household, for travel and for leisure among 327,789 adults from 104 countries. Br. J. Sports Med. 2020, 54, 1488–1497. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Powell, K.E.; Jakicic, J.M.; Troiano, R.P.; Piercy, K.; Tennant, B. Sedentary Behavior and Health: Update from the 2018 Physical Activity Guidelines Advisory Committee. Med. Sci. Sports Exerc. 2019, 51, 1227–1241. [Google Scholar] [CrossRef] [PubMed]
- Akins, J.D.; Crawford, C.K.; Burton, H.M.; Wolfe, A.S.; Vardarli, E.; Coyle, E.F. Inactivity induces resistance to the metabolic benefits following acute exercise. J. Appl. Physiol. 2019, 126, 1088–1094. [Google Scholar] [CrossRef]
- Leiva, A.M.; Martínez, M.A.; Cristi-Montero, C.; Salas, C.; Ramírez-Campillo, R.; Díaz Martínez, X.; Aguilar-Farías, N.; Celis-Morales, C. El sedentarismo se asocia a un incremento de factores de riesgo cardiovascular y metabólicos independiente de los niveles de actividad física. Rev. Med. Chile 2017, 145, 458–467. [Google Scholar] [CrossRef] [Green Version]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M.; Ding, D.; Heath, G.; et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [Green Version]
- Marçal, I.R.; Fernandes, B.; Viana, A.A.; Ciolac, E.G. The Urgent Need for Recommending Physical Activity for the Management of Diabetes During and Beyond COVID-19 Outbreak. Front. Endocrinol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Puccinelli, P.J.; da Costa, T.S.; Seffrin, A.; de Lira, C.A.B.; Vancini, R.L.; Nikolaidis, P.T.; Knechtle, B.; Rosemann, T.; Hill, L.; Andrade, M.S. Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: An internet-based survey. BMC Public Health 2021, 21, 425. [Google Scholar] [CrossRef]
- Friedenreich, C.M.; Ryder-Burbidge, C.; McNeil, J. Physical activity, obesity and sedentary behavior in cancer etiology: Epidemiologic evidence and biologic mechanisms. Mol. Oncol. 2021, 15, 790–800. [Google Scholar] [CrossRef]
- Ferioli, M.; Zauli, G.; Maiorano, P.; Milani, D.; Mirandola, P.; Neri, L.M. Role of physical exercise in the regulation of epigenetic mechanisms in inflammation, cancer, neurodegenerative diseases, and aging process. J. Cell Physiol. 2019, 234, 14852–14864. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.D.; Crippa, A.; Woodcock, J.; Brage, S. Physical activity and incident type 2 diabetes mellitus: A systematic review and dose–response meta-analysis of prospective cohort studies. Diabetologia 2016, 59, 2527–2545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Saeidifard, F.; Medina-Inojosa, J.R.; West, C.P.; Olson, T.P.; Somers, V.K.; Bonikowske, A.R.; Prokop, L.J.; Vinciguerra, M.; Lopez-Jimenez, F. The association of resistance training with mortality: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2019, 26, 1647–1665. [Google Scholar] [CrossRef]
- Garcia-Arellano, A.; Ramallal, R.; Ruiz-Canela, M.; Salas-Salvadó, J.; Corella, D.; Shivappa, N.; Schröder, H.; Hébert, J.; Ros, E.; Gómez-Garcia, E.; et al. Dietary Inflammatory Index and Incidence of Cardiovascular Disease in the PREDIMED Study. Nutrients 2015, 7, 4124–4138. [Google Scholar] [CrossRef] [Green Version]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Ros, E. The PREDIMED study. Endocrinol. Diabetes. Nutr. 2017, 64, 63–66. [Google Scholar] [CrossRef]
- Potì, F.; Santi, D.; Spaggiari, G.; Zimetti, F.; Zanotti, I. Polyphenol health effects on cardiovascular and neurodegenerative disorders: A review and meta-analysis. Int. J. Mol. Sci. 2019, 20, 352. [Google Scholar] [CrossRef] [Green Version]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Y.; Bo, Y.; Liu, Y. Dietary total fat, fatty acids intake, and risk of cardiovascular disease: A dose-response meta-analysis of cohort studies. Lipids Health Dis. 2019, 18, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Caprara, G. Mediterranean-type dietary pattern and physical activity: The winning combination to counteract the rising burden of non-communicable diseases (NCDS). Nutrients 2021, 13, 429. [Google Scholar] [CrossRef]
- W.H.O.; Burton, J. WHO Healthy Workplace Framework and Model: Background and Supporting Literature and Practices; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Hunter, J.R.; Gordon, B.A.; Bird, S.R.; Benson, A.C. Exercise Supervision Is Important for Cardiometabolic Health Improvements: A 16-Week Randomized Controlled Trial. J. Strength Cond. Res. 2020, 34, 866–877. [Google Scholar] [CrossRef] [PubMed]
- Karatrantou, K.; Gerodimos, V.; Manouras, N.; Vasilopoulou, T.; Melissopoulou, A.; Mesiakaris, A.F.; Theodorakis, Y. Health-Promoting Effects of a Concurrent Workplace Training Program in Inactive Office Workers (HealPWorkers): A Randomized Controlled Study. Am. J. Health Promot. 2020, 34, 376–386. [Google Scholar] [CrossRef]
- Vilela, B.L.; Benedito-Silva, A.A.; De Lira, C.A.B.; Dos Santos Andrade, M. Workplace exercise and educational program for improving fitness outcomes related to health in workers: A randomized controlled trial. J. Occup. Environ. Med. 2015, 57, 235–240. [Google Scholar] [CrossRef]
- Ismail, I.; Keating, S.E.; Baker, M.K.; Johnson, N.A. A systematic review and meta-analysis of the effect of aerobic vs. resistance exercise training on visceral fat. Obes. Rev. 2012, 13, 68–91. [Google Scholar] [CrossRef] [PubMed]
- Gepner, Y.; Shelef, I.; Schwarzfuchs, D.; Zelicha, H.; Tene, L.; Yaskolka Meir, A.; Shai, I. Effect of Distinct Lifestyle Interventions on Mobilization of Fat Storage Pools: CENTRAL MRI Randomized Controlled Trial. Circulation 2018, 137, 1143–1157. [Google Scholar] [CrossRef]
- Kong, J.P.; Jok, L.; Ayub, A.B.; Bau, R.A. Worksite weight management program: A 3-months intervention study in a primary health care setting. Nutr. Food Sci. 2018, 47, 39–53. [Google Scholar] [CrossRef]
- Reed, J.L.; Prince, S.A.; Elliott, C.G.; Mullen, K.A.; Tulloch, H.E.; Hiremath, S.; Cotie, L.M.; Pipe, A.L.; Reid, R.D. Impact of workplace physical activity interventions on physical activity and cardiometabolic health among working-age women. Circ. Cardiovasc. Qual. Outcomes. 2017, 10, e003516. [Google Scholar] [CrossRef]
- Hutcheson, A.K.; Piazza, A.J.; Knowlden, A.P. Work Site–Based Environmental Interventions to Reduce Sedentary Behavior: A Systematic Review. Am. J. Heal. Promot. 2018, 32, 32–47. [Google Scholar] [CrossRef] [PubMed]
- Shai, I.; Schwarzfuchs, D.; Henkin, Y.; Shahar, D.R.; Witkow, S.; Greenberg, I.; Golan, R.; Fraser, D.; Bolotin, A.; Vardi, H.; et al. Weight Loss with a Low-Carbohydrate, Mediterranean, or Low-Fat Diet. N. Engl. J. Med. 2008, 359, 229–241. [Google Scholar] [CrossRef] [Green Version]
- Middleton, K.R.; Anton, S.D.; Perri, M.G. Long-Term Adherence to Health Behavior Change. Am. J. Lifestyle Med. 2013, 7, 395–404. [Google Scholar] [CrossRef] [Green Version]
- Schoeppe, S.; Alley, S.; Van Lippevelde, W.; Bray, N.A.; Williams, S.L.; Duncan, M.J.; Vandelanotte, C. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13. [Google Scholar] [CrossRef] [Green Version]
- Stephenson, A.; McDonough, S.M.; Murphy, M.H.; Nugent, C.D.; Mair, J.L. Using computer, mobile and wearable technology enhanced interventions to reduce sedentary behaviour: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 105. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.M.; LaMontagne, A.D.; English, D.R.; Howard, P. Efficacy of a workplace osteoporosis prevention intervention: A cluster randomized trial. BMC Public Health 2016, 16. [Google Scholar] [CrossRef] [Green Version]
- Howarth, A.; Quesada, J.; Silva, J.; Judycki, S.; Mills, P.R. The impact of digital health interventions on health-related outcomes in the workplace: A systematic review. Digit. Health 2018, 4, 205520761877086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buckingham, S.A.; Williams, A.J.; Morrissey, K.; Price, L.; Harrison, J. Mobile health interventions to promote physical activity and reduce sedentary behaviour in the workplace: A systematic review. Digit. Health 2019, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. WHO Physical Activity Recommendations. Available online: https://www.who.int/publications/i/item/9789241599979 (accessed on 8 April 2021).
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-item mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS ONE 2012, 7, e043134. [Google Scholar] [CrossRef] [Green Version]
- Field, C.A.; Adinoff, B.; Harris, T.R.; Ball, S.A.; Carroll, K.M. Construct, concurrent and predictive validity of the URICA: Data from two multi-site clinical trials. Drug Alcohol Depend. 2009, 101, 115–123. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Fortis, A.; Ulla Díez, S.M.; Padilla, J.L. Psychometric properties of the Spanish version of the health-promoting lifestyle profile II. Res. Nurs. Health 2012, 35, 301–313. [Google Scholar] [CrossRef]
- University of Nebraska. Health Promoting Lifestyle Profile II Nursing University of Nebraska Medical Center. Available online: https://www.unmc.edu/nursing/faculty/health-promoting-lifestyle-profile-II.html (accessed on 7 April 2021).
- Alzahrani, S.H.; Malik, A.A.; Bashawri, J.; Shaheen, S.A.; Shaheen, M.M.; Alsaib, A.A.; Mubarak, M.A.; Adam, Y.S.; Abdulwassi, H.K. Health-promoting lifestyle profile and associated factors among medical students in a Saudi university. SAGE Open Med. 2019, 7, 205031211983842. [Google Scholar] [CrossRef] [PubMed]
- Sayón-Orea, C.; Razquin, C.; Bulló, M.; Corella, D.; Fitó, M.; Romaguera, D.; Vioque, J.; Alonso-Gómez, Á.M.; Wärnberg, J.; Martínez, J.A.; et al. Effect of a Nutritional and Behavioral Intervention on Energy-Reduced Mediterranean Diet Adherence among Patients with Metabolic Syndrome: Interim Analysis of the PREDIMED-Plus Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2019, 322, 1486–1499. [Google Scholar] [CrossRef]
- Cleland, C.L.; Hunter, R.F.; Kee, F.; Cupples, M.E.; Sallis, J.F.; Tully, M.A. Validity of the Global Physical Activity Questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Public Health. 2014, 14, 1255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alonso, J. La versión española del SF-36 Health Survey (Cuestionario de Salud SF-36): Un instrumento para la medida de los resultados clínicos. Med. Clin. 1995, 104, 771–776. [Google Scholar]
- Jayadevappa, R.; Cook, R.; Chhatre, S. Minimal important difference to infer changes in health-related quality of life—a systematic review. J. Clin. Epidemiol. 2017, 89, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.T.E. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [Green Version]
- Alonso-Domínguez, R.; García-Ortiz, L.; Patino-Alonso, M.C.; Sánchez-Aguadero, N.; Gómez-Marcos, M.A.; Recio-Rodríguez, J.I. Effectiveness of a multifactorial intervention in increasing adherence to the mediterranean diet among patients with diabetes mellitus type 2: A controlled and randomized study (EMID study). Nutrients 2019, 11, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulla Díez, S.M.; Fortis, A.P.; Franco, S.F. Efficacy of a health-promotion intervention for college students: A randomized controlled trial. Nurs. Res. 2012, 61, 129–140. [Google Scholar] [CrossRef]
- Matthews, C.E.; George, S.M.; Moore, S.C.; Bowles, H.R.; Blair, A.; Park, Y.; Troiano, R.P.; Hollenbeck, A.; Schatzkin, A. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am. J. Clin. Nutr. 2012, 95, 437–445. [Google Scholar] [CrossRef] [Green Version]
- Vilagut, G.; Valderas, J.M.; Ferrer, M.; Garin, O.; López-García, E.; Alonso, J. Interpretación de los cuestionarios de salud SF-36 y SF-12 en España: Componentes físico y mental. Med. Clin. 2008, 130, 726–735. [Google Scholar] [CrossRef] [Green Version]
- Dishman, R.K.; DeJoy, D.M.; Wilson, M.G.; Vandenberg, R.J. Move to Improve: A Randomized Workplace Trial to Increase Physical Activity. Am. J. Prev. Med. 2009, 36, 133–141. [Google Scholar] [CrossRef]
- McEachan, R.R.C.; Lawton, R.J.; Jackson, C.; Conner, M.; Meads, D.M.; West, R.M. Testing a workplace physical activity intervention: A cluster randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2011, 8. [Google Scholar] [CrossRef] [Green Version]
- Madden, S.K.; Cordon, E.L.; Bailey, C.; Skouteris, H.; Ahuja, K.; Hills, A.P.; Hill, B. The effect of workplace lifestyle programmes on diet, physical activity, and weight-related outcomes for working women: A systematic review using the TIDieR checklist. Obes. Rev. 2020, 21. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Ogborn, D.; Krieger, J.W. Dose-response relationship between weekly resistance training volume and increases in muscle mass: A systematic review and meta-analysis. J. Sports Sci. 2017, 35, 1073–1082. [Google Scholar] [CrossRef]
- Gloster, A.T.; Lamnisos, D.; Lubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; Aydın, G.; Chong, Y.Y.; et al. Impact of COVID-19 pandemic on mental health: An international study. PLoS ONE 2020, 15, e0244809. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Di Clemente, C.C. Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy 1982, 19, 276–288. [Google Scholar] [CrossRef]
- Stonerock, G.L.; Blumenthal, J.A. Role of Counseling to Promote Adherence in Healthy Lifestyle Medicine: Strategies to Improve Exercise Adherence and Enhance Physical Activity. Prog. Cardiovasc. Dis. 2017, 59, 455–462. [Google Scholar] [CrossRef] [Green Version]
- Howlett, N.; Trivedi, D.; Troop, N.A.; Chater, A.M. Are physical activity interventions for healthy inactive adults effective in promoting behavior change and maintenance, and which behavior change techniques are effective? A systematic review and meta-analysis. Transl. Behav. Med. 2019, 9, 147–157. [Google Scholar] [CrossRef] [PubMed]
| Variables | Group | T1 | T2 | p-Value Time | p-Value Group | p-Value txg | η2p txg |
|---|---|---|---|---|---|---|---|
| HPLP II | |||||||
| Health-Promoting Lifestyle (total score) | IG CG | 121.27 ± 12.54 123.67 ± 15.33 | 141.73 ± 17.43 131.58 ± 13.83 | <0.001 | 0.50 | * 0.03 | 0.22 |
| Health Responsibility | IG CG | 17.00 ± 2.61 18.08 ± 4.52 | 21.36 ± 4.25 19.67 ± 4.16 | <0.001 | 0.85 | * 0.02 | 0.22 |
| Physical Activity | IG CG | 14.00 ± 4.27 13.33 ± 3.60 | 19.81 ± 4.31 14.83 ± 4.45 | <0.001 | 0.07 | * 0.02 | 0.22 |
| Nutrition | IG CG | 21.82 ± 2.68 22.25 ± 4.71 | 26.64 ± 2.84 24.08 ± 4.70 | <0.001 | 0.49 | * 0.02 | 0.23 |
| Spiritual growth | IG CG | 24.64 ± 2.80 26.50 ± 3.75 | 27.27 ± 2.90 28.33 ± 4.10 | 0.001 | 0.28 | 0.52 | 0.02 |
| Interpersonal Relations | IG CG | 27.18 ± 3.79 27.33 ± 3.85 | 27.67 ± 3.91 27.42 ± 3.87 | 0.69 | 0.98 | 0.78 | 0.004 |
| Stress management | IG CG | 16.64 ± 2.77 16.17 ± 2.41 | 19.00 ± 3.46 17.25 ± 2.80 | 0.01 | 0.30 | 0.28 | 0.06 |
| MEDAS | |||||||
| Adherence to the Mediterranean diet | IG CG | 7.00 ± 1.41 7.08 ± 1.08 | 9.82 ± 1.60 8.92 ± 2.02 | <0.001 | 0.47 | 0.16 | 0.09 |
| GPAQ | |||||||
| Physical activity levels (METS-min per week) | IG CG | 327.27 ± 258.96 316.67 ± 367.48 | 1327.27 ± 1046.15 1016.67 ± 1039.26 | 0.001 | 0.49 | 0.52 | 0.02 |
| Daily sitting time (min) | IG CG | 463.64 ± 180.18 540.00 ± 209.41 | 312.73 ± 150.80 559.17 ± 259.32 | 0.18 | 0.03 | 0.09 | 0.13 |
| SF-36 | |||||||
| Physical Component Summary | IG CG | 49.06 ± 5.04 51.78 ± 7.20 | 54.51 ± 4.02 50.25 ± 8.52 | 0.37 | 0.65 | 0.12 | 0.11 |
| Mental Component Summary | IG CG | 51.43 ± 8.24 40.60 ± 12.76 | 53.07 ± 5.99 43.70 ± 11.73 | 0.32 | 0.01 | 0.75 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García Pérez de Sevilla, G.; Barceló Guido, O.; De la Cruz, M.d.l.P.; Blanco Fernández, A.; Alejo, L.B.; Montero Martínez, M.; Pérez-Ruiz, M. Adherence to a Lifestyle Exercise and Nutrition Intervention in University Employees during the COVID-19 Pandemic: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 7510. https://doi.org/10.3390/ijerph18147510
García Pérez de Sevilla G, Barceló Guido O, De la Cruz MdlP, Blanco Fernández A, Alejo LB, Montero Martínez M, Pérez-Ruiz M. Adherence to a Lifestyle Exercise and Nutrition Intervention in University Employees during the COVID-19 Pandemic: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(14):7510. https://doi.org/10.3390/ijerph18147510
Chicago/Turabian StyleGarcía Pérez de Sevilla, Guillermo, Olga Barceló Guido, María de la Paz De la Cruz, Ascensión Blanco Fernández, Lidia B. Alejo, María Montero Martínez, and Margarita Pérez-Ruiz. 2021. "Adherence to a Lifestyle Exercise and Nutrition Intervention in University Employees during the COVID-19 Pandemic: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 14: 7510. https://doi.org/10.3390/ijerph18147510
APA StyleGarcía Pérez de Sevilla, G., Barceló Guido, O., De la Cruz, M. d. l. P., Blanco Fernández, A., Alejo, L. B., Montero Martínez, M., & Pérez-Ruiz, M. (2021). Adherence to a Lifestyle Exercise and Nutrition Intervention in University Employees during the COVID-19 Pandemic: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(14), 7510. https://doi.org/10.3390/ijerph18147510







