Interorganizational Networks in Physical Activity Promotion: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy and Selection Process
2.3. Data Extraction
2.4. Quality Assessment
3. Results
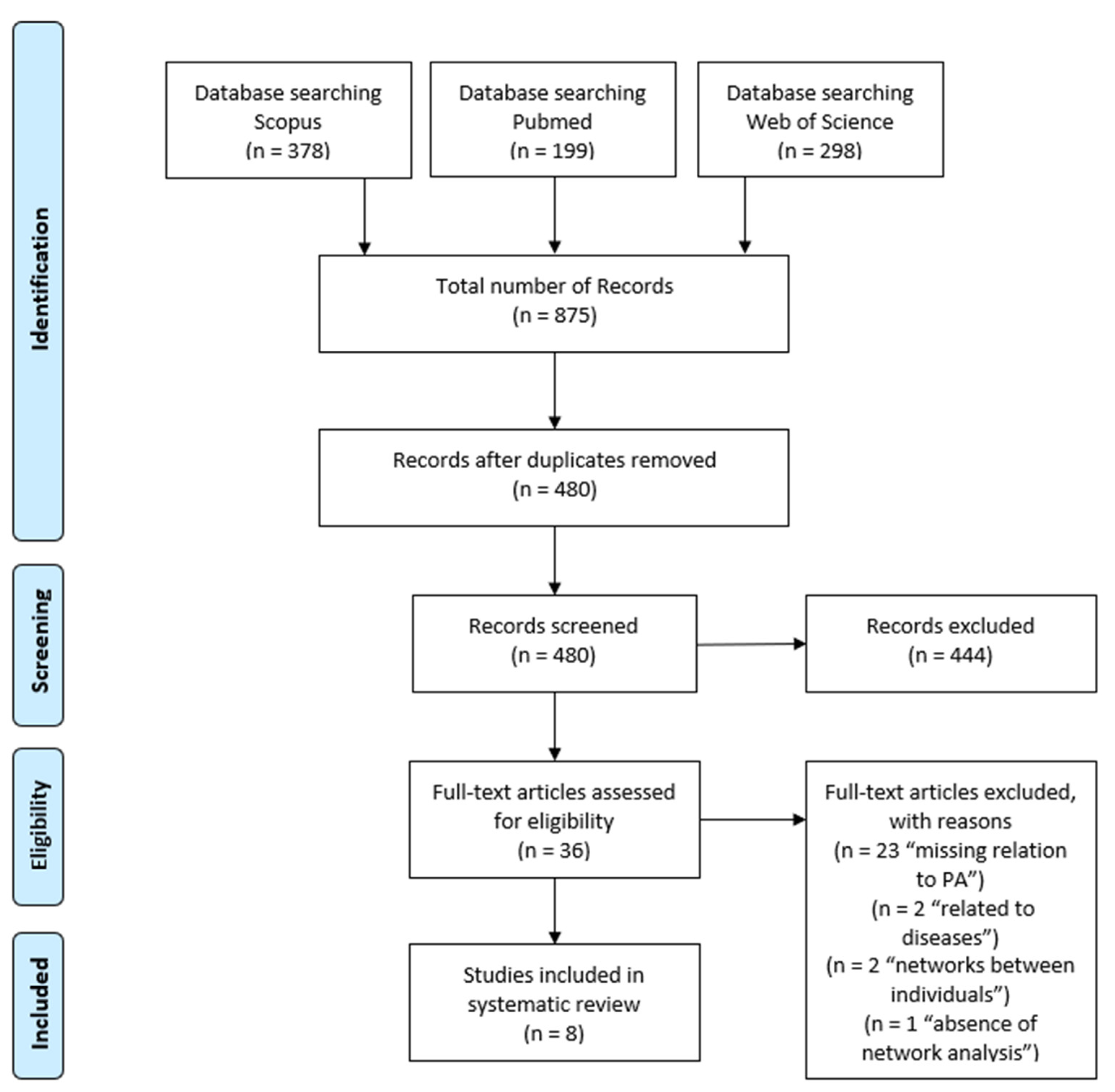
3.1. Selection Process
3.2. Study and Network Characteristics
3.3. Quality Assessment
3.4. Key Findings
3.4.1. Network Level
3.4.2. Individual Level
3.4.3. Subgraph Level
3.4.4. Determinants of Network Outcome
4. Discussion
Limitations
5. Practical Implications
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [Green Version]
- Yang, L.; Cao, C.; Kantor, E.D.; Nguyen, L.H.; Zheng, X.; Park, Y.; Giovannucci, E.L.; Matthews, C.E.; Colditz, G.A.; Cao, Y. Trends in sedentary behavior among the US population, 2001–2016. JAMA 2019, 16, 1587–1597. [Google Scholar] [CrossRef]
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- Trost, S.G.; Owen, N.; Bauman, A.E.; Sallis, J.F.; Brown, W. Correlates of adults’ participation in physical activity: Review and update. Med. Sci. Sports Exerc. 2002, 34, 1996–2001. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.R.; Nicol, C.W.; Bredin, S.S.D. Health benefits of physical activity: The evidence. CMAJ 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pratt, M.; Ramirez Varela, A.; Salvo, D.; Kohl Iii, H.W.; Ding, D. Attacking the pandemic of physical inactivity: What is holding us back? Br. J. Sports Med. 2020, 13, 760–762. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020; ISBN 9789240015128. [Google Scholar]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 1, 42. [Google Scholar] [CrossRef] [Green Version]
- Valente, T.W.; Pumpuang, P. Identifying opinion leaders to promote behavior change. Health Educ. Behav. 2007, 6, 881–896. [Google Scholar] [CrossRef]
- World Health Organization. More Active People for a Healthier World: Global Action Plan on Physical Activity 2018–2030; World Health Organization: Geneva, Switzerland, 2018; ISBN 9789241514187. [Google Scholar]
- Rhodes, R.E.; McEwan, D.; Rebar, A.L. Theories of physical activity behaviour change: A history and synthesis of approaches. Psychol. Sport Exerc. 2019, 42, 100–109. [Google Scholar] [CrossRef]
- Kok, G.; Gurabardhi, Z.; Gottlieb, N.H.; Zijlstra, F.R.H. Influencing organizations to promote health: Applying stakeholder theory. Health Educ. Behav. 2015, 42, 123S–132S. [Google Scholar] [CrossRef]
- Hoeijmakers, M.; de Leeuw, E.; Kenis, P.; de Vries, N.K. Local health policy development processes in the Netherlands: An expanded toolbox for health promotion. Health Promot. Int. 2007, 22, 112–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. The Public Health System and the 10 Essential Public Health Services. Available online: https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html (accessed on 15 June 2021).
- Bevc, C.A.; Retrum, J.H.; Varda, D.M. Patterns in PARTNERing across Public Health Collaboratives. Int. J. Environ. Res. Public Health 2015, 12, 12412–12425. [Google Scholar] [CrossRef] [Green Version]
- Litt, J.; Varda, D.; Reed, H.; Retrum, J.; Tabak, R.; Gustat, J.; O’Hara Tompkins, N. How to identify success among networks that promote active living. Am. J. Public Health 2015, 11, 2298–2305. [Google Scholar] [CrossRef]
- Contandriopoulos, D.; Hanusaik, N.; Maximova, K.; Paradis, G.; O’Loughlin, J.L. Mapping Collaborative Relations among Canada’s Chronic Disease Prevention Organizations. Healthc. Policy 2016, 12, 101–115. [Google Scholar] [CrossRef] [Green Version]
- Wäsche, H.; Gerke, A. Interorganisational network governance in sport. In Research Handbook on Sport Governance; Winand, M., Anagnostopoulos, C., Eds.; Edward Elgar Publishing: Cheltenham, UK, 2019; pp. 202–215. [Google Scholar]
- Mäkinen, J.T.; Lämsä, J.; Lehtonen, K. The analysis of structural changes in Finnish sport policy network from 1989 to 2017. Int. J. Sport Policy 2019, 11, 561–583. [Google Scholar] [CrossRef]
- Provan, K.G.; Kenis, P. Modes of Network Governance: Structure, Management, and Effectiveness. J. Public Adm. Res. Theory 2007, 18, 229–252. [Google Scholar] [CrossRef] [Green Version]
- Naraine, M.; Schenk, J.; Parent, M.M. Coordination in international and domestic sports events: Examining stakeholder network governance. J. Sport Manag. 2016, 5, 521–537. [Google Scholar] [CrossRef]
- Wäsche, H.; Dickson, G.; Woll, A.; Brandes, U. Social network analysis in sport research: An emerging paradigm. Eur. J. Sport Soc. 2017, 14, 138–165. [Google Scholar] [CrossRef]
- Wäsche, H. Interorganizational cooperation in sport tourism: A social network analysis. Sport Manag. Rev. 2015, 4, 542–554. [Google Scholar] [CrossRef]
- Luke, D.A.; Harris, J.K. Network analysis in public health: History, methods, and applications. Annu. Rev. Public Health 2007, 28, 69–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chambers, D.; Wilson, P.; Thompson, C.; Harden, M. Social network analysis in healthcare settings: A systematic scoping review. PLoS ONE 2012, 8, e41911. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.; Carrington, P.J. The SAGE Handbook of Social Network Analysis; SAGE Publications: Newbury Park, CA, USA, 2011; ISBN 101847873952. [Google Scholar]
- Prell, C. Social Network Analysis: History, Theory and Methodology; SAGE Publications: Los Angeles, CA, USA, 2011; ISBN 9781446254103. [Google Scholar]
- Kadushin, C. Understanding Social Networks: Theories, Concepts, and Findings; Oxford University Press: Oxford, UK, 2012; ISBN 9780195379471. [Google Scholar]
- Wasserman, S.; Faust, K. Social Network Analysis: Methods and Applications; Cambridge University Press: Cambridge, UK, 1994; ISBN 100521387078. [Google Scholar]
- Borgatti, S.P.; Everett, M.G.; Johnson, J.C. Analyzing Social Networks; SAGE Publications: Los Angeles, CA, USA, 2013; p. 296. ISBN 101526404109. [Google Scholar]
- Provan, K.G.; Fish, A.; Sydow, J. Interorganizational Networks at the Network Level: A Review of the Empirical Literature on Whole Networks. J. Manag. 2007, 33, 479–516. [Google Scholar] [CrossRef] [Green Version]
- Kenis, P.; Knoke, D. How Organizational Field Networks Shape Interorganizational Tie-Formation Rates. Acad. Manag. Rev. 2002, 27, 275–293. [Google Scholar] [CrossRef] [Green Version]
- Harris, J.K.; Luke, D.A.; Burke, R.C.; Mueller, N.B. Seeing the forest and the trees: Using network analysis to develop an organizational blueprint of state tobacco control systems. Soc. Sci. Med. 2008, 67, 1669–1678. [Google Scholar] [CrossRef]
- Das, K.; Samanta, S.; Pal, M. Study on centrality measures in social networks: A survey. Soc. Netw. Anal. Min. 2018, 8, 13. [Google Scholar] [CrossRef]
- Provan, K.G.; Harvey, J.; de Zapien, J.G. Network structure and attitudes toward collaboration in a community partnership for diabetes control on the US-Mexican border. J. Health Organ. Manag. 2005, 19, 504–518. [Google Scholar] [CrossRef]
- Freeman, L.C. Centrality in social networks: Conceptual clarification. Soc. Netw. 1979, 1, 215–239. [Google Scholar] [CrossRef] [Green Version]
- Borgatti, S.P.; Jones, C.; Everett, M.G. Network measures of social capital. Connections 1998, 21, 27–36. [Google Scholar]
- Hawe, P.; Webster, C.; Shiell, A. A glossary of terms for navigating the field of social network analysis. J. Epidemiol. Community Health 2004, 58, 971–975. [Google Scholar] [CrossRef]
- Borgatti, S.P.; Everett, M.G.; Freeman, L.C. UCINET 6 for Windows: Software for Social Network Analysis; Analytic Technologies: Harvard, MA, USA, 2002. [Google Scholar]
- Borgatti, S.P. NetDraw: Graph Visualization Software; Analytic Technologies: Harvard, MA, USA, 2002. [Google Scholar]
- Snijders, T.A. Statistical Models for Social Networks. Annu. Rev. Sociol. 2011, 37, 131–153. [Google Scholar] [CrossRef]
- Glegg, S.M.N.; Jenkins, E.; Kothari, A. How the study of networks informs knowledge translation and implementation: A scoping review. Implement. Sci. 2019, 14, 34–61. [Google Scholar] [CrossRef]
- Valente, T.W.; Palinkas, L.A.; Czaja, S.; Chu, K.-H.; Brown, C.H. Social network analysis for program implementation. PLoS ONE 2015, 10, e0131712. [Google Scholar] [CrossRef] [Green Version]
- Valente, T.W.; Fujimoto, K. Bridging: Locating critical connectors in a network. Soc. Netw. 2010, 32, 212–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Provan, K.G.; Veazie, M.A.; Staten, L.K.; Teufel-Shone, N.I. The Use of Network Analysis to Strengthen Community Partnerships. Public Adm. Rev. 2005, 65, 603–613. [Google Scholar] [CrossRef]
- Honeycutt, T.C.; Strong, D.A. Using Social Network Analysis to Predict Early Collaboration Within Health Advocacy Coalitions. Am. J. Eval. 2012, 33, 221–239. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung, and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 15 June 2021).
- Spencer, L.; Ritchie, J.; Lewis, J.; Dillon, L. Quality in Qualitative Evaluation: A Framework for Assessing Research Evidence: A Quality Framework; Government Chief Social Researcher’s Office: London, UK, 2003; ISBN 07115044658.
- Hoy, D.; Brooks, P.; Woolf, A.; Blyth, F.; March, L.; Bain, C.; Baker, P.; Smith, E.; Buchbinder, R. Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 2012, 65, 934–939. [Google Scholar] [CrossRef] [PubMed]
- Critical Appraisal Skills Programme: CASP Qualitative Research Checklist. Available online: https://casp-uk.b-cdn.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf (accessed on 15 June 2021).
- De Brún, A.; McAuliffe, E. Social Network Analysis as a Methodological Approach to Explore Health Systems: A Case Study Exploring Support among Senior Managers/Executives in a Hospital Network. Int. J. Environ. Res. Public Health 2018, 15, 511. [Google Scholar] [CrossRef] [Green Version]
- Kossinets, G. Effects of missing data in social networks. Soc. Netw. 2006, 28, 247–268. [Google Scholar] [CrossRef] [Green Version]
- Smith, J.A.; Moody, J.; Morgan, J. Network sampling coverage II: The effect of non-random missing data on network measurement. Soc. Netw. 2017, 48, 78–99. [Google Scholar] [CrossRef] [Green Version]
- Smith, J.A.; Moody, J. Structural Effects of Network Sampling Coverage I: Nodes Missing at Random1. Soc. Netw. 2013, 35, 652–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meisel, J.D.; Sarmiento, O.L.; Montes, F.; Martinez, E.O.; Lemoine, P.D.; Valdivia, J.A.; Brownson, R.C.; Zarama, R. Network analysis of Bogotá’s Ciclovia Recreativa, a self-organized multisectorial community program to promote physical activity in a middle-income country. Am. J. Health Promot. 2014, 28, e127–e136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parra, D.C.; Dauti, M.; Harris, J.K.; Reyes, L.; Malta, D.C.; Brownson, R.C.; Quintero, M.A.; Pratt, M. How does network structure affect partnerships for promoting physical activity? Evidence from Brazil and Colombia. Soc. Sci. Med. 2011, 73, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Buchthal, O.V.; Taniguchi, N.; Iskandar, L.; Maddock, J. Assessing State-Level Active Living Promotion Using Network Analysis. J. Phys. Act. Health 2013, 10, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Yessis, J.; Riley, B.; Stockton, L.; Brodovsky, S.; von Sychowski, S. Interorganizational relationships in the Heart and Stroke Foundation’s Spark Together for Healthy Kids™: Insights from using network analysis. Health Educ. Behav. 2013, 40, 43S–50S. [Google Scholar] [CrossRef]
- Loitz, C.C.; Stearns, J.A.; Fraser, S.N.; Storey, K.; Spence, J.C. Network analysis of inter-organizational relationships and policy use among active living organizations in Alberta, Canada. BMC Public Health 2017, 17, 649. [Google Scholar] [CrossRef]
- Slonim, A.B.; Callaghan, C.; Daily, L.; Leonard, B.A.; Wheeler, F.C.; Gollmar, C.W.; Young, W.F. Recommendations for integration of chronic disease programs: Are your programs linked? Prev. Chronic Dis. 2007, 4, A34. [Google Scholar]
- Brownson, R.C.; Parra, D.C.; Dauti, M.; Harris, J.K.; Hallal, P.C.; Hoehner, C.; Malta, D.C.; Reis, R.S.; Ramos, L.R.; Ribeiro, I.C.; et al. Assembling the Puzzle for Promoting Physical Activity in Brazil: A Social Network Analysis. J. Phys. Act. Health 2010, 7, 242–252. [Google Scholar] [CrossRef]
- Barnes, M.; Maclean, J.; Cousens, L. Understanding the structure of community collaboration: The case of one Canadian health promotion network. Health Promot. Int. 2010, 25, 238–247. [Google Scholar] [CrossRef]
- Andrade, D.R.; Garcia, L.M.T.; Perez, D.C.P. Local collaborations for physical activity promotion: A network analysis. Cad. Saude Publica 2018, 34, e00127517. [Google Scholar] [CrossRef]
- Mays, G.P.; Hogg, R.A.; Castellanos-Cruz, D.M.; Hoover, A.G.; Fowler, L.C. Public health research implementation and translation: Evidence from practice-based research networks. Am. J. Prev. Med. 2013, 45, 752–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCullough, J.M.; Eisen-Cohen, E.; Salas, S.B. Partnership capacity for community health improvement plan implementation: Findings from a social network analysis. BMC Public Health 2016, 16, 566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- An, R.; Khan, N.; Loehmer, E.; McCaffrey, J. Assessing the Network of Agencies in Local Communities that Promote Healthy Eating and Lifestyles among Populations with Limited Resources. Am. J. Health Behav. 2017, 41, 127–138. [Google Scholar] [CrossRef]
- Cohen, R.; Havlin, S. Complex Networks: Structure, Robustness and Function; Cambridge University Press: Cambridge, UK, 2010; ISBN 1139489275. [Google Scholar]
- Krauss, M.; Mueller, N.; Luke, D. Interorganizational Relationships within State Tobacco Control Networks: A Social Network Analysis. Prev. Chronic Dis. 2004, 1, 1–25. [Google Scholar] [PubMed]
- McPherson, M.; Smith-Lovin, L.; Cook, J.M. Birds of a Feather: Homophily in Social Networks. Annu. Rev. Sociol. 2001, 27, 415–444. [Google Scholar] [CrossRef] [Green Version]
- An, R.; Loehmer, E.; Khan, N.; Scott, M.K.; Rindfleisch, K.; McCaffrey, J. Community partnerships in healthy eating and lifestyle promotion: A network analysis. Prev. Med. Rep. 2017, 6, 294–301. [Google Scholar] [CrossRef]
- Hoe, C.; Adhikari, B.; Glandon, D.; Das, A.; Kaur, N.; Gupta, S. Using social network analysis to plan, promote and monitor intersectoral collaboration for health in rural India. PLoS ONE 2019, 14, e0219786. [Google Scholar] [CrossRef] [Green Version]
- Harper, G.W.; Neubauer, L.C.; Bangi, A.K.; Francisco, V.T. Transdisciplinary research and evaluation for community health initiatives. Health Promot. Pract. 2008, 9, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Kobus, K.; Mermelstein, R. Bridging basic and clinical science with policy studies: The Partners with Transdisciplinary Tobacco Use Research Centers experience. Nicotine Tob. Res. 2009, 11, 467–474. [Google Scholar] [CrossRef]
- Granovetter, M. The strength of weak ties: A network theory revisited. Sociol Theory 1983, 1, 201. [Google Scholar] [CrossRef]
- Burt, R.S. Structural Holes: The Social Structure of Competition; Harvard University Press: Cambridge, MA, USA, 1992; ISBN 0674029097. [Google Scholar]
- Valente, T.W.; Pitts, S.R. An Appraisal of Social Network Theory and Analysis as Applied to Public Health: Challenges and Opportunities. Annu. Rev. Public Health 2017, 38, 103–118. [Google Scholar] [CrossRef] [Green Version]
- Spoth, R.L.; Greenberg, M.T. Toward a comprehensive strategy for effective practitioner-scientist partnerships and larger-scale community health and well-being. Am. J. Community Psychol. 2005, 35, 107–126. [Google Scholar] [CrossRef]
- Pineo, H.; Turnbull, E.R.; Davies, M.; Rowson, M.; Hayward, A.C.; Hart, G.; Johnson, A.M.; Aldridge, R.W. A new transdisciplinary research model to investigate and improve the health of the public. Health Promot. Int. 2021, 36, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.; Cousens, L.; MacLean, J. Trust and collaborative ties in a community sport network. Manag. Sport Leis. 2018, 22, 310–324. [Google Scholar] [CrossRef]
- Hennig, M.; Brandes, U.; Pfeffer, J.; Mergel, I. Studying Social Networks: A Guide to Empirical Research; Campus Verlag: Frankfurt am Main, Germany, 2012; ISBN 3593397633. [Google Scholar]
- Stirman, S.W.; Kimberly, J.; Cook, N.; Calloway, A.; Castro, F.; Charns, M. The sustainability of new programs and innovations: A review of the empirical literature and recommendations for future research. Implement. Sci. 2012, 7, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Everett, M.G.; Valente, T.W. Bridging, brokerage and betweenness. Soc. Netw. 2016, 44, 202–208. [Google Scholar] [CrossRef] [Green Version]
- Jaramillo, A.M.; Montes, F.; Sarmiento, O.L.; Ríos, A.P.; Rosas, L.G.; Hunter, R.F.; Rodríguez, A.L.; King, A.C. Social cohesion emerging from a community-based physical activity program: A temporal network analysis. Net. Sci. 2021, 9, 35–48. [Google Scholar] [CrossRef]
- Stokols, D.; Hall, K.L.; Vogel, A.L. Transdisciplinary public health: Definitions, core characteristics, and strategies for success. In Transdisciplinary Public Health: Research, Education, and Practice, 1st ed.; Haire-Joshu, D., McBride, T.D., Eds.; Jossey-Bass: San Francisco, CA, USA, 2013; pp. 3–30. ISBN 0470621990. [Google Scholar]
- Luke, D.A.; Harris, J.K.; Shelton, S.; Allen, P.; Carothers, B.J.; Mueller, N.B. Systems analysis of collaboration in 5 national tobacco control networks. Am. J. Public Health 2010, 100, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Lucidarme, S.; Marlier, M.; Cardon, G.; de Bourdeaudhuij, I.; Willem, A. Critical success factors for physical activity promotion through community partnerships. Int. J. Public Health 2014, 59, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Batonda, G.; Perry, C. Approaches to relationship development processes in inter—firm networks. Eur. J. Mark. 2003, 37, 1457–1484. [Google Scholar] [CrossRef]
| Authors | Network Setting | Aim | Type of Analysis | No. of Networks (Organizations) | Types of Nodes | Types of Ties | Network Concepts/Parameters |
|---|---|---|---|---|---|---|---|
| Andrade et al. (2018) | District of Sao Paulo, Brazil (community level) | Assessment of network structure, describe factors associated to establish collaboration or partnership ties | Descriptive, explanatory (ERGM) | One network (n = 32) | Actors from open streets, community clubs, social organizations, and public sector | Collaborative integration, contact, distance | Density, betweenness-/in-degree-/out-degree- centrality, transitivity, centralization, |
| Barnes et al. (2010) | One region in Canada (community level) | Assessment of network structure, identification of types of ties | Descriptive | One network (n = 31) | Community-based, non-profit and public actors (education, government, recreation, health, social services) | Collaborative integration (resources, information, fundraising, marketing) | Density, centralization, cliques |
| Brownson et al. (2010) | Brazil, USA (national level) | Assessment of network structure, roles, gaps and barriers | Explanatory (ERGM) | One network (n = 28) | Actors from research, education, promotion of PA in practice settings, actors developing and implementing policy | Collaborative integration, leadership, contact, importance | Density, closeness-/betweenness-/ in-degree-/out-degree- centrality, transitivity, centralization, structural equivalence |
| Buchthal et al. (2013) | Hawaii, USA (state level) | Assessment of network structure and identification of key roles; provision of a model for evaluation | Descriptive | One network (n = 23) | Department of health, nutrition and physical activity coalition agencies, other government agencies, voluntary organizations, health insurance companies | Collaborative integration, communication, funding, importance | Density, betweenness centralization/centrality |
| Loitz et al. (2017) | Province of Alberta, Canada (state level) | Assessment of network structure, examination of PA-policy use | Explanatory (discriminant function analysis) | One network (n = 27) | Actors from education, health, recreation, community, human services, transportation, fitness, child services or programming | Collaborative integration, funding | Density, degree-/betweenness centralization, degree-/betweenness centrality |
| Meisel et al. (2014) | Bogotá, Colombia (community level) | Identification of agencies, roles, structure, subgroups; relationship between structural characteristics and integration | Explanatory (ERGM) | One network (n = 22) | Actors from transport and urban planning, marketing services, research and academy, sports and recreation, government, health, security, education, environment | Collaborative integration, relationship, contact, importance, leadership | Density, closeness-/betweenness-/in-degree-/out-degree-centrality, reciprocity, structural equivalence |
| Parra et al. (2011) | Colombia and Brazil (national level) | Description and comparison of predictors of collaboration | Explanatory (ERGM) | Two networks: Brazil (n = 28), Colombia (n = 45) | Actors from the government sector and non-government sector (research, education, policy, practice) | Collaborative integration, importance, distance | Density, centralization |
| Yessis et al. (2013) | School setting in Canada, Ontario (community level) | Testing the method of network analysis for evaluating the program Spark | Descriptive | One network (n = 52) | National, provincial, regional, local organizations from urban and rural settings (health, education, recreation, public service, community/citizen groups) | Collaborative integration | Density, centralization, centrality, degree-/betweenness centrality |
| Authors | 1. Aims of the Research | 2. Boundary Setting/Actor Identification | 3. Participation Rate ≥ 75% | 4. Data Collection | 5. Description of Investigated Network | 6.1. Definition of Health Promotion and Physical Activity | 6.2. Definition of Social Network Analysis | 6.3. Definition of Variables | 7. Same Mode of Data Collection for all Subjects | 8. Ethics | 9. Findings | Total Number Yes/No/Cannot Determine |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Andrade et al. (2018) | + | + | 0 | + | + | − | − | + | + | + | + | 8/2/1 |
| Barnes et al. (2010) | + | + | + | + | + | − | + | + | − | − | + | 8/3/0 |
| Brownson et al. (2010) | + | + | + | + | + | − | − | + | − | + | + | 8/3/0 |
| Buchthal et al. (2013) | + | + | + | + | + | + | + | + | + | − | + | 10/1/0 |
| Loitz et al. (2017) | + | + | + | + | + | + | + | + | + | + | + | 11/0/0 |
| Meisel et al. (2014) | + | + | + | − | + | 0 | 0 | + | + | + | + | 8/1/2 |
| Parra et al. (2011) | + | + | + | 0 | + | 0 | + | + | + | + | + | 9/0/2 |
| Yessis et al. (2013) | + | + | + | + | + | − | + | + | − | − | + | 8/3/0 |
| Total number Yes/No/Cannot determine | 8/0/0 | 8/0/0 | 7/0/1 | 6/1/1 | 8/0/0 | 2/5/3 | 5/2/1 | 8/0/0 | 5/3/0 | 5/3/0 | 8/0/0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Timm, I.; Rapp, S.; Jeuter, C.; Bachert, P.; Reichert, M.; Woll, A.; Wäsche, H. Interorganizational Networks in Physical Activity Promotion: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7306. https://doi.org/10.3390/ijerph18147306
Timm I, Rapp S, Jeuter C, Bachert P, Reichert M, Woll A, Wäsche H. Interorganizational Networks in Physical Activity Promotion: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(14):7306. https://doi.org/10.3390/ijerph18147306
Chicago/Turabian StyleTimm, Irina, Simone Rapp, Christian Jeuter, Philip Bachert, Markus Reichert, Alexander Woll, and Hagen Wäsche. 2021. "Interorganizational Networks in Physical Activity Promotion: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 14: 7306. https://doi.org/10.3390/ijerph18147306
APA StyleTimm, I., Rapp, S., Jeuter, C., Bachert, P., Reichert, M., Woll, A., & Wäsche, H. (2021). Interorganizational Networks in Physical Activity Promotion: A Systematic Review. International Journal of Environmental Research and Public Health, 18(14), 7306. https://doi.org/10.3390/ijerph18147306






