Mental Health Consequences of the Three Mile Island, Chernobyl, and Fukushima Nuclear Disasters: A Scoping Review
Abstract
1. Introduction
- (1)
- To clarify the mental health consequences after the three major NPP accidents (TMI, Chernobyl, and Fukushima) over a long period.
- (2)
- To identify positive and negative factors that are associated with the mental health outcomes of people who were exposed to these NPP disasters.
- (3)
- To compare the mental health consequences among the three NPP disasters and identify similarities and differences.
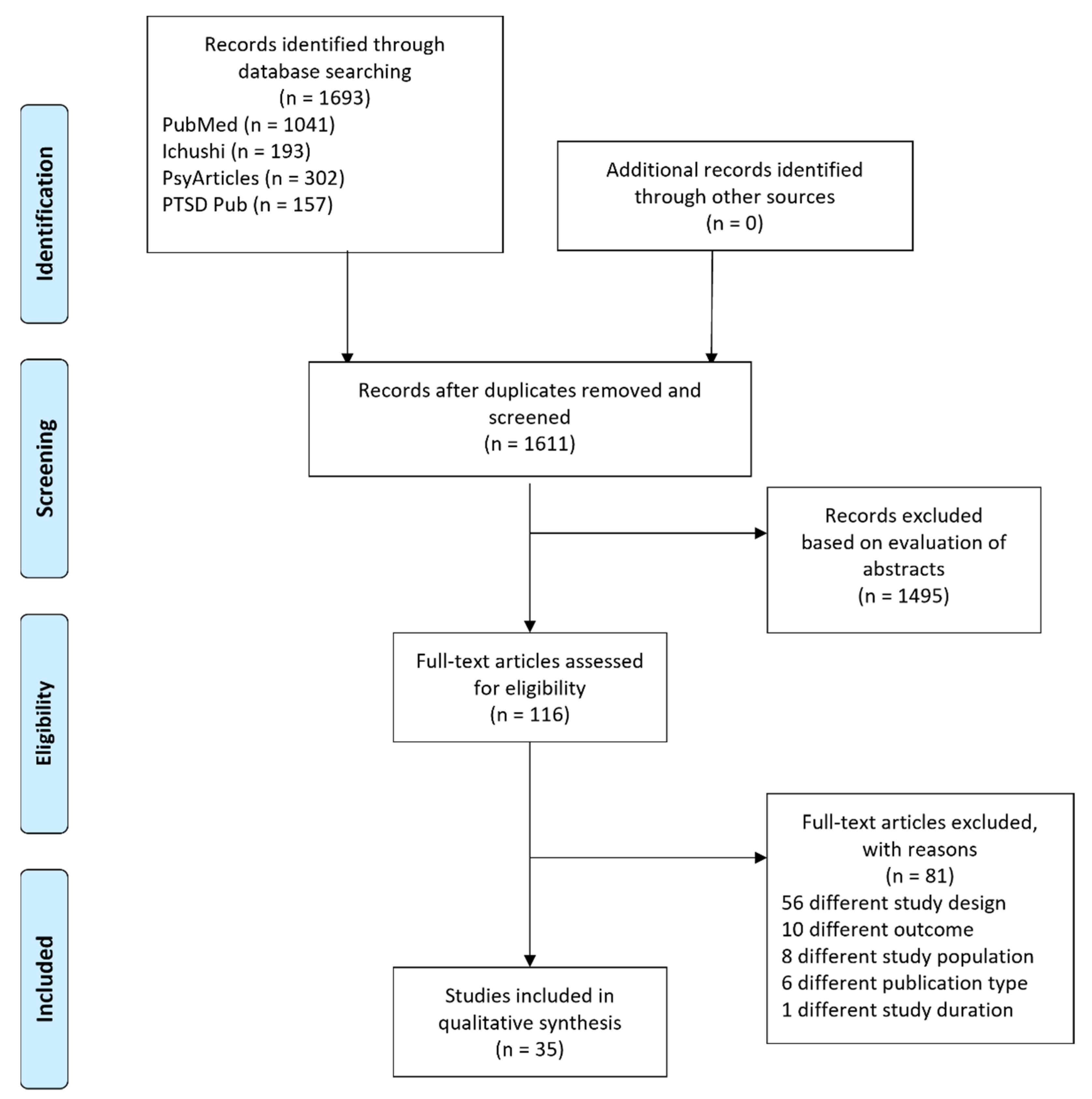
2. Methods
3. Results
3.1. Characteristics of the Included Studies
3.2. Changes in Mental Health Measures over Time
3.2.1. TMI
3.2.2. Chernobyl
3.2.3. Fukushima
3.2.4. Temporal Profiles
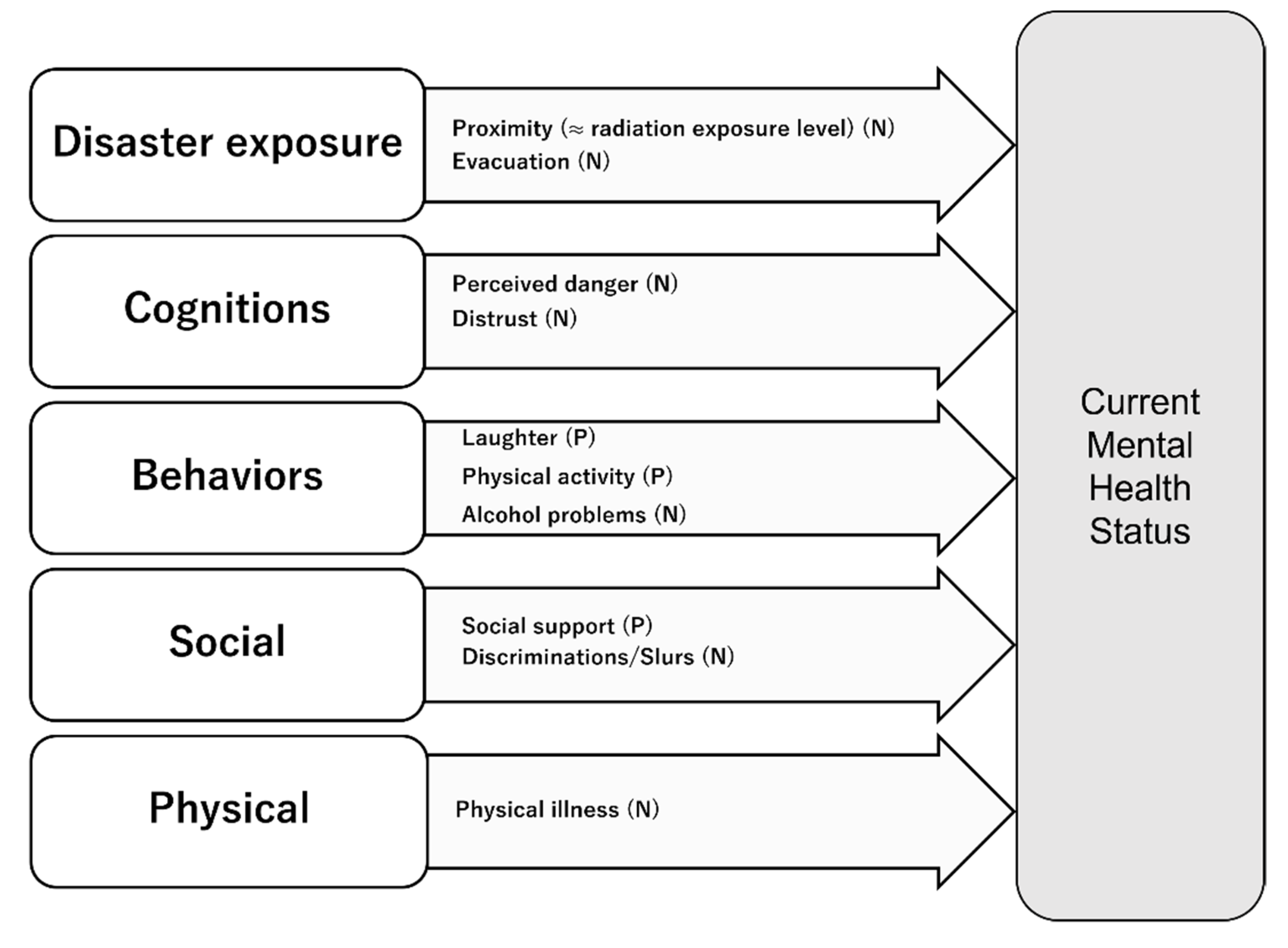
3.3. Risk and Protective Factors According to Psychological Distress
4. Discussion
4.1. Study Settings
4.2. Changes in Mental Health Outcomes over Time
4.3. Risk and Protective Factors
4.3.1. Radiation Exposure Level
4.3.2. Stigma
4.3.3. Behavioral Factors (Laughter, Physical Activity)
4.3.4. Physical Illness
4.4. Comparison between Nuclear and Natural Disasters
4.5. Similarities and Differences
4.6. Limitations
4.7. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Christodouleas, J.P.; Forrest, R.D.; Ainsley, C.G.; Tochner, Z.; Hahn, S.M.; Glatstein, E. Short-term and long-term health risks of nuclear power-plant accidents. N. Engl. J. Med. 2011, 364, 2334–2341. [Google Scholar] [CrossRef]
- International Atomic Energy Agency. The International Nuclear and Radiological Event Scale. Available online: https://www.iaea.org/resources/databases/international-nuclear-and-radiological-event-scale (accessed on 29 June 2021).
- U.S. Government Printing Office. President’s Commission on the accident at Three Mile Island; U.S. Government Printing Office: Washington, DC, USA, 1979.
- International Atomic Energy Agency. Chernobyl’s Legacy: Health, Environmental and Socio-Economic Impacts and Recommendations to the Governments of Belarus, the Russian federation and Ukraine, 2003–2005. Available online: https://www.iaea.org/sites/default/files/chernobyl.pdf (accessed on 28 June 2021).
- Bromet, E.J.; Havenaar, J.M.; Guey, L.T. A 25 year retrospective review of the psychological consequences of the Chernobyl accident. Clin. Oncol. 2011, 23, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Shigemura, J.; Terayama, T.; Kurosawa, M.; Kobayashi, Y.; Toda, H.; Nagamine, M.; Yoshino, A. Mental health consequences for survivors of the 2011 Fukushima nuclear disaster: A systematic review. Part 1: Psychological consequences. CNS Spectr. 2020, 26, 14–29. [Google Scholar] [CrossRef] [PubMed]
- Terayama, T.; Shigemura, J.; Kobayashi, Y.; Kurosawa, M.; Nagamine, M.; Toda, H.; Yoshino, A. Mental health consequences for survivors of the 2011 Fukushima nuclear disaster: A systematic review. Part 2: Emotional and behavioral consequences. CNS Spectr. 2020, 26, 30–42. [Google Scholar] [CrossRef]
- Norris, F.H.; Tracy, M.; Galea, S. Looking for resilience: Understanding the longitudinal trajectories of responses to stress. Soc. Sci. Med. 2009, 68, 2190–2198. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Diminich, E.D. Annual Research Review: Positive adjustment to adversity--trajectories of minimal-impact resilience and emergent resilience. J. Child. Psychol. Psychiatry 2013, 54, 378–401. [Google Scholar] [CrossRef]
- Davis, K.; Drey, N.; Gould, D. What are scoping studies? A review of the nursing literature. Int. J. Nurs. Stud. 2009, 46, 1386–1400. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Park, J.E.; Lee, Y.J.; Seo, H.J.; Sheen, S.S.; Hahn, S.; Jang, B.H.; Son, H.J. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J. Clin. Epidemiol. 2013, 66, 408–414. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Bromet, E.; Schulberg, H.C.; Dunn, L. Reactions of psychiatric patients to the Three Mile Island nuclear accident. Arch. Gen. Psychiatry 1982, 39, 725–730. [Google Scholar] [CrossRef]
- Dohrenwend, B.P.; Dohrenwend, B.S.; Warheit, G.J.; Bartlett, G.S.; Goldsteen, R.L.; Goldsteen, K.; Martin, J.L. Stress in the community: A report to the President’s Commission on the Accident at Three Mile Island. Ann. N. Y. Acad. Sci. 1981, 365, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Goldsteen, R.; Schorr, J.K.; Goldsteen, K.S. Longitudinal study of appraisal at Three Mile Island: Implications for life event research. Soc. Sci. Med. 1989, 28, 389–398. [Google Scholar] [CrossRef]
- Goldsteen, R.; Schorr, J.K. The long-term impact of a man-made disaster: An examination of a small town in the aftermath of the Three Mile Island Nuclear Reactor Accident. Disasters 1982, 6, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Bromet, E.J.; Parkinson, D.K.; Schulberg, H.C.; Dunn, L.O.; Gondek, P.C. Mental health of residents near the Three Mile Island reactor: A comparative study of selected groups. J. Prev. Psychiary 1982, 1, 225–275. [Google Scholar]
- Dew, M.A.; Bromet, E.J.; Schulberg, H.C. A comparative analysis of two community stressors’ long-term mental health effects. Am. J. Community Psychol. 1987, 15, 167–184. [Google Scholar] [CrossRef]
- Bromet, E.J.; Parkinson, D.K.; Dunn, L.O. Long-term Mental Health Consequences of the Accident at Three Mile Island. Int. J. Ment. Health 1990, 19, 48–60. [Google Scholar] [CrossRef]
- Dew, M.A.; Bromet, E.J. Predictors of temporal patterns of psychiatric distress during 10 years following the nuclear accident at Three Mile Island. Soc. Psychiatry Psychiatr. Epidemiol. 1993, 28, 49–55. [Google Scholar] [CrossRef]
- Baum, A.; Cohen, L.; Hall, M. Control and intrusive memories as possible determinants of chronic stress. Psychosom. Med. 1993, 55, 274–286. [Google Scholar] [CrossRef]
- Davidson, L.M.; Weiss, L.; O’Keeffe, M.; Baum, A. Acute stressors and chronic stress at Three Mile Island. J. Trauma. Stress 1991, 4, 481–493. [Google Scholar] [CrossRef]
- Prince-Embury, S.; Rooney, J.F. Psychological adaptation among residents following restart of Three Mile Island. J. Trauma. Stress 1995, 8, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Koscheyev, V.S.; Martens, V.K.; Kosenkov, A.A.; Lartzev, M.A.; Leon, G.R. Psychological Status of Chernobyl Nuclear Power Plant Operators After the Nuclear Disaster. J. Trauma. Stress 1993, 6, 561–568. [Google Scholar] [CrossRef]
- Cwikel, J.; Rozovski, U. Coping with the stress of immigration among new immigrants to Israel from Commonwealth of Independent States (CIS) who were exposed to Chernobyl: The effect of age. Int. J. Aging Hum. Dev. 1998, 46, 305–318. [Google Scholar] [CrossRef] [PubMed]
- Cwikel, J.; Abdelgani, A.; Goldsmith, J.R.; Quastel, M.; Yevelson, I.I. Two-year follow up study of stress-related disorders among immigrants to Israel from the Chernobyl area. Environ. Health Perspect. 1997, 105 (Suppl. 6), 1545–1550. [Google Scholar]
- Rahu, K.; Bromet, E.J.; Hakulinen, T.; Auvinen, A.; Uusküla, A.; Rahu, M. Non-cancer morbidity among Estonian Chernobyl cleanup workers: A register-based cohort study. BMJ Open 2014, 4, e004516. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, A.; Charvat, H.; Shigemura, J.; Kales, S.N.; Tanigawa, T. Longitudinal trends in disaster-related insomnia among Fukushima nuclear plant workers: The Fukushima Nuclear Energy Workers’ Support Project study. Sleep 2019, 42, zsz043. [Google Scholar] [CrossRef]
- Kato, K.; Sekiguchi, M.; Nikaido, T.; Otoshi, K.I.; Matsuo, Y.; Igari, T.; Kobayashi, Y.; Takegami, M.; Fukumori, N.; Fukuma, S.; et al. Psychosocial Stress After a Disaster and Low Back Pain-Related Interference With Daily Living Among College Students: A Cohort Study in Fukushima. Spine 2017, 42, 1255–1260. [Google Scholar] [CrossRef]
- Ikeda, A.; Tanigawa, T.; Charvat, H.; Wada, H.; Shigemura, J.; Kawachi, I. Longitudinal effects of disaster-related experiences on mental health among Fukushima nuclear plant workers: The Fukushima NEWS Project Study. Psychol. Med. 2017, 47, 1936–1946. [Google Scholar] [CrossRef] [PubMed]
- Sawa, M.; Osaki, Y.; Koishikawa, H. Delayed recovery of caregivers from social dysfunction and psychological distress after the Great East Japan Earthquake. J. Affect. Disord. 2013, 148, 413–417. [Google Scholar] [CrossRef][Green Version]
- Oe, M.; Takahashi, H.; Maeda, M.; Harigane, M.; Fujii, S.; Miura, I.; Nagai, M.; Yabe, H.; Ohira, T.; Suzuki, Y.; et al. Changes of Posttraumatic Stress Responses in Evacuated Residents and Their Related Factors. Asia Pac. J. Public Health 2017, 29, 182S–192S. [Google Scholar] [CrossRef]
- Oe, M.; Maeda, M.; Nagai, M.; Yasumura, S.; Yabe, H.; Suzuki, Y.; Harigane, M.; Ohira, T.; Abe, M. Predictors of severe psychological distress trajectory after nuclear disaster: Evidence from the Fukushima Health Management Survey. BMJ Open 2016, 6, e013400. [Google Scholar] [CrossRef]
- Oe, M.; Maeda, M.; Ohira, T.; Itagaki, S.; Harigane, M.; Suzuki, Y.; Yabe, H.; Yasumura, S.; Kamiya, K.; Ohto, H. Trajectories of Emotional Symptoms and Peer Relationship Problems in Children after Nuclear Disaster: Evidence from the Fukushima Health Management Survey. Int. J. Environ. Res. Public Health 2018, 15, 82. [Google Scholar] [CrossRef] [PubMed]
- Oe, M.; Maeda, M.; Ohira, T.; Itagaki, S.; Harigane, M.; Suzuki, Y.; Yabe, H.; Yasumura, S.; Kamiya, K.; Ohto, H. Parental Recognition of Bullying and Associated Factors Among Children After the Fukushima Nuclear Disaster: A 3-Year Follow-Up Study From the Fukushima Health Management Survey. Front. Psychiatry 2019, 10, 283. [Google Scholar] [CrossRef]
- Fukasawa, M.; Kawakami, N.; Umeda, M.; Akiyama, T.; Horikoshi, N.; Yasumura, S.; Yabe, H.; Suzuki, Y.; Bromet, E.J. Long-lasting effects of distrust in government and science on mental health eight years after the Fukushima nuclear power plant disaster. Soc. Sci. Med. 2020, 258, 113108. [Google Scholar] [CrossRef] [PubMed]
- Bromet, E.J.; Guey, L.T.; Taormina, D.P.; Carlson, G.A.; Havenaar, J.M.; Kotov, R.; Gluzman, S.F. Growing up in the shadow of Chornobyl: Adolescents’ risk perceptions and mental health. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Guey, L.T.; Bromet, E.J.; Gluzman, S.F.; Zakhozha, V.; Paniotto, V. Determinants of participation in a longitudinal two-stage study of the health consequences of the Chornobyl nuclear power plant accident. BMC Med. Res. Methodol. 2008, 8, 27. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, Y.; Iwasa, H.; Goto, A.; Yoshida, K.; Matsuda, K.; Iwamitsu, Y.; Yasumura, S. Occurrence of depressive tendency and associated social factors among elderly persons forced by the Great East Japan Earthquake and nuclear disaster to live as long-term evacuees: A prospective cohort study. BMJ Open 2017, 7, e014339. [Google Scholar] [CrossRef]
- Komuro, H.; Shigemura, J.; Uchino, S.; Takahashi, S.; Nagamine, M.; Tanichi, M.; Saito, T.; Toda, H.; Kurosawa, M.; Kubota, K.; et al. Longitudinal Factors Associated With Increased Alcohol and Tobacco Use in Fukushima Nuclear Power Plant Workers 32 Months After the Nuclear Disaster: The Fukushima News Project Study. J. Occup. Environ. Med. 2019, 61, 69–74. [Google Scholar] [CrossRef]
- Tanisho, Y.; Shigemura, J.; Kubota, K.; Tanigawa, T.; Bromet, E.J.; Takahashi, S.; Matsuoka, Y.; Nishi, D.; Nagamine, M.; Harada, N.; et al. The longitudinal mental health impact of Fukushima nuclear disaster exposures and public criticism among power plant workers: The Fukushima NEWS Project study. Psychol. Med. 2016, 46, 3117–3125. [Google Scholar] [CrossRef]
- Murakami, M.; Hirosaki, M.; Suzuki, Y.; Maeda, M.; Yabe, H.; Yasumura, S.; Ohira, T. Reduction of radiation-related anxiety promoted wellbeing after the 2011 disaster: ‘Fukushima Health Management Survey’. J. Radiol. Prot. 2018, 38, 1428–1440. [Google Scholar] [CrossRef]
- Miura, I.; Nagai, M.; Maeda, M.; Harigane, M.; Fujii, S.; Oe, M.; Yabe, H.; Suzuki, Y.; Takahashi, H.; Ohira, T.; et al. Perception of Radiation Risk as a Predictor of Mid-Term Mental Health after a Nuclear Disaster: The Fukushima Health Management Survey. Int. J. Environ. Res. Public Health 2017, 14, 1067. [Google Scholar] [CrossRef]
- Suzuki, Y.; Takebayashi, Y.; Yasumura, S.; Murakami, M.; Harigane, M.; Yabe, H.; Ohira, T.; Ohtsuru, A.; Nakajima, S.; Maeda, M. Changes in Risk Perception of the Health Effects of Radiation and Mental Health Status: The Fukushima Health Management Survey. Int. J. Environ. Res. Public Health 2018, 15, 1219. [Google Scholar] [CrossRef]
- Fukasawa, M.; Kawakami, N.; Umeda, M.; Akiyama, T.; Horikoshi, N.; Yasumura, S.; Yabe, H.; Suzuki, Y.; Bromet, E.J. Longitudinal associations of radiation risk perceptions and mental health among non-evacuee residents of Fukushima prefecture seven years after the nuclear power plant disaster. SSM Popul. Health 2020, 10, 100523. [Google Scholar] [CrossRef]
- Yamanouchi, T.; Hiroshima, M.; Takeuchi, Y.; Sawada, Y.; Takahashi, M.; Amagai, M. Factors Associated with Worsened or Improved Mental Health in the Great East Japan Earthquake Survivors. Arch. Psychiatr. Nurs. 2018, 32, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Imamura, K.; Sekiya, Y.; Asai, Y.; Umeda, M.; Horikoshi, N.; Yasumura, S.; Yabe, H.; Akiyama, T.; Kawakami, N. The effect of a behavioral activation program on improving mental and physical health complaints associated with radiation stress among mothers in Fukushima: A randomized controlled trial. BMC Public Health 2016, 16, 1144. [Google Scholar] [CrossRef] [PubMed]
- Yasumura, S.; Hosoya, M.; Yamashita, S.; Kamiya, K.; Abe, M.; Akashi, M.; Kodama, K.; Ozasa, K.; Fukushima Health Management Survey Group. Study protocol for the Fukushima Health Management Survey. J. Epidemiol. Jpn. Epidemiol. Assoc. 2012, 22, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Yabe, H.; Suzuki, Y.; Mashiko, H.; Nakayama, Y.; Hisata, M.; Niwa, S.; Yasumura, S.; Yamashita, S.; Kamiya, K.; Abe, M.; et al. Psychological distress after the Great East Japan Earthquake and Fukushima Daiichi Nuclear Power Plant accident: Results of a mental health and lifestyle survey through the Fukushima Health Management Survey in FY2011 and FY2012. Fukushima J. Med. Sci. 2014, 60, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Bromet, E.J.; Havenaar, J.M. The Long-Term Mental Health Impacts of the Chernobyl Accident. In Mental Helath and Disasters; Neria, Y., Galea, S., Norris, F.H., Eds.; Cambrige University Press: New York, NY, USA, 2009. [Google Scholar]
- Niagu, A.I.; Noshchenko, A.G.; Loganovskiĭ, K.N. Late effects of psychogenic and radiation factors of the accident at the Chernobyl nuclear power plant on the functional state of human brain. Zhurnal Nevropatol. Psikhiatr. Im. SS Korsakova 1992, 92, 72–77. [Google Scholar]
- Momoi, M.; Murakami, M.; Horikoshi, N.; Maeda, M. Dealing with Community Mental Health post the Fukushima disaster: Lessons learnt for the COVID-19 pandemic. QJM 2020, 113, 787–788. [Google Scholar] [CrossRef]
- Maeda, M.; Oe, M.; Suzuki, Y. Psychosocial effects of the Fukushima disaster and current tasks: Differences between natural and nuclear disasters. J. Natl. Inst. Public Health 2018, 67, 50–58. [Google Scholar]
- Goldmann, E.; Galea, S. Mental health consequences of disasters. Annu. Rev. Public Health 2014, 35, 169–183. [Google Scholar] [CrossRef]
- Ohkuma, R.; Takahashi, J.; Sharshakova, T.; Sachkouskaya, A.; Lyzikov, A.; Voropaev, E.; Ruzanov, D.; Orita, M.; Taira, Y.; Takamura, N. Thirty-two years post-Chernobyl: Risk perception about radiation and health effects among the young generation in Gomel, Republic of Belarus. J. Radiat. Res. 2018, 59, 765–766. [Google Scholar] [CrossRef]
- Bromet, E.J. Emotional consequences of nuclear power plant disasters. Health Phys. 2014, 106, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Kamite, Y. Prejudice and Health Anxiety about Radiation Exposure from Second-Generation Atomic Bomb Survivors: Results from a Qualitative Interview Study. Front. Psychol. 2017, 8, 1462. [Google Scholar] [CrossRef] [PubMed]
- Maeda, M.; Oe, M. The Great East Japan Earthquake: Tsunami and Nuclear Disaster. In Traumatic Stress and Long-Term Recovery Coping with Disasters and Other Negative Life Events; Cherry, K.E., Ed.; Springer International Publishing: Cham, Switzerland, 2015. [Google Scholar]
- Ben-Ezra, M.; Shigemura, J.; Palgi, Y.; Hamama-Raz, Y.; Lavenda, O.; Suzuki, M.; Goodwin, R. From Hiroshima to Fukushima: PTSD symptoms and radiation stigma across regions in Japan. J. Psychiatr. Res. 2015, 60, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Hirosaki, M.; Ohira, T.; Yasumura, S.; Maeda, M.; Yabe, H.; Harigane, M.; Takahashi, H.; Murakami, M.; Suzuki, Y.; Nakano, H.; et al. Lifestyle factors and social ties associated with the frequency of laughter after the Great East Japan Earthquake: Fukushima Health Management Survey. Qual. Life Res. 2018, 27, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Keltner, D.; Bonanno, G.A. A study of laughter and dissociation: Distinct correlates of laughter and smiling during bereavement. J. Pers. Soc. Psychol. 1997, 73, 687–702. [Google Scholar] [CrossRef] [PubMed]
- Lund, D.A.; Utz, R.; Caserta, M.S.; De Vries, B. Humor, laughter, and happiness in the daily lives of recently bereaved spouses. Omega (Westport) 2008, 58, 87–105. [Google Scholar] [CrossRef] [PubMed]
- Morishima, T.; Miyashiro, I.; Inoue, N.; Kitasaka, M.; Akazawa, T.; Higeno, A.; Idota, A.; Sato, A.; Ohira, T.; Sakon, M.; et al. Effects of laughter therapy on quality of life in patients with cancer: An open-label, randomized controlled trial. PLoS ONE 2019, 14, e0219065. [Google Scholar] [CrossRef]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; Ponce De Leon, A.; Dunn, A.L.; Deslandes, A.C.; et al. Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef]
- Wegner, M.; Amatriain-Fernández, S.; Kaulitzky, A.; Murillo-Rodriguez, E.; Machado, S.; Budde, H. Systematic Review of Meta-Analyses: Exercise Effects on Depression in Children and Adolescents. Front. Psychiatry 2020, 11, 81. [Google Scholar] [CrossRef]
- Soysal, P.; Veronese, N.; Thompson, T.; Kahl, K.G.; Fernandes, B.S.; Prina, A.M.; Solmi, M.; Schofield, P.; Koyanagi, A.; Tseng, P.T.; et al. Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2017, 36, 78–87. [Google Scholar] [CrossRef]
- Chang, K.V.; Hsu, T.H.; Wu, W.T.; Huang, K.C.; Han, D.S. Is sarcopenia associated with depression? A systematic review and meta-analysis of observational studies. Age Ageing 2017, 46, 738–746. [Google Scholar] [CrossRef]
- van den Berk-Clark, C.; Secrest, S.; Walls, J.; Hallberg, E.; Lustman, P.J.; Schneider, F.D.; Scherrer, J.F. Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occuring smoking: A systematic review and meta-analysis. Health Psychol. 2018, 37, 407–416. [Google Scholar] [CrossRef]
- Schnurr, P.P.; Green, B.L. Understanding relationships among trauma, posttraumatic stress disorder, and health outcomes. In Trauma and Health: Physical Health Consequences of Exposure to Extreme Stress; Schnurr, P.P., Green, B.L., Eds.; American Psychological Association: Washington, DC, USA, 2004. [Google Scholar]
- Vancampfort, D.; Rosenbaum, S.; Ward, P.B.; Steel, Z.; Lederman, O.; Lamwaka, A.V.; Richards, J.W.; Stubbs, B. Type 2 Diabetes Among People With Posttraumatic Stress Disorder: Systematic Review and Meta-Analysis. Psychosom. Med. 2016, 78, 465–473. [Google Scholar] [CrossRef]
- Emdin, C.A.; Odutayo, A.; Wong, C.X.; Tran, J.; Hsiao, A.J.; Hunn, B.H. Meta-Analysis of Anxiety as a Risk Factor for Cardiovascular Disease. Am. J. Cardiol. 2016, 118, 511–519. [Google Scholar] [CrossRef]
- Takahashi, A.; Ohira, T.; Okazaki, K.; Yasumura, S.; Sakai, A.; Maeda, M.; Yabe, H.; Hosoya, M.; Ohtsuru, A.; Kawasaki, Y.; et al. Effects of Psychological and Lifestyle Factors on Metabolic Syndrome Following the Fukushima Daiichi Nuclear Power Plant Accident: The Fukushima Health Management Survey. J. Atheroscler. Thromb. 2020, 27, 1010–1018. [Google Scholar] [CrossRef] [PubMed]
- Neria, Y.; Nandi, A.; Galea, S. Post-traumatic stress disorder following disasters: A systematic review. Psychol. Med. 2008, 38, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Maeda, M.; Oe, M.; Bromet, E.; Yasumura, S.; Ohto, H. Fukushima, mental health and suicide. J. Epidemiol. Community Health 2016. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. A Framework for Mental Health and Psychosocial Support in Radiological and Nuclear Emergencies; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
| Disasters | TMI (n = 11), Chernobyl (n = 6), Fukushima (n = 18) |
|---|---|
| Study participants (multiple answer allowed) | Residents (n = 20), workers (n = 8), mothers or caregivers with/without their children (n = 8), mental health system clients or patients (n = 2) |
| No. of surveys | Two (n = 19), three (n = 9), four (n = 5), six (n = 1), eight (n = 1) |
| No. of target populations | Lower than 50 (n = 3), between 50 and 999 (n = 21), more than 1000 (n = 11) |
| Presence of control group | Yes (n = 14), no (n = 21) |
| Mental health measure (in Category A, multiple answer allowed) | SCL-90 or SCL-90R (n = 9), IES-R or IES (n =4), K6 (n = 3), PCL-S or PCL-S6 (n = 2) Demoralization score (n = 2), CES-D (n = 2), original distress scale (n = 1), MMPI (n = 1), three-digit ICD-10 code (n = 1), JPSS (n = 1), AIS (n = 1), GHQ-12 (n = 1), emotional symptoms (n = 1), peer relationship (n = 1), victimization (n = 1) |
| Included Studies | Study Design | Selection of Participants | Confounding Variables | Measurement of Exposure | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Outcome Reporting |
|---|---|---|---|---|---|---|---|
| TMI | |||||||
| Bromet 1982 [14] | Cohort study | 2 | 1 | 1 | 2 | 3 | 1 |
| Dohrenwend 1981 [15] | − | − | − | − | − | − | − |
| Goldsteen 1989 [16] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Goldsteen 1982 [17] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Bromet 1982 [18] | Cohort study | 2 | 1 | 1 | 2 | 3 | 1 |
| Dew 1987 [19] | Cohort study | 2 | 1 | 1 | 2 | 3 | 1 |
| Bromet 1990 [20] | Cohort study | 2 | 1 | 1 | 2 | 3 | 1 |
| Dew 1993 [21] | Before–after study | 1 | 1 | 1 | 2 | 1 | 1 |
| Baum 1993 [22] | − | − | − | − | − | − | − |
| Davidson 1991 [23] | Cohort study | 2 | 3 | 1 | 1 | 3 | 1 |
| Prince-Embury 1995 [24] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Chernobyl | |||||||
| Koscheyev 1993 [25] | − | − | − | − | − | − | − |
| Cwikel 1998 [26] | Cohort study | 2 | 1 | 1 | 2 | 3 | 1 |
| Cwikel 1997 [27] | Cohort study | 2 | 1 | 1 | 2 | 3 | 2 |
| Rahu 2014 [28] | Cohort study | 2 | 1 | 1 | 1 | 1 | 1 |
| Fukushima | |||||||
| Ikeda 2019 [29] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Kato 2017 [30] | Before–after study | 1 | 1 | 1 | 2 | 1 | 1 |
| Ikeda 2017 [31] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Sawa 2013 [32] | Cohort study | 2 | 1 | 1 | 2 | 1 | 1 |
| Oe 2017 [33] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Oe 2016 [34] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Oe 2018 [35] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Oe 2019 [36] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Fukasawa 2020 [37] | Before–after study | 1 | 1 | 1 | 2 | 3 | 1 |
| Randomization Process | Deviations from the Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall Risk of Bias |
|---|---|---|---|---|---|
| 1 | 1 | 1 | 3 | 1 | 3 |
| Target Populations | Reasons |
|---|---|
| People in close proximity to extremely stressful events, such as an explosion at an accident site | High-dose radiation exposure, death threats |
| Parents and future parents concerned about the long-term effects of radiation and health of their children | Risks of thyroid cancer, stomach cancer and solid cancer |
| Children from affected areas | May face discrimination, stigmatization and bullying at school |
| People with additional physical health needs, such as ill, older or disabled individuals | High risk of health hazards at the time of evacuation |
| People with a low level of literacy | May struggle to follow advice and instructions provided by risk communicators |
| First responders, health workers, clean-up workers, reporters and other responders working under hazardous or stressful conditions | Risk of high-dose radiation exposure, burdensome workload |
| People in residential facilities/institutions (assisted living, retirement homes, correctional facilities) | May not receive enough information, high risk of health hazards at the time of evacuation |
| Evacuees, as well as the members of hosting communities, whose lives were affected by the evacuation | Drastic changes in living environment |
| People with pre-existing mental health and psychosocial needs | High risk of worsening symptoms |
| Workers (and their families) at the nuclear facility where the accident took place | Risk of high-dose radiation exposure, burdensome workload, discrimination/slurs from the public |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oe, M.; Takebayashi, Y.; Sato, H.; Maeda, M. Mental Health Consequences of the Three Mile Island, Chernobyl, and Fukushima Nuclear Disasters: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 7478. https://doi.org/10.3390/ijerph18147478
Oe M, Takebayashi Y, Sato H, Maeda M. Mental Health Consequences of the Three Mile Island, Chernobyl, and Fukushima Nuclear Disasters: A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(14):7478. https://doi.org/10.3390/ijerph18147478
Chicago/Turabian StyleOe, Misari, Yui Takebayashi, Hideki Sato, and Masaharu Maeda. 2021. "Mental Health Consequences of the Three Mile Island, Chernobyl, and Fukushima Nuclear Disasters: A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 14: 7478. https://doi.org/10.3390/ijerph18147478
APA StyleOe, M., Takebayashi, Y., Sato, H., & Maeda, M. (2021). Mental Health Consequences of the Three Mile Island, Chernobyl, and Fukushima Nuclear Disasters: A Scoping Review. International Journal of Environmental Research and Public Health, 18(14), 7478. https://doi.org/10.3390/ijerph18147478






