Lonely in the City–Sociodemographic Status and Somatic Morbidities as Predictors of Loneliness and Depression among Seniors–Preliminary Results
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Group
- informed consent for participation in the study,
- age of at least sixty.
- lack of informed consent,
- diagnosis of major neurocognitive disorder,
- aphasia due to any reason,
- serious and unstable somatic disease,
- a severe psychological trauma within six months preceding the study,
- serious mental illness (e.g., schizophrenia or bipolar affective disorder or other psychotic disorder).
2.2. Operationalization of the Variables-Questionnaires
2.3. Ethical Considerations
2.4. Statistical Analysis
3. Results
3.1. Intergroup Comparisons by Place of Residence
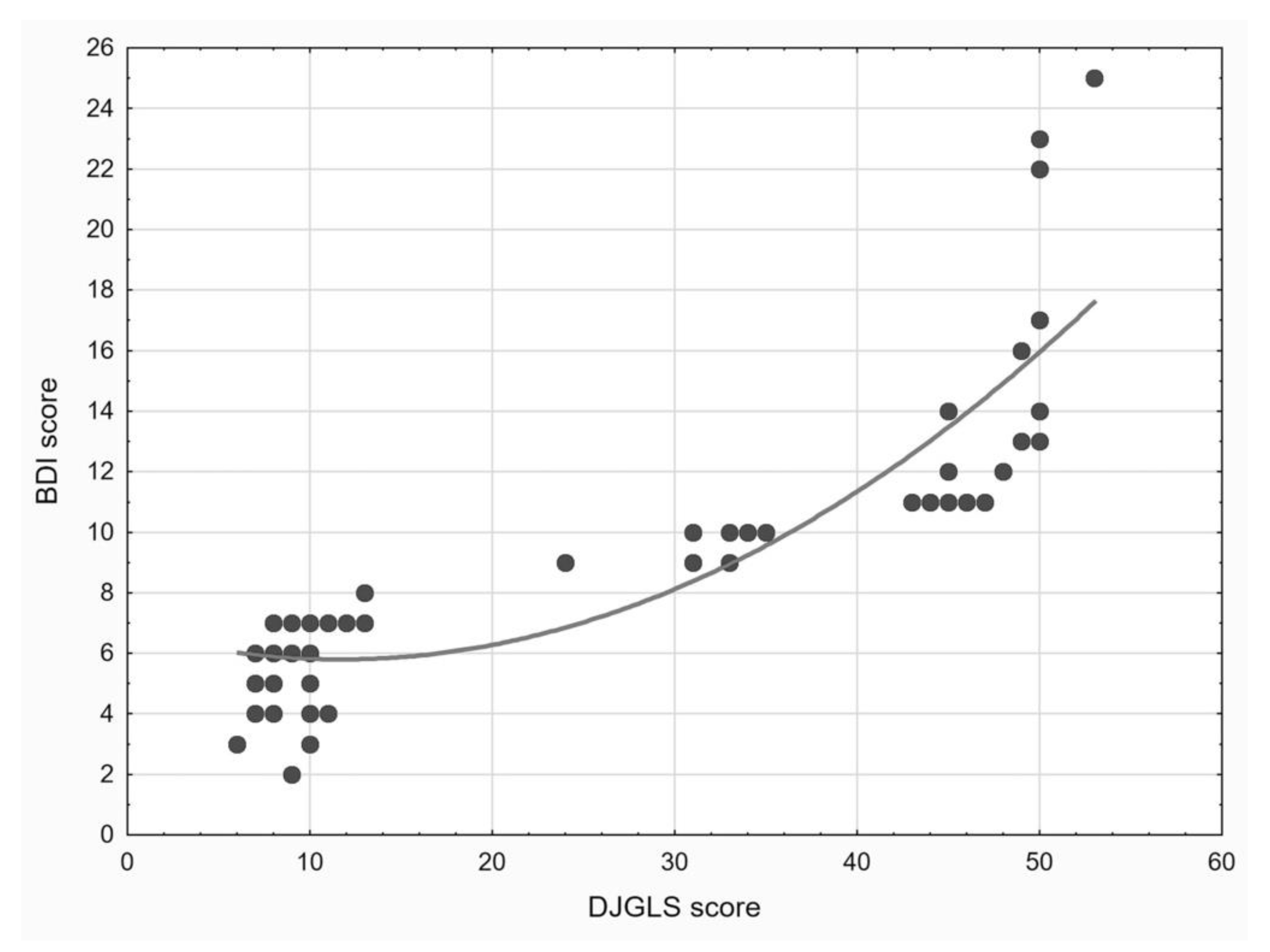
3.2. Correlation between Severity of Depression and Loneliness
3.3. Prediction of the Severity of Loneliness
3.4. Prediction of the Severity of Depression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Freedman, A.; Nicolle, J. Social Isolation and Loneliness: The New Geriatric Giants Approach for Primary Care. Can. Fam. Phys. 2020, 66, 176–182. [Google Scholar]
- Chang, E.S.; Kannoth, S.; Levy, S.; Wang, S.Y.; Lee, J.E.; Levy, B.R. Global Reach of Ageism on Older Persons’ Health: A Systematic Review. PLoS ONE 2020, 15. [Google Scholar] [CrossRef] [Green Version]
- Cacioppo, S.; Grippo, A.J.; London, S.; Goossens, L.; Cacioppo, J.T. Loneliness: Clinical Import and Interventions. Perspect. Psychol. Sci. 2015, 10, 238–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Jong Gierveld, J. A Review of Loneliness: Concept and Definitions, Determinants and Consequences. Rev. Clin. Gerontol. 1998, 8, 73–80. [Google Scholar] [CrossRef] [Green Version]
- Wenger, G.C.; Davies, R.; Shahtahmasebi, S.; Scott, A. Social Isolation and Loneliness in Old Age: Review and Model Refinement. Ageing Soc. 1996, 16, 333–358. [Google Scholar] [CrossRef] [Green Version]
- Rodda, J.; Walker, Z.; Carter, J. Depression in Older Adults. BMJ 2011, 343, d5219. [Google Scholar] [CrossRef]
- Fiske, A.; Wetherell, J.L.; Gatz, M. Depression in Older Adults. Annu. Rev. Clin. Psychol. 2009, 5, 363–389. [Google Scholar] [CrossRef]
- Jansson, A.H.; Savikko, N.M.; Pitkälä, K.H. Training Professionals to Implement a Group Model for Alleviating Loneliness among Older People—10-Year Follow-up Study. Educ. Gerontol. 2018, 44, 119–127. [Google Scholar] [CrossRef] [Green Version]
- Dykstra, P.A. Older Adult Loneliness: Myths and Realities. Eur. J. Ageing 2009, 6, 91. [Google Scholar] [CrossRef] [Green Version]
- National Academies of Sciences and Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; The National Academies Press: Washington, DC, USA, 2020; ISBN 978-0-309-67100-2. [Google Scholar]
- Rodriguez, H.; Brathwaite, D.; Dorsey, S. Depression and Social Support in the Elderly Population: A Study of Rural South African Elders. ABNF J. Off. J. Assoc. Black Nurs. Fac. High. Educ. Inc. 2002, 13, 45–48. [Google Scholar]
- Kok, R.M.; Reynolds, C.F. 3rd Management of Depression in Older Adults: A Review. JAMA 2017, 317, 2114–2122. [Google Scholar] [CrossRef] [PubMed]
- Meeks, T.W.; Vahia, I.V.; Lavretsky, H.; Kulkarni, G.; Jeste, D.V. A Tune in “a Minor” Can “b Major”: A Review of Epidemiology, Illness Course, and Public Health Implications of Subthreshold Depression in Older Adults. J. Affect. Disord. 2011, 129, 126–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Mental Health of Older Adults. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults (accessed on 7 June 2021).
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender Differences in Depression in Representative National Samples: Meta-Analyses of Diagnoses and Symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S.; Ahrens, C. Age Differences and Similarities in the Correlates of Depressive Symptoms. Psychol. Aging 2002, 17, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a Specific Risk Factor for Depressive Symptoms: Cross-Sectional and Longitudinal Analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Berg-Weger, M.; Morley, J.E. Loneliness in Old Age: An Unaddressed Health Problem. J. Nutr. Health Aging 2020, 24, 243–245. [Google Scholar] [CrossRef] [Green Version]
- Silverman, S.F. Agricultural Organization, Social Structure, and Values in Italy: Amoral Familism Reconsidered. Am. Anthropol. 1968, 70, 1–20. [Google Scholar] [CrossRef]
- Błachnio, A.; Buliński, L. Wellbeing and Older Adults in Primary Health Care in Poland. Ann. Agric. Environ. Med. 2019, 26, 55–61. [Google Scholar] [CrossRef]
- Barczykowska, A. Positive, Negative or Neutral?—Question about Nature of Social Capital. Studia Eduk. 2012, 81–95. Available online: https://repozytorium.amu.edu.pl/handle/10593/5880 (accessed on 7 June 2021). (In Polish).
- Tung, E.L.; Hawkley, L.C.; Cagney, K.A.; Peek, M.E. Social Isolation, Loneliness, And Violence Exposure In Urban Adults. Health Aff. 2019, 38, 1670–1678. [Google Scholar] [CrossRef]
- Patel, J.N.; Klein, D.S.; Sreekumar, S.; Liporace, F.A.; Yoon, R.S. Outcomes in Multidisciplinary Team-Based Approach in Geriatric Hip Fracture Care: A Systematic Review. J. Am. Acad. Orthop. Surg. 2020, 28, 128–133. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G.K. BDI-II. Manual, 2nd ed.; Test Laboratory of the Polish Psychological Association: Warsaw, Poland, 2019. [Google Scholar]
- Beck, A.T.; Steer, R.A.; Brown, G.K. BDI-II. Beck Depression Inventory; The Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Grygiel, P.; Humenny, G.; Rebisz, S.; Świtaj, P.; Sikorska, J. Validating the Polish Adaptation of the 11-Item De Jong Gierveld Loneliness Scale. Eur. J. Psychol. Assess. 2013, 29, 129–139. [Google Scholar] [CrossRef]
- Giza-Poleszczuk, A. Family and Social System. Reproduction and Cooperation in an Interdisciplinary Perspective; Wydawnictwo Uniwersytetu Warszawskiego: Warsaw, Poland, 2005. [Google Scholar]
- van Hout, E.; Peters, S.; Jansen, L.; Rober, P.; van den Akker, M. An Exploration of Spousal Caregivers’ Well-Being after the Death of Their Partners Who Were Older Cancer Patients—A Phenomenological Approach. Eur. J. Oncol. Nurs. 2020, 47, 101779. [Google Scholar] [CrossRef] [PubMed]
- Abbas Asghar-Ali, A.; Braun, U.K. Depression in Geriatric Patients. Minerva Med. 2009, 100, 105–113. [Google Scholar] [PubMed]
- Rondán-Cataluña, F.J.; Ramírez-Correa, P.E.; Arenas-Gaitán, J.; Ramírez-Santana, M.; Grandón, E.E.; Alfaro-Pérez, J. Social Network Communications in Chilean Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 6078. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Chen, H. Age Sequences of the Elderly’ Social Network and Its Efficacies on Well-Being: An Urban-Rural Comparison in China. BMC Geriatr. 2020, 20, 372. [Google Scholar] [CrossRef] [PubMed]
- León, L.P.; Mangin, J.P.; Ballesteros, S. Psychosocial Determinants of Quality of Life and Active Aging. A Structural Equation Model. Int. J. Environ. Res. Public Health 2020, 17, 6023. [Google Scholar] [CrossRef]
- Cybulski, M.; Cybulski, L.; Krajewska-Kulak, E.; Cwalina, U. Self-Assessment of the Mental Health Status in Older Adults in Poland: A Cross-Sectional Study. BMC Psychiatry 2017, 17, 383. [Google Scholar] [CrossRef] [Green Version]
- Tondo, L.; Vázquez, G.H.; Baldessarini, R.J. Depression and Mania in Bipolar Disorder. Curr. Neuropharmacol. 2017, 15, 353–358. [Google Scholar] [CrossRef] [Green Version]
- Smith, K.J.; Gavey, S.; RIddell, N.E.; Kontari, P.; Victor, C. The Association between Loneliness, Social Isolation and Inflammation: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2020, 112, 519–541. [Google Scholar] [CrossRef]
- Deckx, L.; van den Akker, M.; Buntinx, F. Risk Factors for Loneliness in Patients with Cancer: A Systematic Literature Review and Meta-Analysis. Eur. J. Oncol. Nurs. 2014, 18, 466–477. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, B.J.; Jayakody, D.M.P.; Bennett, R.J.; Eikelboom, R.H.; Gasson, N.; Friedland, P.L. Hearing Loss and Depression in Older Adults: A Systematic Review and Meta-Analysis. Gerontology 2020, 60, e137–e154. [Google Scholar] [CrossRef] [PubMed]
- Alpass, F.M.; Neville, S. Loneliness, Health and Depression in Older Males. Aging Ment. Health 2003, 7, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hawkley, L.C.; Thisted, R.A. Perceived Social Isolation Makes Me Sad: 5-Year Cross-Lagged Analyses of Loneliness and Depressive Symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol. Aging 2010, 25, 453–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, K.B.; Sanders, S.; Auth, E.A. Loneliness and Depression in Independent Living Retirement Communities: Risk and Resilience Factors. Aging Ment. Health 2004, 8, 475–485. [Google Scholar] [CrossRef] [PubMed]
- Theeke, L.A.; Goins, R.T.; Moore, J.; Campbell, H. Loneliness, Depression, Social Support, and Quality of Life in Older Chronically Ill Appalachians. J. Psychol. 2012, 146, 155–171. [Google Scholar] [CrossRef]
- Paul, C.; Ayis, S.; Ebrahim, S. Psychological Distress, Loneliness and Disability in Old Age. Psychol. Health Med. 2006, 11, 221–232. [Google Scholar] [CrossRef]
| City (n = 47) | Rural Area (n = 45) | |
|---|---|---|
| Age, M ± SD (min-max) * | 68.9 ± 4.6 (65–85) | 71.6 ± 5.5 (64–85) |
| Female sex, n (%) | 27 (57%) | 32 (71%) |
| Current income monthly in PLN, M ± SD (min-max) ** | 1773.0 ± 323.3 (1280–2700) | 1505.4 ± 192.6 (1200–1950) |
| Number of children, n (%): ** | ||
| none | 10 (21%) | 0 (0%) |
| one | 22 (47%) | 4 (9%) |
| two | 12 (26%) | 21 (29%) |
| three | 3 (6%) | 13 (29%) |
| four | 0 (0%) | 5 (11%) |
| five | 0 (0%) | 2 (4%) |
| Marital status, n (%): | ||
| single | 5 (11%) | 0 (0%) |
| married | 25 (53%) | 32 (71%) |
| widowed | 7 (15%) | 10 (22%) |
| divorced | 10 (21%) | 3 (7%) |
| Informal relationship, n (%) | 6 (13%) | 2 (4%) |
| Place of habitat, n (%): ** | ||
| house | 10 (21%) | 44 (98%) |
| flat | 37 (79%) | 1 (2%) |
| Co-inhabitants, n (%): ** | ||
| lives alone | 13 (34%) | 3 (7%) |
| with spouse only | 20 (43%) | 12 (27%) |
| with children only | 1 (2%) | 8 (18%) |
| with spouse and children | 5 (11%) | 20 (44%) |
| with other close person | 5 (11%) | 2 (4%) |
| Morbidities, n (%): | ||
| Type 2 diabetes | 12 (26%) | 14 (31%) |
| Arterial hypertension | 12 (25%) | 8 (18%) |
| Heart failure | 9 (19%) | 7 (16%) |
| Upper gastrointestinal tract disease | 3 (6%) | 5 (11%) |
| Arthritis (rheumathoid or ostheoarthritis) | 2 (4%) | 3 (7%) |
| Asthma | 1 (2%) | 1 (2%) |
| Stroke in the past | 1 (2%) | 1 (2%) |
| Visual impairment (e.g., cataract) | 2 (4%) | 4 (9%) |
| Neoplasm | 2 (4%) | 0 (0%) |
| Other | 10 (21%) | 4 (9%) |
| BDI score, M ± SD (min-max) ** | 9.6 ± 4.9 (4–25) | 6.1 ± 1.9 (2–11) |
| DJGS score, M ± SD (min-max) ** | 26.4 ± 17.6 (8–53) | 11.4 ± 9.1 (6–46) |
| B | B 95%CI | sR | |||
|---|---|---|---|---|---|
| Intercept | 27.799 * | 3.008 | 52.591 | ||
| Age | −0.034 | −0.366 | 0.299 | −0.008 | |
| Female sex | 1.750 | −0.005 | 3.505 | 0.079 | |
| Number of children | −2.826 ** | −4.604 | −1.048 | −0.126 | |
| Marital status | single vs. married | −2.227 | −8.639 | 4.185 | −0.027 |
| widowed vs. married | −2.120 | −8.766 | 4.525 | −0.025 | |
| divorced vs. married | −4.377 * | −7.740 | −1.014 | −0.103 | |
| Place of residence-city vs. rural area | 1.819 | −0.640 | 4.277 | 0.059 | |
| Place of habitat-flat vs. house | −2.255 | −4.671 | 0.161 | −0.074 | |
| Co-inhabitants | alone vs. with spouse | 29.727 † | 22.344 | 37.111 | 0.319 |
| with children only vs. with spouse | −1.505 | −11.709 | 8.699 | −0.012 | |
| with spouse and children vs. with spouse | −15.157 † | −23.453 | −6.861 | −0.145 | |
| Monthly income (pension) | 0.004 | −0.003 | 0.010 | 0.045 | |
| Visual impairment | −1.208 | −4.312 | 1.896 | −0.031 | |
| Neoplasm | 11.390† | 6.441 | 16.339 | 0.182 | |
| B | B 95%CI | sR | |||
|---|---|---|---|---|---|
| Intercept | 9.916 ** | 2.902 | 16.930 | ||
| Age | 0.071 | −0.021 | 0.164 | 0.064 | |
| Female sex | 0.529 * | 0.055 | 1.004 | 0.093 | |
| Number of children | −0.874 ** | −1.355 | −0.393 | −0.151 | |
| Marital status | single vs. married | 0.318 | −1.475 | 2.112 | 0.015 |
| widowed vs. married | −0.745 | −2.550 | 1.061 | −0.034 | |
| divorced vs. married | −0.686 | −1.610 | 0.238 | −0.062 | |
| Place of residence-city vs. rural area | 0.010 | −0.659 | 0.679 | 0.001 | |
| Place of habitat-flat vs. house | −0.007 | −0.661 | 0.647 | −0.001 | |
| Co-inhabitants | alone vs. with spouse | 4.823 † | 2.826 | 6.820 | 0.201 |
| with children only vs. with spouse | −0.007 | −2.779 | 2.764 | 0.000 | |
| with spouse and children vs. with spouse | −2.490 * | −4.734 | −0.246 | −0.092 | |
| Monthly income | 0.002 | 0.000 | 0.003 | 0.075 | |
| Asthma | 2.049 ** | 0.774 | 3.325 | 0.134 | |
| Diabetes mellitus | 0.167 | −0.278 | 0.613 | 0.031 | |
| Visual impairment | −0.315 | −1.178 | 0.547 | −0.030 | |
| Neoplasm | 6.769 † | 5.406 | 8.132 | 0.413 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sipowicz, K.; Podlecka, M.; Mokros, Ł.; Pietras, T. Lonely in the City–Sociodemographic Status and Somatic Morbidities as Predictors of Loneliness and Depression among Seniors–Preliminary Results. Int. J. Environ. Res. Public Health 2021, 18, 7213. https://doi.org/10.3390/ijerph18147213
Sipowicz K, Podlecka M, Mokros Ł, Pietras T. Lonely in the City–Sociodemographic Status and Somatic Morbidities as Predictors of Loneliness and Depression among Seniors–Preliminary Results. International Journal of Environmental Research and Public Health. 2021; 18(14):7213. https://doi.org/10.3390/ijerph18147213
Chicago/Turabian StyleSipowicz, Kasper, Marlena Podlecka, Łukasz Mokros, and Tadeusz Pietras. 2021. "Lonely in the City–Sociodemographic Status and Somatic Morbidities as Predictors of Loneliness and Depression among Seniors–Preliminary Results" International Journal of Environmental Research and Public Health 18, no. 14: 7213. https://doi.org/10.3390/ijerph18147213
APA StyleSipowicz, K., Podlecka, M., Mokros, Ł., & Pietras, T. (2021). Lonely in the City–Sociodemographic Status and Somatic Morbidities as Predictors of Loneliness and Depression among Seniors–Preliminary Results. International Journal of Environmental Research and Public Health, 18(14), 7213. https://doi.org/10.3390/ijerph18147213







