Effectiveness of Text Messaging as an Incentive to Maintain Physical Activity after Cardiac Rehabilitation: A Randomized Controlled Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Participants
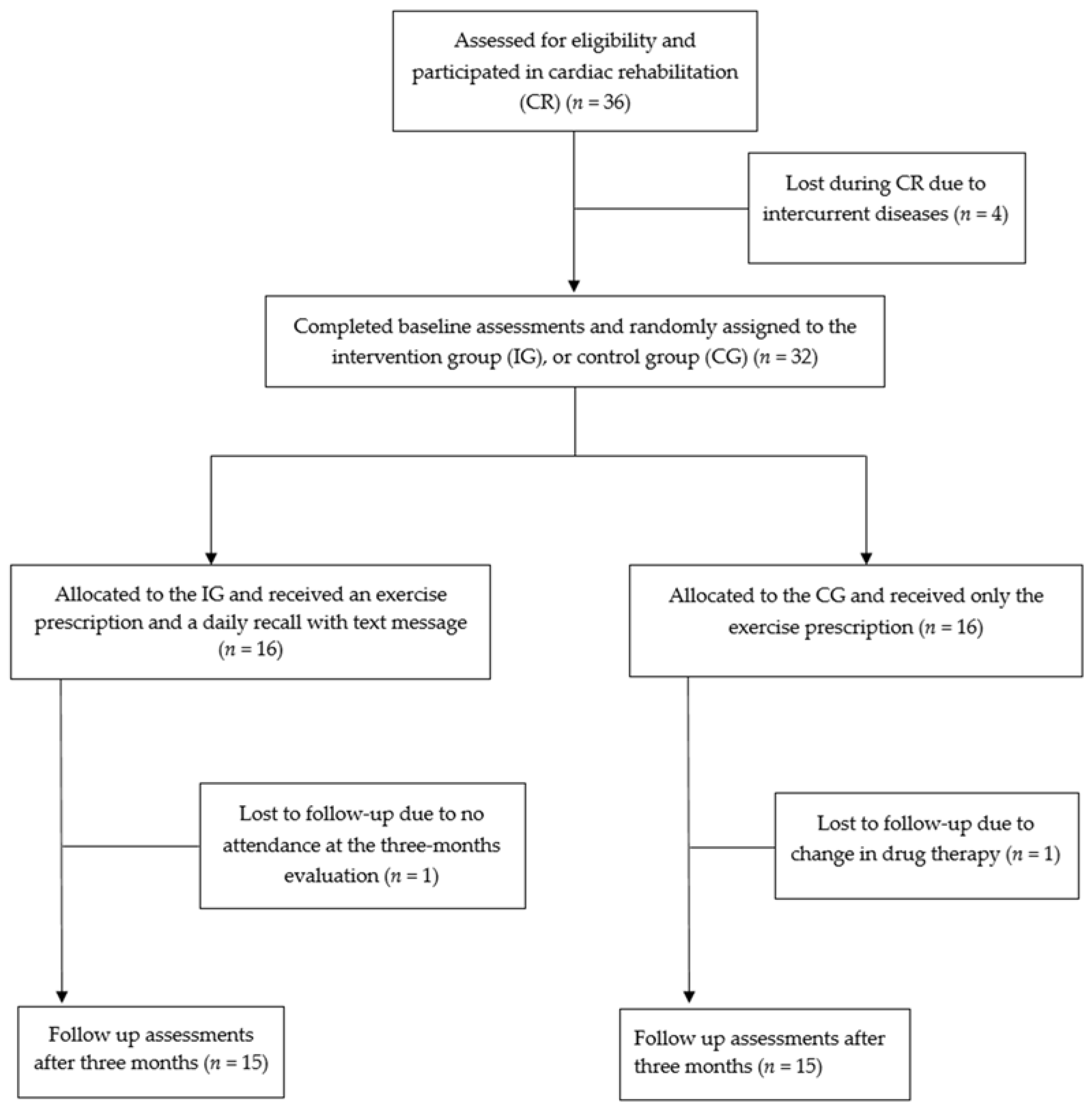
2.2. Design
2.3. Intervention
2.4. Endpoints and Assessments
2.5. Statistical Analyses
3. Results
3.1. Characteristics of the Study Population
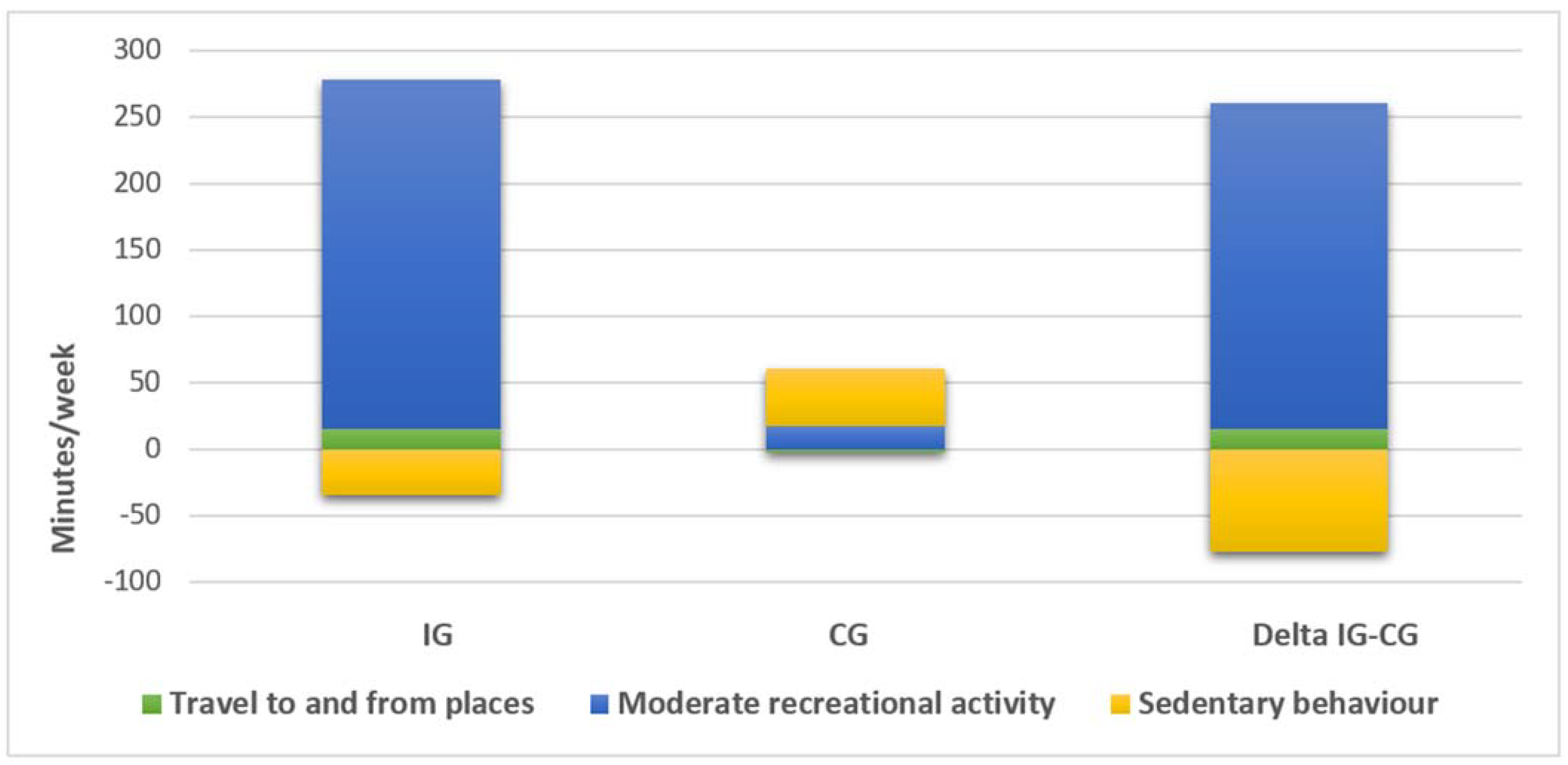
3.2. GPAQ
3.3. Submaximal Iso-Watt Exercise Test
3.4. Strength Tests
3.5. Final Follow-Up Survey
4. Discussion
Limitations and Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur. Heat. J. 2016, 37, 3232–3245. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Ajani, U.A.; Croft, J.B.; Critchley, J.A.; Labarthe, D.R.; Kottke, T.E.; Giles, W.H.; Capewell, S. Explaining the Decrease in US Deaths from Coronary Disease, 1980–2000. Surv. Anesthesiol. 2007, 51, 326. [Google Scholar] [CrossRef]
- Task Force Members; Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. J. Prev. Cardiol. 2016, 23, NP1–NP96. [Google Scholar] [CrossRef]
- Anderson, L.; Oldridge, N.; Thompson, D.; Zwisler, A.-D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease. J. Am. Coll. Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef]
- Brawner, C.A.; Girdano, D.; Ehrman, J.K.; Keteyian, S.J. Association between Phase 3 Cardiac Rehabilitation and Clinical Events. J. Cardiopulm. Rehabil. Prev. 2017, 37, 111–118. [Google Scholar] [CrossRef]
- Ruano-Ravina, A.; Pena-Gil, C.; Abu-Assi, E.; Raposeiras, S.; van’t Hof, A.; Meindersma, E.; Prescott, E.I.B.; González-Juanatey, J.R. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int. J. Cardiol. 2016, 223, 436–443. [Google Scholar] [CrossRef]
- Zores, F.; Iliou, M.-C.; Gellen, B.; Kubas, S.; Berthelot, E.; Guillo, P.; Bauer, F.; Lamblin, N.; Bosser, G.; Damy, T.; et al. Physical activity for patients with heart failure: Position paper from the heart failure (GICC) and cardiac rehabilitation (GERS-P) Working Groups of the French Society of Cardiology. Arch. Cardiovasc. Dis. 2019, 112, 723–731. [Google Scholar] [CrossRef]
- Murphy, R.L.; Bird, K.T. Telediagnosis: A new community health resource. Observations on the feasibility of telediagnosis based on 1000 patient transactions. Am. J. Public Health 1974, 64, 113–119. [Google Scholar] [CrossRef]
- Palmer, M.J.; Barnard, S.; Perel, P.; Free, C. Mobile phone-based interventions for improving adherence to medication prescribed for the primary prevention of cardiovascular disease in adults. Cochrane Database Syst. Rev. 2018, 6, CD012675. [Google Scholar] [CrossRef]
- Gandhi, S.; Chen, S.; Hong, L.; Sun, K.; Gong, E.; Li, C.; Yan, L.L.; Schwalm, J.-D. Effect of Mobile Health Interventions on the Secondary Prevention of Cardiovascular Disease: Systematic Review and Meta-analysis. Can. J. Cardiol. 2017, 33, 219–231. [Google Scholar] [CrossRef] [PubMed]
- Boesch, C.; Myers, J.; Habersaat, A.; Ilarraza, H.; Kottman, W.; Dubach, P. Maintenance of Exercise Capacity and Physical Activity Patterns 2 Years after Cardiac Rehabilitation. J. Cardiopulm. Rehabil. 2005, 25, 14–21. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Holmbäck, A.M.; Säwe, U.; Fagher, B. Training after myocardial infarction: Lack of long-term effects on physical capacity and psychological variables. Arch. Phys. Med. Rehabil. 1994, 75, 551–554. [Google Scholar] [PubMed]
- Ståhle, A.; Mattsson, E.; Rydén, L.; Unden, A.-L.; Nordlander, R. Improved physical fitness and quality of life following training of elderly patients after acute coronary events. A 1 year follow-up randomized controlled study. Eur. Heat. J. 1999, 20, 1475–1484. [Google Scholar] [CrossRef] [PubMed]
- Hage, C.; Mattsson, E.; Ståhle, A. Long-term effects of exercise training on physical activity level and quality of life in elderly coronary patients—A three- to six-year follow-up. Physiother. Res. Int. 2003, 8, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Lunde, P.; Bye, A.; Bergland, A.; Grimsmo, J.; Jarstad, E.; Nilsson, B.B. Long-term follow-up with a smartphone application improves exercise capacity post cardiac rehabilitation: A randomized controlled trial. Eur. J. Prev. Cardiol. 2020, 27, 1782–1792. [Google Scholar] [CrossRef]
- Zheng, X.; Spatz, E.S.; Bai, X.; Huo, X.; Ding, Q.; Horak, P.; Wu, X.; Guan, W.; Chow, C.K.; Yan, X.; et al. Effect of Text Messaging on Risk Factor Management in Patients with Coronary Heart Disease. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005616. [Google Scholar] [CrossRef]
- Pandey, A.; Krumme, A.A.; Patel, T.; Choudhry, N.K.; Vervloet, M.; Gatwood, J.; Holtz, B. The Impact of Text Messaging on Medication Adherence and Exercise Among Postmyocardial Infarction Patients: Randomized Controlled Pilot Trial. JMIR mHealth uHealth 2017, 5, e110. [Google Scholar] [CrossRef]
- Thakkar, J.; Redfern, J.; Thiagalingam, A.; Chow, C.K. Patterns, predictors and effects of texting intervention on physical activity in CHD—Insights from the TEXT ME randomized clinical trial. Eur. J. Prev. Cardiol. 2016, 23, 1894–1902. [Google Scholar] [CrossRef]
- Dale, L.P.; Whittaker, R.; Jiang, Y.; Stewart, R.; Rolleston, A.; Maddison, R. Text Message and Internet Support for Coronary Heart Disease Self-Management: Results from the Text4Heart Randomized Controlled Trial. J. Med Internet Res. 2015, 17, e237. [Google Scholar] [CrossRef]
- Frederix, I.; Van Driessche, N.; Hansen, D.; Berger, J.; Bonne, K.; Alders, T.; Dendale, P. Increasing the medium-term clinical benefits of hospital-based cardiac rehabilitation by physical activity telemonitoring in coronary artery disease patients. Eur. J. Prev. Cardiol. 2015, 22, 150–158. [Google Scholar] [CrossRef]
- Frederix, I.; Hansen, D.; Coninx, K.; Vandervoort, P.; Vandijck, D.; Hens, N.; Van Craenenbroeck, E.; Van Driessche, N.; Dendale, P. Medium-Term Effectiveness of a Comprehensive Internet-Based and Patient-Specific Telerehabilitation Program with Text Messaging Support for Cardiac Patients: Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e185. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.K.; Redfern, J.; Hillis, G.S.; Thakkar, J.; Santo, K.; Hackett, M.; Jan, S.; Graves, N.; De Keizer, L.; Barry, T.; et al. Effect of Lifestyle-Focused Text Messaging on Risk Factor Modification in Patients with Coronary Heart Disease. JAMA 2015, 314, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Chow, S.-C.; Shao, J.; Wang, H.; Lokhnygina, Y. Sample Size Calculations in Clinical Research, 3rd ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 2017. [Google Scholar]
- Neunhäuserer, D.; Reich, B.; Mayr, B.; Kaiser, B.; Lamprecht, B.; Niederseer, D.; Ermolao, A.; Studnicka, M.; Niebauer, J. Impact of exercise training and supplemental oxygen on submaximal exercise performance in patients with COPD. Scand. J. Med. Sci. Sports 2021, 31, 710–719. [Google Scholar] [CrossRef]
- Myers, J.; Prakash, M.; Froelicher, V.; Do, D.; Partington, S.; Atwood, J.E. Exercise Capacity and Mortality among Men Referred for Exercise Testing. N. Engl. J. Med. 2002, 346, 793–801. [Google Scholar] [CrossRef]
- Ozyemisci-Taskiran, O.; Demirsoy, N.; Atan, T.; Yuksel, S.; Coskun, O.; Aytur, Y.K.; Tur, B.S.; Karakas, M.; Turak, O.; Topal, S. Development and Validation of a Scale to Measure Fear of Activity in Patients with Coronary Artery Disease (Fact-CAD). Arch. Phys. Med. Rehabil. 2020, 101, 479–486. [Google Scholar] [CrossRef]
- Foccardi, G.; Hansen, D.; Quinto, G.; Favero, C.; Coninx, K.; Ruiz, G.R.; Dendale, P.; Niebauer, J.; Ermolao, A.; Neunhaeuserer, D. How do General Practitioners assess physical activity and prescribe exercise in patients with different cardiovascular diseases? An Italian pilot study. Eur. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Hansen, D.; Dendale, P.; Coninx, K.; Vanhees, L.; Piepoli, M.F.; Niebauer, J.; Cornelissen, V.; Pedretti, R.; Geurts, E.; Ruiz, G.R.; et al. The European Association of Preventive Cardiology Exercise Prescription in Everyday Practice and Rehabilitative Training (EXPERT) tool: A digital training and decision support system for optimized exercise prescription in cardiovascular disease. Concept, definitions and construction methodology. Eur. J. Prev. Cardiol. 2017, 24, 1017–1031. [Google Scholar] [CrossRef]
| Control Group (n = 16) | Intervention Group (n = 16) | |
|---|---|---|
| Age (DS) years | 61.1 (10.6) | 61.4 (8.9) |
| Men (%) | 13 (81.3) | 14 (87.5) |
| BMI (DS) kg/m2 | 27.0 (2.9) | 26.6 (3.2) |
| Cardiac pathology n (%) | ||
| HFrEF | 1 (6.3) | 1 (6.3) |
| STEMI | 5 (31.3) | 5 (31.3) |
| NSTEMI | 3 (18.8) | 2 (12.5) |
| Type of intervention n (%) | ||
| PTCA | 12 (75.0) | 12 (75.0) |
| CABG | 4 (25.0) | 4 (25.0) |
| Comorbidities n (%) | ||
| Dyslipidemia | 12 (75.0) | 11 (68.8) |
| Arterial hypertension | 10 (62.5) | 9 (56.3) |
| Chronic kidney disease | 1 (6.3) | 3 (18.8) |
| Impaired fasting glucose | 4 (25.0) | 4 (25.0) |
| Type 2 diabetes mellitus | 2 (12.5) | 3 (18.8) |
| Control Group (CG) | Intervention Group (IG) | Δ between Groups | |||
|---|---|---|---|---|---|
| Baseline | Three Months | Baseline | Three Months | Δ IG (3 Months—Baseline)–Δ CG (3 Months—Baseline) | |
| Travel to and from places (min) | 43.8 (89.6) | 43.4 (68.2) | 134.6 (319.0) | 150.0 (316.0) * | 15.3 (−13.7, 44.3) |
| Moderate recreational activity (min) | 150.0 (98.4) | 166.9 (158.5) | 119.4 (111.4) | 380.9 (167.4) *** | 244.7 (189.1, 300.4) *** |
| Sedentary behavior (min) | 251.3 (88.5) | 294.4 (44.1) * | 255.0 (91.7) | 220.6 (89.5) | −77.5 (−104.9, −50.1) ** |
| Control Group (CG) | Intervention Group (IG) | Δ between Groups | |||
|---|---|---|---|---|---|
| Baseline | Three Months | Baseline | Three Months | Δ IG (3 Months—Baseline)–CG (3 Months—Baseline) | |
| Resting HR (bpm) | 62.7 (6.4) | 63.1 (6.3) | 63.9 (4.2) | 62.6 (5.2) | −1.7 (−3.9, −0.3) |
| Resting SBP (mmHg) | 120.6 (12.6) | 121.1 (13.3) | 122.1 (7.4) | 120.5 (8.9) | −2.1 (−4.6, 0.4) |
| Resting DBP (mmHg) | 72.0 (7.9) | 73.1 (6.8) | 74.4 (7.7) | 74.1 (8.0) | −0.6 (−1.5, 0.3) |
| Exercise HR (bpm) | 87.5 (8.9) | 91.8 (9.6) * | 90.7 (8.7) | 88.5 (9.8) * | −6.6 (−9.5, −3.7) ** |
| Exercise SBP (mmHg) | 148.3 (17.5) | 153.1 (19.5) * | 149.2 (15.4) | 144.4 (16.8) * | −9.6 (−12.5, −6.7) ** |
| Exercise DBP (mmHg) | 76.3 (9.0) | 80.3 (10.2) * | 77.2 (8.0) | 76.3 (7.2) | −5.0 (−7.1, −2.9) * |
| CR10 | 3.9 (0.9) | 4.6 (1.5) * | 4.1 (1.3) | 3.6 (1.7) * | −1.2 (−1.7, −0.8) ** |
| Control Group (CG) | Intervention Group (IG) | Δ between Groups | |||
|---|---|---|---|---|---|
| Baseline | Three Months | Baseline | Three Months | Δ IG (3 Months—Baseline)–Δ CG (3 Months—Baseline) | |
| 30 s chair sit-to-stand test (reps) | 14.1 (3.4) | 12.3 (3.2) ** | 15.6 (3.8) | 16.0 (4.7) | 2.2 (1.23, 3.17) * |
| Right arm curl test (reps) | 14.7 (3.8) | 12.8 (4.6) * | 15.8 (4.2) | 14.0 (3.9) * | 0.1 (−0.59, 0.79) |
| Left arm curl test (reps) | 13.8 (3.9) | 12.0 (4.6) ** | 14.3 (3.0) | 12.6 (3.4) ** | 0.0 (−0.52, 0.52) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foccardi, G.; Vecchiato, M.; Neunhaeuserer, D.; Mezzaro, M.; Quinto, G.; Battista, F.; Duregon, F.; Carlon, R.; Ermolao, A. Effectiveness of Text Messaging as an Incentive to Maintain Physical Activity after Cardiac Rehabilitation: A Randomized Controlled Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 6645. https://doi.org/10.3390/ijerph18126645
Foccardi G, Vecchiato M, Neunhaeuserer D, Mezzaro M, Quinto G, Battista F, Duregon F, Carlon R, Ermolao A. Effectiveness of Text Messaging as an Incentive to Maintain Physical Activity after Cardiac Rehabilitation: A Randomized Controlled Pilot Study. International Journal of Environmental Research and Public Health. 2021; 18(12):6645. https://doi.org/10.3390/ijerph18126645
Chicago/Turabian StyleFoccardi, Giulia, Marco Vecchiato, Daniel Neunhaeuserer, Michele Mezzaro, Giulia Quinto, Francesca Battista, Federica Duregon, Roberto Carlon, and Andrea Ermolao. 2021. "Effectiveness of Text Messaging as an Incentive to Maintain Physical Activity after Cardiac Rehabilitation: A Randomized Controlled Pilot Study" International Journal of Environmental Research and Public Health 18, no. 12: 6645. https://doi.org/10.3390/ijerph18126645
APA StyleFoccardi, G., Vecchiato, M., Neunhaeuserer, D., Mezzaro, M., Quinto, G., Battista, F., Duregon, F., Carlon, R., & Ermolao, A. (2021). Effectiveness of Text Messaging as an Incentive to Maintain Physical Activity after Cardiac Rehabilitation: A Randomized Controlled Pilot Study. International Journal of Environmental Research and Public Health, 18(12), 6645. https://doi.org/10.3390/ijerph18126645







