Prevalence of High Resilience in Old Age and Association with Perceived Threat of COVID-19—Results from a Representative Survey
Abstract
:1. Introduction
- What is the prevalence rate of high resilience within a representative sample of the German old age population (65+)?
- How are socio-demographic factors associated with high resilience in the old age population?
- How is high resilience associated with the perceived threat of COVID-19 in the old age population?
2. Materials and Methods
2.1. Study Design and Sample
2.2. Assessments
2.2.1. Socio-Demographic Characteristics
2.2.2. Perceived Threat of COVID-19
2.2.3. High Resilience
2.3. Data Analysis
3. Results
3.1. Prevalence of Resilience
3.2. High Resilience and Socio-Demographic Characteristics
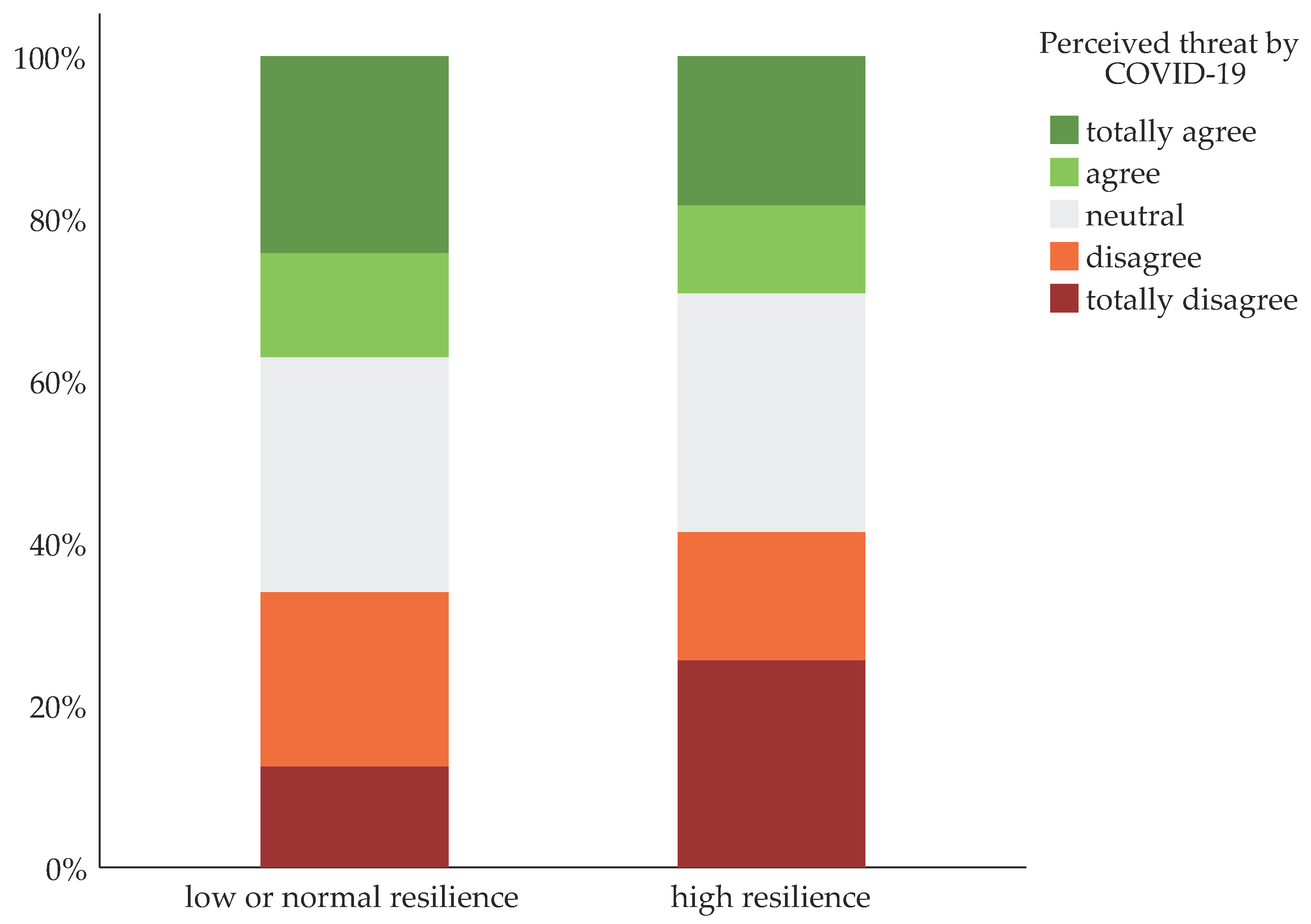
3.3. Resilience and the Perceived Threat of COVID-19
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Luthar, S.S.; Cicchetti, D. The construct of resilience: Implications for interventions and social policies. Dev. Psychopathol. 2000, 12, 857–885. [Google Scholar] [CrossRef] [PubMed]
- APA. Building Your Resilience. Available online: http://www.apa.org/topics/resilience (accessed on 1 February 2021).
- MacLeod, S.; Musich, S.; Hawkins, K.; Alsgaard, K.; Wicker, E.R. The impact of resilience among older adults. Geriatr. Nurs. 2016, 37, 266–272. [Google Scholar] [CrossRef] [Green Version]
- Hardy, S.E.; Concato, J.; Gill, T.M. Resilience of community-dwelling older persons. J. Am. Geriatr. Soc. 2004, 52, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Netuveli, G.; Wiggins, R.D.; Montgomery, S.M.; Hildon, Z.; Blane, D. Mental health and resilience at older ages: Bouncing back after adversity in the British Household Panel Survey. J. Epidemiol. Community Health 2008, 62, 987–991. [Google Scholar] [CrossRef]
- Hildon, Z.; Montgomery, S.M.; Blane, D.; Wiggins, R.D.; Netuveli, G. Examining resilience of quality of life in the face of health-related and psychosocial adversity at older ages: What is “right” about the way we age? Gerontologist 2010, 50, 36–47. [Google Scholar] [CrossRef]
- Wells, M. Resilience in Older Adults Living in Rural, Suburban, and Urban Areas. OJRNHC 2010, 10, 45–54. [Google Scholar] [CrossRef]
- Perna, L.; Mielck, A.; Lacruz, M.E.; Emeny, R.T.; Holle, R.; Breitfelder, A.; Ladwig, K.H. Socioeconomic position, resilience, and health behaviour among elderly people. Int. J. Public Health 2012, 57, 341–349. [Google Scholar] [CrossRef]
- Dray, J.; Bowman, J.; Campbell, E.; Freund, M.; Wolfenden, L.; Hodder, R.K.; McElwaine, K.; Tremain, D.; Bartlem, K.; Bailey, J.; et al. Systematic Review of Universal Resilience-Focused Interventions Targeting Child and Adolescent Mental Health in the School Setting. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 813–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8, e017858. [Google Scholar] [CrossRef] [Green Version]
- Gooding, P.A.; Hurst, A.; Johnson, J.; Tarrier, N. Psychological resilience in young and older adults. Int. J. Geriatr. Psychiatry 2012, 27, 262–270. [Google Scholar] [CrossRef]
- Wells, M. Resilience in Rural Community-Dwelling Older Adults. J. Rural Health 2009, 25, 415–419. [Google Scholar] [CrossRef]
- Nygren, B.; Aléx, L.; Jonsén, E.; Gustafson, Y.; Norberg, A.; Lundman, B. Resilience, sense of coherence, purpose in life and self-transcendence in relation to perceived physical and mental health among the oldest old. Aging Ment. Health 2005, 9, 354–362. [Google Scholar] [CrossRef]
- Glonti, K.; Gordeev, V.S.; Goryakin, Y.; Reeves, A.; Stuckler, D.; McKee, M.; Roberts, B. A systematic review on health resilience to economic crises. PLoS ONE 2015, 10, e0123117. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Wagnild, G.M.; Young, H.M. Development and Psychometric Evaluation of the Resilience Scale. J. Nurs. Meas. 1993, 1, 165–178. [Google Scholar]
- Friborg, O.; Hjemdal, O.; Rosenvinge, J.H.; Martinussen, M. A new rating scale for adult resilience: What are the central protective resources behind healthy adjustment? Int. J. Methods Psychiatr. Res. 2003, 12, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, V.G.; Wallston, K.A. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef]
- Whatnall, M.C.; Patterson, A.J.; Siew, Y.Y.; Kay-Lambkin, F.; Hutchesson, M.J. Are Psychological Distress and Resilience Associated with Dietary Intake Among Australian University Students? Int. J. Environ. Res. Public Health 2019, 16, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Labrague, L.J.; de Los Santos, J.A.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef]
- Woods-Jaeger, B.; Siedlik, E.; Adams, A.; Piper, K.; O’Connor, P.; Berkley-Patton, J. Building a Contextually-Relevant Understanding of Resilience among African American Youth Exposed to Community Violence. Behav. Med. 2020, 46, 330–339. [Google Scholar] [CrossRef]
- Riedel-Heller, S.; Richter, D. COVID-19-Pandemie trifft auf Psyche der Bevölkerung: Gibt es einen Tsunami psychischer Störungen? Psychiatr. Prax. 2020, 47, 452–456. [Google Scholar] [CrossRef]
- Noor, F.M.; Islam, M.M. Prevalence and Associated Risk Factors of Mortality among COVID-19 Patients: A Meta-Analysis. J. Community Health 2020, 45, 1270–1282. [Google Scholar] [CrossRef]
- Nwachukwu, I.; Nkire, N.; Shalaby, R.; Hrabok, M.; Vuong, W.; Gusnowski, A.; Surood, S.; Urichuk, L.; Greenshaw, A.J.; Agyapong, V.I.O. COVID-19 Pandemic: Age-Related Differences in Measures of Stress, Anxiety and Depression in Canada. Int. J. Environ. Res. Public Health 2020, 17, 6366. [Google Scholar] [CrossRef] [PubMed]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Röhr, S.; Reininghaus, U.; Riedel-Heller, S.G. Mental wellbeing in the German old age population largely unaltered during COVID-19 lockdown: Results of a representative survey. BMC Geriatr. 2020, 20, 489. [Google Scholar] [CrossRef] [PubMed]
- López, J.; Perez-Rojo, G.; Noriega, C.; Carretero, I.; Velasco, C.; Martinez-Huertas, J.A.; López-Frutos, P.; Galarraga, L. Psychological well-being among older adults during the COVID-19 outbreak: A comparative study of the young–old and the old–old adults. Int. Psychogeriatr. 2020, 18, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Plomecka, M.B.; Gobbi, S.; Neckels, R.; Radziński, P.; Skórko, B.; Lazerri, S.; Almazidou, K.; Dedić, A.; Bakalović, A.; Hrustić, L.; et al. Mental Health Impact of COVID-19: A global study of risk and resilience factors. medRxiv 2020. [Google Scholar] [CrossRef]
- Thyrian, J.R.; Kracht, F.; Nikelski, A.; Boekholt, M.; Schumacher-Schönert, F.; Rädke, A.; Michalowsky, B.; Vollmar, H.C.; Hoffmann, W.; Rodriguez, F.S.; et al. The situation of elderly with cognitive impairment living at home during lockdown in the Corona-pandemic in Germany. BMC Geriatr. 2020, 20, 540. [Google Scholar] [CrossRef]
- Killgore, W.D.S.; Taylor, E.C.; Cloonan, S.A.; Dailey, N.S. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020, 291, 113216. [Google Scholar] [CrossRef] [PubMed]
- Barzilay, R.; Moore, T.M.; Greenberg, D.M.; DiDomenico, G.E.; Brown, L.A.; White, L.K.; Gur, R.C.; Gur, R.E. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl. Psychiatry 2020, 10, 291. [Google Scholar] [CrossRef]
- Gao, S.; Burney, H.N.; Callahan, C.M.; Purnell, C.E.; Hendrie, H.C. Incidence of Dementia and Alzheimer Disease Over Time: A Meta-Analysis. J. Am. Geriatr. Soc. 2019, 67, 1361–1369. [Google Scholar] [CrossRef]
- Brauns, H.; Scherer, S.; Steinmann, S. The CASMIN Educational Classification in International Comparative Research. In Advances in Cross-National Comparison; Springer: Boston, MA, USA, 2003. [Google Scholar]
- Chmitorz, A.; Wenzel, M.; Stieglitz, R.-D.; Kunzler, A.; Bagusat, C.; Helmreich, I.; Gerlicher, A.; Kampa, M.; Kubiak, T.; Kalisch, R.; et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE 2018, 13, e0192761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCullagh, P. Regression Models for Ordinal Data. J. R. Stat. Soc. Ser. B (Methodol.) 1980, 42, 109–142. [Google Scholar] [CrossRef]
- Stein, J.; Bär, J.M.; König, H.-H.; Angermeyer, M.; Riedel-Heller, S.G. Soziale Verlusterlebnisse und deren Zusammenhang mit Depressionen im hohen Alter—Ergebnisse der Leipziger Langzeitstudie in der Altenbevölkerung (LEILA 75+). Psychiatr. Prax. 2019, 46, 141–147. [Google Scholar] [CrossRef]
- Leopold, L. Education and Physical Health Trajectories in Later Life: A Comparative Study. Demography 2018, 55, 901–927. [Google Scholar] [CrossRef] [Green Version]
- Röhr, S.; Müller, F.; Jung, F.; Apfelbacher, C.; Seidler, A.; Riedel-Heller, S.G. Psychosoziale Folgen von Quarantänemaßnahmen bei schwerwiegenden Coronavirus-Ausbrüchen: Ein Rapid Review. Psychiatr. Prax. 2020, 47, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-Y.; Tung, H.-H.; Peng, L.-N.; Chen, L.-K.; Hsu, C.-I.; Huang, Y.-L. Resilience among older cardiovascular disease patients with probable sarcopenia. Arch. Gerontol. Geriatr. 2020, 86, 103939. [Google Scholar] [CrossRef]
| Total | Low or Normal Resilience | High Resilience | ||||||
|---|---|---|---|---|---|---|---|---|
| n | n | % | 95% CI | n | % | 95% CI | p | |
| Total | 954 | 768 | 81.3 | [78.8; 83.3] | 186 | 18.7 | [16.3; 21.2] | |
| Age group in years | 954 | 0.002 | ||||||
| 65-74 | 466 | 359 | 77.3 | [73.3; 80.9] | 107 | 22.7 | [19.1; 26.7] | |
| ≥ 75 | 488 | 409 | 85.2 | [81.9; 88.1] | 79 | 14.8 | [11.9; 18.1] | |
| Gender | 954 | 0.085 | ||||||
| Male | 466 | 325 | 78.9 | [74.8; 82.6] | 90 | 21.1 | [17.4; 25.2] | |
| Female | 488 | 443 | 83.3 | [79.9; 86.2] | 96 | 16.7 | [13.8; 20.1] | |
| Marital status | 950 | 0.486 | ||||||
| Married | 449 | 363 | 80.5 | [77.0; 83.7] | 86 | 19.5 | [16.3; 23.0] | |
| Single/divorced/widowed | 501 | 402 | 82.3 | [78.4; 85.7] | 99 | 17.7 | [14.3; 21.6] | |
| Education | 943 | 0.001 | ||||||
| Low | 273 | 241 | 88.8 | [84.6; 82.2] | 32 | 11.2 | [7.8; 15.4] | |
| Middle | 332 | 259 | 78.6 | [73.7; 82.5] | 73 | 21.4 | [17.2; 26.0] | |
| High | 338 | 258 | 78.2 | [73.6; 82.3] | 80 | 21.8 | [17.7; 26.4] | |
| Total | Low or Normal Resilience | High Resilience | Group Difference | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p | |
| Perceived threat of COVID-19 | <0.001 | ||||||
| Strongly disagree | 143 | 14.8 | 97 | 12.4 | 46 | 25.5 | |
| Disagree | 197 | 20.5 | 163 | 21.5 | 34 | 15.8 | |
| Neither agree nor disagree | 277 | 29.0 | 221 | 28.9 | 56 | 29.4 | |
| Agree | 122 | 12.5 | 106 | 12.9 | 16 | 10.9 | |
| Strongly Agree | 214 | 23.2 | 180 | 24.3 | 34 | 18.4 | |
| Perceived threat of COVID-19 | |||
|---|---|---|---|
| OR | 95% CI | p | |
| Socio-demographic factors | |||
| Gender (ref. male) | |||
| Female | 0.978 | [0.767; 1.246] | 0.856 |
| Age group in years (ref. 65–74) | |||
| ≥ 75 | 1.175 | [0.931; 1.482] | 0.175 |
| Marital status (ref. married) | |||
| Single/ divorced/ widowed | 0.892 | [0.700; 1.135] | 0.353 |
| Education (ref. high) | |||
| Low | 1.101 | [0.823; 1.472] | 0.517 |
| Middle | 0.876 | [0.666; 1.151] | 0.342 |
| Resilience | |||
| Resilience (ref. low/normal) | |||
| high | 0.657 | [0.490; 0.883] | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weitzel, E.C.; Löbner, M.; Röhr, S.; Pabst, A.; Reininghaus, U.; Riedel-Heller, S.G. Prevalence of High Resilience in Old Age and Association with Perceived Threat of COVID-19—Results from a Representative Survey. Int. J. Environ. Res. Public Health 2021, 18, 7173. https://doi.org/10.3390/ijerph18137173
Weitzel EC, Löbner M, Röhr S, Pabst A, Reininghaus U, Riedel-Heller SG. Prevalence of High Resilience in Old Age and Association with Perceived Threat of COVID-19—Results from a Representative Survey. International Journal of Environmental Research and Public Health. 2021; 18(13):7173. https://doi.org/10.3390/ijerph18137173
Chicago/Turabian StyleWeitzel, Elena Caroline, Margrit Löbner, Susanne Röhr, Alexander Pabst, Ulrich Reininghaus, and Steffi G. Riedel-Heller. 2021. "Prevalence of High Resilience in Old Age and Association with Perceived Threat of COVID-19—Results from a Representative Survey" International Journal of Environmental Research and Public Health 18, no. 13: 7173. https://doi.org/10.3390/ijerph18137173
APA StyleWeitzel, E. C., Löbner, M., Röhr, S., Pabst, A., Reininghaus, U., & Riedel-Heller, S. G. (2021). Prevalence of High Resilience in Old Age and Association with Perceived Threat of COVID-19—Results from a Representative Survey. International Journal of Environmental Research and Public Health, 18(13), 7173. https://doi.org/10.3390/ijerph18137173






