The Acceptability, Feasibility, and Effectiveness of Wearable Activity Trackers for Increasing Physical Activity in Children and Adolescents: A Systematic Review
Abstract
1. Introduction
Research Questions
- How acceptable are wearables for increasing PA in 5 to 19-year-olds?
- How feasible are wearables for increasing PA in 5 to 19-year-olds?
- How effective are wearables for increasing PA in 5 to 19-year-olds?
- What are the mechanisms of action (BCTs) underlying the influence of wearables on PA in 5 to 19-year-olds?
2. Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Study Selection and Data Extraction
2.5. Behaviour Change Techniques (BCTs)
2.6. Risk of Bias
2.7. Data Synthesis
3. Results
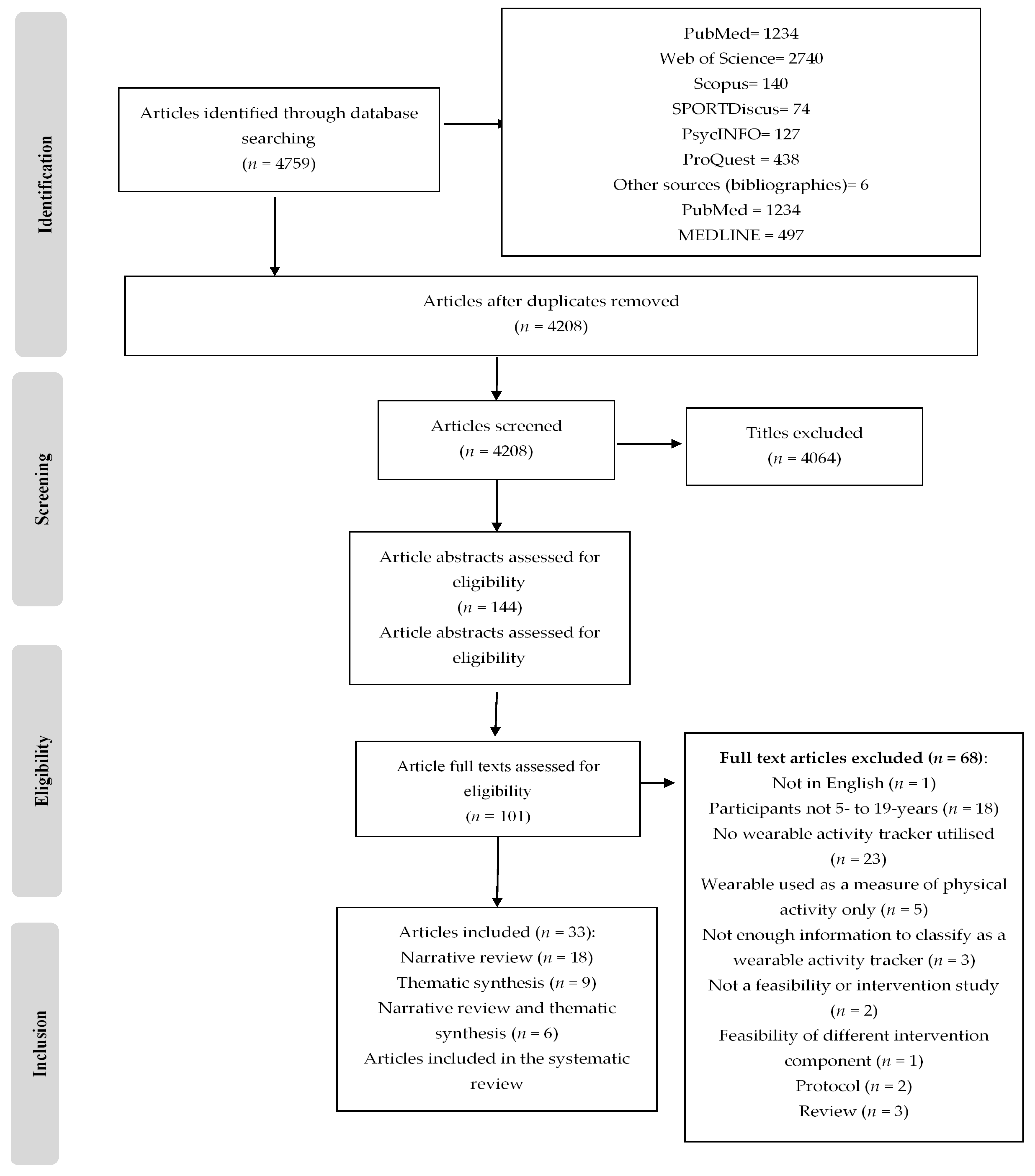
3.1. Search Results
3.2. Countries
3.3. Population
3.4. Study Design
3.5. Devices
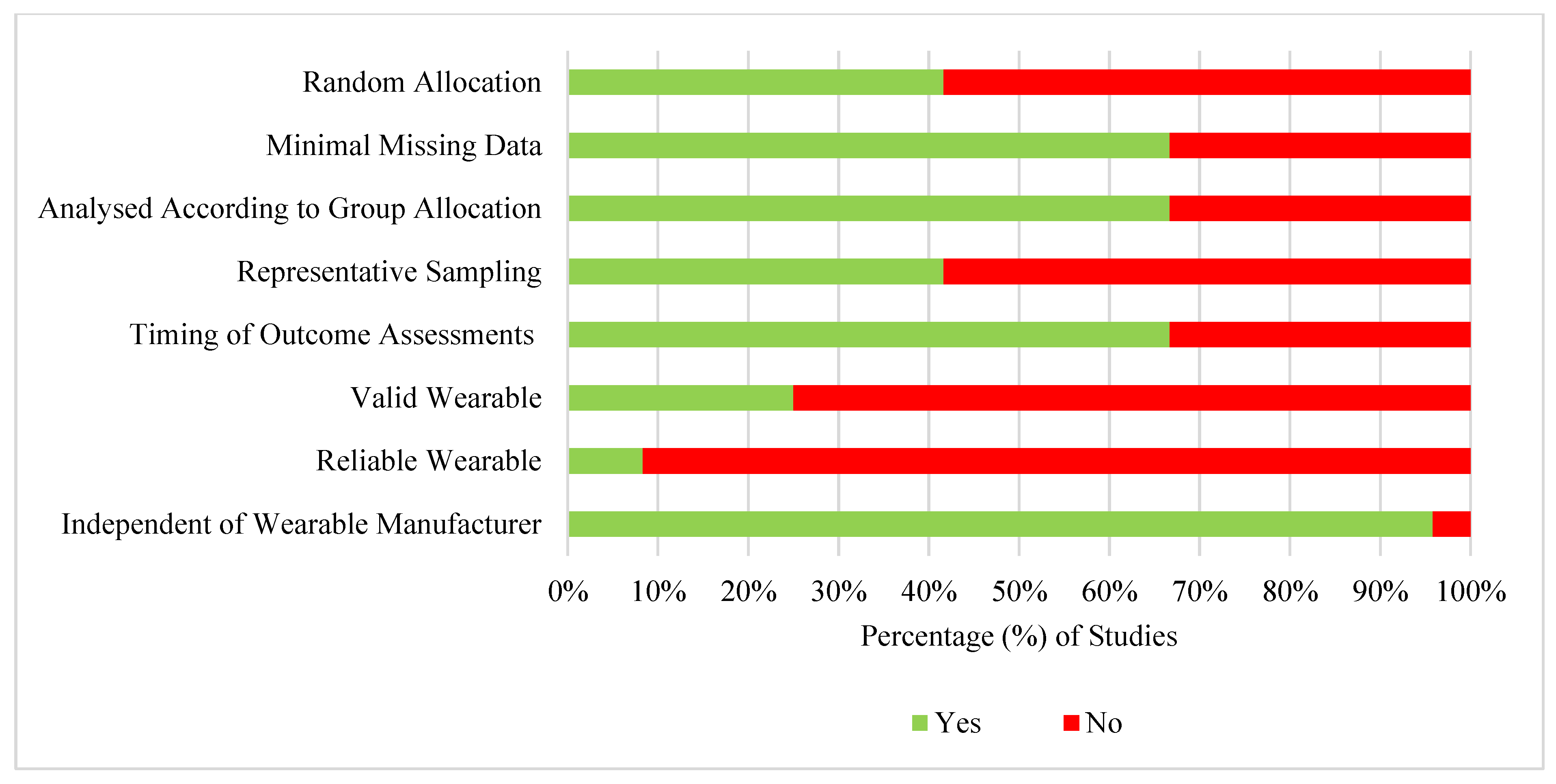
3.6. Risk of Bias
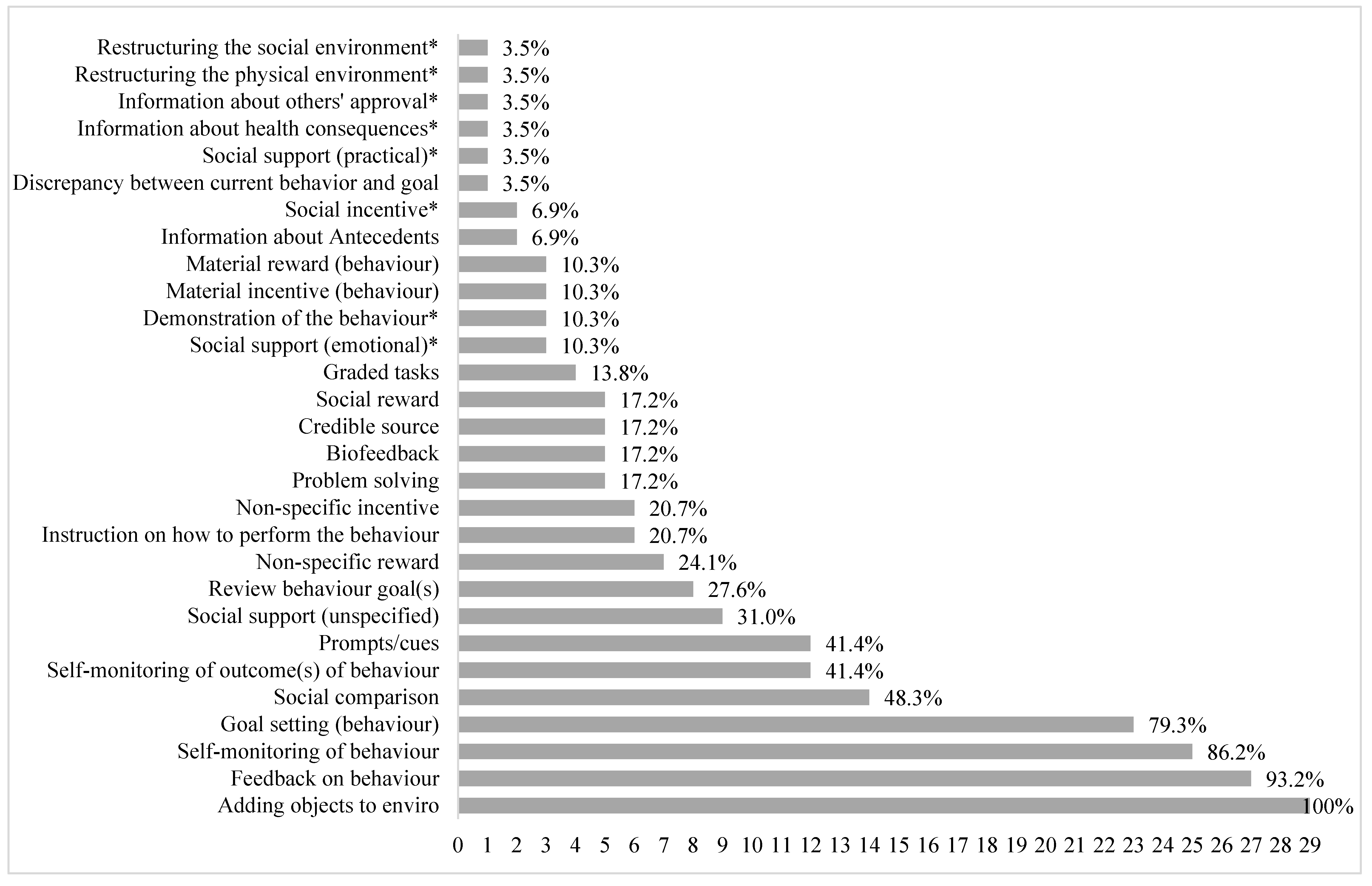
3.7. Behaviour Change Techniques (BCTs)
3.8. Outcomes
3.9. Effectiveness of Wearables on Physical Activity Outcomes
3.9.1. Step Count
3.9.2. Achievement of Step Goals
3.9.3. Moderate-to-Vigorous Physical Activity (MVPA)
3.9.4. Light, Moderate, and Vigorous-Intensity Physical Activity (LPA, MPA, VPA), Sedentary Time, and Metabolic Equivalents (METs)
3.9.5. Total Physical Activity
3.9.6. Active Minutes
3.9.7. Calorie Expenditure
3.10. Thematic Synthesis
4. Discussion
4.1. Effectiveness of Wearables on Physical Activity Outcomes
4.2. Mechanisms of Action
4.3. Acceptability and Feasibility
4.3.1. Perceived Ease of Use
4.3.2. Perceived Usefulness
4.4. Strengths and Limitations
4.5. Conclusions
Supplementary Materials
Authors Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Competing Interests
References
- Kim, J.; Chun, S.; Heo, J.; Lee, S.; Han, A. Contribution of Leisure-Time Physical Activity on Psychological Benefits Among Elderly Immigrants. Appl. Res. Qual. Life 2016, 11, 461–470. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.; Pate, R.R.; Gorber, S.C.; Kho, M.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef] [PubMed]
- Reiner, M.; Niermann, C.; Jekauc, D.; Woll, A. Long-term health benefits of physical activity—A systematic review of longitudinal studies. BMC Public Health 2013, 13, 813. [Google Scholar] [CrossRef] [PubMed]
- Mark, A.E.; Janssen, I. Influence of Movement Intensity and Physical Activity on Adiposity in Youth. J. Phys. Act. Health 2011, 8, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, B.G.C.; da Silva, I.C.M.; Ekelund, U.; Brage, S.; Ong, K.K.; Rolfe, E.D.L.; Lima, N.P.; da Silva, S.G.; de França, G.V.A.; Horta, B.L. Associations of physical activity and sedentary time with body composition in Brazilian young adults. Sci. Rep. 2019, 9, 5444. [Google Scholar] [CrossRef]
- Larouche, R.; Boyer, C.; Tremblay, M.S.; Longmuir, P. Physical fitness, motor skill, and physical activity relationships in grade 4 to 6 children. Appl. Physiol. Nutr. Metab. 2014, 39, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.; Ciaccioni, S.; Thomas, G.; Vergeer, I. Physical activity and mental health in children and adolescents: An updated review of reviews and an analysis of causality. Psychol. Sport Exerc. 2019, 42, 146–155. [Google Scholar] [CrossRef]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Ortega, F.B.; Martínez-Gómez, D.; Labayen, I.; Moreno, L.A.; De Bourdeaudhuij, I.; Manios, Y.; Gonzalez-Gross, M.; Mauro, B.; Molnar, D.; et al. Objectively Measured Physical Activity and Sedentary Time in European Adolescents: The HELENA Study. Am. J. Epidemiol. 2011, 174, 173–184. [Google Scholar] [CrossRef]
- Metcalf, B.; Henley, W.; Wilkin, T. Effectiveness of intervention on physical activity of children: Systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ 2012, 345, e5888. [Google Scholar] [CrossRef]
- Hynynen, S.T.; van Stralen, M.; Sniehotta, F.F.; Araújo-Soares, V.; Hardeman, W.; Chinapaw, M.; Vasankari, T.; Hankonen, N. A systematic review of school-based interventions targeting physical activity and sedentary behaviour among older adolescents. Int. Rev. Sport Exerc. Psychol. 2015, 9, 22–44. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Düking, P.; Tafler, M.; Wallmann-Sperlich, B.; Sperlich, B.; Kleih, S. Behavior Change Techniques in Wrist-Worn Wearables to Promote Physical Activity: Content Analysis. JMIR mHealth uHealth 2020, 8, e20820. [Google Scholar] [CrossRef]
- Mercer, K.; Giangregorio, L.; Schneider, E.; Chilana, P.; Li, M.; Grindrod, K. Acceptance of commercially available weara-ble activity trackers among adults aged over 50 and with chronic illness: A mixed-methods evaluation. JMIR mHealth uHealth 2016, 4, e7. [Google Scholar] [CrossRef]
- Dean, D.A.L.; Griffith, D.M.; McKissic, S.A.; Cornish, E.K.; Johnson-Lawrence, V. Men on the Move–Nashville: Feasibility and Acceptability of a Technology-Enhanced Physical Activity Pilot Intervention for Overweight and Obese Middle and Older Age African American Men. Am. J. Men’s Health 2018, 12, 798–811. [Google Scholar] [CrossRef]
- Hardcastle, S.J.; Galliott, M.; Lynch, B.M.; Nguyen, N.H.; Cohen, P.A.; Mohan, G.R.; Johansen, N.J.; Saunders, C. Acceptability and utility of, and preference for wearable activity trackers amongst non-metropolitan cancer survivors. PLoS ONE 2018, 13, e0210039. [Google Scholar] [CrossRef]
- Hartman, S.J.; Nelson, S.H.; Weiner, L.S.; Lyons, E.; Dominick, G. Patterns of Fitbit Use and Activity Levels Throughout a Physical Activity Intervention: Exploratory Analysis from a Randomized Controlled Trial. JMIR mHealth uHealth 2018, 6, e29. [Google Scholar] [CrossRef]
- Lewis, Z.H.; Lyons, E.J.; Jarvis, J.M.; Baillargeon, J. Using an electronic activity monitor system as an intervention modality: A systematic review. BMC Public Health 2015, 15, 1–15. [Google Scholar] [CrossRef]
- Coughlin, S.S.; Stewart, J. Use of consumer wearable devices to promote physical activity: A review of health inter-vention studies. J. Environ. Health Sci. 2016, 2, 6. [Google Scholar] [CrossRef]
- Brickwood, K.-J.; Watson, G.; O’Brien, J.; Williams, A.D. Consumer-Based Wearable Activity Trackers Increase Physical Activity Participation: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2019, 7, e11819. [Google Scholar] [CrossRef]
- Cajita, M.I.; Kline, C.E.; Burke, L.E.; Bigini, E.G.; Imes, C.C. Feasible but Not Yet Efficacious: A Scoping Review of Wearable Activity Monitors in Interventions Targeting Physical Activity, Sedentary Behavior, and Sleep. Curr. Epidemiol. Rep. 2020, 7, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ridgers, N.D.; A McNarry, M.; A Mackintosh, K. Feasibility and Effectiveness of Using Wearable Activity Trackers in Youth: A Systematic Review. JMIR mHealth uHealth 2016, 4, e129. [Google Scholar] [CrossRef] [PubMed]
- Hayes, L.B.; Van Camp, C.M. Increasing physical activity of children during school recess. J. Appl. Behav. Anal. 2015, 48, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Slootmaker, S.M.; Chinapaw, M.J.; Seidell, J.; van Mechelen, W.; Schuit, J. Accelerometers and Internet for physical activity promotion in youth? Feasibility and effectiveness of a minimal intervention [ISRCTN93896459]. Prev. Med. 2010, 51, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Hooke, M.C.; Gilchrist, L.S.; Tanner, L.; Hart, N.; Withycombe, J.S. Use of a Fitness Tracker to Promote Physical Activity in Children With Acute Lymphoblastic Leukemia. Pediatr. Blood Cancer 2016, 63, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Ainsworth, B.; Arden-Close, E.; Muller, I. The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot Feasibility Stud. 2015, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shaw, R.L.; Larkin, M.; Flowers, P. Expanding the evidence within evidence-based healthcare: Thinking about the context, acceptability and feasibility of interventions. Evid. Based Med. 2014, 19, 201–203. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Tudor-Locke, C. A systematic review of studies using pedometers to promote physical activity among youth. Prev. Med. 2009, 48, 307–315. [Google Scholar] [CrossRef]
- Ho, V.; Simmons, R.K.; Ridgway, C.L.; van Sluijs, E.; Bamber, D.J.; Goodyer, I.M.; Dunn, V.J.; Ekelund, U.; Corder, K. Is wearing a pedometer associated with higher physical activity among adolescents? Prev. Med. 2013, 56, 273–277. [Google Scholar] [CrossRef]
- Ridgers, N.D.; Lai, S.K. Use of Wearable Activity Trackers for Physical Activity Promotion; Oxford University Press (OUP): Oxford, UK, 2018. [Google Scholar]
- Kahan, D.; Nicaise, V. Walk as Directed! Adolescents’ Adherence to Pedometer Intervention Protocol. J. Phys. Act. Health 2012, 9, 962–969. [Google Scholar] [CrossRef]
- Schaefer, S.E.; Van Loan, M.; German, J.B. A Feasibility Study of Wearable Activity Monitors for Pre-Adolescent School-Age Children. Prev. Chronic Dis. 2014, 11, E85. [Google Scholar] [CrossRef]
- Schaefer, S.E.; Ching, C.C.; Breen, H.; German, J.B. Wearing, Thinking, and Moving: Testing the Feasibility of Fitness Tracking with Urban Youth. Am. J. Health Educ. 2016, 47, 8–16. [Google Scholar] [CrossRef]
- Sekhon, M.; Cartwright, M.; Francis, J.J. Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv. Res. 2017, 17, 1–13. [Google Scholar] [CrossRef]
- Abbott, J.H. The Distinction Between Randomized Clinical Trials (RCTs) and Preliminary Feasibility and Pilot Studies: What They Are and Are Not. J. Orthop. Sports Phys. Ther. 2014, 44, 555–558. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Brown, H.E.; Atkin, A.J.; Panter, J.; Wong, G.; Chinapaw, M.; van Sluijs, E. Family-based interventions to increase physical activity in children: A systematic review, meta-analysis and realist synthesis. Obes. Rev. 2016, 17, 345–360. [Google Scholar] [CrossRef]
- Horsley, T.; Dingwall, O.; Sampson, M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database Syst. Rev. 2011, 2011, MR000026. [Google Scholar] [CrossRef]
- Shih, P.C.; Han, K.; Poole, E.S.; Rosson, M.B.; Carroll, J.M. Use and Adoption Challenges of Wearable Activity Trackers. In Proceedings of the iConference 2015, Newport Beach, CA, USA, 24–27 March 2015. [Google Scholar]
- Lauricella, A.R.; Cingel, D.P.; Blackwell, C.; Wartella, E.; Conway, A. The Mobile Generation: Youth and Adolescent Ownership and Use of New Media. Commun. Res. Rep. 2014, 31, 357–364. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. The Cochrane Collaboration. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Chichester, UK, 2011; Volume 4. [Google Scholar]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions; Silverback Publishing: London, UK, 2014. [Google Scholar]
- Viswanathan, M.; Patnode, C.D.; Berkman, N.D.; Bass, E.B.; Chang, S.; Hartling, L.; Murad, M.H.; Treadwell, J.R.; Kane, R.L. Assessing the risk of bias in sys-tematic reviews of health care interventions. In Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet]: Agency for Healthcare Research and Quality (US); U.S. Department of Health & Human Services: Washington, DC, USA, 2017. [Google Scholar]
- Fletcher, B.R.; Hinton, L.; Hartmann-Boyce, J.; Roberts, N.W.; Bobrovitz, N.; McManus, R.J. Self-monitoring blood pressure in hypertension, patient and provider perspectives: A systematic review and thematic synthesis. Patient Educ. Couns. 2016, 99, 210–219. [Google Scholar] [CrossRef]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008, 8, 45. [Google Scholar] [CrossRef]
- Bianchi-Hayes, J.; Schoenfeld, E.; Cataldo, R.; Hou, W.; Messina, C.; Pati, S. Combining Activity Trackers with Motivational Interviewing and Mutual Support to Increase Physical Activity in Parent-Adolescent Dyads: Longitudinal Observational Feasibility Study. JMIR Pediatr. Parent. 2018, 1, e3. [Google Scholar] [CrossRef] [PubMed]
- Bronikowski, M.; Bronikowska, M.; Glapa, A. Do they need goals or support? A report from a goal-setting intervention using physical activity monitors in youth. Int. J. Environ. Res. Public Health 2016, 13, 914. [Google Scholar] [CrossRef] [PubMed]
- Harris, H.B.; Chen, W. Technology-Enhanced Classroom Activity Breaks Impacting Children’s Physical Activity and Fitness. J. Clin. Med. 2018, 7, 165. [Google Scholar] [CrossRef] [PubMed]
- Drehlich, M.; Naraine, M.; Rowe, K.; Lai, S.K.; Salmon, J.; Brown, H.; Koorts, H.; Macfarlane, S.; Ridgers, N.D. Using the Technology Acceptance Model to Ex-plore Adolescents’ Perspectives on Combining Technologies for Physical Activity Promotion Within an Intervention: Usability Study. J. Med. Internet Res. 2020, 22, e15552. [Google Scholar] [CrossRef]
- Evans, E.W.; Abrantes, A.M.; Chen, E.; Jelalian, E. Using Novel Technology within a School-Based Setting to Increase Physical Activity: A Pilot Study in School-Age Children from a Low-Income, Urban Community. BioMed Res. Int. 2017, 2017, 1–7. [Google Scholar] [CrossRef]
- Galy, O.; Yacef, K.; Caillaud, C. Improving Pacific Adolescents’ Physical Activity Toward International Recommendations: Exploratory Study of a Digital Education App Coupled With Activity Trackers. JMIR mHealth uHealth 2019, 7, e14854. [Google Scholar] [CrossRef]
- Gaudet, J.; Gallant, F.; Bélanger, M.; Wang, J.; Coa, K. A Bit of Fit: Minimalist Intervention in Adolescents Based on a Physical Activity Tracker. JMIR mHealth uHealth 2017, 5, e92. [Google Scholar] [CrossRef]
- Götte, M.; Kesting, S.V.; Gerss, J.; Rosenbaum, D.; Boos, J. Feasibility and effects of a home-based intervention using activity trackers on achievement of individual goals, quality of life and motor performance in patients with paediatric cancer. BMJ Open Sport Exerc. Med. 2018, 4, e000322. [Google Scholar] [CrossRef]
- Guthrie, N.; Bradlyn, A.; Thompson, S.K.; Yen, S.; Haritatos, J.; Dillon, F.; Cole, S.W. Development of an Accelerometer-Linked Online Intervention System to Promote Physical Activity in Adolescents. PLoS ONE 2015, 10, e0128639. [Google Scholar] [CrossRef]
- Heale, L.D.; Dover, S.; Goh, Y.I.; Maksymiuk, V.A.; Wells, G.D.; Feldman, B.M. A wearable activity tracker intervention for promoting physical activity in adolescents with juvenile idiopathic arthritis: A pilot study. Pediatr. Rheumatol. 2018, 16, 1–8. [Google Scholar] [CrossRef]
- Kerner, C.; Burrows, A.; McGrane, B. Health wearables in adolescents: Implications for body satisfaction, motivation and physical activity. Int. J. Health Promot. Educ. 2019, 57, 191–202. [Google Scholar] [CrossRef]
- Kerner, C.; Goodyear, V. The Motivational Impact of Wearable Healthy Lifestyle Technologies: A Self-determination Perspective on Fitbits with Adolescents. Am. J. Health Educ. 2017, 48, 287–297. [Google Scholar] [CrossRef]
- Knox, E.; Glazebrook, C.; Randell, T.; Leighton, P.; Guo, B.; Greening, J.; Davies, E.B.; Amor, L.; Blake, H. SKIP (Supporting Kids with diabetes In Physical activity): Feasibility of a randomised controlled trial of a digital intervention for 9-12 year olds with type 1 diabetes mellitus. BMC Public Health 2019, 19, 1–14. [Google Scholar] [CrossRef]
- Larson, J.N.; Brusseau, T.A.; Wengreen, H.; Fairclough, S.J.; Newton, M.M.; Hannon, J.C. Fit “N” Cool Kids: The Effects of Character Modeling and Goal Setting on Children’s Physical Activity and Fruit and Vegetable Consumption. Clin. Med. Insights Pediatr. 2018, 12, 2–6. [Google Scholar] [CrossRef]
- Mackintosh, K.A.; E Chappel, S.; Salmon, J.; Timperio, A.; Ball, K.; Brown, H.; Macfarlane, S.; Ridgers, N.D. Parental Perspectives of a Wearable Activity Tracker for Children Younger Than 13 Years: Acceptability and Usability Study. JMIR mHealth uHealth 2019, 7, e13858. [Google Scholar] [CrossRef]
- Marttinen, R.; Daum, D.; Fredrick, R.N.; Santiago, J.; Silverman, S. Students’ Perceptions of Technology Integration During the F.I.T. Unit. Res. Q. Exerc. Sport 2019, 90, 206–216. [Google Scholar] [CrossRef]
- Masteller, B.; Sirard, J.; Freedson, P.; Routen, A.; Fuemmeler, B. The Physical Activity Tracker Testing in Youth (P.A.T.T.Y) Study: Content Analysis and Children’s Perceptions. JMIR mHealth uHealth 2017, 5, e55. [Google Scholar] [CrossRef]
- Mendoza, J.A.; Baker, K.S.; Moreno, M.A.; Whitlock, K.; Abbey-Lambertz, M.; Waite, A.; Colburn, T.; Chow, E.J. A Fitbit and Facebook mHealth intervention for promoting physical activity among adolescent and young adult childhood cancer survivors: A pilot study. Pediatr. Blood Cancer 2017, 64, e26660. [Google Scholar] [CrossRef]
- Müller, J.; Hoch, A.-M.; Zoller, V.; Oberhoffer, R. Feasibility of Physical Activity Assessment with Wearable Devices in Children Aged 4–10 Years—A Pilot Study. Front. Pediatr. 2018, 6, 5. [Google Scholar] [CrossRef]
- Nation-Grainger, S. ‘It’s just PE’ till ‘It felt like a computer game’: Using technology to improve motivation in physical education. Res. Pap. Educ. 2017, 23, 1–18. [Google Scholar] [CrossRef]
- Phan, T.-L.T.; Barnini, N.; Xie, S.; Martinez, A.; Falini, L.; Abatemarco, A.; Waldron, M.; Benton, J.M.; Frankenberry, S.; Coleman, C.; et al. Feasibility of Using a Commercial Fitness Tracker as an Adjunct to Family-Based Weight Management Treatment: Pilot Randomized Trial. JMIR mHealth uHealth 2018, 6, e10523. [Google Scholar] [CrossRef] [PubMed]
- Remmert, J.E.; Woodworth, A.; Chau, L.; Schumacher, L.M.; Butryn, M.L.; Schneider, M. Pilot Trial of an Acceptance-Based Behavioral Intervention to Promote Physical Activity Among Adolescents. J. Sch. Nurs. 2019, 35, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Ridgers, N.D.; Timperio, A.; Brown, H.; Ball, K.; Macfarlane, S.; Lai, S.K.; Richards, K.; A Mackintosh, K.; A McNarry, M.; Foster, M.; et al. Wearable Activity Tracker Use Among Australian Adolescents: Usability and Acceptability Study. JMIR mHealth uHealth 2018, 6, e86. [Google Scholar] [CrossRef] [PubMed]
- Ruotsalainen, H.; Kyngäs, H.; Tammelin, T.; Heikkinen, H.; Kääriäinen, M. Effectiveness of Facebook-Delivered Lifestyle Counselling and Physical Activity Self-Monitoring on Physical Activity and Body Mass Index in Overweight and Obese Adolescents: A Randomized Controlled Trial. Nurs. Res. Pr. 2015, 2015, 1–14. [Google Scholar] [CrossRef]
- Schoenfelder, E.; Moreno, M.; Wilner, M.; Whitlock, K.B.; Mendoza, J.A. Piloting a mobile health intervention to increase physical activity for adolescents with ADHD. Prev. Med. Rep. 2017, 6, 210–213. [Google Scholar] [CrossRef]
- Sharaievska, I.; A Battista, R.; Zwetsloot, J.; Brakenridge, C.; Lyons, E. Use of Physical Activity Monitoring Devices by Families in Rural Communities: Qualitative Approach. JMIR Pediatr. Parent. 2019, 2, e10658. [Google Scholar] [CrossRef]
- Yoost, J.; Gerlach, J.; Sinning, K.; Cyphert, H. The Use of Fitbit Technology among Rural Obese Adolescents. J. Obes. Nutr. Disord. 2018, 10. [Google Scholar]
- He, Z.; Wu, H.; Yu, F.; Fu, J.; Sun, S.; Huang, T.; Wang, R.; Chen, D.; Zhao, G.; Quan, M. Effects of Smartphone-Based Interventions on Physical Activity in Children and Adolescents: Systematic Review and Meta-analysis. JMIR mHealth uHealth 2021, 9, e22601. [Google Scholar] [CrossRef]
- Maher, C.; Ryan, J.; Ambrosi, C.; Edney, S. Users’ experiences of wearable activity trackers: A cross-sectional study. BMC Public Health 2017, 17, 1–8. [Google Scholar] [CrossRef]
- Kinney, D.A.; Nabors, L.A.; Merianos, A.L.; Vidourek, R.A. College Students’ Use and Perceptions of Wearable Fitness Trackers. Am. J. Heal. Educ. 2019, 50, 298–307. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Duncan, M.J.; Kolt, G.S.; Caperchione, C.M.; Savage, T.N.; Van Itallie, A.; Oldmeadow, C.; Alley, S.J.; Tague, R.; Maeder, A.J.; et al. More real-world trials are needed to establish if web-based physical activity interventions are effective. Br. J. Sports Med. 2018, 53, 1553–1554. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Stanton, R.; Rebar, A.L.; Van Itallie, A.K.; Caperchione, C.M.; Duncan, M.J.; Savage, T.N.; Rosenkranz, R.R.; Kolt, G.S. Physical activity screening to recruit inactive randomized controlled trial participants: How much is too much? Trials 2015, 16, 1–3. [Google Scholar] [CrossRef]
- Eckerstorfer, L.V.; Tanzer, N.K.; Vogrincic-Haselbacher, C.; Kedia, G.; Brohmer, H.; Dinslaken, I.; Corcoran, K. Key Elements of mHealth Interventions to Successfully Increase Physical Activity: Meta-Regression. JMIR mHealth uHealth 2018, 6, e10076. [Google Scholar] [CrossRef]
- Samdal, G.B.; Eide, G.E.; Barth, T.; Williams, G.; Meland, E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–14. [Google Scholar] [CrossRef]
- Ryan, R.M.; Patrick, H. Self-determination theory and physical. Hell. J. Psychol. 2009, 6, 107–124. [Google Scholar]
- Ryan, J.; Edney, S.; Maher, C. Anxious or empowered? A cross-sectional study exploring how wearable activity trackers make their owners feel. BMC Psychol. 2019, 7, 1–8. [Google Scholar] [CrossRef]
- Golley, R.K.; Hendrie, G.A.; Slater, A.; Corsini, N. Interventions that involve parents to improve children’s weight-related nutrition intake and activity patterns—What nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obes. Rev. 2011, 12, 114–130. [Google Scholar] [CrossRef]
- Williams, S.L.; French, D.P. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour--and are they the same? Health Educ. Res. 2011, 26, 308–322. [Google Scholar] [CrossRef]
- Dusseldorp, E.; Van Genugten, L.; van Buuren, S.; Verheijden, M.W.; Van Empelen, P. Combinations of techniques that effectively change health behavior: Evidence from Meta-CART analysis. Health Psychol. 2014, 33, 1530–1540. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How We Design Feasibility Studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- Davis, F.D. A Technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results. Ph.D. Thesis, Massachusetts Institute of Technology, Cambridge, MA, USA, 1985. [Google Scholar]
- Lee, Y.; Kozar, K.A.; Larsen, K.R. The technology acceptance model: Past, present, and future. Commun. Assoc. Inf. Syst. 2003, 12, 50. [Google Scholar] [CrossRef]
- Marangunić, N.; Granić, A. Technology acceptance model: A literature review from 1986 to 2013. Univers. Access Inf. Soc. 2015, 14, 81–95. [Google Scholar] [CrossRef]
- Lunney, A.; Cunningham, N.R.; Eastin, M.S. Wearable fitness technology: A structural investigation into acceptance and perceived fitness outcomes. Comput. Hum. Behav. 2016, 65, 114–120. [Google Scholar] [CrossRef]
- Friel, C.P.; Garber, C.E. Who Uses Wearable Activity Trackers and Why? A Comparison of Former and Current Users in the United States. Am. J. Health Promot. 2020, 34, 762–769. [Google Scholar] [CrossRef]
- Schneider, M.; Chau, L. Validation of the Fitbit Zip for monitoring physical activity among free-living adolescents. BMC Res. Notes 2016, 9, 448. [Google Scholar] [CrossRef]
- Hamari, L.; Kullberg, T.; Ruohonen, J.; Heinonen, O.J.; Díaz-Rodríguez, N.; Lilius, J.; Pakarinen, A.; Myllymäki, A.; Leppänen, V.; Salanterä, S. Physical activity among children: Objective measurements using Fitbit One® and ActiGraph. BMC Res. Notes 2017, 10, 1–6. [Google Scholar] [CrossRef]
- Willenberg, L.J.; Ashbolt, R.; Holland, D.; Gibbs, L.; MacDougall, C.; Garrard, J.; Green, J.B.; Waters, E. Increasing school playground physical activity: A mixed methods study combining environmental measures and children’s perspectives. J. Sci. Med. Sport 2010, 13, 210–216. [Google Scholar] [CrossRef]
- Kolehmainen, N.; Ramsay, C.; McKee, L.; Missiuna, C.; Owen, C.; Francis, J. Participation in Physical Play and Leisure in Children With Motor Impairments: Mixed-Methods Study to Generate Evidence for Developing an Intervention. Phys. Ther. 2015, 95, 1374–1386. [Google Scholar] [CrossRef]
- Khan, M.; Bell, R. Bell Effects of a School Based Intervention on Children’s Physical Activity and Healthy Eating: A Mixed-Methods Study. Int. J. Environ. Res. Public Health 2019, 16, 4320. [Google Scholar] [CrossRef]
- Withall, J.; Jago, R.; Fox, K.R. Why some do but most don’t. Barriers and enablers to engaging low-income groups in physical activity programmes: A mixed methods study. BMC Public Health 2011, 11, 507. [Google Scholar] [CrossRef]
- Fetters, M.D.; Freshwater, D. The 1 + 1 = 3 Integration Challenge; SAGE Publications Sage: Los Angeles, CA, USA, 2015. [Google Scholar]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving Integration in Mixed Methods Designs-Principles and Practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef] [PubMed]
| Stages of Thematic Synthesis | Description |
|---|---|
| Code each line of text according to its meaning and content. |
| Consider the similarities and differences between free codes (stage 1) and group them together to develop descriptive themes. |
| Develop themes that “go beyond” the descriptive themes, by addressing how the themes relate to the review aim and generate additional understanding of concepts and hypotheses. |
| Citation | Location | Participants | Wearable Model | Review Question Addressed | Study Design | Study Description | Study Duration | BCTs (n) | Key PA Findings |
|---|---|---|---|---|---|---|---|---|---|
| Bianchi-Hayes et al. [46] | NY, USA | Nine parent–adolescent (14–16 years, BMIa ≥85 percentile) dyads. | Jawbone UP MOVE | Effectiveness | One-arm pilot study. | Adolescents and their parents received a Jawbone UP MOVE. Participants worked with researchers to identify new activities. | 10 weeks | 5 | Participants achieved their step and active minute goals on 35–39% and 55% of intervention days, respectively. |
| Bronikowski et al. [47] | Poznań, Poland | 196 participants (M = 11.5–17.2 years) from an urban school. | Garmin Vivofit | Effectiveness | Two-arm pilot study (two experimental groups). | Both groups received the Garmin Vivofit. IG1b: Daily goal to achieve. IG2 c: Achieve as many steps as they could/wanted. | 8 weeks | IG1: 4 IG2: 3 | No difference in days spent in MVPA between IG1 and IG2. Adolescents in IG2 took more steps/day than adolescents in IG1. |
| Buchele Harris et al. [48] | Not specified. | 116 adolescents (10–11 years) from two schools. | Fitbit Charge HR | Effectiveness | Three-arm quasi-experimental (2 intervention) and 1 control). | IG1: Received a Fitbit Charge HR. IG2: Received a Fitbit Charge HR, took part in a step challenge, and a series of 20 video-based PA exercises. CGd: No intervention. | 20 days | IG1: 7 IG2: 11 CG:0 | Participants in IG2 took 2197 more daily steps, spent more time being fairly and very active and less time being sedentary than participants in IG1. |
| Drehlich et al. [49] | Melbourne, Australia | 124 inactive adolescents (13–14 years), from low SES schools. | Fitbit Flex | Acceptability, feasibility | Two-arm randomised controlled trial but assessed one-arm’s experience using the wearable (thus a one-arm feasibility study). | Received a Fitbit Flex and behaviour change resources via a private, research-moderated Facebook group. | 12 weeks | N/Ae | N/A |
| Evans et al. (study 1; [50]) | Rhode Island, USA | 32 children (M = 10 years) recruited from two fifth-grade classrooms in a low-income urban community. | Fitbit Zip | Effectiveness | One-arm pilot study. | Participants received a Fitbit Zip and a handout stating 10 ways to increase their step count. | 4 weeks | 6 | Participants took a mean of 10,000 steps per day and increased their mean daily steps by 381 from week 1 to week 4. |
| Evans (study 2; [50]) | Rhode Island, USA | 42 adolescents (M = 12.3 years) recruited from four classrooms in a low-income urban community. | Fitbit Charge | Acceptability, feasibility, effectiveness | Three-arm open controlled pilot (school-level intervention (two groups) and control group). | IG1: Received a Fitbit Charge and 6 weekly 40 minute PA sessions led by their teachers and the research team. Incentives were provided to those who met their daily step goal. Participants took part in competitions between pupils and teachers. IG2: Provided with a Fitbit Charge. Did not receive incentives, competitions, or goal setting. CG: No intervention. | 6 weeks | IG1: 10 IG2: 4 CG: 0 | Mean daily step count and MVPA did not differ between IG1, IG2 and CG. |
| Galy et al. [51] | Lifou Island, New Caledonia | 24 adolescents (12–14 years) from a rural school. | Misfit Shine 2 | Effectiveness | One-arm pilot study. | Received a Misfit Shine 2 and a self-paced 8 module (1 h each) learning app (iEngage). | 4 weeks | 8 | Participants averaged 64 mins/day, 14 mins/day and 7 mins/day of LPA, MPA and VPA, respectively. Participants achieving at least 11,000 steps/day increased from 48% of days (week 1) to 54% of days (week 4). |
| Gaudet et al. [52] | Canada | 46 adolescents (13–14 years). | Fitbit Charge HR | Effectiveness | Cross-over pilot study (intervention and control period). | Received a Fitbit Charge HR. | 7 weeks | IG: 6 CG: 0 | No difference in MVPA between groups. |
| Götte et al. [53] | Not specified | 40 adolescents (M = 14.7 years), with cancer. | Fitbit One or Flex | Effectiveness | Two-arm prospective, quasi-experimental study (intervention and control group). | IG: Received a Fitbit One (n = 5) or Flex (n = 35), encouraged to meet PA goals, and received an at-home exercise plan consisting of 5–7 exercises to improve strength, coordination and endurance. CG: Wait-list. | 6–8 weeks | IG: 7 CG: 0 | Participants increased their mean daily step count and active minutes by 1580 and 11.8, respectively. Steps, achievement of step goals, active minutes and achievement of active minute goals did not differ between groups. |
| Guthrie et al. [54] | Morgantown WV, Mountain View CA, and Vista CA, USA | 182 adolescents (13–14 years) from three study sites. | Zamzee | Effectiveness | Three-arm pilot multi-site randomized controlled experiment (intervention group, active control and passive control group). | IG: Received the Zamzee and access to the website (PA progress and rewards). CG1 (Active control): Received Zamzee (no access to website) and an active game (Dance Dance Revolution). CG2 (Passive control): Received a Zamzee (no access to website). | 6 weeks | IG: 9 CG1: 1 CG2: 1 | Participants in the IG demonstrated an average of 15.26 minutes of MVPA/day, which was 67% and 49% greater than those in CG1 (9.12 mins) and CG2 (10.27 mins). |
| Hayes and van Camp [23] | USA | Six girls (8 years) from one school. | Fitbit Tracker (first model) | Effectiveness | Cross-over study (intervention and control period). | Received a Fitbit and step goal during seven recess sessions (20 min) and a final recess session where three step goals were set. | 8 sessions (20 min each) | IG: 12 CG: 0 | Participants took 47% more steps, and 21% more time in MVPA, during intervention than control periods. |
| Heale et al. [55] | Toronto, Canada | 31 patients (12.8–18.6 years) with juvenile idiopathic arthritis. n = 28 in analysis. | Misfit Flash | Effectiveness | One-arm pilot study. | Received a Misfit Flash and set a daily PA goal. | 4 weeks | 4 | Participants did not demonstrate a significant difference in mean METs/day or MVPA blocks/day from baseline to week 5. |
| Hooke et al. [25] | Midwest and South-eastern region, USA | 16 children (6–15 years) with acute lymphoblastic leukemia. | Fitbit One | Effectiveness | One-arm pilot study. | Received a Fitbit One. A research nurse emailed participants and their parent(s) daily with their daily step count and PA levels, along with a brief message of encouragement. | 17 days intervention | 10 | No significant changes in daily steps. |
| Kerner et al. [56] | North-west England | 62 adolescents (14–15 years) from one school. n = 28 in analysis. | Fitbit Charge HR | Effectiveness | One-arm pilot study. | Received a Fitbit Charge HR, with instructions on how to use. | 5 weeks | 8 | Participants decreased their daily MVPA by 9.53 minutes/day from pre- to post-intervention. |
| Kerner and Goodyear [57] | Southeast and northwest England | 84 adolescents (13–14 years) from two schools. | Fitbit Charge | Acceptability, feasibility | One-arm feasibility study. | Received a Fitbit Charge. | 8 weeks | N/A | N/A |
| Knox et al. [58] | Nottingham and Leicester, England. | 49 participants (9–12 years) diagnosed with type 1 diabetes mellitus. | Polar Active | Acceptability, Feasibility, Effectiveness | Two-arm randomised controlled trial (intervention and control hospital site) | IG: Received a Polar Active, access to the Steps to Active Kids with Diabetes (STAK-D) website, and usual care for diabetes. CG: Received usual care for diabetes. | 6 months | IG: 9 CG: 0 | Mean change in daily steps from baseline to post-intervention and follow-up were 1162 and 899 steps/day greater in the IG than the CG. Changes in self-reported PA, MPA, VPA, and easy minutes did not differ between the IG and CG. PAQ sedentary scores significantly decreased in the IG from pre- to post-intervention (but not follow-up). |
| Larson et al. [59] | Mountain West region, USA | 187 children (8–10 years) from two schools. n = 159 in analysis. | New Lifestyles NL−1000 | Effectiveness | Two-way quasi-experimental (intervention school and control school) | IG: Received the NL−1000 and the “Fit ‘n’ Cool Kids” intervention. CG: Received no intervention. | 16 school days. | IG: 11 CG: 0 | Intervention participants took significantly more steps and spent more time in MVPA than the CG. Participants in the IG had a mean increase of 6.5 minutes of MVPA from pre- to post-intervention. |
| Mackintosh et al. [60] | Australia | 25 families (36 children; 7–12 years). | Kidfit | Acceptability, feasibility | One-arm feasibility study. | Received a Kidfit. | 4 weeks | N/A | N/A |
| Marttinen et al. [61] | Northeast, USA | 13 adolescents (M = 12.15 years). | MOVband | Acceptability, feasibility | One-arm feasibility study. | Received a MOVband and took part in the F.I.T Unit, which delivered 12 fitness-based lessons while integrating academic subjects to develop a fitness plan and used PA data to develop fitness plans. | 12 lessons | N/A | N/A |
| Masteller et al. [62] | Not Specified | 16 children (M = 8.6 years). | Sqord, MOVband, and Zamzee. | Acceptability, feasibility | One-arm feasibility study. | Participants wore all three devices simultaneously and were instructed to spend ≥10 mins/day on each partnering website. | 4 days | N/A | N/A |
| Mendoza et al. [63] | Seattle Children’s Hospital, USA | 59 cancer survivors (14–18 years). | Fitbit Flex | Acceptability, feasibility, effectiveness | Two-arm, unblinded, RCT (hospital site-level intervention and control group). | IG: Received a Fitbit Flex (encouraged to reach daily step goal), voluntary participation in a researcher-moderated Facebook group, and usual care. A researcher sent text messages every other day to encourage and remind participants to reach their PA goal. CG: Received usual care. | 10 weeks | IG: 12 CG: 1 | Mean change in MVPA and sedentary time did not differ between the IG and CG. |
| Müller et al. [64] | Bavaria and Baden- Württemberg, Germany | 59 children (M = 7.1 years). | Garmin Vivofit jr | Effectiveness | One-arm pilot study. | Received a Garmin Vivofit jr (partnering app was monitored by parents). | 7 days | 9 | Participants took a mean daily step count of 12,202 and participated in 83 minutes of daily MVPA. |
| Nation-Grainger [65] | England | 10 male adolescents (14–15 years) with low PA motivation from 1 school. | Samsung Galaxy Gear HR | Acceptability, feasibility, effectiveness | Two-arm quasi-experimental (school-level intervention and control group). | IG: Wore a masked Samsung Galaxy Gear HR in 6 PE lessons (1 per week). Received biofeedback after each PE lesson. CG: Wore a masked Samsung Galaxy Gear HR in 6 PE lessons (1 per week). Did not receive any biofeedback. | 6 PE lessons (1 per week) | IG: 2 CG: 1 | No difference in calories expended between IG and CG. |
| Phan et al. [66] | Two tertiary care weight management clinics (Mid-Atlantic and South Atlantic), USA | 88 adolescents (13–17 years, BMI ≥85 th percentile). | Not reported | Effectiveness | Two-way randomised pilot study (two intervention groups). | Received standard weight management treatment and a wearable device and encouraged to increase their step goals. IG1: Only the adolescent received a wearable device. IG2: Adolescent and their parent received a wearable device, | 3 months | IG1: 11 IG2: 11 | Daily steps, MVPA, and calories expended did not differ between IG1 and IG2. |
| Remmert et al. [67] | California, USA | 20 inactive adolescents (M = 12 years). n = 15 in analysis. | Fitbit Flex 2 | Acceptability, feasibility, effectiveness | Two-way non-randomised pilot study (two intervention groups at school-level). | IG1: Received a Fitbit Flex 2 and acceptance-based behavioural counselling combined with preferred-intensity exercise for 30 minutes. IG2: Received a Fitbit Flex 2 only. | 12 weeks | IG1: 6 IG2: 3 | Participants in IG1 increased their daily steps and MVPA by 125 and 0.99 mins/day, respectively From pre- to post-intervention, IG1 increased their minutes of MVPA/day by 7.25 and IG2 increased their minutes of MVPA/day by 11.99. |
| Ridgers et al. [68] | Melbourne, Australia | 60 adolescents (13–14 years) from three secondary schools. | Fitbit Flex | Acceptability, feasibility | One-arm feasibility study. | Received a Fitbit. No other information (e.g., goal setting, how often to wear the device) was provided. | 6 weeks | N/A | N/A |
| Ruotsalainen et al. [69] | Northern Finland | 46 overweight or obese adolescents (13–14 years). | Polar Active | Effectiveness | Three-arm randomised controlled trial (2 intervention groups and 1 control group). | IG1: Received a physiotherapist moderated Facebook-delivered lifestyle counselling, to discuss how to motivate participants to increase PA. IG2: Received the Facebook-delivered lifestyle counselling and a Polar Active. CG: No intervention. | 12 weeks | IG1: 8 IG2: 11 CG: 0 | Changes in LPA, MPA, MVPA and VPA, from baseline to post-intervention did not differ between IG1, IG2 and CG. Participants in IG2 (but not IG1) were less sedentary, than the CG, at post-intervention. |
| Schaefer et al. [32] | Yolo County, CA, USA | 24 children (7–10-years). | Four devices, of which two were considered wearables (Polar Active and SenseWear ArmBand) | Acceptability, feasibility | One-arm feasibility study. | Wore the SenseWear Armband and Polar Active for 1 week each. | 2 weeks | N/A | N/A |
| Schaefer et al. [33] | Northern California, USA | 34 adolescents (11–12 years) recruited from a school with “high poverty”. n = 24 in analysis. | Fitbit One | Acceptability, feasibility | One-arm feasibility study. | Received the Fitbit One during an afterschool program, then all day, every day for 5 months. | 6 months | N/A | N/A |
| Schoenfelder et al. [70] | Washington, USA | 11 adolescents (14–18 years), with ADHD. | Fitbit Flex | Effectiveness | One-arm pilot study. | Received a Fitbit Flex, with a daily step goal, and joined a private Facebook group, where they were encouraged to post in the group (e.g., encourage participants and post their Fitbit data). | 4 weeks | 11 | Participants increased their daily step count by 107 steps/day. |
| Sharaievska et al. [71] | Appalachia, USA | 11 families from a rural community, with one to three children (7–13 years) per family. | Fitbit Zip | Acceptability, feasibility | One-arm feasibility study. | Family members received a Fitbit Zip. | 2 weeks | N/A | N/A |
| Slootmaker et al. [24] | Amsterdam, Netherlands | 87 inactive adolescents (13–17 years) from five schools. n = 68 at follow-up. | PAM | Effectiveness | Two-arm randomised controlled trial (intervention and control group). | IG: Received the PAM and its partnering website (PAM COACH). CG: Received a single information brochure with general PA recommendations. | 3 months | IG: 8 CG: 0 | No difference in pre- and post-intervention (3 month) and follow-up (8 month) LPA, VPA and MVPA between the IG and CG. Compared to the CG, boys in the IG reduced their sedentary time by 1801 minutes/week from pre-intervention to 8-month follow-up, and girls in the IG increased their weekly MPA by 411 minutes/week from pre-intervention to post-intervention (but not follow-up). |
| Yoost et al. [72] | USA | 34 adolescents aged 13–18 years (BMI >95th percentile). n = 24 in analysis. | Fitbit Charge | Acceptability, feasibility, effectiveness | One-arm pilot study. | Received standardised diet and exercise counselling, and a Fitbit Charge. | 6 months | 7 | Participants took a mean of 5101 steps per day throughout the intervention. Participants decreased their average daily step from 6462 steps/day (month 1) to 5101 steps/day (month 3). |
| Citation | Random Allocation | Minimal Missing Data | Analysed According to Group | Representative Sampling | Timing of Outcome Assessments | Validity of Wearable | Reliability of Wearable | Independent of Wearable Manufacturer | Summary Score | Rob Level |
|---|---|---|---|---|---|---|---|---|---|---|
| Bianchi-Hayes et al. [46] | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 4 | Medium |
| Bronikowski et al. [47] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 6 | Low |
| Buchele Harris et al. [48] | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 5 | Medium |
| Evans et al. (study 1; [50]) | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 4 | Medium |
| Evans et al. (study 2; [50]) | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 4 | Medium |
| Galy et al. [51] | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 4 | Medium |
| Gaudet et al. [52] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 6 | Low |
| Götte et al. [53] | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 4 | Medium |
| Guthrie et al. [54] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 | Low |
| Hayes & van Camp [23] | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | High |
| Heale et al. [55] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | High |
| Hooke et al. [25] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | High |
| Kerner et al. [56] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | High |
| Knox et al. [58] | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 5 | Medium |
| Larson et al. [59] | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 5 | Medium |
| Mendoza et al. [63] | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 5 | Medium |
| Müller et al. [64] | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 4 | Medium |
| Nation-Grainger [65] | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 6 | Low |
| Phan et al. [66] | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 6 | Low |
| Remmert et al. [67] | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 4 | Medium |
| Ruotsalainen et al. [69] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 5 | Medium |
| Schoenfelder et al. [70] | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 3 | Medium |
| Slootmaker et al. [24] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 6 | Low |
| Yoost et al. [72] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | High |
| Review Aim | Analytical Theme | Descriptive Theme | Subthemes | Number of Supporting Studies | Findings and Supporting Quotations |
|---|---|---|---|---|---|
| Feasibility | Perceived facilitators and barriers of using a wearable may impact device use | Factors impacting the use of wearables | Device technical difficulties | 8 | Some adolescents reported general barriers to technology, such as access to a computer [61] or the Internet [33], that may limit device use. Some participants reported difficulties with charging and syncing devices (n = 3): “They didn’t charge properly” (Kidfit [60]). Other participants reported daily syncing and charging as burdensome: “Sometimes I forgot, it’s like getting a little bit annoying to have to like do it every day” (Fitbit Flex [49]). |
| Device design impacts wearability | 10 | Some wrist-worn devices were deemed uncomfortable and bulky: “The wristband wasn’t comfortable” (Kidfit [60]). “I kind of got annoyed with it at the end because of the bulkiness… It was a factor in like I didn’t really want to have to wear it” (MOVband [61]). However, participants were worried they would lose the Fitbit One due to its small size: “I didn’t like it because it was too tiny, I thought I was going to lose it” [33]. | |||
| Removal for sports and daily activities | 7 | Some participants disliked that the wearable was unable to capture their activity during sports: “Because I kind of like it when you can see that you’re getting really high [step counts] and not being able to wear it during sporting events. I wasn’t able to see what I was really getting and how high I could really get” (MOVband [61]). Participants reported forgetting to wear the device following removal due to daily activities, such as showering and getting changed: “Now that it’s not waterproof, I like forget to put it back on after a shower” (Polar Active [58]). “Changed into my pyjamas I was like, ‘Oh, I forgot I had that’” (Fitbit One [33]). | |||
| Acceptability | Affective attitude: Feelings towards using wearables | Participants’ feelings of enjoyment, boredom, frustration, and distrust towards using wearables. | Enjoyment of using wearables | 8 | Participants enjoyed using the devices, which may be attributed to their gamification components: “It was fun to compare steps” (Fitbit One [33]). “It felt like a computer game” (Samsung Galaxy Gear HR [65]) “It was fun. It’s almost like a game” (MOVband [61]). |
| Novelty effect | 6 | Participants reported a potential novelty effect of using the device, which may be attributed to boredom: “It’s fun for a bit … the novelty rubs off and just... oh well, I don’t really care anymore” (Fitbit Flex [49]). “I used it for the first 4 weeks, then just gave up” (Fitbit Charge [57]). One parent reported their child was not interested in owning a device after the study: “I said, ‘oh would you want to wear them, like would you want one of your own?’ They said ‘no, we’ve kind of used it now’” (Kidfit [60]). | |||
| Questions regarding the integrity of wearables | 4 | Some participants admitted to testing the integrity of the device by shaking the device or counting their steps: “I tried to count actually how many steps I do, and then I looked at the Fitbit, and it was like 16 off” (Fitbit One [33]). “I would like shake it to see if it’s working and sometimes it wouldn’t” (Fitbit Flex [49]). One adolescent suggested people could “cheat” their PA data, by shaking the device: “But sometimes people can cheat on that, I think” (Fitbit Flex [49]). | |||
| Disappointment due to child restrictions and parental control | 2 | Child restrictions resulted in feelings of disappointment in younger participants: “My mom feels like she didn’t really want this [software] on my laptop” (MOVband [61]). “Bit disappointed that she couldn’t access her own information … because they’d want to see what they’d scored” (Kidfit [60]). | |||
| Perceived effectiveness and intervention coherence: wearables perceived ease of use, interpretation of PA outputs and impact on PA | Wearables ease of use, understanding of PA outputs, and perceived impact on PA varies between devices and individuals. | Understanding how to use wearables and interpret PA outputs | 6 | Participants reported wearables were easy to use, and PA outputs were easy to understand: “It was kind of easy to understand. It wasn’t confusing at all” (Sqord [62]). However, some participants reported a lack of understanding of how to use device features: “I was trying to like add more onto goals and stuff I found it like hard to use and I just like stopped using it” (Fitbit Flex [49]). “I sometimes look at the challenges but I don’t really know what they are”, “It’s really, really confusing how to get sqoins and stuff” (Sqord [62]). | |
| A perceived increase in PA levels | 8 | Some adolescents suggested the mere presence of the device made them more active: “Just knowing it’s on your wrist, it makes me want to be more active” (Fitbit Flex [68]). Most participants referred to a change in lifestyle: “So, we knew [due to the feedback report] we needed to go out a bit more on a Sunday, which we do actually do quite a bit now” (Polar Active [58]). “I would like try to do extra, like offer to take the dog out instead of complaining about it” (Fitbit One [33]). However, one adolescent believed this increase in PA would diminish when they no longer had access to the device: “Cuz I won’t see the results that I done” (Samsung Galaxy Gear HR [65]). | |||
| Wearables do not impact PA levels | 3 | Some participants reported the wearable did not impact their PA levels. However, these participants perceived themselves to be active, and used the device to confirm their beliefs about their active lifestyle: “We were already pretty active so I don’t know” (Fitbit Zip [71]). “I think it just showed me what I was doing” (MOVband [61]). | |||
| Mechanisms of action | Perceived mechanisms of action underlying wearables impact on PA | Wearables may motivate or discourage PA via BCTs: feedback, self-monitoring and goal setting, competition, and rewards and incentives. | Feedback, self-monitoring, and goal-setting | 9 | Participants used immediate feedback to increase their PA levels, and awareness of their PA levels: “When it says get off the couch, he did respond to that” (Kidfit [60]). “Yeah, it makes you so aware of how many or how active you are and then you wanna try to harder” (Fitbit Flex [49]). Participants disliked feedback displayed as a visual representation, or that was only displayed via the partnering app: “What was the flower about?” (Fitbit One [33]) “Didn’t like the fact, unlike this [Fitbit] where you can see your steps instantaneously” (Kidfit [60]). Feedback promoted the use of self-monitoring and goal setting to increase PA. Participants reported a conscious effort to increase their PA to reach their PA goal, or when achieved, increase their PA goal: “In two days, I did 15 miles. My goal was, the next day, to do 6 more miles”, “I want to reach my goal” (MOVband [61]). However, some adolescents reported that predetermined goals (10,000 steps/day) may create feelings of pressure and guilt: “You can feel under pressure to do a certain amount of steps or to be better than what you’re maybe capable of” (Fitbit Charge [57]). |
| Competition with the self and others | 6 | Participants suggested that “beating” their previous score, or their friends’ score, encouraged them to be more physically active: “I wanted to beat my score”, “I always tried to push myself to the next lesson … to try and get a higher mark” (Samsung Galaxy Gear HR [65]). Parents suggested that children may enjoy collective school competitions: “It would be great to have a competition between the classes, rather than amongst each individual kid, because then they’re helping each other along” (Kidfit [60]). However, 3 studies reported that competition may create feelings of pressure and guilt: “Some people maybe feel peer pressure to do fitness, to keep their steps and stuff up”, “You can sometimes feel guilty … I couldn’t let someone else beat me” (Fitbit Charge [57]). | |||
| Rewards and incentives | 3 | Participants reported enjoying rewards and incentives, including social rewards: “I really like that, um, you get rewards”, “I like how you can “like” things because then it makes me feel good when people like my stuff because it makes me feel happy” (Zamzee [62]). However, some participants suggested virtual rewards, such as badges, were not considered an incentive to be physically active: “It’s not like a huge achievement or anything” (Fitbit Flex [68]). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Creaser, A.V.; Clemes, S.A.; Costa, S.; Hall, J.; Ridgers, N.D.; Barber, S.E.; Bingham, D.D. The Acceptability, Feasibility, and Effectiveness of Wearable Activity Trackers for Increasing Physical Activity in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6211. https://doi.org/10.3390/ijerph18126211
Creaser AV, Clemes SA, Costa S, Hall J, Ridgers ND, Barber SE, Bingham DD. The Acceptability, Feasibility, and Effectiveness of Wearable Activity Trackers for Increasing Physical Activity in Children and Adolescents: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(12):6211. https://doi.org/10.3390/ijerph18126211
Chicago/Turabian StyleCreaser, Amy V., Stacy A. Clemes, Silvia Costa, Jennifer Hall, Nicola D. Ridgers, Sally E. Barber, and Daniel D. Bingham. 2021. "The Acceptability, Feasibility, and Effectiveness of Wearable Activity Trackers for Increasing Physical Activity in Children and Adolescents: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 12: 6211. https://doi.org/10.3390/ijerph18126211
APA StyleCreaser, A. V., Clemes, S. A., Costa, S., Hall, J., Ridgers, N. D., Barber, S. E., & Bingham, D. D. (2021). The Acceptability, Feasibility, and Effectiveness of Wearable Activity Trackers for Increasing Physical Activity in Children and Adolescents: A Systematic Review. International Journal of Environmental Research and Public Health, 18(12), 6211. https://doi.org/10.3390/ijerph18126211








