Facilitating Exercise Habit Formation among Cardiac Rehabilitation Patients: A Randomized Controlled Pilot Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Trial Design
2.2. Participants
2.3. Intervention
2.4. Outcomes
2.5. Fidelity Tests: Contextual Predictors
2.6. Statistical Methods
3. Results
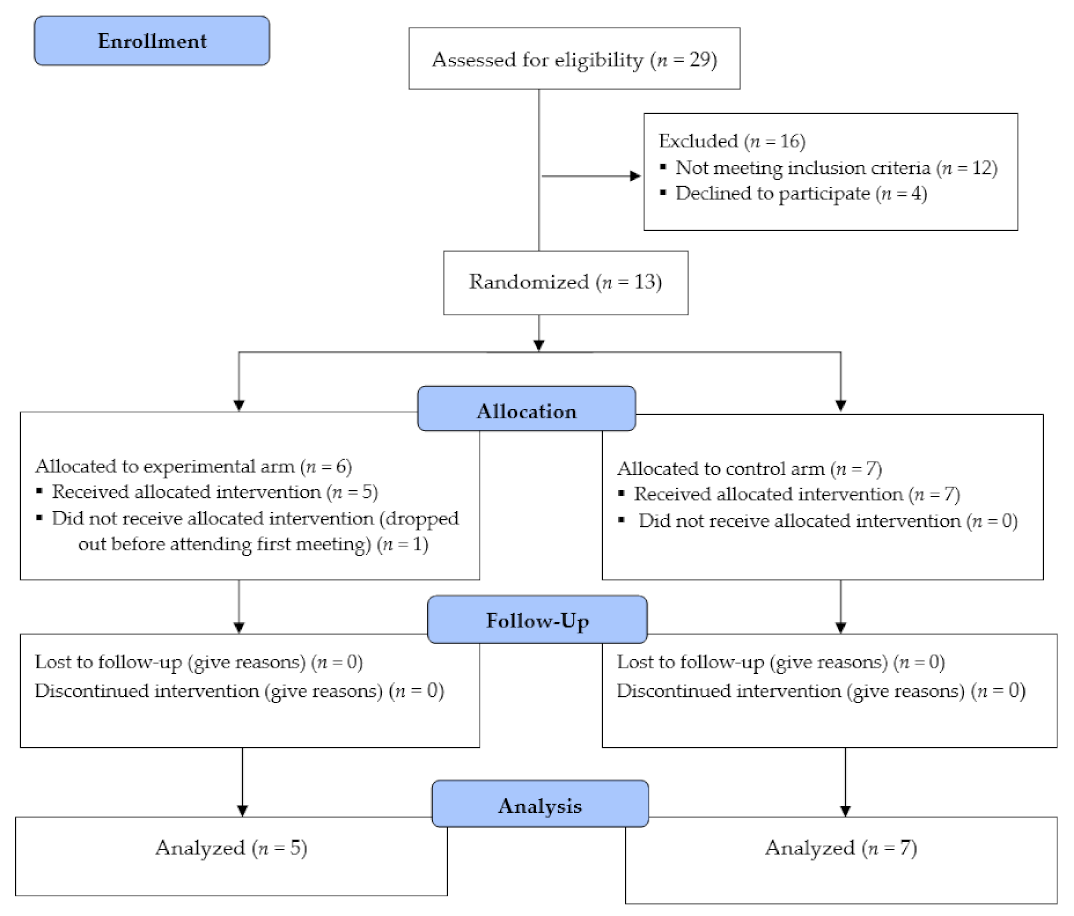
3.1. Participant Flow and Baseline Data
3.2. Missing Outcomes
3.3. Baseline Data
3.4. Participation and Behavior Change
3.5. Fidelity Tests-Contextual Variables
3.6. Harms
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adabag, A.S.; Therneau, T.M.; Gersh, B.J.; Weston, S.A.; Roger, V.L. Sudden death after myocardial infarction. JAMA 2008, 300, 2022–2029. [Google Scholar] [CrossRef] [PubMed]
- Thakkar, J.; Redfern, J.; Thiagalingam, A.; Chow, C.K. Patterns, predictors and effects of texting intervention on physical activity in CHD—insights from the TEXT ME randomized clinical trial. Eur. J. Prev. Cardiol. 2016, 23, 1894–1902. [Google Scholar] [CrossRef]
- EACPR Committee for Science Guidelines; Corrà, U.; Piepoli, M.F.; Carré, F.; Heuschmann, P.; Hoffmann, U.; Verschuren, M.; Halcox, J.; Giannuzzi, P.; Saner, H.; et al. Secondary prevention through cardiac rehabilitation: Physical activity counselling and exercise training: Key components of the position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur. Heart J. 2010, 31, 1967–1974. [Google Scholar] [CrossRef]
- Ekblom, O.; Ek, A.; Cider, Å.; Hambraeus, K.; Börjesson, M. Increased Physical Activity Post-Myocardial Infarction Is Related to Reduced Mortality: Results From the SWEDEHEART Registry. J. Am. Heart Assoc. 2018, 7. [Google Scholar] [CrossRef] [PubMed]
- Stewart, R.A.H.; Held, C.; Brown, R.; Vedin, O.; Hagstrom, E.; Lonn, E.; Armstrong, P.; Granger, C.B.; Hochman, J.S.; Davies, R.; et al. Physical activity in patients with stable coronary heart disease: An international perspective. Eur. Heart J. 2013, 34, 3286–3293. [Google Scholar] [CrossRef] [PubMed]
- Martinello, N.; Saunders, S.; Reid, R. The effectiveness of interventions to maintain exercise and physical activity in post-cardiac rehabilitation populations: A systematic review and meta-analysis of randomized controlled trials. J. Cardiopulm. Rehabil. Prev. 2019, 39, 161–167. [Google Scholar] [CrossRef]
- Dibben, G.; Dalal, H.M.; Taylor, R.S.; Doherty, P.; Tang, L.H.; Hillsdon, M. Cardiac rehabilitation and physical activity: Systematic review and meta-analysis. Heart 2018, 104, 1394–1402. [Google Scholar] [CrossRef]
- Chase, J.-A.D. Systematic review of physical activity intervention studies after cardiac rehabilitation. J. Cardiovasc. Nurs. 2011, 26, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.; Campbell, R.; Hildon, Z.; Hobbs, L.; Michie, S. Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychol. Rev. 2015, 9, 323–344. [Google Scholar] [CrossRef]
- Glanz, K.; Bishop, D.B. The role of behavioral science theory in development and implementation of public health interventions. Annu. Rev. Public Health 2010, 31, 399–418. [Google Scholar] [CrossRef]
- Rhodes, R.E.; De Bruijn, G.-J. What predicts intention-behavior discordance? A review of the action control framework. Exerc. Sport Sci. Rev. 2013, 41, 201–207. [Google Scholar] [CrossRef]
- Sheeran, P.; Webb, T.L. The intention-behavior Gap. Soc. Pers. Psychol. Compass 2016, 10, 503–518. [Google Scholar] [CrossRef]
- Hagger, M.S. Habit and physical activity: Theoretical advances, practical implications, and agenda for future research. Psychol. Sport Exerc. 2019, 42, 118–129. [Google Scholar] [CrossRef]
- Sheeran, P.; Gollwitzer, P.M.; Bargh, J.A. Nonconscious processes and health. Health Psychol. 2013, 32, 460–473. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.S.B.T. Dual-Processing accounts of reasoning, judgment, and social cognition. Annu. Rev. Psychol. 2008, 59, 255–278. [Google Scholar] [CrossRef] [PubMed]
- Ouellette, J.A.; Wood, W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychol. Bull. 1998, 124, 54–74. [Google Scholar] [CrossRef]
- Wood, W.; Rünger, D. Psychology of Habit. Annu. Rev. Psychol. 2016, 67, 289–314. [Google Scholar] [CrossRef]
- Gardner, B. A review and analysis of the use of ‘habit’ in understanding, predicting and influencing health-related behaviour. Health Psychol. Rev. 2015, 9, 277–295. [Google Scholar] [CrossRef]
- Kaushal, N.; Rhodes, R.E.; Spence, J.C.; Meldrum, J.T. Increasing physical activity through principles of habit formation in new gym members: A randomized controlled trial. Ann. Behav. Med. 2017, 51, 578–586. [Google Scholar] [CrossRef]
- British Association for Cardiovascular Prevention and Rehabilitation. Available online: https://www.bacpr.com/resources/BACPR_Standards_and_Core_Components_2017.pdf (accessed on 20 March 2021).
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomized trials. Ann. Intern. Med. 2010, 152, 726–732. [Google Scholar] [CrossRef]
- American College of Sports Medicine Guidelines for Exercise Testing and Prescription, 10th ed.; American College of Sports Medicine; Wolters Kluwer: Philadelphia, PA, USA, 2017.
- Nasreddine, Z.S.; Phillips, N.A.; Bedirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Larouche, E.; Tremblay, M.-P.; Potvin, O.; Laforest, S.; Bergeron, D.; LaForce, R.; Monetta, L.; Boucher, L.; Tremblay, P.; Belleville, S.; et al. Normative data for the montreal cognitive assessment in middle-aged and elderly quebec-french people. Arch. Clin. Neuropsychol. 2016, 31, 819–826. [Google Scholar] [CrossRef]
- Kaushal, N.; Rhodes, R.E. Exercise habit formation in new gym members: A longitudinal study. J. Behav. Med. 2015, 38, 652–663. [Google Scholar] [CrossRef]
- Godin, G.; Jobin, J.; Bouillon, J. Assessment of leisure time exercise behavior by self-report: A concurrent validity study. [Evaluation De l’Exercise Physique Pendant les Loisirs, d’Apres les Indications Fournies par les Interesses: Une Etude de Concordance]. Can. J. Public Health 1986, 77, 359–362. [Google Scholar]
- Godin, G.; Shephard, R.J.; Colantonio, A. The cognitive profile of those who intend to exercise but do not. Public Health Rep. 1986, 101, 521–526. [Google Scholar] [PubMed]
- Arain, M.; Campbell, M.J.; Cooper, C.L.; Lancaster, G.A. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med. Res. Methodol. 2010, 10, 67. [Google Scholar] [CrossRef] [PubMed]
- Thabane, L.; Ma, J.; Chu, R.; Cheng, J.; Ismaila, A.; Rios, L.P.; Robson, R.; Thabane, M.; Giangregorio, L.; Goldsmith, C.H. A tutorial on pilot studies: The what, why and how. BMC Med. Res. Methodol. 2010, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Miles, J.; Shevlin, M. Applying Regression & Correlation: A Guide for Students and Researchers; SAGE Publications: London, UK, 2001. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.; Streiner, D. Biostatistics: The Bare Essentials, 4th ed.; People’s Medical Publishing House: Beijing, China, 2014. [Google Scholar]
- Jackson, N.; Waters, E. Criteria for the systematic review of health promotion and public health interventions. Health Promot. Int. 2005, 20, 367–374. [Google Scholar] [CrossRef]
- Lou, W.; Wan, L.; Abner, E.L.; Fardo, D.W.; Dodge, H.H.; Kryscio, R.J. Multi-state models and missing covariate data: Expectation–maximization algorithm for likelihood estimation. Biostat. Epidemiol. 2017, 1, 20–35. [Google Scholar] [CrossRef]
- Hagger, M.S.; Luszczynska, A. Implementation intention and action planning interventions in health contexts: State of the research and proposals for the way forward. Appl. Psychol. Health Well-Being 2014, 6, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Bélanger-Gravel, A.; Godin, G.; Amireault, S. A meta-analytic review of the effect of implementation intentions on physical activity. Health Psychol. Rev. 2013, 7, 23–54. [Google Scholar] [CrossRef]
- Perk, J. Maintaining physical activity in patients after acute coronary syndromes, the challenge remains. Eur. J. Prev. Cardiol. 2020, 27, 365–366. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | F or χ2 | p | Control Mean (SD) | Experimental Mean (SD) |
|---|---|---|---|---|
| Age | F = 7.32 | 0.02 | 60.43 (5.74) | 69.60 (5.86) |
| BMI | F = 0.816 | 0.39 | 26.18 (5.43) | 29.83 (7.73) |
| MVPA | F = 0.125 | 0.73 | 71.38 (58.83) | 56.80 (84.67) |
| Female | χ2 = 0.80 | 0.67 | 5 | 4 |
| Married/common law | χ2 = 0.01 | 0.92 | 4 | 3 |
| >$75,000 Income | χ2 = 3.08 | 0.08 | 2 | 4 |
| Completed University | χ2 = 1.03 | 0.52 | 6 | 3 |
| Currently Employed | χ2 = 1.67 | 0.29 | 3 | 4 |
| Overall Health | F = 0.06 | 0.82 | 3.29 (0.76) | 3.40 (0.89) |
| Geriatric Depression Scale | F = 2.28 | 0.16 | 1.59 (1.37) | 4.17 (4.62) |
| MoCa Score | F = 1.96 | 0.19 | 25.93 (1.57) | 27.17 (1.72) |
| Cardiac-Related Health Symptoms | ||||
| Angina | χ2 = 1.53 | 0.22 | 7 | 4 |
| Chest pain or discomfort | χ2 = 1.53 | 0.22 | 7 | 4 |
| Upper body discomfort | χ2 = 0.069 | 0.80 | 6 | 4 |
| Shortness of breath | χ2 = 0.343 | 0.56 | 3 | 3 |
| Palpitations | χ2 = 0.069 | 0.80 | 6 | 4 |
| Other Health Conditions | F = 0.488 | 0.50 | 9.40 (1.67) | 7.60 (1.98) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaushal, N.; Payer, M.; Bérubé, B.; Juneau, M.; Bherer, L. Facilitating Exercise Habit Formation among Cardiac Rehabilitation Patients: A Randomized Controlled Pilot Trial. Int. J. Environ. Res. Public Health 2021, 18, 6440. https://doi.org/10.3390/ijerph18126440
Kaushal N, Payer M, Bérubé B, Juneau M, Bherer L. Facilitating Exercise Habit Formation among Cardiac Rehabilitation Patients: A Randomized Controlled Pilot Trial. International Journal of Environmental Research and Public Health. 2021; 18(12):6440. https://doi.org/10.3390/ijerph18126440
Chicago/Turabian StyleKaushal, Navin, Marie Payer, Béatrice Bérubé, Martin Juneau, and Louis Bherer. 2021. "Facilitating Exercise Habit Formation among Cardiac Rehabilitation Patients: A Randomized Controlled Pilot Trial" International Journal of Environmental Research and Public Health 18, no. 12: 6440. https://doi.org/10.3390/ijerph18126440
APA StyleKaushal, N., Payer, M., Bérubé, B., Juneau, M., & Bherer, L. (2021). Facilitating Exercise Habit Formation among Cardiac Rehabilitation Patients: A Randomized Controlled Pilot Trial. International Journal of Environmental Research and Public Health, 18(12), 6440. https://doi.org/10.3390/ijerph18126440






