Intimate Partner Violence during the COVID-19 Pandemic: A Review of the Phenomenon from Victims’ and Help Professionals’ Perspectives
Abstract
1. Introduction
Aim of the Study
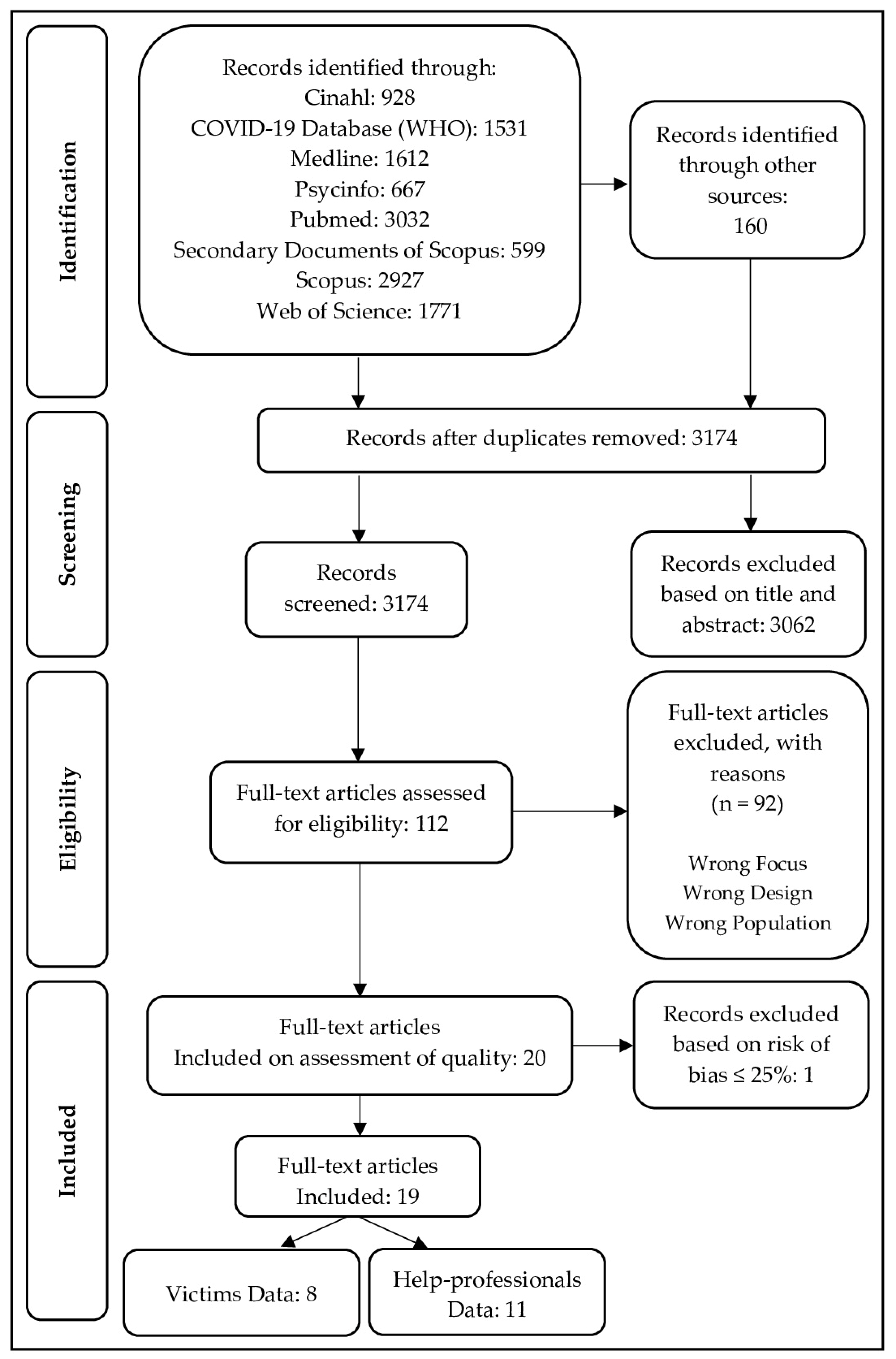
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Risk of Bias Assessment
2.3. Data Analysis
3. Results
3.1. Studies with Victims
3.1.1. IPV Assessment
3.1.2. Other Variables Assessment
3.1.3. Results
Gender Differences in IPV Victimization
Risk Factors for IPV Victimization
3.2. Studies with Help-Professionals
3.2.1. IPV Assessment
3.2.2. Other Variables Assessment
3.2.3. Results
Data Collected from Healthcare Facilities
Data Collected from Police Records
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ertan, D.; El-Hage, W.; Thierrée, S.; Javelot, H.; Hingray, C. COVID-19: Urgency for Distancing from Domestic Violence. Eur. J. Psychotraumatol. 2020, 11, 1800245. [Google Scholar] [CrossRef]
- van Gelder, N.; Peterman, A.; Potts, A.; O’Donnell, M.; Thompson, K.; Shah, N.; Oertelt-Prigione, S. COVID-19: Reducing the Risk of Infection Might Increase the Risk of Intimate Partner Violence. EClinicalMedicine 2020, 21, 100348. [Google Scholar] [CrossRef]
- Boserup, B.; McKenney, M.; Elkbuli, A. Alarming Trends in US Domestic Violence during the COVID-19 Pandemic. Am. J. Emerg. Med. 2020, 38, 2753–2755. [Google Scholar] [CrossRef] [PubMed]
- Barbara, G.; Facchin, F.; Micci, L.; Rendiniello, M.; Giulini, P.; Cattaneo, C.; Vercellini, P.; Kustermann, A. COVID-19, Lockdown, and Intimate Partner Violence: Some Data from an Italian Service and Suggestions for Future Approaches. J. Womens Health 2020, 29, 1239–1242. [Google Scholar] [CrossRef]
- Santos, L.; Monteiro Nunes, L.M.; Rossi, B.A.; Taets, G. Impacts of the COVID-19 Pandemic on Violence against Women: Reflections from the Theory of Human Motivation from Abraham Maslow. SciELO 2020. [Google Scholar] [CrossRef]
- Stavrou, E.; Poynton, S.; Weatherburn, D. Intimate Partner Violence against Women in Australia: Related Factors and Help-Seeking Behaviours. BOCSAR NSW Crime Justice Bull. 2016, 200, 16. Available online: https://www.bocsar.nsw.gov.au/Publications/CJB/Report-2016-Intimate-partner-violence-against-women-in-Australia-CJB200.pdf (accessed on 12 January 2021).
- Lanier, C.; Maume, M.O. Intimate Partner Violence and Social Isolation across the Rural/Urban Divide. Violence Against Women 2009, 15, 1311–1330. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.Y.; Cheung, Y.W.; Cheung, A.K. Social Isolation and Spousal Violence: Comparing Female Marriage Migrants with Local Women. J. Marriage Fam. 2012, 74, 444–461. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Violence against Women during COVID-19. Available online: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-violence-against-women (accessed on 15 January 2021).
- Freeman, K. Monitoring Changes in Domestic Violence in the Wake of COVID-19 Social Isolation Measures. Crime Justice Stat. Bur. Brief. 2020, 145. Available online: https://www.bocsar.nsw.gov.au/Pages/bocsar_publication/Pub_Summary/BB/Summary-DV-COVID-19-BB145.aspx (accessed on 12 January 2021).
- Matoori, S.; Khurana, B.; Balcom, M.C.; Koh, D.M.; Froehlich, J.M.; Janssen, S.; Kolokythas, O.; Gutzeit, A. Intimate Partner Violence Crisis in the COVID-19 Pandemic: How Can Radiologists Make a Difference? Eur. Radiol. 2020, 30, 6933–6936. [Google Scholar] [CrossRef]
- Mari, E.; Fraschetti, A.; Lausi, G.; Pizzo, A.; Baldi, M.; Paoli, E.; Giannini, A.M.; Avallone, F. Forced Cohabitation during Coronavirus Lockdown in Italy: A Study on Coping, Stress and Emotions among Different Family Patterns. J. Clin. Med. 2020, 9, 3906. [Google Scholar] [CrossRef]
- Barbosa, J.P.M.; Lima, R.C.D.; de Brito Martins, G.; Drumond Lanna, S.; Carvalho Andrade, M.A. Intersectionality and Other Views on Violence against Women in Times of Pandemic by COVID-19. SciELO 2020. [Google Scholar] [CrossRef]
- Perez-Vincent, S.M.; Carreras, E.; Gibbons, M.A.; Murphy, T.E.; Rossi, M.A. (Eds.) Evidence from a Domestic Violence Hotline in Argentina In COVID-19 Lockdowns and Domestic Violence; Inter-American Development Bank: Washington, DC, USA, 2020. [Google Scholar]
- Ivandic, R.; Kirchmaier, T.; Linton, B. Changing Patterns of Domestic Abuse during COVID-19 Lockdown. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Speed, A.; Thomson, C.; Richardson, K. Stay Home, Stay Safe, Save Lives? An Analysis of the Impact of COVID-19 on the Ability of Victims of Gender-based Violence to Access Justice. J. Cri. Law 2020, 84, 539–572. [Google Scholar] [CrossRef]
- Williamson, E.; Lombard, N.; Brooks-Hay, O. Domestic Violence and Abuse, Coronavirus, and the Media Narrative. J. Gend. Based Violence 2020, 4, 289–294. [Google Scholar] [CrossRef]
- Usher, K.; Bhullar, N.; Durkin, J.; Gyamfi, N.; Jackson, D. Family Violence and COVID-19: Increased Vulnerability and Reduced Options for Support. Int. J. Ment. Health Nurs. 2020, 29, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Brantingham, P.J.; Brantingham, P.L. Patterns in Crime; Collier Macmillan: New York, NY, USA, 1984. [Google Scholar]
- Campedelli, G.M.; Aziani, A.; Favarin, S. Exploring the Effects of COVID-19 Containment Policies on Crime: An Empirical Analysis of the Short-term Aftermath in Los Angeles. arXiv 2020, arXiv:2003.11021. [Google Scholar] [CrossRef]
- Cohen, L.E.; Felson, M. Social Change and Crime Rate Trends: A Routine Activity Approach. Am. Sociol. Rev. 1979, 44, 588–608. [Google Scholar] [CrossRef]
- Fraser, E. Impact of COVID-19 Pandemic on Violence against Women and Girls. VAWG Helpdesk Research Report. 2020, Volume 284. Available online: https://www.sddirect.org.uk/media/1881/vawg-helpdesk-284-covid-19-and-vawg.pdf (accessed on 18 January 2021).
- United Nation Women. COVID-19 and Ending Violence against Women and Girls. Gender-Based Violence. 2020, Volume 1. Available online: https://digitalcommons.wcl.american.edu/wlpviolence/1/ (accessed on 15 January 2021).
- Kagi, J. Crime Rate in WA Plunges Amid Coronavirus Social Distancing Lockdown Measures. ABC News Australia. Available online: https://www.abc.net.au/news/2020-04-08/coronavirus-shutdown-sees-crime-rate-drop-in-wa/12132410 (accessed on 18 January 2021).
- Poate, S. 75% Increase in Domestic Violence Searches Since Coronavirus. NBN News. Available online: https://www.nbnnews.com.au/2020/03/31/dvsearches-coronavirus/ (accessed on 18 January 2021).
- Campbell, A.M. An Increasing Risk of Family Violence during the Covid-19 Pandemic: Strengthening Community Collaborations to Save Lives. Forensic Sci. Int. 2020, 2, 100089. [Google Scholar] [CrossRef]
- Council of Europe. Promoting and Protecting Women’s Rights at National Level. Available online: https://www.coe.int/en/web/genderequality/promoting-and-protecting-women-s-rights (accessed on 12 January 2021).
- Gosangi, B.; Park, H.; Thomas, R.; Gujrathi, R.; Bay, C.P.; Raja, A.S.; Seltzer, S.E.; Balcom, M.C.; McDonald, M.L.; Orgill, D.P.; et al. Exacerbation of Physical Intimate Partner Violence during COVID-19 Pandemic. Radiology 2021, 298, E38–E45. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, H.X.; Petersen, K.; Lunsford, L.; Biswas, S. COVID-19 Resilience for Survival: Occurrence of Domestic Violence during Lockdown at a Rural American College of Surgeons Verified Level One Trauma Center. Cureus 2020, 12, e10059. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Health Care for Women Subjected to Intimate Partner Violence or Sexual Violence. A Clinical Handbook. Available online: https://apps.who.int/iris/bitstream/handle/10665/136101/WHO_RHR_14.26_eng.pdf (accessed on 15 January 2021).
- Cattaneo, L.B. Contributors to Assessments of Risk in Intimate Partner Violence: How Victims and Professionals Differ. J. Community Psychol. 2007, 35, 57–75. [Google Scholar] [CrossRef]
- Meyer, S. Seeking Help for Intimate Partner Violence: Victims’ Experiences when Approaching the Criminal Justice System for IPV-related Support and Protection in an Australian Jurisdiction. Fem. Criminol. 2011, 6, 268–290. [Google Scholar] [CrossRef]
- Loke, A.Y.; Wan, M.L.E.; Hayter, M. The Lived Experience of Women Victims of Intimate Partner Violence. J. Clin. Nurs. 2012, 21, 2336–2346. [Google Scholar] [CrossRef] [PubMed]
- Waalen, J.; Goodwin, M.M.; Spitz, A.M.; Petersen, R.; Saltzman, L.E. Screening for Intimate Partner Violence by Health Care Providers-Barriers and Interventions. Am. J. Prev. Med. 2000, 4, 230–237. [Google Scholar] [CrossRef]
- Djikanovic, B.; Celik, H.; Simic, S.; Matejic, B.; Cucic, V. Health Professionals’ Perceptions of Intimate Partner Violence against Women in Serbia: Opportunities and Barriers for Response Improvement. Patient Educ. Couns. 2009, 80, 88–93. [Google Scholar] [CrossRef]
- Chang, J.C.; Buranosky, R.; Dado, D.; Cluss, P.; Hawker, L.; Rothe, E.; McNeil, M.; Scholle, S. Helping Women Victims of Intimate Partner Violence: Comparing the Approaches of Two Health Care Settings. Violence Vict. 2009, 24, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Panic, N.; Leoncini, E.; de Belvis, G.; Ricciardi, W.; Boccia, S. Evaluation of the Endorsement of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Statement on the Quality of Published Systematic Review and Meta-Analyses. PLoS ONE 2013, 8, e83138. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P) 2015 Statement. Syst. Rev. 2015, 4. [Google Scholar] [CrossRef] [PubMed]
- Boman, J.H.; Gallupe, O. Has COVID-19 Changed Crime? Crime Rates in the United States during the Pandemic. Am. J. Crim. Justice 2020, 45, 537–545. [Google Scholar] [CrossRef]
- Thomas, J.; Harden, A. Methods for the Thematic Synthesis of Qualitative Research in Systematic Reviews. BMC Med. Res. Methodol. 2008, 8. [Google Scholar] [CrossRef]
- Ghimire, C.; Acharya, S.; Shrestha, C.; KC, P.; Singh, S.; Sharma, P. Interpersonal Violence during the COVID-19 Lockdown Period in Nepal: A Descriptive Cross-sectional Study. JNMA J. Nepal Med. Assoc. 2020, 58, 751–757. [Google Scholar] [CrossRef]
- Gibbons, M.A.; Murphy, T.E.; Rossi, M.A. Confinement and Intimate Partner Violence: The Short-Term Effect of COVID-19. In COVID-19 Lockdowns and Domestic Violence; Perez-Vincent, S.M., Carreras, E., Gibbons, M.A., Murphy, T.E., Rossi, M.A., Eds.; Inter-American Development Bank: Washington, DC, USA, 2020. [Google Scholar]
- Sediri, S.; Zgueb, Y.; Ouanes, S.; Ouali, U.; Bourgou, S.; Jomli, R.; Nacef, F. Women’s Mental Health: Acute Impact of COVID-19 Pandemic on Domestic Violence. Arch. Womens Ment. Health 2020, 23, 749–756. [Google Scholar] [CrossRef]
- Davis, M.; Gilbar, O.; Padilla-Medina, D. Intimate Partner Violence Victimization and Perpetration among U.S. Adults during COVID-19: A Brief Report. medRxiv 2020. [Google Scholar] [CrossRef]
- Gebrewahd, G.T.; Gebremeskel, G.G.; Tadesse, D.B. Intimate Partner Violence against Reproductive Age Women during COVID-19 Pandemic in Northern Ethiopia 2020: A Community-based Cross-sectional Study. Reprod. Health 2020, 17. [Google Scholar] [CrossRef]
- Hamadani, J.D.; Hasan, M.I.; Baldi, A.J.; Hossain, S.J.; Shiraji, S.; Bhuiyan, M.S.; Mehrin, S.; Fisher, J.; Tofail, F.; Tipu, S.; et al. Immediate Impact of Stay-at-Home Orders To Control COVID-19 Transmission on Socioeconomic Conditions, Food Insecurity, Mental Health, and Intimate Partner Violence in Bangladeshi Women and their Families: An Interrupted Time Series. Lancet Glob. Health 2020, 8. [Google Scholar] [CrossRef]
- Jetelina, K.K.; Knell, G.; Molsberry, R.J. Changes in Intimate Partner Violence during the Early Stages of the COVID-19 Pandemic in the USA. Inj. Prev. 2020, 27, 93–97. [Google Scholar] [CrossRef]
- Sabri, B.; Hartley, M.; Saha, J.; Murray, S.; Glass, N.; Campbell, J.C. Effect of COVID-19 Pandemic on Women’s Health and Safety: A Study of Immigrant Survivors of Intimate Partner Violence. Health Care Women Int. 2020, 41, 1294–1312. [Google Scholar] [CrossRef] [PubMed]
- Agüero, J.M. COVID-19 and the Rise of Intimate Partner Violence. World Dev. 2021, 137, 105217. [Google Scholar] [CrossRef] [PubMed]
- Silverio-Murillo, A.; Balmori de la Miyar, J.R.; Hoehn-Velasco, L. Families under Confinement: COVID-19, Domestic Violence, and Alcohol Consumption. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Hassan, K.; Prescher, H.; Wang, F.; Chang, D.W.; Reid, R.R. Evaluating the Effects of COVID-19 on Plastic Surgery Emergencies: Protocols and Analysis From a Level I Trauma Center. Ann. Plast. Surg. 2020, 85, S161–S165. [Google Scholar] [CrossRef] [PubMed]
- Olding, J.; Zisman, S.; Olding, C.; Fan, K. Penetrating Trauma during a Global Pandemic: Changing Patterns in Interpersonal Violence, Self-harm and Domestic Violence in the Covid-19 Outbreak. Surgeon 2021, 19, e9–e13. [Google Scholar] [CrossRef] [PubMed]
- Bullinger, L.R.; Carr, J.; Packham, A. COVID-19 and Crime: Effects of Stay-at-Home Orders on Domestic Violence. Natl. Bur. Econ. Res. 2020. [Google Scholar] [CrossRef]
- Balmori de la Miyar, J.R.; Hoehn-Velasco, L.; Silverio-Murillo, A. Druglords don’t Stay at Home: COVID-19 Pandemic and Crime Patterns in Mexico City. J. Crim. Justice 2021, 72, 101745. [Google Scholar] [CrossRef]
- Pattojoshi, A.; Sidana, A.; Garg, S.; Mishra, S.N.; Singh, L.K.; Goyal, N.; Tikka, S.K. Staying Home is NOT ‘Staying Safe’: A Rapid 8-Day Online Survey on Spousal Violence against Women during the COVID-19 Lockdown in India. Psychiatry Clin. Neurosci. 2020. [Google Scholar] [CrossRef]
- Moreira, D.N.; da Costa, M.P. The Impact of the Covid-19 Pandemic in the Precipitation of Intimate Partner Violence. Int. J. Law Psychiatry 2020, 71, 101606. [Google Scholar] [CrossRef]
- Kaukinen, C. When Stay-at-Home Orders Leave Victims Unsafe at Home: Exploring the Risk and Consequences of Intimate Partner Violence during the COVID-19 Pandemic. Am. J. Crim. Law 2020, 45, 668–679. [Google Scholar] [CrossRef]
- Bradbury-Jones, C.; Isham, L. The Pandemic Paradox: The Consequences of COVID-19 on Domestic Violence. J. Clin. Nurs. 2020, 29, 13–14. [Google Scholar] [CrossRef]
- Fawole, O.I.; Okedare, O.O.; Reed, E. Home Was Not a Safe Haven: Women’s Experiences of Intimate Partner Violence during the COVID-19 Lockdown in Nigeria. BMC Womens Health 2021, 21, 32. [Google Scholar] [CrossRef] [PubMed]
- Salom, C.L.; Williams, G.M.; Najman, J.M.; Alati, R. Substance Use and Mental Health Disorders are Linked to Different Forms of Intimate Partner Violence Victimisation. Drug Alcohol Depend. 2015, 151, 121–127. [Google Scholar] [CrossRef]
- Sanz-Barbero, B.; Pereira, P.L.; Barrio, G.; Vives-Cases, C. Intimate Partner Violence against Young Women: Prevalence and Associated Factors in Europe. J. Epidemiol. Community Health 2018, 72, 611–616. [Google Scholar] [CrossRef]
- Yakubovich, A.R.; Stöckl, H.; Murray, J.; Melendez-Torres, G.J.; Steinert, J.I.; Glavin, C.E.Y.; Humphreys, D.K. Risk and Protective Factors for Intimate Partner Violence against Women: Systematic Review and Meta-analyses of Prospective-Longitudinal Studies. Am. J. Public Health 2018, 108, e1–e11. [Google Scholar] [CrossRef]
- Herbert, A.; Heron, J.; Barter, C.; Szilassy, E.; Barnes, M.; Howe, L.D.; Feder, G.; Fraser, A. Risk Factors for Intimate Partner Violence and Abuse among Adolescents and Young Adults: Findings from a UK Population-based Cohort. Wellcome Open Res. 2020, 5, 176. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, E.; Salivar, E.G. Using a Vulnerability-stress-adaptation Framework to Model Intimate Partner Violence Risk Factors in Late Life: A Systematic Review. Aggress. Violent Behav. 2021, 57. [Google Scholar] [CrossRef]
- Gracia, E. Unreported Cases of Domestic Violence against Women: Towards an Epidemiology of Social Silence, Tolerance, and Inhibition. J. Epidemiol. Community Health 2004, 58, 536–537. [Google Scholar] [CrossRef]
- Hester, M. Making it through the Criminal Justice System: Attrition and Domestic Violence. Soc. Policy Soc. 2006, 5, 79–90. [Google Scholar] [CrossRef]
- Fanslow, J.L.; Robinson, E.M. Help-seeking Behaviors and Reasons for Help Seeking Reported by a Representative Sample of Women Victims of Intimate Partner Violence in New Zealand. J. Interpers. Violence 2006, 25, 929–951. [Google Scholar] [CrossRef]
- Fernández-González, L.; O’Leary, K.D.; Muñoz-Rivas, M.J. We Are Not Joking: Need for Controls in Reports of Dating Violence. J. Interpers. Violence 2012, 28, 602–620. [Google Scholar] [CrossRef]
- Birdsey, E.; Snowball, L. Reporting Violence to Police: A Survey of Victims Attending Domestic Violence Services. Crime Justice Stat. 2013, 91, 1–8. [Google Scholar]
- Palermo, T.; Bleck, J.; Peterman, A. Tip of the Iceberg: Reporting and Gender-Based Violence in Developing Countries. Am. J. Epidemiol. 2014, 179, 602. [Google Scholar] [CrossRef]
- Sleath, E.; Smith, L.L. Understanding the Factors that Predict Victim Retraction in Police Reported Allegations of Intimate Partner Violence. Psychol. Violence 2017, 7, 140–149. [Google Scholar] [CrossRef]
- Holliday, C.N.; Kahn, G.; Thorpe, R.J.; Shah, R.; Hameeduddin, Z.; Decker, M.R. Racial/Ethnic Disparities in Police Reporting for Partner Violence in the National Crime Victimization Survey and Survivor-Led Interpretation. J. Racial Ethn. Health Disparit. 2020, 7, 468–480. [Google Scholar] [CrossRef]
- Andrews, E.; Berghofer, K.; Long, J.; Prescott, A.; Caboral-Stevens, M. Satisfaction with the use of telehealth during COVID-19: An integrative review. Int. J. Nurs. Stud. Adv. 2020, 2, 100008. [Google Scholar] [CrossRef] [PubMed]
- Asad, M.; Sabzwari, S. Telemedicine: A New Frontier in Clinical Practice. Pak. J. Med. Sci. 2021, 37, 588–590. [Google Scholar] [CrossRef] [PubMed]
| Studies | 1. | 2. | 3. | 4. | 5. | 6. * | 7. * | 8. ** | 9. | 10. *** | 11. | 12. | 13. **** | 14. | Quality Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [41] | Y | Y | Y | Y | NR | N | N | NA | N | NA | Y | Y | NA | Y | Good |
| [42] | Y | Y | CD | Y | NR | N | N | NA | N | NA | N | Y | NA | Y | Fair |
| [43] | Y | Y | Y | NR | NR | N | N | NA | N | NA | N | Y | NA | N | Poor |
| [44] | Y | N | Y | Y | NR | N | N | NA | Y | NA | Y | Y | NA | Y | Good |
| [45] | Y | Y | Y | Y | Y | N | N | NA | N | NA | Y | Y | NA | Y | Good |
| [46] | Y | Y | Y | Y | Y | N | N | NA | N | NA | Y | Y | NA | N | Good |
| [47] | Y | Y | Y | Y | NR | N | N | NA | N | NA | Y | Y | NA | CD | Fair |
| [48] | Y | N | CD | Y | NR | N | N | NA | N | NA | N | Y | NA | CD | Poor |
| Studies | 1. | 2. | 3. | 4. * | 5. ** | 6. | 7. | 8. | 9. *** | 10. | 11. | 12. **** | Quality Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [10] | Y | Y | Y | CD | NA | Y | Y | Y | NA | N | N | NA | Good |
| [15] | Y | Y | Y | CD | NA | Y | Y | Y | NA | Y | Y | NA | Good |
| [20] | Y | Y | Y | CD | NA | Y | Y | Y | NA | Y | Y | NA | Good |
| [28] | Y | Y | N | CD | NA | N | Y | N | NA | Y | N | NA | Fair |
| [29] | Y | Y | N | CD | NA | Y | Y | NR | NA | Y | N | NA | Fair |
| [39] | Y | CD | Y | CD | NA | N | N | CD | NA | N | N | NA | Excluded |
| [49] | NR | N | Y | CD | NA | Y | Y | Y | NA | Y | Y | NA | Good |
| [50] | Y | Y | N | CD | NA | Y | Y | Y | NA | Y | Y | NA | Good |
| [51] | Y | Y | N | CD | NA | Y | Y | CD | NA | N | N | NA | Fair |
| [52] | NR | Y | N | CD | NA | Y | Y | NR | NA | N | N | NA | Poor |
| [53] | Y | Y | Y | CD | NA | Y | Y | Y | NA | Y | Y | NA | Good |
| [54] | Y | N | Y | CD | NA | Y | Y | Y | NA | Y | Y | NA | Good |
| Authors | 2020 SAH Period (*) | 2020 Target Period | Country | Sample Details | Assessment of IPV | Assessment of Other Variables | |||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean Age (SD) | Gender | Ethnicity | ||||||
| [41] | March–July | April–July | Nepal | 556 | 25.93 (6.88) | F = 48.7% PnS = 0.4% | NA | AdHoc_Q | SA WHO-5 |
| [42] | March– (May) | May | Argentina | 1502 | 43.04 (11.43) | F | NA | AdHoc_Q | COVID-19_RB SC SEC |
| [43] | March– (June) | April–May | Tunisia | 751 | 37 (8.2) | F | NA | AdHoc_Q | DASS-21 FBAS |
| [44] | - | March–May | USA | 2045 | 46.63 (17.19) | F = 49.9% Ot = 1.5% | Af-Am = 11.9% As-Am = 2% Hs = 3.3% Ot = 20.1% Wt/Eu-Am = 62.6% | J-IPV | COVID19_CxS COVID-19_RB COVID-19 Status |
| [45] | (April–September) | April–May | Ethiopia | 682 | 29.78 (5.78) | F | Ethiopian: Tigray = 99% Amara = 1% | WHO VAW | SDF |
| [46] | March–May | May–June | Bangladesh | 2424 | 24.1 (4.8) | F | NA | WHO_MST | GAD-7 HFIAS |
| [47] | - | April | USA | 1730 | 42 (13) | F = 59% | Hs = 8% Ot = 6% Wt = 73% | E-HITS | COVID-19_RB SDF |
| [48] | - | - | USA | 45 | - | F | Af As | Interview | - |
| Authors | 2020 SAH Period (*) | 2020 Target Period | Country (USA State) | Sample Details | Assessment of IPV | Assessment of Other Variable | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean Age (SD) | Gender | Ethnicity | ||||||||||
| Covid Period | No Covid Period | Covid Period | No Covid Period | Covid Period | No Covid Period | Covid Period | No Covid Period | ||||||
| [10] | (March–May) | January–May | Australia | - | - | - | - | - | - | - | - | COPS | - |
| [15] | March–(May) | January–June | UK | PR: (2015-20): 385873 CP: (2019-20): 328385 | - | - | - | - | - | - | PR/ CP | - | |
| [20] | (March–May) | January–March | USA (CA) | 47252 | 685615 | - | - | - | - | - | - | PR | - |
| [28] | (April–June) | March–May | USA (MA) | 62 | 342 | 37 (13) | 41 (15) | F = 96% | F = 95% | AfAm = 8% Hs = 15% Ot = 12% Wt = 65% | AfAm = 36% Hs = 24% Ot = 14% Wt = 26% | EMR | ISS |
| [29] | March–April | March–April | USA (SC) | 50 | 78 | 34.3 (12.4) | 33.1 (15.6) | F = 38% | F = 47.4% | Bk = 22.0% Ot = 6% Ukn = 0% Wt = 72% | Bk = 28.2% Ot = 10.3% Ukn = 1.3% Wt = 60.3% | EDA | - |
| [49] | (March–May) | January–July | Peru | 4075 | - | - | - | - | - | - | - | CH | DSH |
| [50] | March–(May) | February–May | Mexico | - | - | - | - | F | - | - | - | CH | - |
| [51] | (March–May) | March–April | USA (IL) | 62 | 88 | 32.4 (19.1) | 36.9 (18.7) | F = 27.42% | F = 27.27% | AfAm = 80.7% As = 0% Cc = 12.9% Hs = 6.5% | AfAm = 75.0% As = 2.3% Cc = 13.6% Hs = 9.9% | EMR | - |
| [52] | (March–May) | March–April | UK | 30 | 94 | 30.6 | 31 | F = 10% | F = 4.26% | - | - | EMR | - |
| [53] | March–May | January–April | USA (IL) | - | - | - | - | - | - | - | - | PR/ CP/Arrests | L-Train SafeGraph Vehicular Traffic |
| [54] | March–(May) | January–May | Mexico | - | - | - | - | - | - | - | - | PR | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lausi, G.; Pizzo, A.; Cricenti, C.; Baldi, M.; Desiderio, R.; Giannini, A.M.; Mari, E. Intimate Partner Violence during the COVID-19 Pandemic: A Review of the Phenomenon from Victims’ and Help Professionals’ Perspectives. Int. J. Environ. Res. Public Health 2021, 18, 6204. https://doi.org/10.3390/ijerph18126204
Lausi G, Pizzo A, Cricenti C, Baldi M, Desiderio R, Giannini AM, Mari E. Intimate Partner Violence during the COVID-19 Pandemic: A Review of the Phenomenon from Victims’ and Help Professionals’ Perspectives. International Journal of Environmental Research and Public Health. 2021; 18(12):6204. https://doi.org/10.3390/ijerph18126204
Chicago/Turabian StyleLausi, Giulia, Alessandra Pizzo, Clarissa Cricenti, Michela Baldi, Rita Desiderio, Anna Maria Giannini, and Emanuela Mari. 2021. "Intimate Partner Violence during the COVID-19 Pandemic: A Review of the Phenomenon from Victims’ and Help Professionals’ Perspectives" International Journal of Environmental Research and Public Health 18, no. 12: 6204. https://doi.org/10.3390/ijerph18126204
APA StyleLausi, G., Pizzo, A., Cricenti, C., Baldi, M., Desiderio, R., Giannini, A. M., & Mari, E. (2021). Intimate Partner Violence during the COVID-19 Pandemic: A Review of the Phenomenon from Victims’ and Help Professionals’ Perspectives. International Journal of Environmental Research and Public Health, 18(12), 6204. https://doi.org/10.3390/ijerph18126204










