Interventions to Support Mental Health among Those with Health Conditions That Present Risk for Severe Infection from Coronavirus Disease 2019 (COVID-19): A Scoping Review of English and Chinese-Language Literature †
Abstract
1. Introduction
- i.
- What mental health conditions and substance use risk factors are related to the COVID-19 pandemic among populations with chronic physical health conditions who are at risk of contracting COVID-19 and having severe symptoms?
- ii.
- What are effective health promotion, primary prevention, screening, and treatment interventions to enhance mental health outcomes and to reduce risk of substance use for populations with chronic physical health conditions who are at risk of contracting COVID-19 and having severe symptoms?
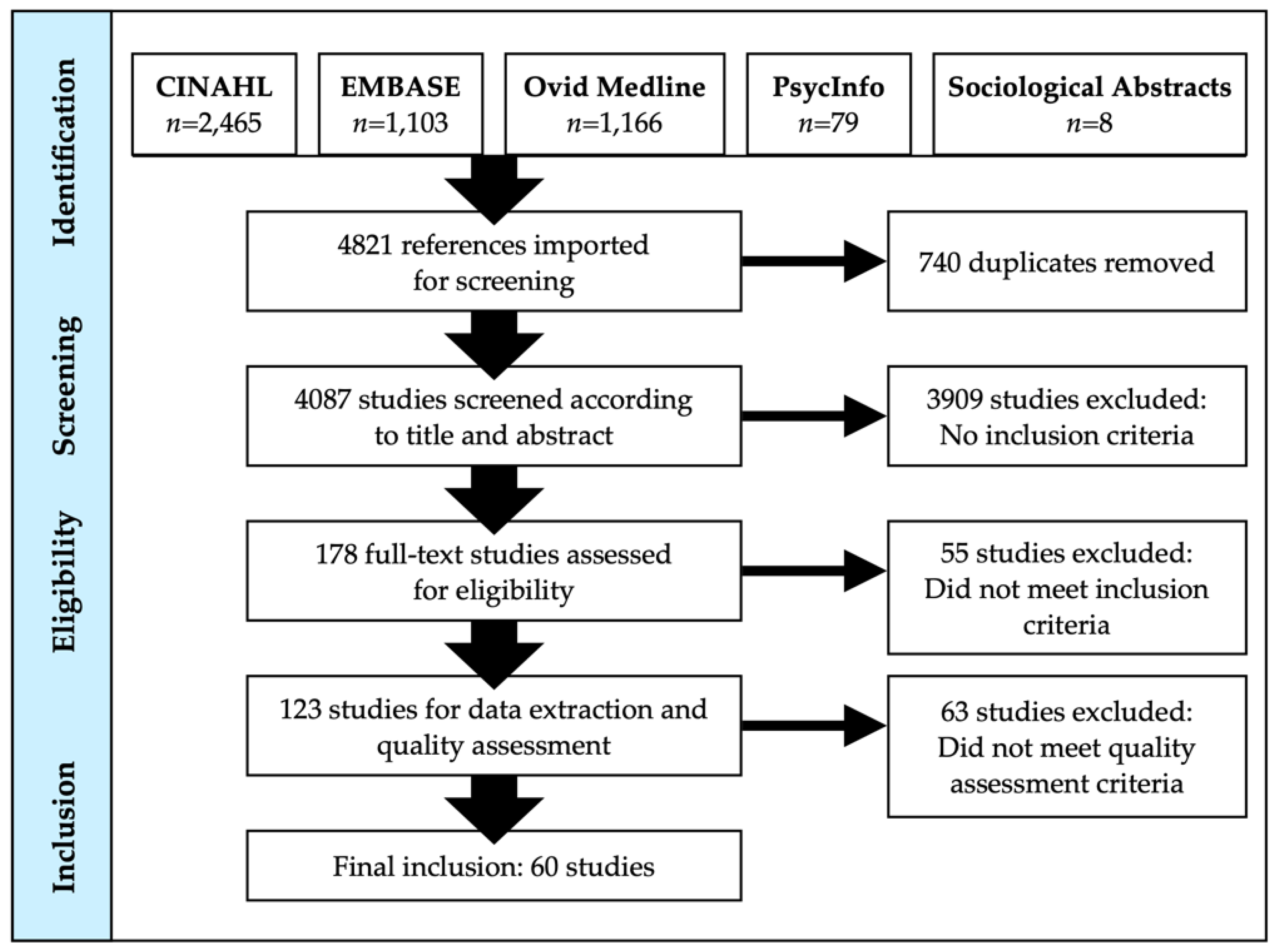
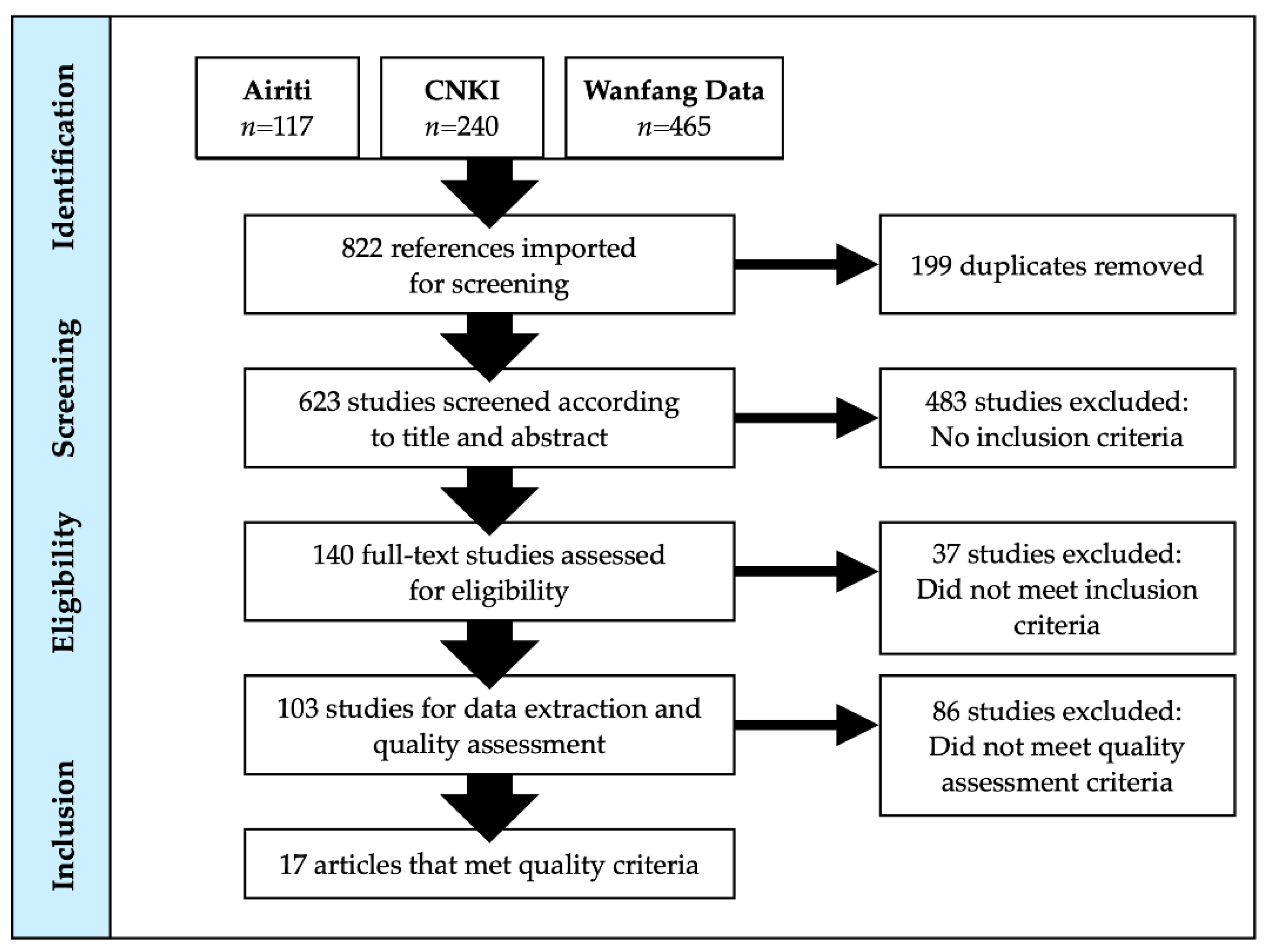
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion/Exclusion Criteria and Search Dates
2.3. Screening, Data Extraction, and Quality Assessment
3. Results
3.1. Results Relevant to Scoping Review Question 1
3.1.1. Mental Health Conditions
Individuals with Cancer
Individuals with Diabetes
Individuals with Epilepsy
Individuals with Obesity
Individuals with Parkinson’s Disease
Individuals with Respiratory Conditions
3.1.2. Substance Use
Individuals with Risk Factors for Substance Use
3.2. Results Relevant to Scoping Review Question 2
3.2.1. Individuals with Various Physical Health Conditions
3.2.2. Health Promotion and Primary to Tertiary Prevention
Individuals Living with Cancer
- i.
- accept that distress is a normal response to cancer and the COVID-19 epidemic;
- ii.
- trust the doctor and build a harmonious doctor-patient relationship;
- iii.
- maintain a stable life routine; be positive and optimistic;
- iv.
- communicate with relatives and friends; do not conceal your health status;
- v.
- arrange appropriate recreational activities every day and perform aerobic exercises when your physical condition allows. Recommended activities include yoga and traditional Chinese-based aerobic activities such as Tai Chi and Baduan Jin to balance qi (circulating life force);
- vi.
- establish a healthy sleep cycle and avoid using a mobile phone in bed;
- vii.
- when self-regulation cannot relieve anxiety, depression, and other emotions, seek professional help from a psychiatrist or psychologist.
Individuals Living with Other Chronic Health Conditions
- i.
- strengthen health education related to COVID-19 through the WeChat online platform;
- ii.
- increase information transparency to reduce anxiety, especially to correct misunderstandings about the pandemic from unreliable sources;
- iii.
- strengthen the support offered by the doctor and family members. By receiving external support, patients may be better able to face the challenges of the pandemic;
- iv.
- provide nutrition guidance. Proteins are especially crucial, as the process of dialysis leads to a loss of proteins;
- v.
- guide individuals to use the professional mental health channel, as established by the hospital through the WeChat online platform.
Individuals Living with Complications from COVID-19
Individuals Living with Dementia
Equity-Seeking Individuals with Pre-Existing Physical Health Conditions
Individuals Living with Substance Use
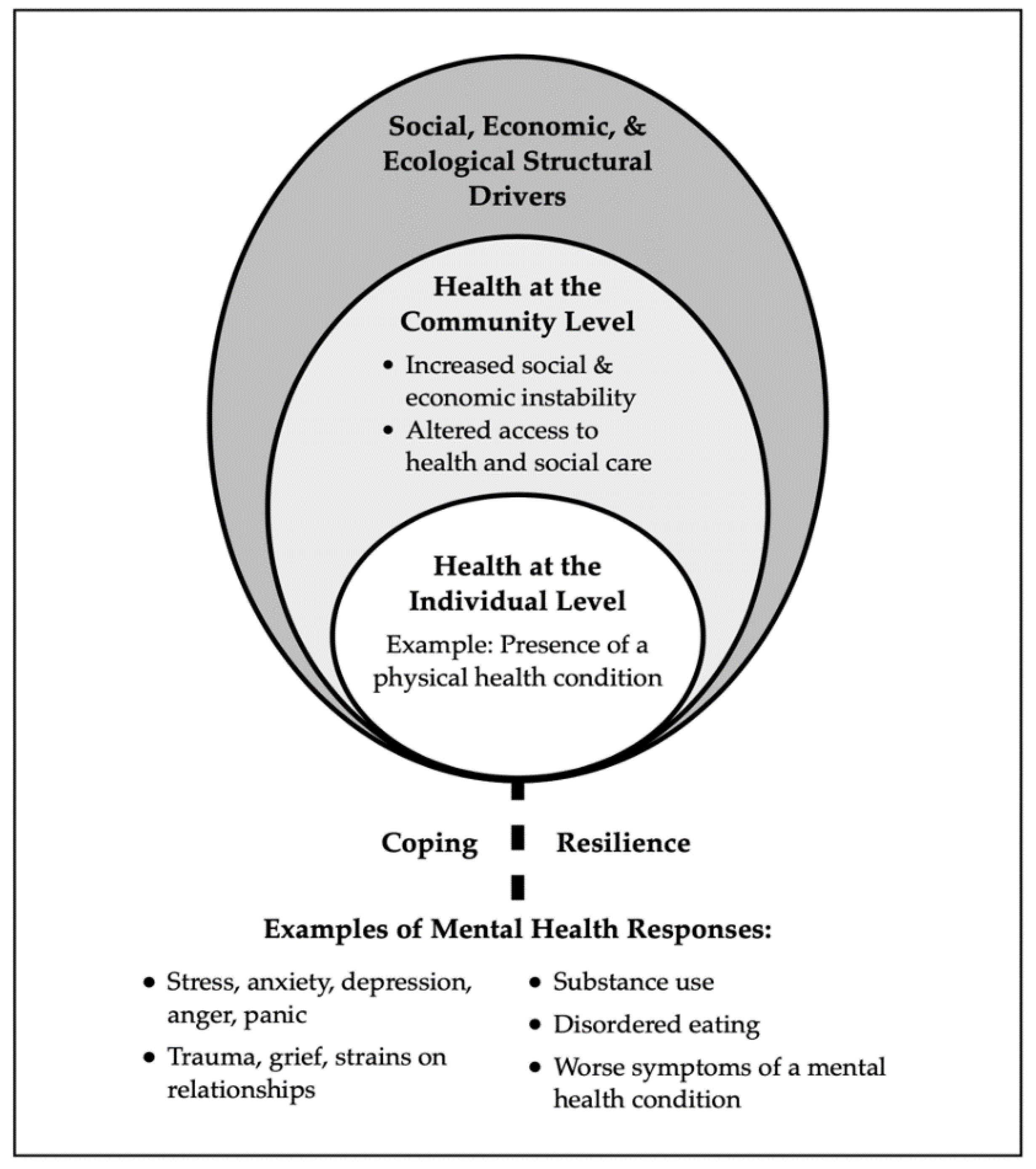
4. Discussion
4.1. Factors Contributing to Mental Health and Well-Being
4.2. Mental Health Promotion and Policy
4.3. Health Education and Literacy
4.4. Health and Social Care Delivery
- registries of people with complex needs to track preventative care, disease/illness management, and referrals to secondary and tertiary care services;
- health care system navigation supports and shared decision-making approaches;
- competencies among practitioners to deliver high-quality health care to people with mental health problems;
- training practitioners in the recovery model, including stigma, discrimination, and trauma-informed care;
- evidence-based mental health screening guidelines with accompanying management pathways.
4.5. Mental Health Screening and Assessment
4.6. Psychological, Lifestyle, and Peer Approaches
4.7. Strengths and Limitations of the Scoping Review
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. People Who Are at Higher Risk for Severe Illness. 2020. Available online: www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html (accessed on 30 October 2020).
- Government of Canada. Health Infobase Canada. 2020. Available online: Health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html (accessed on 24 November 2020).
- Soklaridis, S.; Lin, E.; Lalani, Y.; Rodak, T.; Sockalingam, S. Mental health interventions and supports during COVID-19 and other medical pandemics: A rapid systematic review of the evidence. Gen. Hosp. Psychiatry 2020, 66, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Bloom, D.E.; Cafiero, E.T.; Jané-Llopis, E.; Abrahams-Gessel, S.; Bloom, L.R.; Fathima, S.; Feigl, A.B.; Gaziano, T.; Mowafi, M.; Pandya, A.; et al. The Global Economic Burden of Noncommunicable Diseases. Geneva. 2011. Available online: www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf (accessed on 24 November 2020).
- Cox, J.; Hamelin, A.M.; McLinden, T.; Moodie, E.E.; Anema, A.; Rollet-Kurhajec, K.C.; Paradis, G.; Rourke, S.B.; Walmsley, S.L.; Klein, M.B. Canadian Co-infection Cohort Investigators. Food insecurity in HIV-hepatitis C virus co-infected individuals in Canada: The importance of co-morbidities. AIDS Behav. 2017, 21, 792–802. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Risks Mortality and Burden of Disease Attributable to Selected Major Risk. 2009. Available online: https://apps.who.int/iris/bitstream/handle/10665/44203/9789241563871_eng.pdf?sequence=1&isAllowed=y (accessed on 25 November 2020).
- Keyes, C.L.M. The mental health continuum: From languishing to flourishing in life. J. Health Soc. Behav. 2002, 43, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Lunn, P.; Belton, C.; Lavin, C.; McGowan, F.; Timmons, S.; Robertson, D. Using Behavioural Science to Help Fight the Coronavirus (No. WP656). Economic and Social Research Institute (ESRI). 2020. Available online: www.esri.ie/pubs/WP656.pdf (accessed on 25 November 2020).
- Taha, S.; Matheson, K.; Cronin, T.; Anisman, H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H1N1 pandemic. Br. J. Health Psychol. 2014, 19, 592–605. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Davison, K.M.; Holloway, C.; Gondara, L.; Hatcher, A.S. Independent associations and effect modification between lifetime substance use and recent mood disorder diagnosis with household food insecurity. PLoS ONE 2018, 13, e0191072. [Google Scholar] [CrossRef]
- Brooks, S.K.; Dunn, R.; Amlôt, R.; Rubin, G.J.; Greenberg, N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J. Occup. Environ. Med. 2018, 60, 248–257. [Google Scholar] [CrossRef]
- Kosinski, S.; Mohammad, R.A.; Pitcher, M.; Haezebrouck, E.; Coe, A.B.; Costa, D.K.; Prescott, H.C.; Iwashyna, T.J.; McSarron, J.I. What is post-intensive care syndrome (PICS)? Am. J. Respir. Crit. Care Med. 2020, 201, 15–16. [Google Scholar] [CrossRef]
- Lee, M.; Kang, J.; Jeong, Y.J. Risk factors for post-intensive care syndrome: A systematic review and meta-analysis. Aust. Crit. Care 2020, 33, 287–294. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Covidence Systematic Review Software. 2020. Available online: www.covidence.org (accessed on 30 June 2020).
- Knottnerus, A.; Tugwel, l.P. STROBE—A Checklist to Strengthen the Reporting of Observational Studies in Epidemiology. J. Clin. Epidemiol. 2008, 61, 323. [Google Scholar] [CrossRef] [PubMed]
- Manchikanti, L.; Datta, S.; Smith, H.S.; Hirsch, J.A. Evidence-based medicine, systematic reviews, and guidelines in interventional pain management: Part 6. Systematic reviews and meta-analyses of observational studies. Pain Physician 2009, 12, 819. [Google Scholar] [CrossRef]
- Pace, R.; Pluye, P.; Bartlett, G.; Macaulay, A.C.; Salsberg, J.; Jagosh, J.; Seller, R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int. J. Nurs. Stud. 2012, 49, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.; Tiwari, A.; Fu, R.; Moe, E.; Buckley, D.I. A Framework to Facilitate the Use of Systematic Reviews and Meta-Analyses in the Design of Primary Research Studies. Rockville (MD). 2012. Available online: https://pubmed.ncbi.nlm.nih.gov/22299187 (accessed on 25 November 2020).
- Haines, A.; de Barros, E.F.; Berlin, A.; Heymann, D.L.; Harris, M.J. National UK programme of community health workers for COVID-19 response. Lancet 2020, 395, 1173–1175. [Google Scholar] [CrossRef]
- Ahmed, M.Z.; Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and associated psychological problems. Asian. J. Psychiatr. 2020, 51, 102092. [Google Scholar] [CrossRef]
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef] [PubMed]
- Nachimuthu, S.; Vijayalakshmi, R.; Sudha, M.; Viswanathan, V. Coping with diabetes during the COVID–19 lockdown in India: Results of an online pilot survey. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 579–582. [Google Scholar] [CrossRef] [PubMed]
- Mediouni, M.; Madiouni, R.; Kaczor-Urbanowicz, K.E. COVID-19: How the quarantine could lead to the Depreobesity. Obes. Med. 2020, 19, 100255. [Google Scholar] [CrossRef]
- Moghadasi, A.N. One aspect of coronavirus disease (COVID-19) Outbreak in Iran: High anxiety among MS Patients. Mult. Scler. Relat. Disord. 2020, 41, 102138. [Google Scholar] [CrossRef]
- Zhao, M.; Wang, M.; Zhang, J.; Ye, J.; Xu, Y.; Wang, Z.; Ye, D.; Liu, J.; Wan, J. Advances in the relationship between coronavirus infection and cardiovascular diseases. Biomed. Pharmacother. 2020, 127, 110230. [Google Scholar] [CrossRef]
- Zhao, M.; Peng, D.; Liu, Q.; Ouyang, Y. Investigation on mental status of patients with hematological malignancies during the COVID-19 outbreak and related influencing factors. Nurs. Integr. Tradit. Chin. West. Med. 2020, 6, 38–41. [Google Scholar]
- Chen, X.; Chen, C.; Chen, X.; Lin, X.; Lai, S.; Xu, L. Psychological Distress and Influencing Factors of Cancer Patients during the New Coronary Pneumonia Epidemic. Chin. J. of Health Psychol 2020. Available online: https://kns.cnki.net/kcms/detail/11.5257.R.20200720.1025.002.html (accessed on 15 July 2020).
- Xu, H.; Yang, K.; Yang, G.; Yang, L.; Mi, Y.; Cui, X.; Yang, M.; Wang, D.; Wang, Y. Optimize the exploration of solving the diagnosis and treatment problems and psychological problems of lung cancer patients during the new coronavirus pneumonia epidemic. Chin. J. Lung Cancer 2020, 23, 247–254. [Google Scholar]
- Vanni, G.; Materazzo, M.; Pellicciaro, M.; Ingallinella, S.; Rho, M.; Santori, F.; Cotesta, M.; Caspi, J.; Makarova, A.; Pistolese, C.A.; et al. Breast cancer and COVID-19: The effect of fear on patients’ decision-making process. In Vivo 2020, 34 (Suppl. S3), 1651–1659. [Google Scholar] [CrossRef]
- Zhang, C.; Wu, J.; Li, J.; Guo, X.; Liu, S.; Zeng, Y. Analysis of psychological status of diabetic patients during the epidemic of new coronavirus pneumonia. Gen. Nurs. 2020, 18, 965–968. [Google Scholar]
- Hao, X.; Zhou, D.; Li, Z.; Zeng, G.; Hao, N.; Li, E.; Li, W.; Deng, A.; Lin, M.; Yan, B. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia 2020, 61, 1166–1173. [Google Scholar] [CrossRef]
- Walędziak, M.; Różańska-Walędziak, A.; Pędziwiatr, M.; Szeliga, J.; Proczko-Stepaniak, M.; Wysocki, M.; Stefura, T.; Major, P. Bariatric surgery during COVID-19 pandemic from patients’ point of view-The results of a national survey. J. Clin. Med. 2020, 9, 1697. [Google Scholar] [CrossRef] [PubMed]
- Sockalingam, S.; Leung, S.E.; Cassin, S.E. The impact of coronavirus disease 2019 on bariatric surgery: Redefining psychosocial care. Obesity 2020, 28, 1010–1012. [Google Scholar] [CrossRef] [PubMed]
- Zipprich, H.M.; Teschner, U.; Witte, O.W.; Schönenberg, A.; Prell, T. Knowledge, attitudes, practices, and burden during the COVID-19 pandemic in people with Parkinson’s disease in Germany. J. Clin. Med. 2020, 9, 1643. [Google Scholar] [CrossRef] [PubMed]
- Lili, W.; Zhilei, S.; Fan, A.; Luna, S.; Weizhi, L. Investigation of post-traumatic stress symptoms in 2 confirmed and 6 suspected new coronavirus pneumonia patients. J. Second Mil. Med Univ. 2020, 41, 186–190. [Google Scholar]
- Rozanova, J.; Shenoi, S.; Zaviryukha, I.; Zeziulin, O.; Kiriazova, T.; Rich, K.; Mamedova, E.; Yariy, V. Social support is key to retention in care during COVID-19 pandemic among older people with HIV and substance use disorders in Ukraine. Subst. Use Misuse 2020, 55, 1902–1904. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Umucu, E.; Lee, B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil. Psychol. 2020, 65, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Germani, A.; Buratta, L.; Delvecchio, E.; Mazzeschi, C. Emerging adults and COVID-19: The role of individualism-collectivism on perceived risks and psychological maladjustment. Int. J. Environ. Res. Public. Health. 2020, 17, 3497. [Google Scholar] [CrossRef] [PubMed]
- Singelis, T.M.; Triandis, H.C.; Bhawuk, D.P.S.; Gelfand, M.J. Horizontal and vertical dimensions of individualism and collectivism: A theoretical and measurement refinement. Cross Cult. Res. 1995, 29, 240–275. [Google Scholar] [CrossRef]
- Nguyen, N.P.; Vinh-Hung, V.; Baumert, B.; Zamagni, A.; Arenas, M.; Motta, M.; Lara, P.C.; Myint, A.S.; Bonet, M.; Popescu, T.; et al. Older cancer patients during the COVID-19 epidemic: Practice Proposal of the International Geriatric Radiotherapy Group. Cancers 2020, 12, 1287. [Google Scholar] [CrossRef] [PubMed]
- Rodler, S.; Apfelbeck, M.; Schulz, G.B.; Ivanova, T.; Buchner, A.; Staehler, M.; Heinemann, V.; Stief, C.; Casuscelli, J. Telehealth in Uro-oncology Beyond the Pandemic: Toll or Lifesaver? Eur. Urol. Focus. 2020, 6, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.P.; Luo, X.; Zhang, J. Psychological stress and protective strategies in cancer patients during the outbreak of Corona Virus Disease 2019. J. Cancer Control Treat. 2020, 33, 106–110. [Google Scholar]
- Yuan, J.; Li, Q. Treatment process and doctor-patient protection measures for tumor radiotherapy patients under the epidemic of new coronavirus infection pneumonia. Modern Oncol. 2020, 28, 1407–1409. [Google Scholar]
- Zhang, Y.; Luo, X.; Zhang, J. Psychological stress and protective countermeasures of tumor patients during the epidemic period of new coronavirus pneumonia. Tumor Prev. Treat. 2020, 33, 106–110. [Google Scholar]
- Zhou, J.; Yan, J.; Tong, H. Management and practice of mental health of hemodialysis patients during the novel coronavirus pneumonia epidemic. Nurs. Integr. Tradit. Chin. West. Med. 2020, 6, 139–141. [Google Scholar]
- Zhang, J.; Sun Rong, Y.J. Anxiety and depression status of elderly patients and its influencing factors during the epidemic of novel coronavirus pneumonia. Chin. J. Mult. Organ. Dis. Elder. 2020, 19, 246–250. [Google Scholar]
- Helmich, R.C.; Bloem, B.R. The impact of the COVID-19 pandemic on Parkinson’s disease: Hidden sorrows and emerging opportunities. J. Parkinson’s Dis. 2020, 10, 351. [Google Scholar] [CrossRef]
- Dell, N.A.; Sasaki, N.; Stewart, M.; Murphy, A.M.; Klier, M. Service needs of older adults with serious mental illness. J. Gerontol. Soc. Work 2020, 63, 659–661. [Google Scholar] [CrossRef]
- Wang, L.; Huang, R.; Chen, J.; Chen, W. Discussion on Home Care Practice for the Elderly under the Epidemic of Novel Coronavirus Pneumonia. J. Jinan Univ. 2020, 41, 123–128. [Google Scholar]
- Huang, B..; Zhang, T.; Zou, G.; Li, Y.; Wu, L.; Huang, Y. Investigation and prevention and control analysis of the mental state of the elderly under the new coronavirus pneumonia epidemic. Gen. Nurs. 2020, 18, 935–937. [Google Scholar]
- Ceravolo, M.G.; de Sire, A.; Andrenelli, E.; Negrini, F.; Negrini, S. Systematic rapid “living” review on rehabilitation needs due to COVID-19: Update to March 31st, 2020. Eur. J. Phys. Rehabil. Med. 2020, 56, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Barker-Davies, R.M.; O’Sullivan, O.; Senaratne, K.P.P.; Baker, P.; Cranley., M.; Dharm-Datta., S.; Ellis, H.; Goodall, D.; Gough, M.; Lewis, S.; et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br. J. Sports Med. 2020, 54, 949. [Google Scholar] [CrossRef] [PubMed]
- Wei, N.; Huang, B.C.; Lu, S.J.; Hu, J.B.; Zhou, X.Y.; Hu, C.C.; Chen, J.K.; Huang, J.W.; Li, S.G.; Wang, Z.; et al. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J. Zhejiang Univ. Sci. B 2020, 21, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Liu, X.; Guo, H.; Fan, H.; Jiang, R.; Tan, S. Mental health of middle-aged and elderly population during outbreak of corona-virus disease 2019. Chin. J. Mult. Organ Dis. Elder 2020, 19, 241–245. [Google Scholar]
- Padala, S.P.; Jendro, A.M.; Orr, L.C. Facetime to reduce behavioral problems in a nursing home resident with Alzheimer’s dementia during COVID-19. Psychiatry Res. 2020, 288, 113028. [Google Scholar] [CrossRef]
- Goodman-Casanova, J.M.; Dura-Perez, E.; Guzman-Parra, J.; Cuesta-Vargas, A.; Mayoral-Cleries, F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: Survey study. J. Med. Internet. Res. 2020, 22, e19434. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.E.; Kumar, S.; Rajji, T.K.; Pollock, B.G.; Mulsant, B.H. Anticipating and mitigating the impact of the COVID-19 pandemic on Alzheimer’s disease and related dementias. Am. J. Geriatr. Psychiatry 2020, 28, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Ajilore, O.; Thames, A.D. The fire this time: The stress of racism, inflammation and COVID-19. Brain Behav. Immun. 2020, 88, 66–67. [Google Scholar] [CrossRef] [PubMed]
- Fortuna, L.R.; Tolou-Shams, M.; Robles-Ramamurthy, B.; Porche, M.V. Inequity and the disproportionate impact of COVID-19 on communities of color in the United States: The need for a trauma-informed social justice response. Psychol. Trauma 2020, 12, 443–445. [Google Scholar] [CrossRef] [PubMed]
- Armbruster, M.; Fields, E.L.; Campbell, N.; Griffith, D.C.; Kouoh, A.M.; Knott-Grasso, M.A.; Arrington-Sanders, R.; Agwu, A.L. Addressing health inequities exacerbated by COVID-19 among youth with HIV: Expanding our toolkit. J. Adolesc. Health 2020, 67, 290–295. [Google Scholar] [CrossRef]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Algarin, A.B.; Varas-Rodríguez, E.; Valdivia, C.; Fennie, K.P.; Larkey, L.; Hu, N.; Ibañez, G.E. Symptoms, stress, and HIV-related care among older people living with HIV during the COVID-19 pandemic, Miami, Florida. AIDS Behav. 2020, 24, 2236–2238. [Google Scholar] [CrossRef]
- Sanchez, T.H.; Zlotorzynska, M.; Rai, M.; Baral, S.D. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav. 2020, 24, 2024–2032. [Google Scholar] [CrossRef]
- Ahmed, H.; Patel, K.; Greenwood, D.C.; Halpin, S.; Lewthwaite, P.; Salawu, A.; Eyre, L.; Breen, A.; O’Connor, R.; Jones, A.; et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalization or ICU admission: A systematic review and meta-analysis. J. Rehabil. Med. 2020, 52, jrm00063. [Google Scholar]
- Da, B.L.; Im, G.Y.; Schiano, T.D. COVID-19 hangover: A rising tide of alcohol use disorder and alcohol-associated liver disease. Hepatology 2020, 72, 1102–1108. [Google Scholar] [CrossRef]
- Tapper, E.B. Predicting overt hepatic encephalopathy for the population with cirrhosis. Hepatology 2019, 70, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, A.V.; Puviani, M.B.; Nasi, M.; Farinetti, A. COVID-19 pandemic: The effects of quarantine on cardiovascular risk. Eur. J. Clin. Nutr. 2020, 74, 852–855. [Google Scholar] [CrossRef] [PubMed]
- Yuan, N.; Chen, Y.; Xia, Y.; Dai, J.; Liu, C. Inflammation-related biomarkers in major psychiatric disorders: A cross-disorder assessment of reproducibility and specificity in 43 meta-analyses. Transl. Psychiatry 2019, 9, 233. [Google Scholar] [CrossRef] [PubMed]
- Fiest, K.M.; Hitchon, C.A.; Bernstein, C.N.; Peschken, C.A.; Walker, J.R.; Graff, L.A.; Zarychanski, R.; Abou-Setta, A.; Patten, S.B.; Sareen, J.; et al. Systematic review and meta-analysis of interventions for depression and anxiety in persons with rheumatoid arthritis. J. Clin. Rheumatol. 2017, 23, 425–434. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Integrating the Prevention, Treatment and Care of MH Conditions and Other Noncommunicable Diseases within Health Systems. WHO European High-Level Conference on Non-Communicable Diseases. Copenhagen. 2019. Available online: www.euro.who.int/__data/assets/pdf_file/0004/397786/Mental-Health-Conditions-ENG.pdf (accessed on 25 October 2020).
- Cohen, A. Addressing Comorbidity between Mental Disorders and Major Noncommunicable Diseases. Background Technical Report to Support Implementation of the WHO European Mental Health Action Plan 2013–2020 and the WHO European Action Plan for the Prevention and Control of Noncommunicable Diseases 2016–2025. 2017. Available online: http://www.euro.who.int/__data/assets/pdf_file/0009/342297/Comorbidity-report_E-web.pdf (accessed on 25 October 2020).
- Nouwen, A.; Winkley, K.; Twisk, J.; Lloyd, C.E.; Peyrot, M.; Ismail, K.; Pouwer, F.; European Depression in Diabetes (EDID) Research Consortium. Type 2 diabetes mellitus as a risk factor for the onset of depression: A systematic review and meta-analysis. Diabetologia 2010, 53, 2480–2486. [Google Scholar] [CrossRef]
- Mikocka-Walus, A.; Knowles, S.R.; Keefer, L.; Graff, L. Controversies revisited: A systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm. Bowel Dis. 2016, 22, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Doi, M.; Fukahori, H.; Oyama, Y.; Morita, K. Factors associated with depressive symptoms in patients with acute coronary syndrome undergoing percutaneous coronary intervention: A prospective cohort study. Nurs. Open 2018, 5, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Davison, K.M.; Carroll, S.; Collins, B.; D’Andreamatteo, C.; Sorensen, J.; Lung, Y.; Stabler, S.; Thakkar, V.; Garg, A. For the Mental Health Commission of Canada and Canadian Partnership Against Cancer (In Press). Towards Better Mental and Physical Health: Preventing and Managing Concurrent Mental and Physical Conditions: A Scoping and Rapid Realist Review. Available online: https://cihr-irsc.gc.ca/e/52036.html (accessed on 30 November 2020).
- Ingram, R.E.; Luxton, D. Vulnerability-stress models. In Development of Psychopathology: A Vulnerability-Stress Perspective; Hankin, B.L., Abela, J.R.Z., Eds.; Sage: New York, NY, USA, 2005. [Google Scholar]
- Horton, R. Offline: COVID-19 is not a pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef]
- Pan, A.; Sun, Q.; Okereke, O.I.; Rexrode, K.M.; Hu, F.B. Depression and risk of stroke morbidity and mortality: A meta-analysis and systematic review. JAMA 2011, 306, 1241–1249. [Google Scholar] [CrossRef]
- Rodriguez-Llanes, J.M.; Vos, F.; Guha-Sapir, D. Measuring psychological resilience to disasters: Are evidence-based indicators an achievable goal? Environ. Health 2013, 12, 115. [Google Scholar] [CrossRef]
- Centre for Addiction and Mental Health. Best Practice Guidelines for Mental Health Promotion Programs: Children (7–12) and Youth (13–19); Centre for Addiction and Mental Health: Toronto, ON, Canada, 2014. [Google Scholar]
- Wasserman, D.; Iosue, M.; Wuestefeld, A.; Carli, V. Adaptation of evidence-based suicide prevention strategies during and after the COVID-19 pandemic. World Psychiatry 2020, 19, 294–306. [Google Scholar] [CrossRef] [PubMed]
- Mannix, R.; Lee, L.K.; Fleegler, E.W. Coronavirus Disease 2019 (COVID-19) and firearms in the United States: Will an epidemic of suicide follow? Ann. Intern. Med. 2020, 173, 228–229. [Google Scholar] [CrossRef] [PubMed]
- Norström, T.; Rossow, I. Alcohol consumption as a risk factor for suicidal Behavior: A systematic review of associations at the individual and at the population level. Arch. Suicide Res. 2016, 20, 489–506. [Google Scholar] [CrossRef] [PubMed]
- Anderson, M.; Mckee, M.; Mossialos, E. Developing a sustainable exit strategy for COVID-19: Health, economic and public policy implications. J. R. Soc. Med. 2020, 113, 176–178. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Siddique, R.; Li, H.; Ali, A.; Shereen, M.A.; Bashir, N.; Xue, M. Impact of coronavirus outbreak on psychological health. J. Glob. Health 2020, 10, 10331. [Google Scholar] [CrossRef]
- Wolf, M.S.; Gazmararian, J.A.; Baker, D.W. Health literacy and functional health status among older adults. Arch. Intern. Med. 2005, 165, 1946–1952. [Google Scholar] [CrossRef]
- Baker, D.W.; Parker, R.M.; Williams, M.V.; Clark, W.S.; Nurss, J. The relationship of patient reading ability to self-reported health and use of health services. Am. J. Public Health 1997, 87, 1027–1030. [Google Scholar] [CrossRef]
- Vamos, S.; Okan, O.; Sentell, T.; Rootman, I. Making a case for “Education for Health Literacy”: An international perspective. Int. J. Environ. Res. Public Health 2020, 17, 1436. [Google Scholar] [CrossRef] [PubMed]
- Rootman, I.; Gordon-El-Bihbety, D. A Vision for a Health Literate Canada: Report of the Expert Panel on Health Literacy; Canadian Public Health Association: Ottawa, ON, Canada, 2008; Available online: https://www.cpha.ca/sites/default/files/uploads/resources/healthlit/report_e.pdf (accessed on 20 November 2020).
- Hatzenbuehler, M.L.; Phelan, J.C.; Link, B.G. Stigma as a fundamental cause of population health inequalities. Am. J. Public Health 2013, 103, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Frischknecht, U.; Beckmann, B.; Heinrich, M.; Kniest, A.; Nakovics, H.; Kiefer, F.; Mann, K.; Hermann, D. The vicious circle of perceived stigmatization, depressiveness, anxiety, and low quality of life in substituted heroin addicts. Eur. Addict. Res. 2011, 17, 241–249. [Google Scholar] [CrossRef]
- Major, B.; O’Brien, L.T. The social psychology of stigma. Annu. Rev. Psychol. 2005, 56, 393–421. [Google Scholar] [CrossRef]
- Mickelson, K.D. Perceived stigma, social support, and depression. Personal. Soc. Psychol. Bull. 2001, 27, 1046–1056. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Larson, J.E.; Rüsch, N. Self-stigma and the “why try” effect: Impact on life goals and evidence-based practices. World Psychiatry 2009, 8, 75–81. [Google Scholar] [CrossRef]
- Lichtenstein, B. From “Coffin Dodger” to “Boomer Remover”: Outbreaks of ageism in three countries with divergent approaches to coronavirus control. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2021, 76, e206–e212. [Google Scholar] [CrossRef]
- Frank, C.; Zamorski, M.A.; Colman, I. Stigma doesn’t discriminate: Physical and mental health and stigma in Canadian military personnel and Canadian civilians. BMC Psychol. 2018, 6, 61. [Google Scholar] [CrossRef]
- Hamann, H.A.; Ver Hoeve, E.S.; Carter-Harris, L.; Studts, J.L.; Ostroff, J.S. Multilevel opportunities to address lung cancer stigma across the Cancer Control Continuum. J. Thorac. Oncol. 2018, 13, 1062–1075. [Google Scholar] [CrossRef] [PubMed]
- Optimus SBR. Advancing the Integration Conversation: A Report to the Toronto Central LHIN. Toronto. 2016. Available online: www.torontocentrallhin.on.ca/~/media/sites/tc/TC LHIN Docs/Resources/Advancing the Integration Conversation Report and Appendix.pdf?la=en (accessed on 26 November 2020).
- Addiction and Mental Health Collaborative Project Steering Committee. Collaboration for Addiction and Mental Health Care: Best Advice; Canadian Centre on Substance Use and Addiction: Ottawa, ON, Canada, 2014. [Google Scholar]
- Ogden, J. Social prescribing in a time of Covid-19 and social isolation. Prog. Neurol. Psychiatry 2020, 24, 4–5. [Google Scholar] [CrossRef]
- Kates, N.; Mazowita, G.; Lemire, F.; Jayabarathan, A.; Bland, R.; Selby, P.; Isomura, T.; Craven, M.; Gervais, M.; Audet, D. The evolution of collaborative mental health care in Canada: A shared vision for the future. Can. J. Psychiatry 2011, 56, 1–10. [Google Scholar] [CrossRef][Green Version]
- Neville, C. Collaborative care approaches for people with severe mental illness. Clin. Nurs. Spec. 2015, 29, 143–144. [Google Scholar] [CrossRef] [PubMed]
- Swerdlow, D.L.; Finelli, L. Preparation for possible sustained transmission of 2019 novel coronavirus: Lessons from previous epidemics. JAMA. 2020, 323, 1129–1130. [Google Scholar] [CrossRef] [PubMed]
- Gillies, D.; Buykx, P.; Parker, A.G.; Hetrick, S.E. Consultation liaison in primary care for people with mental disorders. Cochrane Database Syst. Rev. 2015, 9, CD007193. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.W.; Wang, W.T.; Lin, L.F.; Liao, C.D.; Liou, T.H.; Lin, H.W. Association between psychiatric disorders and osteoarthritis: A nationwide longitudinal population-based study. Medicine 2016, 95, e4016. [Google Scholar] [CrossRef]
- Fleury, M.J.; Farand, L.; Aubé, D.; Imboua, A. Management of mental health problems by general practitioners in Quebec. Can. Fam. Physician 2012, 58, e732–e738. [Google Scholar] [PubMed]
- Cornelio-Flores, O.; Lestoquoy, A.S.; Abdallah, S.; DeLoureiro, A.; Lorente, K.; Pardo, B.; Olunwa, J.; Gardiner, P. The Latino Integrative Medical Group Visit as a model for pain reduction in underserved Spanish speakers. J. Altern. Complement. Med. 2018, 24, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Remick, R.A.; Araki, Y.; Bruce, R.; Gorman, C.; Allen, J.; Remick, A.K.; Lear, S.A. The Mood Disorders Association of British Columbia Psychiatric Urgent Care Program: A preliminary evaluation of a suggested alternative model of outpatient psychiatric care. Can. J. Psychiatry 2014, 59, 220–227. [Google Scholar] [CrossRef]
- McBrien, K.A.; Ivers, N.; Barnieh, L.; Bailey, J.J.; Lorenzetti, D.L.; Nicholas, D.; Tonelli, M.; Hemmelgarn, B.; Lewanczuk, R.; Edwards, A.; et al. Patient navigators for people with chronic disease: A systematic review. PLoS ONE 2018, 13, e0191980. [Google Scholar]
- Kneipp, S.M.; Kairalla, J.A.; Lutz, B.J.; Pereira, D.; Hall, A.G.; Flocks, J.; Beeber, L.; Schwartz, T. Public health nursing case management for women receiving temporary assistance for needy families: A randomized controlled trial using community-based participatory research. Am. J. Public Health 2011, 101, 1759–1768. [Google Scholar] [CrossRef] [PubMed]
- Farrington, C.; Aristidou, A.; Ruggeri, K. mHealth and global mental health: Still waiting for the mH2 wedding? Glob. Health 2014, 10, 17. [Google Scholar] [CrossRef]
- Marks, I.M.; Kenwright, M.; McDonough, M.; Whittaker, M.; Mataix-Cols, D. Saving clinicians’ time by delegating routine aspects of therapy to a computer: A randomized controlled trial in phobia/panic disorder. Psychol. Med. 2004, 34, 9–17. [Google Scholar] [CrossRef]
- Kuhn, E.; Greene, C.; Hoffman, J.; Nguyen, T.; Wald, L.; Schmidt, J.; Ramsey, K.M.; Ruzek, J. Preliminary evaluation of PTSD Coach, a smartphone app for post-traumatic stress symptoms. Mil. Med. 2014, 179, 12–18. [Google Scholar] [CrossRef]
- Possemato, K.; Kuhn, E.; Johnson, E.; Hoffman, J.E.; Owen, J.E.; Kanuri, N.; De Stefano, L.; Brooks, E. Using PTSD Coach in primary care with and without clinician support: A pilot randomized controlled trial. Gen. Hosp. Psychiatry 2016, 38, 94–98. [Google Scholar] [CrossRef]
- Kuester, A.; Niemeyer, H.; Knaevelsrud, C. Internet-based interventions for posttraumatic stress: A meta-analysis of randomized controlled trials. Clin. Psychol. Rev. 2016, 43, 1–16. [Google Scholar] [CrossRef]
- Litz, B.T.; Engel, C.C.; Bryant, R.A.; Papa, A. A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. Am. J. Psychiatry 2007, 164, 1676–1683. [Google Scholar] [CrossRef] [PubMed]
- Brief, D.J.; Rubin, A.; Keane, T.M.; Enggasser, J.L.; Roy, M.; Helmuth, E.; Hermos, J.; Lachowicz, M.; Rybin, D.; Rosenbloom, D. Web intervention for OEF/OIF veterans with problem drinking and PTSD symptoms: A randomized clinical trial. J. Consult. Clin. Psychol. 2013, 81, 890–900. [Google Scholar] [CrossRef] [PubMed]
- Hobfoll, S.E.; Blais, R.K.; Stevens, N.R.; Walt, L.; Gengler, R. Vets prevail online intervention reduces PTSD and depression in veterans with mild-to-moderate symptoms. J. Consult. Clin. Psychol. 2016, 84, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, B. Virtual Reality and the COVID Mental Health Crisis. Scientific American. 2020. Available online: www.scientificamerican.com/article/virtual-reality-and-the-covid-mental-health-crisis (accessed on 30 October 2020).
- Eruchalu, C.N.; Pichardo, M.S.; Bharadwaj, M.; Rodriguez, C.B.; Rodriguez, J.A.; Bergmark, R.W.; Bates, D.W.; Ortega, G. The expanding digital divide: Digital health access inequities during the COVID-19 pandemic in New York City. J. Urban Health 2021, 98, 183–186. [Google Scholar] [CrossRef]
- Zhao, S.S.; Miller, N.; Harrison, N.; Duffield, S.J.; Dey, M.; Goodson, N.J. Systematic review of mental health comorbidities in psoriatic arthritis. Clin. Rheumatol. 2020, 39, 217–225. [Google Scholar] [CrossRef]
- Hadlaczky, G.; Hökby, S.; Mkrtchian, A.; Carli, V.; Wasserman, D. Mental Health First Aid is an effective public health intervention for improving knowledge, attitudes, and behavior: A meta-analysis. Int. Rev. Psychiatry 2014, 26, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Rozental, A.; Andersson, G.; Boettcher, J.; Eberte, D.D.; Cuijpers, P.; Knaevelsrudd, C.; Ljótssong, B.; Kaldoc, V.; Titovh, V.; Carlbringa, P. Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interv. 2014, 1, 12–19. [Google Scholar] [CrossRef]
- Jeffries, V.; Slaunwhite, A.; Wallace, N.; Menear, M.; Arndt, J.; Dotchin, J.; GermAnn, S.S.J. Collaborative Care for Mental Health and Substance Use Issues in Primary Health Care: Overview of Reviews and Narrative Summaries. Ottawa. 2013. Available online: www.mentalhealthcommission.ca/sites/default/files/PrimaryCare_Overview_Reviews_Narrative_Summaries_ENG_0.pdf (accessed on 21 January 2021).
- Huang, R.; Yan, C.; Tian, Y.; Lei, B.; Yang, D.; Liu, D.; Lei, J. Effectiveness of peer support intervention on perinatal depression: A systematic review and meta-analysis. J. Affect. Dis. 2020, 276, 788–796. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davison, K.M.; Thakkar, V.; Lin, S.; Stabler, L.; MacPhee, M.; Carroll, S.; Collins, B.; Rezler, Z.; Colautti, J.; Xu, C.; et al. Interventions to Support Mental Health among Those with Health Conditions That Present Risk for Severe Infection from Coronavirus Disease 2019 (COVID-19): A Scoping Review of English and Chinese-Language Literature. Int. J. Environ. Res. Public Health 2021, 18, 7265. https://doi.org/10.3390/ijerph18147265
Davison KM, Thakkar V, Lin S, Stabler L, MacPhee M, Carroll S, Collins B, Rezler Z, Colautti J, Xu C, et al. Interventions to Support Mental Health among Those with Health Conditions That Present Risk for Severe Infection from Coronavirus Disease 2019 (COVID-19): A Scoping Review of English and Chinese-Language Literature. International Journal of Environmental Research and Public Health. 2021; 18(14):7265. https://doi.org/10.3390/ijerph18147265
Chicago/Turabian StyleDavison, Karen M., Vidhi Thakkar, Shen (Lamson) Lin, Lorna Stabler, Maura MacPhee, Simon Carroll, Benjamin Collins, Zachary Rezler, Jake Colautti, Chaoqun (Cherry) Xu, and et al. 2021. "Interventions to Support Mental Health among Those with Health Conditions That Present Risk for Severe Infection from Coronavirus Disease 2019 (COVID-19): A Scoping Review of English and Chinese-Language Literature" International Journal of Environmental Research and Public Health 18, no. 14: 7265. https://doi.org/10.3390/ijerph18147265
APA StyleDavison, K. M., Thakkar, V., Lin, S., Stabler, L., MacPhee, M., Carroll, S., Collins, B., Rezler, Z., Colautti, J., Xu, C., Fuller-Thomson, E., Hey, B., Kelly, K., Mullaly, L., Remick, R., Ravindran, A., Paric, A., D’Andreamatteo, C., & Smye, V. (2021). Interventions to Support Mental Health among Those with Health Conditions That Present Risk for Severe Infection from Coronavirus Disease 2019 (COVID-19): A Scoping Review of English and Chinese-Language Literature. International Journal of Environmental Research and Public Health, 18(14), 7265. https://doi.org/10.3390/ijerph18147265





_Lin.jpg)



