Muscle Strength and Physical Performance Are Associated with Reaction Time Performance in Older People
Abstract
1. Introduction
2. Materials and Methods
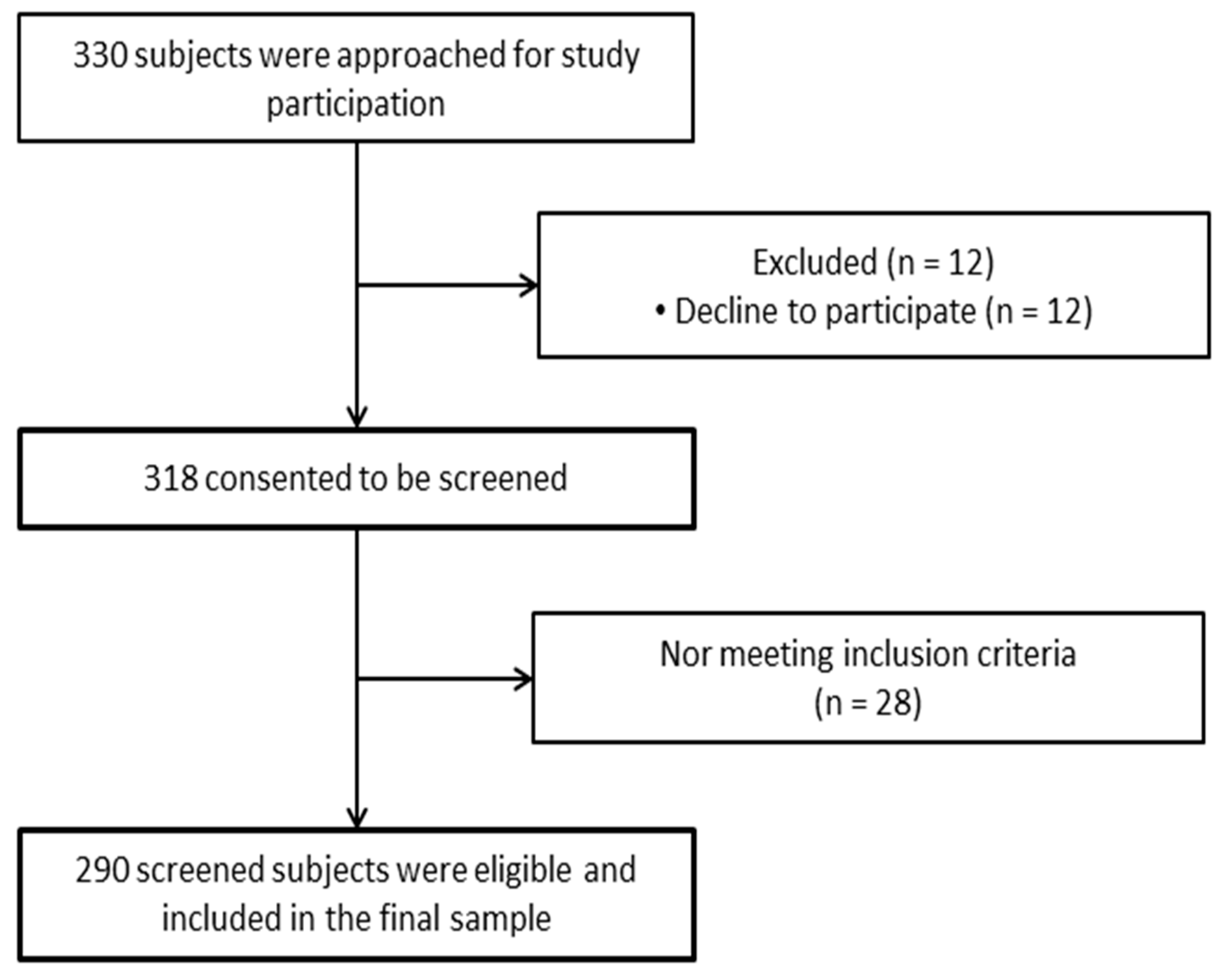
2.1. Study Design and Participants
2.2. Study Outcomes
2.2.1. Sociodemographic and Anthropometric Data
2.2.2. Gait Speed
2.2.3. Functional Mobility
2.2.4. Handgrip Strength
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beaudart, C.; Zaaria, M.; Pasleau, F.; Reginster, J.-Y.; Bruyère, O. Health outcomes of sarcopenia: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0169548. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Landi, F.; Topinková, E.; Michel, J.-P. Understanding sarcopenia as a geriatric syndrome. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 1–7. [Google Scholar] [CrossRef]
- Shafiee, G.; Keshtkar, A.; Soltani, A.; Ahadi, Z.; Larijani, B.; Heshmat, R. Prevalence of sarcopenia in the world: A systematic review and meta- analysis of general population studies. J. Diabetes Metab. Disord. 2017, 16, 1–10. [Google Scholar] [CrossRef]
- Reginster, J.-Y.; Cooper, C.; Rizzoli, R.; Kanis, J.A.; Appelboom, G.; Bautmans, I.; Bischoff-Ferrari, H.A.; Boers, M.; Brandi, M.L.; Bruyere, O.; et al. Recommendations for the conduct of clinical trials for drugs to treat or prevent sarcopenia. Aging Clin. Exp. Res. 2016, 28, 47–58. [Google Scholar] [CrossRef]
- Morley, J.E. Sarcopenia: Diagnosis and treatment. J. Nutr. Health Aging 2008, 12, 452–456. [Google Scholar] [CrossRef]
- World Health Organization. Ageing and Life Course. 2009. Available online: http://www.who.int/ageing/en/ (accessed on 28 February 2021).
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Landi, F.; Liperoti, R.; Russo, A.; Giovannini, S.; Tosato, M.; Capoluongo, E.; Bernabei, R.; Onder, G. Sarcopenia as a risk factor for falls in elderly individuals: Results from the ilSIRENTE study. Clin. Nutr. 2012, 31, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E. Frailty and sarcopenia in elderly. Wien. Klin. Wochenschr. 2016, 128, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Cherubini, A.; Cesari, M.; Calvani, R.; Tosato, M.; Sisto, A.; Martone, A.; Bernabei, R.; Marzetti, E. Sarcopenia and frailty: From theoretical approach into clinical practice. Eur. Geriatr. Med. 2016, 7, 197–200. [Google Scholar] [CrossRef]
- Rizzoli, R.; Reginster, J.-Y.; Arnal, J.F.; Bautmans, I.; Beaudart, C.; Bischoff-Ferrari, H.; Biver, E.; Boonen, S.; Brandi, M.-L.; Chines, A.; et al. Quality of Life in Sarcopenia and Frailty. Calcif. Tissue Int. 2013, 93, 101–120. [Google Scholar] [CrossRef]
- Beaudart, C.; Bauer, J.M.; Landi, F.; Bruyère, O.; Reginster, J.-Y.; Hiligsmann, M. Experts’ preferences for sarcopenia outcomes: A discrete-choice experiment from a working group of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) in collaboration with the European Union of Geriatric Medicine Society (EUGMS). Aging Clin. Exp. Res. 2021, 33, 1079–1083. [Google Scholar] [CrossRef]
- Newman, A.B.; Kupelian, V.; Visser, M.; Simonsick, E.M.; Goodpaster, B.H.; Kritchevsky, S.B.; Tylavsky, F.A.; Rubin, S.M.; Harris, T.B. Strength, But Not Muscle Mass, Is Associated With Mortality in the Health, Aging and Body Composition Study Cohort. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2006, 61, 72–77. [Google Scholar] [CrossRef]
- Lajoie, Y.; Gallagher, S. Predicting falls within the elderly community: Comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch. Gerontol. Geriatr. 2004, 38, 11–26. [Google Scholar] [CrossRef]
- Schonnop, R.; Yang, Y.; Feldman, F.; Robinson, E.; Loughin, M.; Robinovitch, S.N. Prevalence of and factors associated with head impact during falls in older adults in long-term care. Can. Med. Assoc. J. 2013, 185, E803–E810. [Google Scholar] [CrossRef]
- Lord, S.R.; Dayhew, J. Visual Risk Factors for Falls in Older People. J. Am. Geriatr. Soc. 2001, 49, 508–515. [Google Scholar] [CrossRef]
- Coin, A.; Sarti, S.; Ruggiero, E.; Giannini, S.; Pedrazzoni, M.; Minisola, S.; Rossini, M.; Del Puente, A.; Inelmen, E.M.; Manzato, E.; et al. Prevalence of Sarcopenia Based on Different Diagnostic Criteria Using DEXA and Appendicular Skeletal Muscle Mass Reference Values in an Italian Population Aged 20 to 80. J. Am. Med. Dir. Assoc. 2013, 14, 507–512. [Google Scholar] [CrossRef]
- Pahor, M.; Manini, T.; Cesari, M. Sarcopenia: Clinical evaluation, biological markers and other evaluation tools. J. Nutr. Health Aging 2009, 13, 724–728. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association With Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef]
- Evans, W.J.; Bhasin, S.; Cress, E.; Espeland, M.A.; Ferrucci, L.; Fried, L.P.; Gill, T.M.; Pahor, M.; Studenski, S.; Guralnik, J.; et al. Functional outcomes for clinical trials in frail older persons: Time to be moving. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2008, 63, 160–164. [Google Scholar]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Faulkner, K.A.; Redfern, M.S.; Cauley, J.A.; Landsittel, D.P.; Studenski, S.A.; Rosano, C.; Simonsick, E.M.; Harris, T.B.; Shorr, R.I.; Ayonayon, H.N.; et al. Multitasking: Association Between Poorer Performance and a History of Recurrent Falls. J. Am. Geriatr. Soc. 2007, 55, 570–576. [Google Scholar] [CrossRef]
- Concato, J.; Peduzzi, P.; Holford, T.R.; Feinstein, A.R. Importance of events per independent variable in proportional hazards analysis I. Background, goals, and general strategy. J. Clin. Epidemiol. 1995, 48, 1495–1501. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the Probability for Falls in Community-Dwelling Older Adults Using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.; Mesa, J.L.; Gutiérrez, A.; Castillo, M.J. Hand size influences optimal grip span in women but not in men. J. Hand Surg. 2002, 27, 897–901. [Google Scholar] [CrossRef]
- Jakobsen, L.H.; Sorensen, J.M.; Rask, I.K.; Jensen, B.S.; Kondrup, J. Validation of reaction time as a measure of cognitive function and quality of life in healthy subjects and patients. Nutrition 2011, 27, 561–570. [Google Scholar] [CrossRef]
- Choudhary, A.K.; Jiwane, R.; Alam, T.; Kishanrao, S.S. Grip Strength and Impact on Cognitive Function in Healthy Kitchen Workers. Achiev. Life Sci. 2016, 10, 168–174. [Google Scholar] [CrossRef]
- Kansu, K.; Yerlikaya, T.; Angin, S. Relationship between grip strength and reaction time in three different age groups. In Proceedings of the 3rd National Physiotherapy and Rehabilitation Congress, Physiotherapy and Rehabilitation in Life without Pain, Lefke, Cyprus, 6–8 December 2018. [Google Scholar]
- Wiśniowska-Szurlej, A.; Ćwirlej-Sozańska, A.; Wołoszyn, N.; Sozański, B.; Wilmowska-Pietruszyńska, A. Association between Handgrip Strength, Mobility, Leg Strength, Flexibility, and Postural Balance in Older Adults under Long-Term Care Facilities. BioMed Res. Int. 2019, 2019, 1–9. [Google Scholar] [CrossRef]
- Visser, M.; Deeg, D.J.; Lips, P.; Harris, T.B.; Bouter, L.M. Skeletal Muscle Mass and Muscle Strength in Relation to Lower-Extremity Performance in Older Men and Women. J. Am. Geriatr. Soc. 2000, 48, 381–386. [Google Scholar] [CrossRef]
- Lauretani, F.; Russo, C.R.; Bandinelli, S.; Bartali, B.; Cavazzini, C.; Di Iorio, A.; Corsi, A.M.; Rantanen, T.; Guralnik, J.M.; Ferrucci, L. Age-associated changes in skeletal muscles and their effect on mobility: An operational diagnosis of sarcopenia. J. Appl. Physiol. 2003, 95, 1851–1860. [Google Scholar] [CrossRef]
- Chen, L.; Nelson, D.R.; Zhao, Y.; Cui, Z.A.; Johnston, J. Relationship between muscle mass and muscle strength, and the impact of comorbidities: A population-based, cross-sectional study of older adults in the United States. BMC Geriatr. 2013, 13, 74. [Google Scholar] [CrossRef] [PubMed]
- Tun, P.A.; Lachman, M.E. Age differences in reaction time and attention in a national telephone sample of adults: Education, sex, and task complexity matter. Dev. Psychol. 2008, 44, 1421–1429. [Google Scholar] [CrossRef]
- Woods, D.L.; Wyma, J.M.; Yund, E.W.; Herron, T.J.; Reed, B. Age-related slowing of response selection and production in a visual choice reaction time task. Front. Hum. Neurosci. 2015, 9, 1–12. [Google Scholar] [CrossRef]
- Fozard, J.L.; Vercruyssen, M.; Reynolds, S.L.; Hancock, P.A.; Quilter, R.E. Age Differences and Changes in Reaction Time: The Baltimore Longitudinal Study of Aging. J. Gerontol. 1994, 49, P179–P189. [Google Scholar] [CrossRef] [PubMed]
- Inui, N. Simple Reaction Times and Timing of Serial Reactions of Middle-Aged and Old Men. Percept. Mot. Ski. 1997, 84, 219–225. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Rodrigues, B.; Gonçalves, I.D.O.; Asano, R.Y.; Uchida, M.C.; Marzetti, E. The physical capabilities underlying timed “Up and Go” test are time-dependent in community-dwelling older women. Exp. Gerontol. 2018, 104, 138–146. [Google Scholar] [CrossRef]
- Campa, F.; Toselli, S.; Mazzilli, M.; Gobbo, L.; Coratella, G. Assessment of Body Composition in Athletes: A Narrative Review of Available Methods with Special Reference to Quantitative and Qualitative Bioimpedance Analysis. Nutrients 2021, 13, 1620. [Google Scholar] [CrossRef]
| Characteristics. | Values Total = 290 | Values | Men = 51 | Values | Women = 239 | ||
|---|---|---|---|---|---|---|---|
| Age (Years) | 69.35 | 5.55 | 71.37 | 5.36 | 68.74 | 5.48 | |
| BMI (kg/m2) | 29.99 | 3.91 | 30.07 | 3.87 | 29.97 | 3.93 | |
| Occupational status, n (%) | Retired | 263 | 90.68 | 38 | 74.50 | 225 | 94.15 |
| Working | 9 | 3.10 | 7 | 13.72 | 2 | 0.83 | |
| Unemployed | 18 | 6.20 | 6 | 11.78 | 12 | 5.02 | |
| Marital Status, n (%) | Single | 4 | 1.37 | 2 | 3.92 | 2 | 0.83 |
| Married/cohabiting | 185 | 63.79 | 14 | 27.45 | 171 | 71.54 | |
| Separated/divorced/widowed | 101 | 34.82 | 35 | 68.63 | 66 | 27.61 | |
| Educational status, n (%) | No formal education | 80 | 33.10 | 15 | 29.42 | 65 | 27.19 |
| Primary education | 154 | 50.92 | 28 | 54.90 | 126 | 52.71 | |
| Secondary education | 40 | 15.86 | 4 | 7.84 | 36 | 15.06 | |
| University | 16 | 7.58 | 4 | 7.84 | 12 | 5.02 | |
| Smoker, n (%) | Yes | 18 | 6.20 | 12 | 23,52 | 6 | 2.50 |
| No | 272 | 93.79 | 39 | 76,48 | 233 | 97.50 | |
| OALLRT (s) | 0.70 | 0.26 | 0.72 | 0.30 | 0.69 | 0.24 | |
| OLLRT (s) | 0.67 | 0.20 | 0.66 | 0.17 | 0.67 | 0.20 | |
| ALLRT (s) | 0.68 | 0.21 | 0.71 | 0.71 | 0.67 | 0.20 | |
| TUG test (s) | 8.21 | 2.24 | 7.96 | 2.63 | 8.29 | 2.10 | |
| Handgrip strength (kg) | 25.33 | 10.38 | 35.06 | 11.13 | 22.16 | 7.87 | |
| OALLRT (s) | OLLRT (s) | ALLRT (s) | |
|---|---|---|---|
| TUG | 0.104 | 0.091 | 0.030 |
| Handgrip Strength | −0.172 1 | −0.071 | −0.140 1 |
| Sex | −0.049 | 0.005 | −0.084 |
| Educational Status | −1.200 2 | −1.340 2 | −0.150 |
| Age (years) | 0.155 2 | 0.148 1 | 0.077 |
| BMI (kg/m2) | −0.087 | 0.073 | 0.001 |
| Variable | B | β | t | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|---|
| OALLRT (s) | Age | 0.007 | 0.105 | 1.807 | −0.01 | 0.012 | 0.021 |
| Handgrip Strength | −0.006 | −0.170 | −2.119 | −0.011 | 0.000 | 0.035 | |
| OLLRT (s) | Educational | −0.030 | −1.121 | −1.985 | −0.059 | 0.000 | 0.048 |
| Sex | 0.210 | 0.13 | 2.29 | 0.03 | 0.390 | 0.023 | |
| ALLRT (s) | Sex | −0.131 | −0.253 | −3.037 | −0.217 | −0.046 | 0.003 |
| Handgrip Strength | −0.006 | −0.228 | −2.750 | −0.011 | −0.002 | 0.006 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez-García, J.D.; Martínez-Amat, A.; Hita-Contreras, F.; Fábrega-Cuadros, R.; Álvarez-Salvago, F.; Aibar-Almazán, A. Muscle Strength and Physical Performance Are Associated with Reaction Time Performance in Older People. Int. J. Environ. Res. Public Health 2021, 18, 5893. https://doi.org/10.3390/ijerph18115893
Jiménez-García JD, Martínez-Amat A, Hita-Contreras F, Fábrega-Cuadros R, Álvarez-Salvago F, Aibar-Almazán A. Muscle Strength and Physical Performance Are Associated with Reaction Time Performance in Older People. International Journal of Environmental Research and Public Health. 2021; 18(11):5893. https://doi.org/10.3390/ijerph18115893
Chicago/Turabian StyleJiménez-García, José Daniel, Antonio Martínez-Amat, Fidel Hita-Contreras, Raquel Fábrega-Cuadros, Francisco Álvarez-Salvago, and Agustín Aibar-Almazán. 2021. "Muscle Strength and Physical Performance Are Associated with Reaction Time Performance in Older People" International Journal of Environmental Research and Public Health 18, no. 11: 5893. https://doi.org/10.3390/ijerph18115893
APA StyleJiménez-García, J. D., Martínez-Amat, A., Hita-Contreras, F., Fábrega-Cuadros, R., Álvarez-Salvago, F., & Aibar-Almazán, A. (2021). Muscle Strength and Physical Performance Are Associated with Reaction Time Performance in Older People. International Journal of Environmental Research and Public Health, 18(11), 5893. https://doi.org/10.3390/ijerph18115893











