Particulate Matter Exposure across Latino Ethnicities
Abstract
1. Introduction
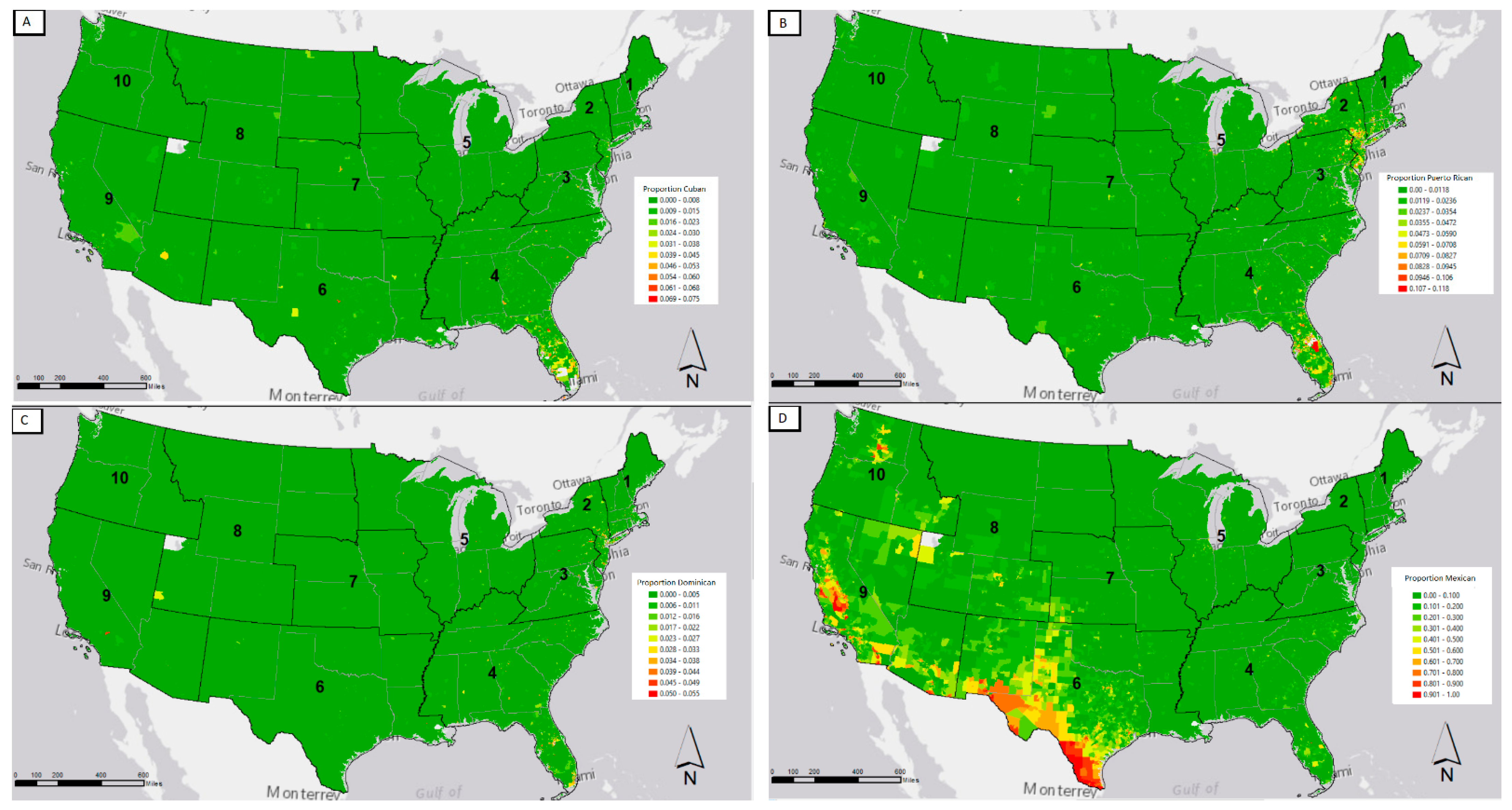
Spatial Patterns of the Latino Population
2. Materials and Methods
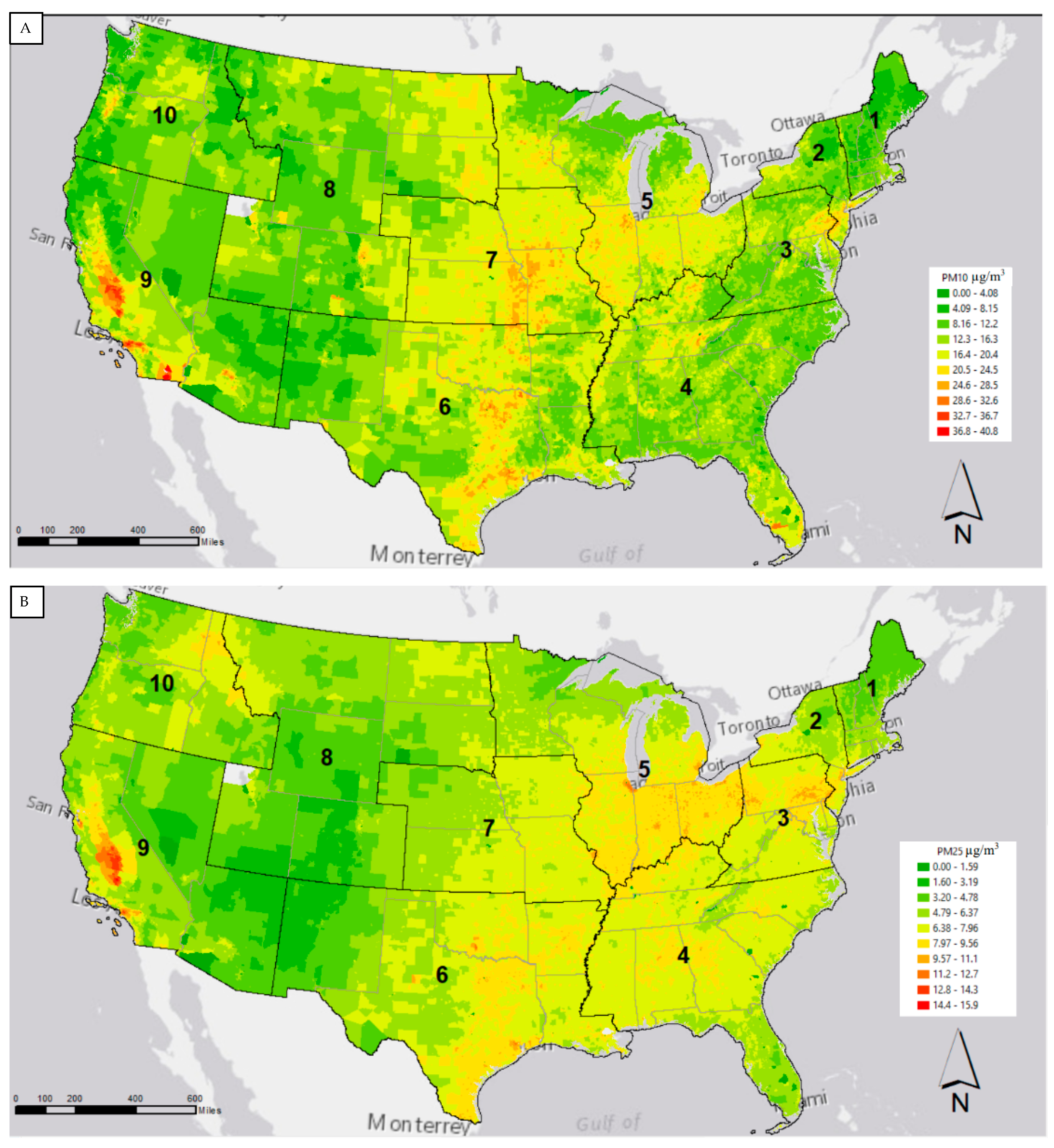
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Palloni, A.; Arias, E. Paradox lost: Explaining the hispanic adult mortality advantage. Demography 2004, 41, 385–415. [Google Scholar] [CrossRef] [PubMed]
- Hummer, R.A.; Chinn, J.J. RACE/ETHNICITY AND U.S. ADULT MORTALITY. Du Bois Rev. Soc. Sci. Res. Race 2011, 8, 5–24. [Google Scholar] [CrossRef] [PubMed]
- Ledogar, R.J.; Penchaszadeh, A.; Garden, C.C. Asthma and Latino cultures: Different prevalence reported among groups sharing the same environment. Am. J. Public Health 2000, 90, 929–935. [Google Scholar] [CrossRef][Green Version]
- Morales, L.S.; Lara, M.; Kington, R.S.; Valdez, R.O.; Escarce, J.J. Socioeconomic, Cultural, and Behavioral Factors Affecting Hispanic Health Outcomes. J. Heal. Care Poor Underserved 2002, 13, 477–503. [Google Scholar] [CrossRef]
- Lo, C.C.; Adame, J.L.; Cheng, T.C. Explaining Chronic Illness and Self-Rated Health Among Immigrants of Five Hispanic Ethnicities. J. Racial Ethn. Health Disparities 2020, 7, 177–191. [Google Scholar] [CrossRef] [PubMed]
- Basu Roy, S.; Olsen, R.N.; Tseng, H. Do Hispanic immigrants spend less on medical care? Implications of the His-panic health paradox. Appl. Econ. 2020, 52, 3951–3964. [Google Scholar] [CrossRef]
- Siañez, M.; Highfield, L.; Balcazar, H.; Collins, T.; Grineski, S. An Examination of the Association of Multiple Acculturation Measures with Asthma Status Among Elementary School Students in El Paso, Texas. J. Immigr. Minor. Health 2017, 20, 884–893. [Google Scholar] [CrossRef]
- Bacon, E.; Riosmena, F.; Rogers, R.G. Does the Hispanic health advantage extend to better management of hypertension? The role of socioeconomic status, sociobehavioral factors, and health care access. Biodemography Soc. Biol. 2017, 63, 262–277. [Google Scholar] [CrossRef]
- Arias, E.; Johnson, N.J.; Vera, B.T. Racial disparities in mortality in the adult hispanic population. SSM Popul. Health 2020, 11, 100583. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, N.A.; Pepper, D. Childhood Asthma, Air Quality, and Social Suffering Among Mexican Americans in California’s San Joaquin Valley: “Nobody Talks to Us Here”. Med. Anthr. 2009, 28, 336–367. [Google Scholar] [CrossRef]
- Grineski, S.E.; Collins, T.W.; Chakraborty, J.; McDonald, Y.J. Environmental Health Injustice: Exposure to Air Toxics and Children’s Respiratory Hospital Admissions in El Paso, Texas. Prof. Geogr. 2013, 65, 31–46. [Google Scholar] [CrossRef]
- Chen, J.; Hoek, G. Long-term exposure to PM and all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ. Int. 2020, 143, 105974. [Google Scholar] [CrossRef] [PubMed]
- Lenschow, P.; Abraham, H.; Kutzner, K.; Lutz, M.; Preub, J.; Reichenbficher, W. Some ideas about the sources of PM10. Atmos. Environ. 2001, 35, 23–33. [Google Scholar] [CrossRef]
- World Health Organization Europe. Air Quality Guidelines: Global Update 2005: Particulate Matter, Ozone, Nitrogen Dioxide, and Sulfur Dioxide; Druckpartner Moser: Verlag, Germany, 2006. [Google Scholar]
- Zhang, Y.; Zhang, L.; Wei, J.; Liu, L.; Wang, Y.; Liu, J.; Zhou, P.; Wang, L.; Ding, Z.; Zhang, Y. Size-specific particulate air pollution and hospitalization for cardiovascular diseases: A case-crossover study in Shenzhen, China. Atmos. Environ. 2021, 251, 118271. [Google Scholar] [CrossRef]
- Lin, L.; Li, T.; Sun, M.; Liang, Q.; Ma, Y.; Wang, F.; Duan, J.; Sun, Z. Effect of particulate matter exposure on the prevalence of allergic rhinitis in children: A systematic review and meta-analysis. Chemosphere 2021, 268, 128841. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, W.; Gu, X.; Deng, F.; Wang, X.; Lin, H.; Guo, X.; Wu, S. Association between particulate matter air pollution and risk of depression and suicide: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. 2021, 28, 9029–9049. [Google Scholar] [CrossRef] [PubMed]
- Egeghy, P.P.; Judson, R.; Gangwal, S.; Mosher, S.; Smith, D.; Vail, J.; Hubal, E.A.C. The exposure data landscape for manufactured chemicals. Sci. Total. Environ. 2012, 414, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Committee on Community-Based Solutions to Promote Health Equity in the United States; Board on Population Health and Public Health Practice; Health and Medicine Division Communities in Action. Communities in Action; National Academies Press: Washington, DC, USA, 2017. [Google Scholar]
- Johnson, A.C.; Jin, X.; Nakada, N.; Sumpter, J.P. Learning from the past and considering the future of chemicals in the environment. Science 2020, 367, 384–387. [Google Scholar] [CrossRef]
- Vineis, P.; Robinson, O.; Chadeau-Hyam, M.; Dehghan, A.; Mudway, I.; Dagnino, S. What is new in the exposome? Environ. Int. 2020, 143, 105887. [Google Scholar] [CrossRef]
- Park, R.E. Human Ecology. Am. J. Sociol. 1936, 42, 1–15. [Google Scholar] [CrossRef]
- Lobo, A.P.; Flores, R.O.; Salvo, J.J. The Overlooked Ethnic Dimension of Hispanic Subgroup Settlement in New York City. Urban. Geogr. 2007, 28, 609–634. [Google Scholar] [CrossRef]
- Zong, J.; Batalova, J. Dominican Immigrants in the United States. Migration Policy Institute 2018. Available online: https://www.migrationpolicy.org/article/dominican-immigrants-united-states-2016 (accessed on 2 March 2021).
- U.S. Census Bureau. Social Explorer Tables: ACS 2019 (5-Year Estimates) (SE), ACS 2019 (5-Year Estimates), Social Explorer. Available online: https://www.socialexplorer.com/data/ACS2019_5yr (accessed on 1 March 2021).
- U.S. Bureau of Labor Statistics. Available online: https://www.bls.gov/opub/ted/2015/hispanics-and-latinos-in-industries-and-occupations.htm (accessed on 1 March 2021).
- Hernández-Valero, M.A.; Bondy, M.L.; Spitz, M.R.; Zahm, S.H. Evaluation of Mexican American migrant farmworker work practices and organochlorine pesticide metabolites. Am. J. Ind. Med. 2001, 40, 554–560. [Google Scholar] [CrossRef]
- Welton, M.; Shen, Y.; Ebell, M.; DeJoy, D.; Robb, S.W. Construction employment mortality among Mexican immigrants in the South Eastern United States, 2003–2013. Int. J. Migr. Heal. Soc. Care 2020, 16, 349–358. [Google Scholar] [CrossRef]
- Niño, M.D.; Hearne, B.N. Dimensions of acculturation and biological dysregulation among Latina/os: The role of ethnic background, gender, and immigrant generation. Ethn. Health 2020, 1–17. [Google Scholar] [CrossRef]
- Godoy, R.; Jenkins, G.P.; Patel, K. Puerto Rican Migration: An Assessment of Quantitative Studies. Cent. J. 2003, XV, 206–231. [Google Scholar]
- Library of Congress (LOC). Migrating to a New Land. Available online: https://www.loc.gov/classroom-materials/immigration/puerto-rican-cuban/migrating-to-a-new-land/# (accessed on 2 March 2021).
- Easley, J. Spatial mismatch beyond black and white: Levels and determinants of job access among Asian and Hispanic subpopulations. Urban. Stud. 2018, 55, 1800–1820. [Google Scholar] [CrossRef]
- Rodriguez, C.J.; Allison, M.; Daviglus, M.L.; Isasi, C.R.; Keller, C.; Leira, E.C.; Palaniappan, L.; Piña, I.L.; Ramirez, S.M.; Rodriguez, B.; et al. Status of Cardiovascular Disease and Stroke in Hispanics/Latinos in the United States: A Science Advisory from the AmericanHeart Association. Circulation 2014, 130, 593–625. [Google Scholar] [CrossRef]
- Murillo, R.; Ayalew, L.; Hernandez, D.C. The association between neighborhood social cohesion and sleep duration in Latinos. Ethn. Heal. 2019, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Adame, J.L.; Lo, C.C.; Cheng, T.C. Ethnicity and Self-reported Depression Among Hispanic Immigrants in the U.S. Community Ment. Health J. 2021, 1–15. [Google Scholar] [CrossRef]
- Jimenez, E.D.; Garza, D.M.; Cárdenas, V.; Marquine, M. Older Latino Mental Health: A Complicated Picture. Innov. Aging 2020, 4, 1–12. [Google Scholar] [CrossRef]
- Cheng, Y.J.; Kanaya, A.M.; Araneta, M.R.G.; Saydah, S.H.; Kahn, H.S.; Gregg, E.W.; Fujimoto, W.Y.; Imperatore, G. Prevalence of Diabetes by Race and Ethnicity in the United States, 2011–2016. JAMA 2019, 322, 2389–2398. [Google Scholar] [CrossRef]
- Kim, S.-Y.; Bechle, M.; Hankey, S.; Sheppard, L.; Szpiro, A.A.; Marshall, J.D. Concentrations of criteria pollutants in the contiguous U.S., 1979–2015: Role of prediction model parsimony in integrated empirical geographic regression. PLoS ONE 2020, 15, e0228535. [Google Scholar] [CrossRef]
- US EPA EasyRSEI Dashboard Version 2.3.9. Available online: https://edap.epa.gov/public/extensions/EasyRSEI/EasyRSEI.html. (accessed on 1 April 2021).
- The EasyRSEI Program Assigns a Health Risk to Each Chemical Based on Peer-Reviewed Studies with the Goal of Making the Different Health Risks of Chemicals Comparable to One Another. Available online: https://www.epa.gov/rsei/get-easyrsei (accessed on 12 May 2021).
- Ard, K. Trends in Exposure to industrial air toxins for different racial and socioeconomic groups: A spatial and temporal examination of environmental inequality in the U.S. from 1995 to 2004. Soc. Sci. Res. 2015, 53, 375–390. [Google Scholar] [CrossRef] [PubMed]
- Wilbur, S.; Abadin, H.; Fay, M.; Yu, D.; Tencza, B.; Ingerman, L.; Klotzbach, J.; James, S. Toxicological Profile for Chromium; Relevance to Public Health; Agency for Toxic Sub-Stances and Disease Registry: Atlanta GA, USA, 2012. [Google Scholar]
- Suh, M.; Thompson, C.M.; Brorby, G.P.; Mittal, L.; Proctor, D.M. Inhalation cancer risk assessment of cobalt metal. Regul. Toxicol. Pharm. 2016, 79, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Jinot, J.; Fritz, J.M.; Vulimiri, S.V.; Keshava, N. Carcinogenicity of ethylene oxide: Key findings and scientific issues. Toxicol. Mech. Methods 2017, 28, 386–396. [Google Scholar] [CrossRef]
- Järup, L. Hazards of heavy metal contamination. Br. Med. Bull. 2003, 68, 167–182. [Google Scholar] [CrossRef]
- Schaumlöffel, D. Nickel species: Analysis and toxic effects. J. Trace Elem. Med. Biol. 2012, 26, 1–6. [Google Scholar] [CrossRef]
- Hughes, K.; Meek, M.E.; Walker, M.; Beauchamp, R. 1,3-Butadiene: Exposure Estimation, Hazard Characterization, and Exposure-Response Analysis. J. Toxicol. Environ. Health Part B 2003, 6, 55–83. [Google Scholar] [CrossRef] [PubMed]
- Melnick, R.L.; Sills, R.C.; Portier, C.J.; Roycroft, J.H.; Chou, B.J.; Grumbein, S.L.; Miller, R.A. Multiple organ carcinogenicity of inhaled chloroprene (2-chloro-1,3-butadiene) in F344/N rats and B6C3F1 mice and comparison of dose–response with 1,3-butadiene in mice. Carcinogenesis 1999, 20, 867–878. [Google Scholar] [CrossRef]
- Allen, J.; Balfour, R.; Bell, R.; Marmot, M. Social determinants of mental health. Int. Rev. Psychiatry 2014, 26, 392–407. [Google Scholar] [CrossRef]
- Vermeulen, R.; Schymanski, E.L.; Barabási, A.-L.; Miller, G.W. The exposome and health: Where chemistry meets biology. Science 2020, 367, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Cifuentes, P.; Reichard, J.; Im, W.; Smith, S.; Colen, C.; Giurgescu, C.; Williams, K.P.; Gillespie, S.; Juarez, P.D.; Hood, D.B. Application of the Public Health Exposome Framework to Estimate Phenotypes of Resilience in a Model Ohio African-American Women’s Cohort. J. Hered. 2019, 96, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Portes, A.; Zhou, M. The New Second Generation: Segmented Assimilation and its Variants. Ann. Am. Acad. Politi. Soc. Sci. 1993, 530, 74–96. [Google Scholar] [CrossRef]
- Lee, B.A.; Martin, M.J.R. Whither the urban diaspora? The spatial redistribution of Latino origin groups in metropolitan America since 1990. J. Urban. Aff. 2019, 41, 960–980. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Xie, J.; Huang, F.; Cao, L. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci. Total Environ. 2020, 727, 138704. [Google Scholar] [CrossRef] [PubMed]
| EPA Region 1 | EPA Region 2 | EPA Region 3 | EPA Region 4 | EPA Region 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| NAICS 3 Digit Code | % | NAICS 3 Digit Code | % | NAICS 3 Digit Code | % | NAICS 3 Digit Code | % | NAICS 3 Digit Code | % |
| Fabricated Metal | 18.36 | Chemical | 23.32 | Chemical | 14.18 | Chemical | 15.18 | Fabricated Metal | 18.46 |
| Computer and Electronic | 10.94 | Fabricated Metal | 13.17 | Fabricated Metal | 13.49 | Fabricated Metal | 9.89 | Chemical | 13.27 |
| Chemical | 10.75 | Computer and Electronic | 6.60 | Primary Metal | 8.25 | Plastics and Rubber | 7.84 | Transportation Equipment | 8.89 |
| Miscellaneous Manufacturing | 6.24 | Primary Metal | 6.12 | Food | 6.41 | Transportation Equipment | 7.63 | Primary Metal | 8.50 |
| Primary Metal | 5.93 | Food | 5.45 | Plastics and Rubber | 6.26 | Food | 6.73 | Plastics and Rubber | 7.78 |
| Plastics and Rubber | 5.47 | Plastics and Rubber | 4.48 | Nonmetallic Mineral Product | 5.73 | Wood Product | 5.85 | Food | 6.66 |
| Elec. Equip., Appliance, Component | 4.94 | Merchant Wholesaler, Nondurable | 4.03 | Machinery | 4.91 | Primary Metal | 4.90 | Machinery | 5.99 |
| Machinery | 4.91 | Machinery | 4.00 | Computer and Electronic | 4.91 | Nonmetallic Mineral Product | 4.77 | Computer and Electronic | 4.62 |
| Paper | 4.54 | Nonmetallic Mineral Product | 3.91 | Transportation Equipment | 4.25 | Machinery | 4.29 | Nonmetallic Mineral Product | 3.42 |
| Nonmetallic Mineral Product | 4.22 | Paper | 3.69 | Wood Product | 3.49 | Textile Mills | 3.97 | Elec. Equip., Appliance, Component | 3.08 |
| Total Region 1 TRI Facilities 3129 | Total Region 2 TRI Facilities 3302 | Total Region 3 TRI Facilities 4521 | Total Region 4 TRI Facilities 9896 | Total Region 5 TRI Facilities 12,590 | |||||
| EPA Region 6 | EPA Region 7 | EPA Region 8 | EPA Region 9 | EPA Region 10 | |||||
| NAICS 3 Digit Code | % | NAICS 3 Digit Code | % | NAICS 3 Digit Code | % | NAICS 3 Digit Code | % | NAICS 3 Digit Code | % |
| Chemical | 19.13 | Food | 16.47 | Chemical | 11.60 | Chemical | 14.57 | Wood Product | 12.72 |
| Fabricated Metal | 12.39 | Chemical | 14.80 | Fabricated Metal | 10.99 | Computer and Electronic | 14.04 | Food | 11.90 |
| Food | 8.06 | Fabricated Metal | 11.09 | Food | 9.64 | Fabricated Metal | 13.40 | Chemical | 10.65 |
| Transportation Equipment | 6.11 | Transportation Equipment | 7.61 | Nonmetallic Mineral Product | 9.19 | Nonmetallic Mineral Product | 6.55 | Fabricated Metal | 9.15 |
| Plastics and Rubber | 6.09 | Machinery | 7.22 | Computer and Electronic | 8.13 | Food | 6.18 | Computer and Electronic | 7.96 |
| Merchant Wholesale, Nondurable | 5.79 | Plastics and Rubber | 6.23 | Machinery | 4.97 | Plastics and Rubber | 5.47 | Transportation Equipment | 7.89 |
| Machinery | 5.50 | Nonmetallic Mineral Product | 5.51 | Plastics and Rubber | 4.82 | Transportation Equipment | 5.22 | Nonmetallic Mineral Product | 6.39 |
| Primary Metal | 5.14 | Primary Metal | 4.43 | Transportation Equipment | 4.52 | Primary Metal | 4.22 | Primary Metal | 5.45 |
| Nonmetallic Mineral Product | 4.81 | Elec. Equip., Appliance, Component | 2.95 | Miscellaneous Manufacturing | 4.29 | Machinery | 3.45 | Plastics and Rubber | 5.26 |
| Computer and Electronic | 4.41 | Computer and Electronic | 2.89 | Petroleum and Coal Products | 4.07 | Merchant Wholesale, Nondurable | 3.22 | Machinery | 3.57 |
| Total Region 6 TRI Facilities 5077 | Total Region 7 TRI Facilities 3048 | Total Region 8 TRI Facilities 1328 | Total Region 9 TRI Facilities 5098 | Total Region 10 TRI Facilities 1596 |
| Census Tract Density of Industrial Facilities by Primary 3-Digit NAICS Code | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wholesale | Machinery | Primary Metal | Computer & Electronics | Mineral | Plastics & Rubber | Transport. | Food | Fab. Metal | Chemical | ||
| Proportion of Tract Population | Dominican | 0.08 | 0.03 | 0.08 | 0.07 | 0.06 | 0.03 | 0.05 | 0.05 | 0.11 | 0.20 |
| Cuban | 0.01 | 0.01 | 0.00 | 0.03 | 0.02 | 0.03 | 0.04 | 0.00 | 0.01 | 0.03 | |
| Puerto Rican | 0.07 | 0.05 | 0.12 | 0.08 | 0.06 | 0.06 | 0.04 | 0.05 | 0.17 | 0.16 | |
| Mexican | 0.06 | 0.06 | 0.05 | 0.05 | 0.06 | 0.05 | 0.05 | 0.08 | 0.10 | 0.07 | |
| White | −0.11 | −0.08 | −0.11 | −0.10 | −0.12 | −0.08 | −0.11 | −0.12 | −0.19 | −0.20 | |
| EPA REGION 1 | EPA REGION 2 | EPA REGION 3 | EPA REGION 4 | EPA REGION 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Chemical | Percent Contribution | Chemical | Percent Contribution | Chemical | Percent Contribution | Chemical | Percent Contribution | Chemical | Percent Contribution |
| Chromium | 34% | Ethylene oxide | 53% | Ethylene oxide | 38% | Ethylene oxide | 26% | Chromium | 27% |
| Cobalt compounds | 18% | Cobalt | 12% | Chromium compounds | 33% | Chromium | 22% | Ethylene oxide | 22% |
| Cobalt | 10% | Chromium | 10% | Chromium | 10% | Chromium compounds | 16% | Cobalt | 19% |
| Nickel compounds | 9% | Nickel | 5% | Nitroglycerin | 3% | Arsenic compounds | 6% | Chromium compounds | 13% |
| Ethylene oxide | 6% | Chromium compounds | 4% | Nickel | 3% | Cobalt compounds | 4% | Cobalt compounds | 4% |
| 77% | 83% | 87% | 74% | 86% | |||||
| EPA REGION 6 | EPA REGION 7 | EPA REGION 8 | EPA REGION 9 | EPA REGION 10 | |||||
| Chemical | Percent Contribution | Chemical | Percent Contribution | Chemical | Percent Contribution | Chemical | Percent Contribution | Chemical | Percent Contribution |
| Ethylene oxide | 59% | Chromium | 39% | Ethylene oxide | 61% | Chromium | 24% | Chromium compounds | 49% |
| Chromium | 8% | Ethylene oxide | 22% | Chromium | 14% | Ethylene oxide | 20% | Cobalt | 20% |
| 1,3-Butadiene | 7% | Chromium compounds | 18% | Arsenic compounds | 12% | Chromium compounds | 17% | Chromium | 9% |
| Chloroprene | 5% | Nickel | 5% | Chromium compounds | 2% | Cobalt | 8% | Nickel | 7% |
| Propyleneimine | 4% | Nitroglycerin | 3% | Hydrogen sulfide | 2% | Arsenic compounds | 7% | Formaldehyde | 5% |
| 84% | 87% | 91% | 76% | 89% | |||||
| Percent Tract: | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| coeff. | SE | coeff. | SE | coeff. | SE | coeff. | SE | coeff. | SE | coeff. | SE | |||||||
| White | ref. | ref. | ref. | ref. | ref. | ref. | ||||||||||||
| Hispanic | 5.48 | ** | 0.08 | |||||||||||||||
| African American | 2.23 | ** | 0.07 | 2.42 | ** | 0.07 | 2.40 | ** | 0.07 | 2.26 | ** | 0.07 | 2.25 | ** | 0.07 | 2.01 | ** | 2.01 |
| Hispanic White | 6.83 | ** | 0.11 | 3.74 | ** | 0.13 | ||||||||||||
| Hispanic Black | −5.19 | ** | 1.55 | −7.82 | ** | 1.52 | ||||||||||||
| Foreign-Born | 7.74 | ** | 0.15 | 7.71 | ** | 0.15 | 6.52 | ** | 0.16 | |||||||||
| Cuban | 9.65 | ** | 0.41 | 2.84 | ** | 0.42 | 3.98 | ** | 0.44 | |||||||||
| Dominican | −7.98 | ** | 0.61 | −10.51 | ** | 0.60 | −8.23 | ** | 0.61 | |||||||||
| Mexican | 6.35 | ** | 0.10 | 4.15 | ** | 0.11 | 4.01 | ** | 0.12 | |||||||||
| Puerto Rican | 2.53 | ** | 0.38 | 2.63 | ** | 0.37 | 0.61 | ** | 0.38 | |||||||||
| Unemp. (White) | −0.28 | 0.20 | ||||||||||||||||
| Unemp. (African American) | −0.60 | ** | 0.08 | |||||||||||||||
| Unemp. (Hispanic) | −0.48 | ** | 0.10 | |||||||||||||||
| Intercept | 16.15 | ** | 0.42 | 16.21 | ** | 0.42 | 15.88 | ** | 0.42 | 16.23 | ** | 0.41 | 15.84 | ** | 0.41 | 16.35 | ** | 0.41 |
| State (EPA Region) | 8.58 | 8.60 | 8.51 | 8.25 | 8.25 | 8.27 | ||||||||||||
| Residual | 13.47 | 13.62 | 13.15 | 13.44 | 12.97 | 12.30 | ||||||||||||
| AIC | 391,403.10 | 392,154.30 | 389,632.00 | 391,220.40 | 388,675.10 | 304,573.10 | ||||||||||||
| BIC | 391,406.90 | 392,158.10 | 389,635.80 | 391,224.20 | 388,678.90 | 304,576.80 | ||||||||||||
| N (tracts) | 71,905 | 71,905 | 71,905 | 71,905 | 71,905 | 71,905 | ||||||||||||
| Percent Tract: | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| coeff. | SE | coeff. | SE | coeff. | SE | coeff. | SE | coeff. | SE | coeff. | SE | |||||||
| White | ref. | ref. | ref. | ref. | ref. | ref. | ||||||||||||
| Hispanic | 1.69 | ** | 0.02 | |||||||||||||||
| African American | 1.58 | ** | 0.02 | 1.64 | ** | 0.02 | 1.63 | ** | 0.02 | 1.57 | ** | 0.02 | 1.56 | ** | 0.02 | 1.33 | ** | 0.02 |
| Hispanic White | 1.97 | ** | 0.03 | 1.20 | ** | 0.04 | ||||||||||||
| Hispanic Black | −2.16 | ** | 0.44 | −2.81 | ** | 0.43 | ||||||||||||
| Foreign-Born | 1.92 | ** | 0.04 | 1.97 | ** | 0.04 | 1.70 | ** | 0.04 | |||||||||
| Cuban | 0.86 | ** | 0.11 | −0.88 | ** | 0.12 | −0.80 | ** | 0.12 | |||||||||
| Dominican | −1.76 | ** | 0.17 | −2.41 | ** | 0.17 | −1.85 | ** | 0.17 | |||||||||
| Mexican | 2.04 | ** | 0.03 | 1.48 | ** | 0.03 | 1.45 | ** | 0.03 | |||||||||
| Puerto Rican | 1.73 | ** | 0.11 | 1.75 | ** | 0.10 | 1.61 | ** | 0.11 | |||||||||
| Unemp. (White) | 0.16 | 0.06 | ||||||||||||||||
| Unemp. (African American) | −0.04 | * | 0.02 | |||||||||||||||
| Unemp. (Hispanic) | −0.08 | * | 0.03 | |||||||||||||||
| Intercept | 6.96 | ** | 0.18 | 6.99 | ** | 0.18 | 6.91 | ** | 0.18 | 6.98 | ** | 0.18 | 6.88 | ** | 0.18 | 7.03 | ** | 0.18 |
| State (EPA Region) | 1.67 | 1.64 | 1.62 | 1.64 | 1.63 | 1.65 | ||||||||||||
| Residual | 1.07 | 1.09 | 1.06 | 1.06 | 1.03 | 0.9705 | ||||||||||||
| AIC | 209,072.70 | 210,537.00 | 208,614.40 | 208,866.60 | 206,769.90 | 160,182.00 | ||||||||||||
| BIC | 209,076.50 | 210,540.80 | 208,618.20 | 208,870.40 | 206,773.60 | 160,185.80 | ||||||||||||
| N (tracts) | 71,905 | 71,905 | 71,905 | 71,905 | 71,905 | 71,905 | ||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ard, K.; Fisher-Garibay, D.; Bonner, D. Particulate Matter Exposure across Latino Ethnicities. Int. J. Environ. Res. Public Health 2021, 18, 5186. https://doi.org/10.3390/ijerph18105186
Ard K, Fisher-Garibay D, Bonner D. Particulate Matter Exposure across Latino Ethnicities. International Journal of Environmental Research and Public Health. 2021; 18(10):5186. https://doi.org/10.3390/ijerph18105186
Chicago/Turabian StyleArd, Kerry, Dax Fisher-Garibay, and Daphney Bonner. 2021. "Particulate Matter Exposure across Latino Ethnicities" International Journal of Environmental Research and Public Health 18, no. 10: 5186. https://doi.org/10.3390/ijerph18105186
APA StyleArd, K., Fisher-Garibay, D., & Bonner, D. (2021). Particulate Matter Exposure across Latino Ethnicities. International Journal of Environmental Research and Public Health, 18(10), 5186. https://doi.org/10.3390/ijerph18105186






