Maintaining Quality of Care among Dialysis Patients in Affected Areas after Typhoon Morakot
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
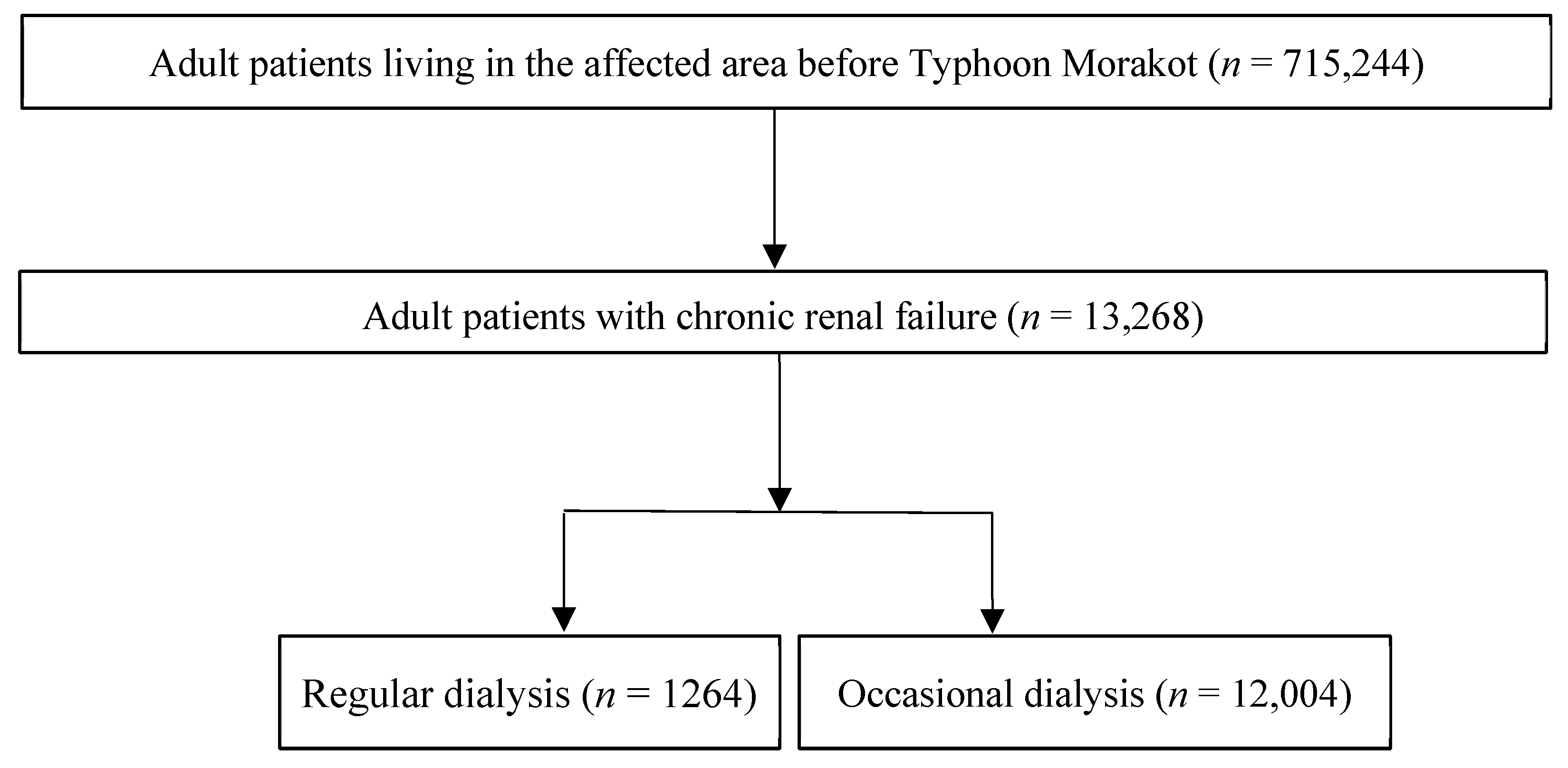
2.2. Study Design
2.3. Social and Spatial Analysis
2.4. Statistical Analysis
2.5. Ethics Issues
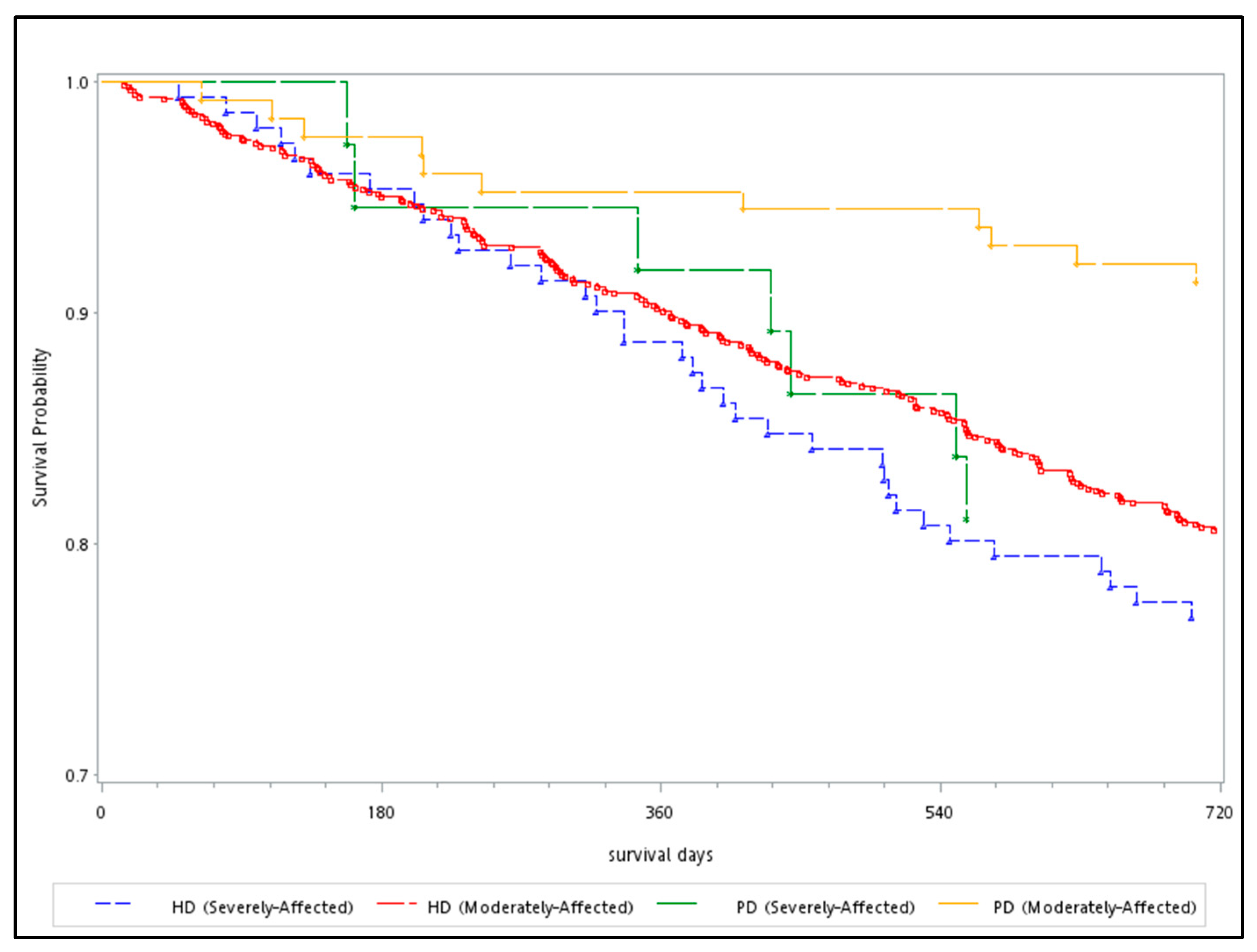
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Diagnosis | ICD-9-CM |
|---|---|
| Hypertension | 401–405 |
| Diabetes mellitus (DM) | 250 |
| Asthma | 493 |
| Chronic heart failure | 428, 410–414 |
| Chronic obstructive pulmonary diseases (COPD) | 491–496, excluding 493, 495 |
| Liver cirrhosis | 571.5 |
| Neoplasm | 140–239 |
| Chronic kidney diseases (CKD) | 585 |
| Acute pulmonary edema | 518.4 |
| Acute ischemic heart diseases (IHD) | 410–414 |
| Acute cerebrovascular diseases (CVD) | 428, 430–437 |
| Heart failure | 428 |
| Peripheral arterial occlusive diseases (PAOD) | 440.0, 440.2, 440.3, 440.8, 440.9, 443, 444.0, 444.2, 444.8, 447.8, and 447.9 |
| Infection with known pathogens | 001–139 |
| Central nervous system (CNS) infection | 320–326 |
| Lower respiratory tract infection | 480–488 |
| Urinary tract infection | 590, 595, 597, 599 |
| Skin and soft tissue infection | 680–686 |
| Trauma and injury | 850–959 |

References
- Costello, A.; Abbas, M.; Allen, A.; Ball, S.; Bell, S.; Bellamy, R.; Friel, S.; Groce, N.; Johnson, A.; Kett, M.; et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 2009, 373, 1693–1733. [Google Scholar] [CrossRef]
- Smith, K.; Woodward, A.; Campbell-Lendrum, D.; Chadee, D.; Honda, Y.; Liu, Q.; Olwoch, J.; Revich, B.; Sauerborn, R. Human Health: Impacts, Adaptation, and Co-Benefits; Cambridge University Press: Cambridge, UK, 2014; pp. 709–754. [Google Scholar]
- Hurricane Katrina Community Advisory Group; Kessler, R.C. Hurricane Katrina’s impact on the care of survivors with chronic medical conditions. J. Gen. Intern. Med. 2007, 22, 1225–1230. [Google Scholar] [PubMed]
- Hales, S.; Edwards, S.J.; Kovats, R.S. Impacts on Health of Climate Extremes. 2003. Available online: https://www.who.int/globalchange/publications/climatechangechap5.pdf (accessed on 6 June 2020).
- Stanke, C.; Murray, V.; Amlot, R.; Nurse, J.; Williams, R. The effects of flooding on mental health: Outcomes and recommendations from a review of the literature. PLoS Curr. 2012, 4, e4f9f1fa9c3cae. [Google Scholar] [CrossRef]
- World Health Organization. Climate Change and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed on 15 March 2020).
- World Health Organization/Regional Office for the Western Pacific. Emergencies and Disasters; Regional Office for The Western Pacific, World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Murakami, N.; Siktel, H.B.; Lucido, D.; Winchester, J.F.; Harbord, N.B. Disaster Preparedness and awareness of patients on hemodialysis after Hurricane Sandy. Clin. J. Am. Soc. Nephrol. CJASN 2015, 10, 1389–1396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraushar, M.L.; Rosenberg, R.E. A Community-led medical response effort in the wake of Hurricane Sandy. Disaster Med. Public Health Prep. 2015, 9, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Lien, C.; Raimo, J.; Abramowitz, J.; Khanijo, S.; Kritharis, A.; Mason, C.; Jarmon, C.H.; Nash, I.S.; Carney, M.T. Community healthcare delivery post-Hurricane Sandy: Lessons from a mobile health unit. J. Community Health 2014, 39, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Tung Bui, S.C. Michael Sovereign, Negotiation Issues in Multinational Humanitarian Assistance/Disaster Relief. In Proceedings of the 32nd Hawaii International Conference on System Sciences, Maui, HI, USA, 5–8 June 1999. [Google Scholar]
- Sharma, A.J.; Weiss, E.C.; Young, S.L.; Stephens, K.; Ratard, R.; Straif-Bourgeois, S.; Sokol, T.M.; Vranken, P.; Rubin, C.H. Chronic disease and related conditions at emergency treatment facilities in the New Orleans area after Hurricane Katrina. Disaster Med. Public Health Prep. 2008, 2, 27–32. [Google Scholar] [CrossRef]
- Anderson, A.H.; Cohen, A.J.; Kutner, N.G.; Kopp, J.B.; Kimmel, P.L.; Muntner, P. Missed dialysis sessions and hospitalization in hemodialysis patients after Hurricane Katrina. Kidney Int. 2009, 75, 1202–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelman, J.; Finne, K.; Bogdanov, A.; Worrall, C.; Margolis, G.; Rising, K.; MaCurdy, T.E.; Lurie, N. Dialysis care and death following Hurricane Sandy. Am. J. Kidney Dis. 2015, 65, 109–115. [Google Scholar] [CrossRef]
- Davis, M.; Kopp, J.B. Preparing for Disasters for Patients on Dialysis. Clin. J. Am. Soc. Nephrol. CJASN 2015, 10, 1316–1317. [Google Scholar] [CrossRef] [Green Version]
- Davis, J.R.; Wilson, S.; Brock-Martin, A.; Glover, S.; Svendsen, E.R. The impact of disasters on populations with health and health care disparities. Disaster Med. Public Health Prep. 2010, 4, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Kaohsiung City Office. The Official List of Survivors in Kaohsiung during the Typhoon Morakot. Available online: http://88taiwan.blogspot.tw/2009/08/0815.html (accessed on 12 June 2019).
- National Science and Technology Center for Disaster Reduction. National Science and Technology Center for Disaster Reduction Anual Report, 2010; National Science and Technology Center for Disaster Reduction: New Taipei City, Taiwan, 2010.
- Ministry of Health and Welfare. Emergency Medical Response for Typhoon Morakot. Available online: https://www.mohw.gov.tw/cp-3162-27392-1.html (accessed on 1 June 2019).
- National Science and Technology Center for Disaster Reduction. Disaster Survey and Analysis of Morakot Typhoon; Reduction, National Science and Technology Center for Disaster Reduction: New Taipei City, Taiwan, 2013.
- Lee, T.C.; Yang, C.L.; Wang, T.M. Population Aging and NHI Expenditures in Taiwan. J. Popul. Stud. 2011, 43, 1–35. [Google Scholar]
- Pan, Y.J.; Yeh, L.L.; Chan, H.Y.; Chang, C.K. Transformation of excess mortality in people with schizophrenia and bipolar disorder in Taiwan. Psychol. Med. 2017, 47, 2483–2493. [Google Scholar] [CrossRef]
- Chiu, Y.W.; Wu, C.S.; Chen, P.C.; Wei, Y.C.; Hsu, L.Y.; Wang, S.H. Risk of acute mesenteric ischemia in patients with diabetes: A population-based cohort study in Taiwan. Atherosclerosis 2020, 296, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Taiwan Society of Nephrology. Annual Report on Kidney Disease in Taiwan; Taiwan Society of Nephrology: Taipei City, Taiwan, 2014. [Google Scholar]
- Center for Survey Research, Academia Sinica. Taiwan Social Change Survey. Available online: http://www2.ios.sinica.edu.tw/sc/en/home2.php (accessed on 6 November 2019).
- World Medical Association. World Medical Association Declaration of Taipei on Ethical Considerations regarding Health Databases and Biobanks. Available online: https://www.wma.net/policies-post/wma-declaration-of-taipei-on-ethical-considerations-regarding-health-databases-and-biobanks/ (accessed on 6 November 2019).
- Howard, D.; Zhang, R.; Huang, Y.; Kutner, N. Hospitalization rates among dialysis patients during Hurricane Katrina. Prehospital Disaster Med. 2012, 27, 325–329. [Google Scholar] [CrossRef] [PubMed]
- The United States Renal Data System (USRDS). USRDS 2007 Annual Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2007.
- Ministry of the Interior, Taiwan. Disaster Prevention and Protection Act. Available online: https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=D0120014 (accessed on 15 August 2020).
- Aitsi-Selmi, A.; Murray, V. The Sendai framework: Disaster risk reduction through a health lens. Bull. World Health Organ. 2015, 93, 362. [Google Scholar] [CrossRef] [PubMed]
- Ministry of the Interior, Taiwan. Toward a Sustainable Taiwan: Summary National Spatial Plan. Taiwan. Available online: https://www.cpami.gov.tw/filesys/file/rp6/rp1081203e.pdf (accessed on 15 August 2020).
- United Nations. United Nations Sustainable Development Goals. Available online: https://sdgs.un.org/goals (accessed on 15 August 2020).
- Ministry of Health and Welfare, Taiwan. Policy Implications of the Health Effects of Climate Change; Ministry of Health and Welfare, Taiwan: Taipei, Taiwan, 2014.
- Shih, H.I.; Chao, T.Y.; Huang, Y.T.; Tu, Y.F.; Sung, T.C.; Wang, J.D.; Chang, C.M. Increased Medical Visits and Mortality among Adults with Cardiovascular Diseases in Severely Affected Areas after Typhoon Morakot. Int. J. Environ. Res. Public Health 2020, 17, 6531. [Google Scholar] [CrossRef] [PubMed]
- Vanholder, R.C.; Van Biesen, W.A.; Sever, M.S. Hurricane Katrina and chronic dialysis patients: Better tidings than originally feared? Kidney Int. 2009, 76, 687–689. [Google Scholar] [CrossRef]
- Kopp, J.B.; Ball, L.K.; Cohen, A.; Kenney, R.J.; Lempert, K.D.; Miller, P.E.; Muntner, P.; Qureshi, N.; Yelton, S.A. Kidney patient care in disasters: Emergency planning for patients and dialysis facilities. Clin. J. Am. Soc. Nephrol. CJASN 2007, 2, 825–838. [Google Scholar] [CrossRef] [PubMed]
- Plough, A.; Fielding, J.E.; Chandra, A.; Williams, M.; Eisenman, D.; Wells, K.B.; Law, G.Y.; Fogleman, S.; Magana, A. Building community disaster resilience: Perspectives from a large urban county department of public health. Am. J. Public Health 2013, 103, 1190–1197. [Google Scholar] [CrossRef]
- Liao, P.A.; Chang, H.H.; Sun, L.C. National Health Insurance program and life satisfaction of the elderly. Aging Ment. Health 2012, 16, 983–992. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Yip, W.; Chang, M.C.; Lin, H.S.; Lee, S.D.; Chiu, Y.L.; Lin, Y.H. The effects of Taiwan’s National Health Insurance on access and health status of the elderly. Health Econ. 2007, 16, 223–242. [Google Scholar] [CrossRef] [PubMed]
- Liao, P.A.; Chang, H.H.; Yang, F.A. Does the universal health insurance program affect urban-rural differences in health service utilization among the elderly? Evidence from a longitudinal study in taiwan. J. Rural Health 2012, 28, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nicholas, S.B.; Kalantar-Zadeh, K.; Norris, K.C. Socioeconomic disparities in chronic kidney disease. Adv. Chronic Kidney Dis. 2015, 22, 6–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asaria, M.; Ali, S.; Doran, T.; Ferguson, B.; Fleetcroft, R.; Goddard, M.; Goldblatt, P.; Laudicella, M.; Raine, R.; Cookson, R. How a universal health system reduces inequalities: Lessons from England. J. Epidemiol. Community Health 2016, 70, 637–643. [Google Scholar] [CrossRef]
- World Health Organization. Commission on Social Determinants of Health–Final Report; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Veugelers, P.J.; Yip, A.M. Socioeconomic disparities in health care use: Does universal coverage reduce inequalities in health? J. Epidemiol. Community Health 2003, 57, 424–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129 (Suppl. 2), 19–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hammond, G.; Luke, A.A.; Elson, L.; Towfighi, A.; Joynt Maddox, K.E. Urban-rural inequities in acute stroke care and in-hospital mortality. Stroke 2020, 51, 2131–2138. [Google Scholar] [CrossRef]
- Kapral, M.K.; Hall, R.; Gozdyra, P.; Yu, A.Y.X.; Jin, A.Y.; Martin, C.; Silver, F.L.; Swartz, R.H.; Manuel, D.G.; Fang, J.; et al. Geographic access to stroke care services in rural communities in Ontario, Canada. Can. J. Neurol. Sci. 2020, 47, 301–308. [Google Scholar] [CrossRef]
| Characteristics | Adult Patients with ESRD (2008/1–2009/7) n = 13,268 | ||||
|---|---|---|---|---|---|
| Regular Dialysis (n = 1264) | |||||
| Moderately Affected Areas | Severely Affected Areas | ||||
| (n = 1076) | (n = 188) | Chi-Squared Test | |||
| No. | % | No. | % | p-Value | |
| Sex | |||||
| Male | 496 | 46.10 | 79 | 42.02 | 0.30 |
| Age (years) | |||||
| Mean (SD) * | 62.37 (12.45) | 62.69, 13.27 | |||
| Age group | |||||
| Elderly | 481 | 44.70 | 94 | 50.00 | 0.18 |
| Socioeconomic status (USD/month) | |||||
| Poor < 750 USD | 647 | 60.13 | 139 | 73.94 | 0.0014 |
| Location | |||||
| Urban | 245 | 22.77 | 0 | 0.00 | <0.0001 |
| Suburban | 586 | 54.46 | 73 | 38.83 | |
| Rural | 245 | 22.77 | 115 | 61.17 | |
| CCI † | |||||
| 0 | - | - | - | - | |
| 1–2 | 309 | 28.72 | 44 | 23.40 | 0.13 |
| >2 | 767 | 71.28 | 144 | 76.60 | |
| Underlying diseases | |||||
| DM | 352 | 32.71 | 79 | 42.02 | 0.01 |
| Hypertension | 309 | 28.72 | 82 | 43.62 | <0.0001 |
| Heart disease | 260 | 24.16 | 36 | 19.15 | 0.13 |
| COPD and asthma | 47 | 4.37 | 9 | 4.79 | 0.80 |
| Liver cirrhosis | 32 | 2.97 | 6 | 3.19 | 0.87 |
| Neoplasms | 111 | 10.32 | 15 | 7.98 | 0.32 |
| Dialysis | |||||
| Hemodialysis | 949 | 88.20 | 151 | 80.32 | 0.003 |
| Peritoneal dialysis | 127 | 11.80 | 37 | 19.68 | |
| Characteristics | Regular Dialysis Patients before the Disaster (n = 1264) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderately Affected Areas (n = 1076) | Severely Affected Areas (n = 88) | |||||||||||
| Before Aug/06/2008–Aug/07/2009 | After Aug/08/2009–Aug/07/2010 | Before Aug/06/2008–Aug/07/2009 | After Aug/08/2009–Aug/07/2010 | |||||||||
| No. | Person-Year | Incidence † | No. | Person-Year | Incidence † | No. | Person-Year | Incidence † | No. | Person-Year | Incidence † | |
| Acute pulmonary edema | 44 | 1035 | 42.51 | 14 | 946 | 14.80 | 10 | 183 | 54.64 | 3 | 165 | 18.17 |
| Acute ischemic heart diseases | 116 | 867 | 133.79 | 81 | 719 | 112.61 | 27 | 150 | 180.00 | 13 | 117 | 111.12 |
| Acute cerebrovascular diseases | 113 | 888 | 127.25 | 83 | 745 | 111.44 | 26 | 163 | 159.51 | 17 | 134 | 127.04 |
| Infection | 274 | 628 | 436.31 | 150 | 340 | 440.78 | 43 | 104 | 413.46 | 25 | 59 | 424.64 |
| PAOD | 6 | 1070 | 5.61 | 5 | 1015 | 4.92 | 2 | 188 | 10.64 | 0 | 178 | 0.00 |
| Injury (800–859) | 169 | 907 | 186.33 | 118 | 695 | 169.72 | 22 | 160 | 137.50 | 19 | 134 | 141.53 |
| Survival, Years | National Dialysis Data | Moderately Affected Areas (n = 1076) | Severely Affected Areas (n = 188) | National Dialysis Data | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yearly | <1 Year (2009/08–2010/07) | 1–2 Year (2010/08–2011/07) | <1 Year (2009/08–2010/07) | 1–2 Year (2010/08–2011/07) | Yearly | |||||||||||
| Mortality † | (n = 100) | (n = 95) | (n = 20) | Mortality † | Mortality † | |||||||||||
| 2008 | No | Cases | Mortality † | No | Cases | Mortality † | No | Cases | Mortality † | No | Cases | Mortality † | 2009 | 2010 | 2011 | |
| Sex | ||||||||||||||||
| Female | 109 | 44 | 580 | 75.9 | 44 | 536 | 82.1 | 10 | 109 | 91.7 | 10 | 99 | 101.0 | 105 | 112 | 115 |
| Male | 126 | 56 | 496 | 112.9 | 51 | 440 | 115.9 | 10 | 79 | 126.6 | 12 | 69 | 173.9 | 117 | 122 | 126 |
| Age group | ||||||||||||||||
| 20–44 | 32 | 1 | 92 | 10.9 | 0 | 91 | - | 3 | 20 | 150.0 | 0 | 17 | - | 26 | 29 | 31 |
| 45–64 | 67 | 27 | 503 | 53.7 | 36 | 476 | 75.6 | 6 | 74 | 81.1 | 6 | 68 | 88.2 | 62 | 66 | 66 |
| 65–74 | 133 | 40 | 312 | 128.2 | 27 | 272 | 99.3 | 7 | 60 | 116.7 | 9 | 53 | 169.8 | 123 | 126 | 128 |
| 75+ | 251 | 32 | 169 | 189.3 | 32 | 137 | 233.6 | 4 | 34 | 117.6 | 7 | 30 | 233.3 | 238 | 244 | 254 |
| Females, age group | ||||||||||||||||
| 20–44 | 26 | 0 | 43 | - | 0 | 43 | - | 1 | 10 | 100.0 | 0 | 9 | - | 22 | 28 | 31 |
| 45–64 | 54 | 16 | 279 | 57.3 | 16 | 263 | 60.8 | 2 | 39 | 51.3 | 3 | 37 | 81.1 | 49 | 55 | 55 |
| 65–74 | 121 | 16 | 170 | 94.1 | 10 | 154 | 64.9 | 4 | 37 | 108.1 | 3 | 33 | 90.9 | 110 | 114 | 116 |
| 75+ | 238 | 12 | 88 | 136.4 | 18 | 76 | 236.8 | 3 | 23 | 130.4 | 4 | 20 | 200.0 | 231 | 233 | 236 |
| Males, age group | ||||||||||||||||
| 20–44 | 38 | 1 | 49 | 20.4 | 0 | 48 | - | 2 | 10 | 200.0 | 0 | 8 | - | 30 | 29 | 31 |
| 45–64 | 81 | 11 | 224 | 49.1 | 20 | 213 | 93.9 | 4 | 35 | 114.3 | 3 | 31 | 96.8 | 74 | 76 | 75 |
| 65–74 | 148 | 24 | 142 | 169.0 | 17 | 118 | 144.1 | 3 | 23 | 130.4 | 6 | 20 | 300.0 | 139 | 141 | 141 |
| 75+ | 267 | 20 | 81 | 246.9 | 14 | 61 | 229.5 | 1 | 11 | 90.9 | 3 | 10 | 300.0 | 247 | 258 | 277 |
| Moderately Affected Areas † (n = 1076) | Severely Affected Areas † (n = 188) | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis Backward Elimination | Univariate Analysis | Multivariate Analysis Backward Elimination | |||||
| HR | 95% CI | aHR | 95% CI | HR | 95% CI | aHR | 95% CI | |
| Location (Ref = Nonrural) | ||||||||
| Rural | 1.15 | 0.84–1.56 | 0.85 | 0.48–1.51 | ||||
| Diabetes (Ref = No) | ||||||||
| Yes | 1.58 * | 1.21–2.07 | 1.58 * | 1.20–2.08 | 1.05 | 0.59–1.86 | ||
| Hypertension (Ref = No) | ||||||||
| Yes | 1.08 | 0.81–1.45 | 0.92 | 0.52–1.63 | ||||
| Arrhythmia history (Ref = No) | ||||||||
| Yes | 1.43 | 0.78–2.63 | 0.79 | 0.11–5.76 | ||||
| Cerebrovascular disease events (Ref = No) | ||||||||
| Yes | 2.06 * | 1.48–2.88 | 1.58 * | 1.12–2.21 | 4.45 * | 2.26–8.76 | 4.52 * | 2.29–8.92 |
| Ischemic heart disease events (Ref = No) | ||||||||
| Yes | 1.51 * | 1.13–2.01 | 1.32 | 0.67–2.59 | ||||
| PAOD (Ref = No) | ||||||||
| Yes | 1.55 | 0.77–3.14 | — | — | ||||
| Two cardiovascular conditions (Ref = No) | ||||||||
| Yes | 1.51 * | 1.12–2.02 | 1.60 | 0.86–2.98 | ||||
| >2 cardiovascular conditions (Ref = No) | ||||||||
| Yes | 1.75 * | 1.17–2.62 | 2.42 | 0.87–6.74 | ||||
| COPD and asthma (Ref = No) | ||||||||
| Yes | 2.57 * | 1.62–4.07 | 1.99 * | 1.25–3.18 | 2.24 | 0.80–6.24 | ||
| Liver cirrhosis (Ref = No) | ||||||||
| Yes | 1.74 | 0.92–3.28 | 1.50 | 0.36–6.18 | ||||
| Neoplasms (Ref = No) | ||||||||
| Yes | 1.02 | 0.66–1.57 | 1.00 | 0.36–2.78 | ||||
| Injury 800–859 (Ref = No) | ||||||||
| Yes | 0.79 | 0.48–1.27 | 1.29 | 0.47–3.60 | ||||
| Infection (Ref = No) | ||||||||
| Yes | 1.22 | 0.86–1.74 | 1.35 | 0.60–3.00 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-M.; Chao, T.-Y.S.; Huang, Y.-T.; Tu, Y.-F.; Sung, T.-C.; Wang, J.-D.; Shih, H.-I. Maintaining Quality of Care among Dialysis Patients in Affected Areas after Typhoon Morakot. Int. J. Environ. Res. Public Health 2021, 18, 7400. https://doi.org/10.3390/ijerph18147400
Chang C-M, Chao T-YS, Huang Y-T, Tu Y-F, Sung T-C, Wang J-D, Shih H-I. Maintaining Quality of Care among Dialysis Patients in Affected Areas after Typhoon Morakot. International Journal of Environmental Research and Public Health. 2021; 18(14):7400. https://doi.org/10.3390/ijerph18147400
Chicago/Turabian StyleChang, Chia-Ming, Tzu-Yuan Stessa Chao, Yi-Ting Huang, Yi-Fang Tu, Tzu-Ching Sung, Jung-Der Wang, and Hsin-I Shih. 2021. "Maintaining Quality of Care among Dialysis Patients in Affected Areas after Typhoon Morakot" International Journal of Environmental Research and Public Health 18, no. 14: 7400. https://doi.org/10.3390/ijerph18147400
APA StyleChang, C.-M., Chao, T.-Y. S., Huang, Y.-T., Tu, Y.-F., Sung, T.-C., Wang, J.-D., & Shih, H.-I. (2021). Maintaining Quality of Care among Dialysis Patients in Affected Areas after Typhoon Morakot. International Journal of Environmental Research and Public Health, 18(14), 7400. https://doi.org/10.3390/ijerph18147400






