Emotional Intelligence Training: Influence of a Brief Slow-Paced Breathing Exercise on Psychophysiological Variables Linked to Emotion Regulation
Abstract
1. Introduction
2. Materials and Methods
2.1. The Participants
2.2. Material and Measures
2.2.1. Cardiac Vagal Activity
2.2.2. Slow-Paced Breathing
2.2.3. Visual Analogue Scale—Perceived stress
2.2.4. Self-Assessment Manikin—Perceived Emotional Arousal and Perceived Emotional Valence
2.3. Procedure
2.4. Data Analysis
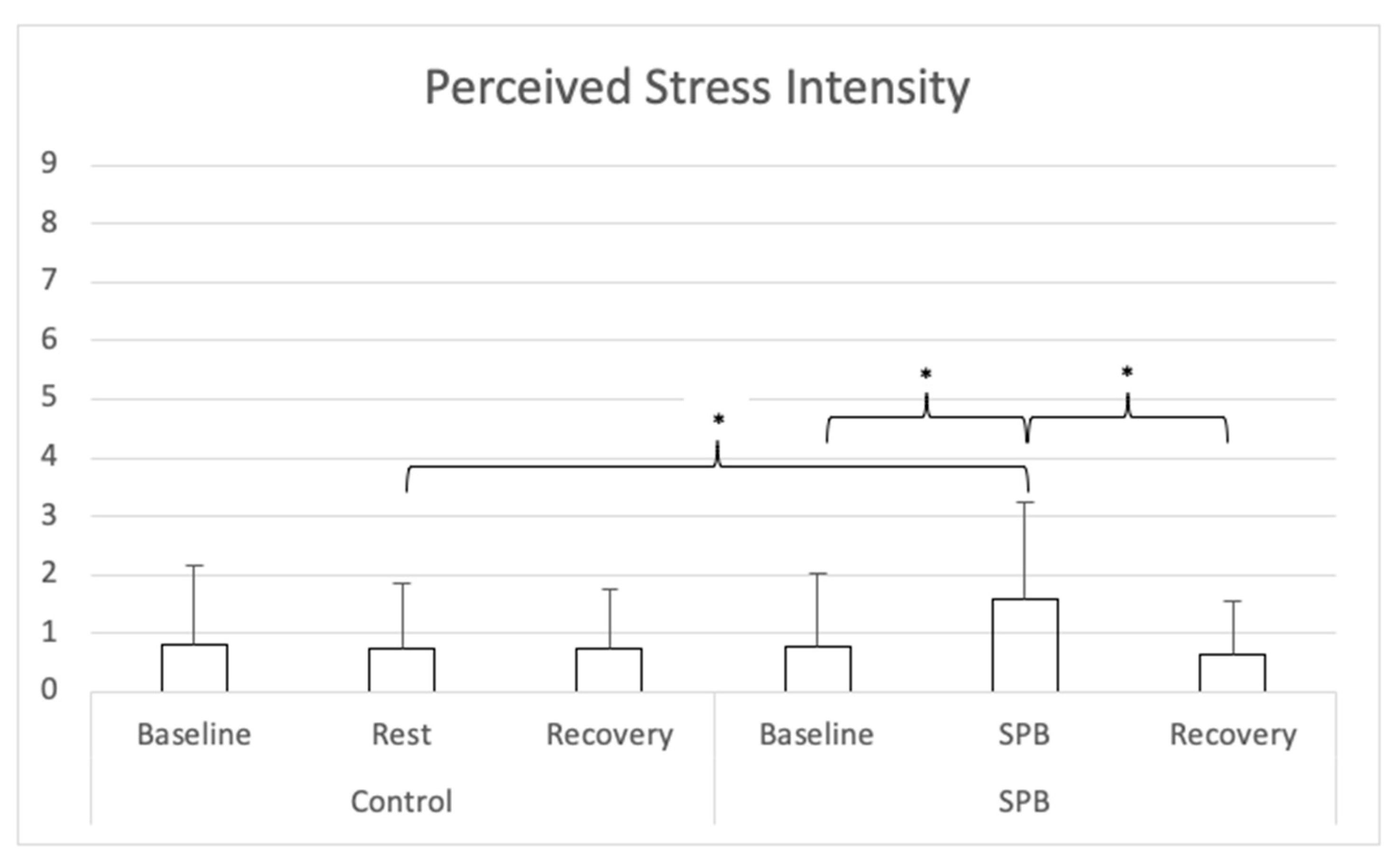
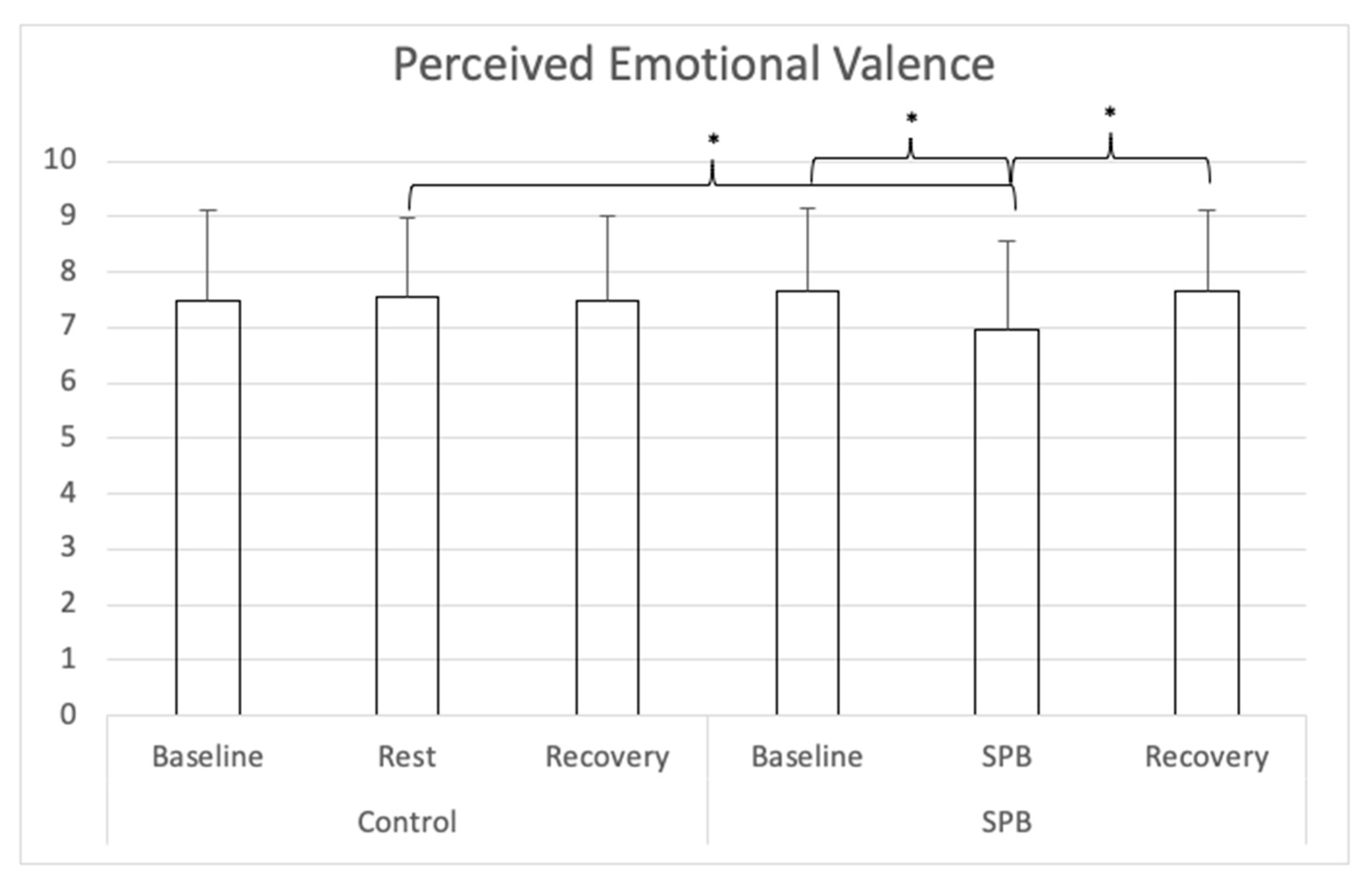
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruiz, M.; Robazza, C. Feelings in Sport—Theory, Research, and Practical Implications for Performance and Well-Being; Routledge: London, UK, 2021. [Google Scholar]
- Lazarus, R.S. How emotions influence performance in competitive sports. Sport Psychol. 2000, 14, 229–252. [Google Scholar] [CrossRef]
- Laborde, S.; Allen, M.S.; Katschak, K.; Mattonet, K.; Lachner, N. Trait personality in sport and exercise psychology: A mapping review and research agenda. Int. J. Sport Exerc. Psychol. 2019, 1–16. [Google Scholar] [CrossRef]
- Petrides, K.V. Technical Manual for the Trait Emotional Intelligence Questionnaire (TEIQue); London Psychometric Laboratory: London, UK, 2009. [Google Scholar]
- Brasseur, S.; Grégoire, J.; Bourdu, R.; Mikolajczak, M. The Profile of Emotional Competence (PEC): Development and validation of a self-reported measure that fits dimensions of emotional competence theory. PLoS ONE 2013, 8, e62635. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Dosseville, F.; Allen, M.S. Emotional intelligence in sport and exercise: A systematic review. Scand. J. Med. Sci. Sports 2016, 26, 862–874. [Google Scholar] [CrossRef] [PubMed]
- Kopp, A.; Jekauc, D. The influence of emotional intelligence on performance in competitive sports: A meta-analytical investigation. Sports 2018, 6, 175. [Google Scholar] [CrossRef]
- Mikolajczak, M. Going beyond the ability-trait debate: The three-level model of emotional intelligence an unifying view: The three-level model of EI. E J. Appl. Psychol. 2009, 5, 25–31. [Google Scholar]
- Laborde, S.; Dosseville, F.; Scelles, N. Trait emotional intelligence and preference for intuition and deliberation: Respective influence on academic performance. Personal. Individ. Differ. 2010, 49, 784–788. [Google Scholar] [CrossRef]
- Laborde, S.; You, M.; Dosseville, F.; Salinas, A. Culture, individual differences, and situation: Influence on coping in French and Chinese table tennis players. Eur. J. Sport Sci. 2012, 12, 255–261. [Google Scholar] [CrossRef]
- Laborde, S.; Dosseville, F.; Guillén, F.; Chávez, E. Validity of the trait emotional intelligence questionnaire in sports and its links with performance satisfaction. Psychol. Sport Exerc. 2014, 15, 481–490. [Google Scholar] [CrossRef]
- Acebes-Sanchez, J.; Granado-Peinado, M.; Giraldez, C.M. Relationship between emotional intelligence and anxiety in a futsal club from Madrid. Retos 2021, 39, 643–648. [Google Scholar]
- Fernandez, M.M.; Brito, C.J.; Miarka, B.; Diaz-de-Durana, A.L. Anxiety and emotional intelligence: Comparisons between combat sports, gender and levels using the trait meta-mood scale and the inventory of situations and anxiety response. Front. Psychol. 2020, 11, 130. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sanchez, M.; Zurita-Ortega, F.; Ramirez-Granizo, I.; Ubago-Jimenez, J.L. Relationship between emotional intelligence and anxiety levels in athletes. J. Sport Health Res. 2020, 12, 42–52. [Google Scholar]
- Laborde, S.; Brüll, A.; Weber, J.; Anders, L.S. Trait emotional intelligence in sports: A protective role against stress through heart rate variability? Personal. Individ. Differ. 2011, 51, 23–27. [Google Scholar] [CrossRef]
- Laborde, S.; Lautenbach, F.; Allen, M.S. The contribution of coping-related variables and heart rate variability to visual search performance under pressure. Physiol. Behav. 2015, 139, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Lautenbach, F.; Allen, M.S.; Herbert, C.; Achtzehn, S. The role of trait emotional intelligence in emotion regulation and performance under pressure. Personal. Individ. Differ. 2014, 57, 43–47. [Google Scholar] [CrossRef]
- Lane, A.M.; Wilson, M.R. Emotions and trait emotional intelligence among ultra-endurance runners. J. Sci. Med. Sport 2011, 14, 358–362. [Google Scholar] [CrossRef]
- Vaughan, R.; Hagyard, J.D.; Brimmell, J.; Edwards, E.J. The effect of trait emotional intelligence on working memory across athletic expertise. J. Sports Sci. 2020, 1–9. [Google Scholar] [CrossRef]
- Vaughan, R.; Laborde, S.; McConville, C. The effect of athletic expertise and trait emotional intelligence on decision-making. Eur. J. Sport Sci. 2019, 19, 225–233. [Google Scholar] [CrossRef]
- Zizzi, S.J.; Deaner, H.R.; Hirschhorn, D.K. The relationship between emotional intelligence and performance among college baseball players. J. Appl. Sport Psychol. 2003, 15, 262–269. [Google Scholar] [CrossRef]
- Perlini, A.H.; Halverson, T.R. Emotional intelligence in the national hockey league. Can. J. Behav. Sci. 2006, 38, 109–119. [Google Scholar] [CrossRef]
- Laborde, S.; Mosley, E.; Dosseville, F. Commentary: Emotional intelligence impact on half marathon finish times. Front. Psychol. 2018, 9, 2593. [Google Scholar] [CrossRef] [PubMed]
- Kotsou, I.; Nelis, D.; Grégoire, J.; Mikolajczak, M. Emotional plasticity: Conditions and effects of improving emotional competence in adulthood. J. Appl. Psychol. 2011, 96, 827–839. [Google Scholar] [CrossRef]
- Nelis, D.; Kotsou, I.; Quoidbach, J.; Hansenne, M.; Weytens, F.; Dupuis, P.; Mikolajczak, M. Increasing emotional competence improves psychological and physical well-being, social relationships, and employability. Emotion 2011, 11, 354–366. [Google Scholar] [CrossRef] [PubMed]
- Kotsou, I.; Mikolajczak, M.; Heeren, A.; Grégoire, J.; Leys, C. Improving emotional intelligence: A systematic review of existing work and future challenges. Emot. Rev. 2019. [Google Scholar] [CrossRef]
- Hodzic, S.; Scharfen, J.; Ripoll, P.; Holling, H.; Zenasni, F. How efficient are emotional intelligence trainings: A meta-analysis. Emot. Rev. 2018, 10, 138–148. [Google Scholar] [CrossRef]
- Campo, M.; Laborde, S.; Mosley, E. Emotional intelligence training in team sports. J. Individ. Differ. 2016, 37, 152–158. [Google Scholar] [CrossRef]
- Campo, M.; Laborde, S.; Martinent, G.; Louvet, B.; Nicolas, M. Emotional intelligence (EI) training adapted to the international preparation constraints in rugby: Influence of EI trainer status on EI training effectiveness. Front. Psychol. 2019, 10, 1939. [Google Scholar] [CrossRef]
- Schütz, K.; Rahders, F.; Mosley, E.; Laborde, S. Emotional competences training in equestrian sport—A preliminary study. Int. J. Sport Exerc. Psychol. 2020, 1–13. [Google Scholar] [CrossRef]
- Crombie, D.; Lombard, C.; Noakes, T.D. Increasing emotional intelligence in cricketers: An intervention study. Int. J. Sports Sci. Coach. 2011, 6, 69–86. [Google Scholar] [CrossRef]
- Barlow, A.; Banks, A.P. Using emotional intelligence in coaching high-performance athletes: A randomised controlled trial. Coach. Int. J. Theory Res. Pract. 2014, 7, 132–139. [Google Scholar] [CrossRef]
- Sherwood, L. Fundamentals of Physiology: A Human Perspective, 3rd ed.; Brooks/Cole: Belmont, CA, USA, 2006. [Google Scholar]
- Tortora, G.J.; Derrickson, B.H. Principles of Anatomy and Physiology; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014. [Google Scholar]
- Russo, M.A.; Santarelli, D.M.; O’Rourke, D. The physiological effects of slow breathing in the healthy human. Breathe 2017, 13, 298–309. [Google Scholar] [CrossRef]
- Zaccaro, A.; Piarulli, A.; Laurino, M.; Garbella, E.; Menicucci, D.; Neri, B.; Gemignani, A. How breath-control can change your life: A systematic review on psycho-physiological correlates of slow breathing. Front. Hum. Neurosci. 2018, 12, 353. [Google Scholar] [CrossRef]
- Schwartz, M.; Andrasik, F. Biofeedback, Fourth Edition: A Practitioner’s Guide; The Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Noble, D.J.; Hochman, S. Hypothesis: Pulmonary afferent activity patterns during slow, deep breathing contribute to the neural induction of physiological relaxation. Front. Physiol. 2019, 10, 1176. [Google Scholar] [CrossRef]
- Gerritsen, R.J.S.; Band, G.P.H. Breath of life: The respiratory vagal stimulation model of contemplative activity. Front. Hum. Neurosci. 2018, 12, 397. [Google Scholar] [CrossRef] [PubMed]
- Mather, M.; Thayer, J.F. How heart rate variability affects emotion regulation brain networks. Curr. Opin. Behav. Sci. 2018, 19, 98–104. [Google Scholar] [CrossRef]
- Lehrer, P.M.; Gevirtz, R. Heart rate variability biofeedback: How and why does it work? Front. Psychol. 2014, 5. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Meehan, Z.M. A practical guide to resonance frequency assessment for heart rate variability biofeedback. Front. Neurosci. 2020, 14. [Google Scholar] [CrossRef]
- Brodal, P. The Central Nervous System—Structure and Function, 5th ed.; Oxford University Press: New York, NY, USA, 2016. [Google Scholar]
- Appelhans, B.M.; Luecken, L.J. Heart rate variability as an index of regulated emotional responding. Rev. Gen. Psychol. 2006, 10, 229–240. [Google Scholar] [CrossRef]
- Thayer, J.F.; Lane, R.D. A model of neurovisceral integration in emotion regulation and dysregulation. J. Affect. Disord. 2000, 61, 201–216. [Google Scholar] [CrossRef]
- Thayer, J.F.; Hansen, A.L.; Saus-Rose, E.; Johnsen, B.H. Heart rate variability, prefrontal neural function, and cognitive performance: The neurovisceral integration perspective on self-regulation, adaptation, and health. Ann. Behav. Med. 2009, 37, 141–153. [Google Scholar] [CrossRef]
- Smith, R.; Thayer, J.F.; Khalsa, S.S.; Lane, R.D. The hierarchical basis of neurovisceral integration. Neurosci. Biobehav. Rev. 2017, 75, 274–296. [Google Scholar] [CrossRef] [PubMed]
- Benarroch, E.E. The central autonomic network: Functional organization, dysfunction, and perspective. Mayo Clin. Proc. 1993, 68, 988–1001. [Google Scholar] [CrossRef]
- Berntson, G.G.; Bigger, J.T.; Eckberg, D.L.; Grossman, P.; Kaufmann, P.G.; Malik, M.; Nagaraja, H.N.; Porges, S.W.; Saul, J.P.; Stone, P.H.; et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology 1997, 34, 623–648. [Google Scholar] [CrossRef]
- Malik, M. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task force of the european society of cardiology and the north american society of pacing and electrophysiology. Eur. Heart J. 1996, 17, 354–381. [Google Scholar] [CrossRef]
- Laborde, S.; Mosley, E.; Thayer, J.F. Heart rate variability and cardiac vagal tone in psychophysiological research—Recommendations for experiment planning, data analysis, and data reporting. Front. Physiol. 2017, 8, 213. [Google Scholar] [CrossRef] [PubMed]
- Penttila, J.; Helminen, A.; Jartti, T.; Kuusela, T.; Huikuri, H.V.; Tulppo, M.P.; Coffeng, R.; Scheinin, H. Time domain, geometrical and frequency domain analysis of cardiac vagal outflow: Effects of various respiratory patterns. Clin. Physiol. 2001, 21, 365–376. [Google Scholar] [CrossRef]
- Laborde, S.; Mosley, E.; Mertgen, A. A unifying conceptual framework of factors associated to cardiac vagal control. Heliyon 2018, 4, e01002. [Google Scholar] [CrossRef]
- Laborde, S.; Mosley, E.; Ueberholz, L. Enhancing cardiac vagal activity: Factors of interest for sport psychology. Prog. Brain Res. 2018, 240, 71–92. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Lentes, T.; Hosang, T.J.; Borges, U.; Mosley, E.; Dosseville, F. Influence of slow-paced breathing on inhibition after physical exertion. Front. Psychol. 2019, 10. [Google Scholar] [CrossRef]
- Laborde, S.; Hosang, T.; Mosley, E.; Dosseville, F. Influence of a 30-day slow paced breathing intervention compared to social media use on subjective sleep quality and cardiac vagal activity. J. Clin. Med. 2019, 8, 193. [Google Scholar] [CrossRef]
- Laborde, S.; Allen, M.; Borges, U.; Hosang, T.; Furley, P.; Mosley, E.; Dosseville, F. The influence of slow-paced breathing on executive function. J. Psychophysiol. 2021. [Google Scholar] [CrossRef]
- You, M.; Laborde, S.; Salvotti, C.; Zammit, N.; Mosley, E.; Dosseville, F. Influence of a single slow-paced breathing session on cardiac vagal activity in athletes. Int. J. Ment. Health Addict. 2021. [Google Scholar] [CrossRef]
- Hoffmann, S.; Jendreizik, L.; Ettinger, U.; Laborde, S. Keeping the pace: The effect of slow-paced breathing on error monitoring. Int. J. Psychophysiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Gross, J.J. The emerging field of emotion regulation: An integrative review. Rev. Gen. Psychol. 1998, 2, 271–299. [Google Scholar] [CrossRef]
- Gross, J.J. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology 2002, 39, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Hanin, Y. Emotions in sport: Current issues and perspectives. In Handbook of Sport Psychology, 3rd ed.; Tenenbaum, G., Eklund, R., Eds.; Wiley: New York, NY, USA, 2007; pp. 31–58. [Google Scholar]
- Di Fronso, S.; Costa, S.; Montesano, C.; Di Gruttola, F.; Ciofi, E.G.; Morgilli, L.; Robazza, C.; Bertollo, M. The effects of COVID-19 pandemic on perceived stress and psychobiosocial states in Italian athletes. Int. J. Sport Exerc. Psychol. 2020, 1–13. [Google Scholar] [CrossRef]
- You, M.; Laborde, S.; Dosseville, F.; Salinas, A.; Allen, M.S. Associations of chronotype, Big Five, and emotional competences with perceived stress in university students. Chronobiol. Int. 2020, 1090–1098. [Google Scholar] [CrossRef]
- De Sio, S.; Buomprisco, G.; Perri, R.; Bruno, G.; Mucci, N.; Nieto, H.A.; Trovato Battagliola, E.; Cedrone, F. Work-related stress risk and preventive measures of mental disorders in the medical environment: An umbrella review. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 821–830. [Google Scholar] [CrossRef] [PubMed]
- Van Diest, I.; Verstappen, K.; Aubert, A.E.; Widjaja, D.; Vansteenwegen, D.; Vlemincx, E. Inhalation/Exhalation ratio modulates the effect of slow breathing on heart rate variability and relaxation. Appl. Psychophysiol. Biofeedback 2014, 39, 171–180. [Google Scholar] [CrossRef]
- Clark, D.M.; Salkovskis, P.M.; Chalkley, A.J. Respiratory control as a treatment for panic attacks. J. Behav. Ther. Exp. Psychiatry 1985, 16, 23–30. [Google Scholar] [CrossRef]
- Hibbert, G.A.; Chan, M. Respiratory control: Its contribution to the treatment of panic attacks. A controlled study. Br. J. Psychiatry J. Ment. Sci. 1989, 154, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.; Friedman, B.H. Positive emotion reduces dyspnea during slow paced breathing. Psychophysiology 2012, 49, 690–696. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society. Dyspnea. Mechanisms, assessment, and management: A consensus statement. American Thoracic Society. Am. J. Respir. Crit. Care Med. 1999, 159, 321–340. [Google Scholar] [CrossRef] [PubMed]
- Quintana, D.S.; Heathers, J.A. Considerations in the assessment of heart rate variability in biobehavioral research. Front. Physiol. 2014, 5, 805. [Google Scholar] [CrossRef]
- Laborde, S.; Allen, M.S.; Gohring, N.; Dosseville, F. The effect of slow-paced breathing on stress management in adolescents with intellectual disability. J. Intellect. Disabil. Res. 2017, 61, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Strauss-Blasche, G.; Moser, M.; Voica, M.; McLeod, D.R.; Klammer, N.; Marktl, W. Relative timing of inspiration and expiration affects respiratory sinus arrhythmia. Clin. Exp. Pharmacol. Physiol. 2000, 27, 601–606. [Google Scholar] [CrossRef]
- Lesage, F.-X.; Berjot, S. Validity of occupational stress assessment using a visual analogue scale. Occup. Med. 2011, 61, 434–436. [Google Scholar] [CrossRef]
- Lesage, F.-X.; Berjot, S.; Deschamps, F. Clinical stress assessment using a visual analogue scale. Occup. Med. 2012, 62, 600–605. [Google Scholar] [CrossRef]
- Bradley, M.; Lang, P.J. Measuring emotion: The self-assessment manikin and the semantic differential. J. Behav. Ther. Exp. Psychiatry 1994, 25, 49–59. [Google Scholar] [CrossRef]
- Fatisson, J.; Oswald, V.; Lalonde, F. Influence diagram of physiological and environmental factors affecting heart rate variability: An extended literature overview. Heart Int. 2016, 11, e32–e40. [Google Scholar] [CrossRef]
- Von Leupoldt, A.; Mertz, C.; Kegat, S.; Burmester, S.; Dahme, B. The impact of emotions on the sensory and affective dimension of perceived dyspnea. Psychophysiology 2006, 43, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Szulczewski, M.T. Training of paced breathing at 0.1 Hz improves CO2 homeostasis and relaxation during a paced breathing task. PLoS ONE 2019, 14, e0218550. [Google Scholar] [CrossRef]
- Jeter, A.M.; Kim, H.C.; Simon, E.; Ritz, T.; Meuret, A.E. Hypoventilation training for asthma: A case illustration. Appl. Psychophysiol. Biofeedback 2012, 37, 63–72. [Google Scholar] [CrossRef]
- Buchheit, M. Monitoring training status with HR measures: Do all roads lead to Rome? Front. Physiol. 2014, 5, 73. [Google Scholar] [CrossRef]
- Lehrer, P.M.; Kaur, K.; Sharma, A.; Shah, K.; Huseby, R.; Bhavsar, J.; Zhang, Y. Heart rate variability biofeedback improves emotional and physical health and performance: A systematic review and meta analysis. Appl. Psychophysiol. Biofeedback 2020. [Google Scholar] [CrossRef]
- Jimenez Morgan, S.; Molina Mora, J.A. Effect of heart rate variability biofeedback on sport performance, a systematic review. Appl. Psychophysiol. Biofeedback 2017. [Google Scholar] [CrossRef] [PubMed]
- Pagaduan, J.; Chen, Y.-S.; Fell, J.W.; Xuan Wu, S.S. Can heart rate variability biofeedback improve athletic performance? A systematic review. J. Hum. Kinet. 2020, 73, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Wells, R.; Outhred, T.; Heathers, J.A.; Quintana, D.S.; Kemp, A.H. Matter over mind: A randomised-controlled trial of single-session biofeedback training on performance anxiety and heart rate variability in musicians. PLoS ONE 2012, 7, e46597. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Mosley, E. Commentary: Heart rate variability and self-control—A meta-analysis. Front. Psychol. 2016, 7. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zahn, D.; Wenzel, M.; Kubiak, T. Response: Commentary: Heart rate variability and self-control—A meta-analysis. Front. Psychol. 2016, 7. [Google Scholar] [CrossRef]
- Zahn, D.; Adams, J.; Krohn, J.; Wenzel, M.; Mann, C.G.; Gomille, L.K.; Jacobi-Scherbening, V.; Kubiak, T. Heart rate variability and self-control—A meta-analysis. Biol. Psychol. 2016, 115, 9–26. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Mosley, E.; Mertgen, A. Vagal tank theory: The three Rs of cardiac vagal control functioning—Resting, reactivity, and recovery. Front. Neurosci. 2018, 12. [Google Scholar] [CrossRef] [PubMed]
- Borges, U.; Lobinger, B.; Javelle, F.; Watson, M.; Mosley, E.; Laborde, S. Using slow-paced breathing to foster endurance, well-being, and sleep quality in athletes during the COVID-19 pandemic. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef]
- Laborde, S.; Raab, M. The tale of hearts and reason: The influence of mood on decision making. J. Sport Exerc. Psychol. 2013, 35, 339–357. [Google Scholar] [CrossRef]
- Laborde, S.; Raab, M.; Kinrade, N.P. Is the ability to keep your mind sharp under pressure reflected in your heart? Evidence for the neurophysiological bases of decision reinvestment. Biol. Psychol. 2014, 100C, 34–42. [Google Scholar] [CrossRef]
- Laborde, S.; Furley, P.; Schempp, C. The relationship between working memory, reinvestment, and heart rate variability. Physiol. Behav. 2015, 139, 430–436. [Google Scholar] [CrossRef]
- Mosley, E.; Laborde, S.; Kavanagh, E. The contribution of coping related variables and cardiac vagal activity on the performance of a dart throwing task under pressure. Physiol. Behav. 2017, 179, 116–125. [Google Scholar] [CrossRef]
- Mosley, E.; Laborde, S.; Kavanagh, E. The contribution of coping-related variables and cardiac vagal activity on prone rifle shooting performance under pressure. J. Psychophysiol. 2018. [Google Scholar] [CrossRef]
- Mosley, E.; Laborde, S.; Kavanagh, E. Coping related variables, cardiac vagal activity and working memory performance under pressure. Acta Psychol. 2018, 191, 179–189. [Google Scholar] [CrossRef]
- Borges, U.; Laborde, S.; Raab, M. Influence of transcutaneous vagus nerve stimulation on cardiac vagal activity: Not different from sham stimulation and no effect of stimulation intensity. PLoS ONE 2019, 14, e0223848. [Google Scholar] [CrossRef] [PubMed]
- Borges, U.; Knops, L.; Laborde, S.; Klatt, S.; Raab, M. Transcutaneous vagus nerve stimulation may enhance only specific aspects of the core executive functions. A randomized crossover trial. Front. Neurosci. 2020, 14. [Google Scholar] [CrossRef] [PubMed]
- Borges, U.; Pfannenstiel, M.; Tsukahara, J.; Laborde, S.; Klatt, S.; Raab, M. Transcutaneous vagus nerve stimulation via tragus or cymba conchae: Are its psychophysiological effects dependent on the stimulation area? Int. J. Psychophysiol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Kauschke, D.; Hosang, T.J.; Javelle, F.; Mosley, E. Performance habits: A framework proposal. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Allen, M.S. Comment: Measurement and the interpretation of trait EI research. Emot. Rev. 2016. [Google Scholar] [CrossRef]
- Laborde, S.; Guillén, F.; Watson, M. Trait emotional intelligence questionnaire full-form and short-form versions: Links with sport participation frequency and duration and type of sport practiced. Personal. Individ. Differ. 2017, 108, 5–9. [Google Scholar] [CrossRef]
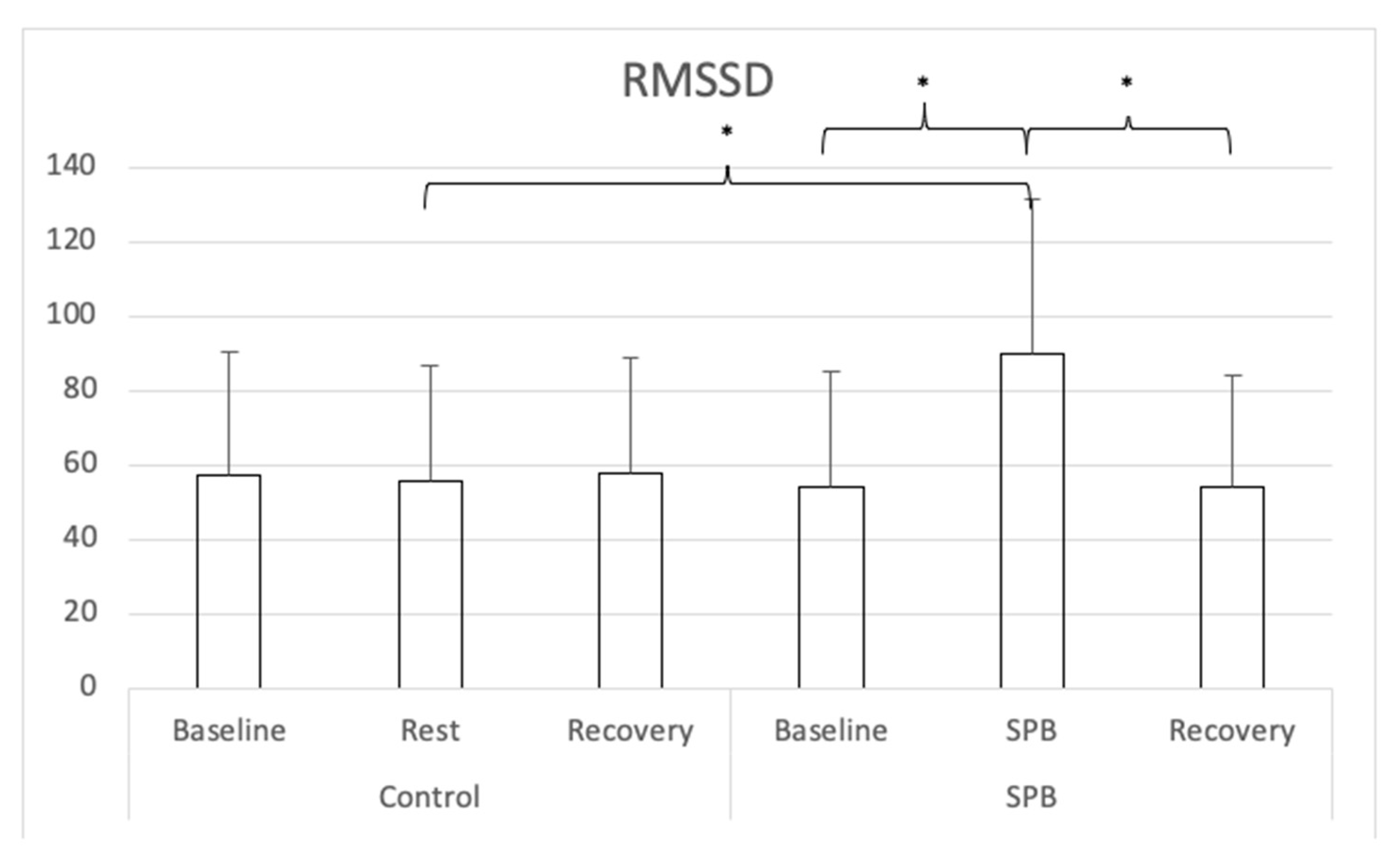

| HR | SDNN | RMSSD | LF | HF | LF/HF | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | ||
| Control condition | Baseline | 67.18 | 7.97 | 92.22 | 37.37 | 57.14 | 33.17 | 3735.74 | 6586.00 | 1266.25 | 1450.35 | 4.09 | 3.91 |
| Rest | 67.66 | 7.81 | 91.53 | 34.09 | 55.52 | 30.96 | 3227.03 | 4809.28 | 1171.95 | 1315.19 | 4.05 | 3.74 | |
| Recovery | 66.71 | 7.76 | 97.36 | 39.60 | 58.08 | 30.77 | 3894.99 | 5905.07 | 1374.02 | 1739.26 | 4.65 | 5.22 | |
| Slow-paced breathing condition | Baseline | 67.65 | 8.43 | 85.67 | 37.61 | 54.08 | 31.23 | 3185.95 | 4969.31 | 1247.59 | 1529.23 | 4.15 | 4.82 |
| Slow-paced breathing | 68.59 | 6.86 | 161.10 | 239.21 | 89.93 | 41.39 | 14580.16 | 11277.36 | 1602.47 | 1403.40 | 16.13 | 13.15 | |
| Recovery | 67.52 | 8.25 | 88.59 | 35.45 | 53.95 | 30.04 | 2927.52 | 3638.94 | 1263.93 | 1869.90 | 4.48 | 5.41 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
You, M.; Laborde, S.; Zammit, N.; Iskra, M.; Borges, U.; Dosseville, F.; Vaughan, R.S. Emotional Intelligence Training: Influence of a Brief Slow-Paced Breathing Exercise on Psychophysiological Variables Linked to Emotion Regulation. Int. J. Environ. Res. Public Health 2021, 18, 6630. https://doi.org/10.3390/ijerph18126630
You M, Laborde S, Zammit N, Iskra M, Borges U, Dosseville F, Vaughan RS. Emotional Intelligence Training: Influence of a Brief Slow-Paced Breathing Exercise on Psychophysiological Variables Linked to Emotion Regulation. International Journal of Environmental Research and Public Health. 2021; 18(12):6630. https://doi.org/10.3390/ijerph18126630
Chicago/Turabian StyleYou, Min, Sylvain Laborde, Nina Zammit, Maša Iskra, Uirassu Borges, Fabrice Dosseville, and Robert S. Vaughan. 2021. "Emotional Intelligence Training: Influence of a Brief Slow-Paced Breathing Exercise on Psychophysiological Variables Linked to Emotion Regulation" International Journal of Environmental Research and Public Health 18, no. 12: 6630. https://doi.org/10.3390/ijerph18126630
APA StyleYou, M., Laborde, S., Zammit, N., Iskra, M., Borges, U., Dosseville, F., & Vaughan, R. S. (2021). Emotional Intelligence Training: Influence of a Brief Slow-Paced Breathing Exercise on Psychophysiological Variables Linked to Emotion Regulation. International Journal of Environmental Research and Public Health, 18(12), 6630. https://doi.org/10.3390/ijerph18126630






