The ASHA (Hope) Project: Testing an Integrated Depression Treatment and Economic Strengthening Intervention in Rural Bangladesh: A Pilot Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sites
2.2. The Intervention
Training and Supervision of Peer Interventionists
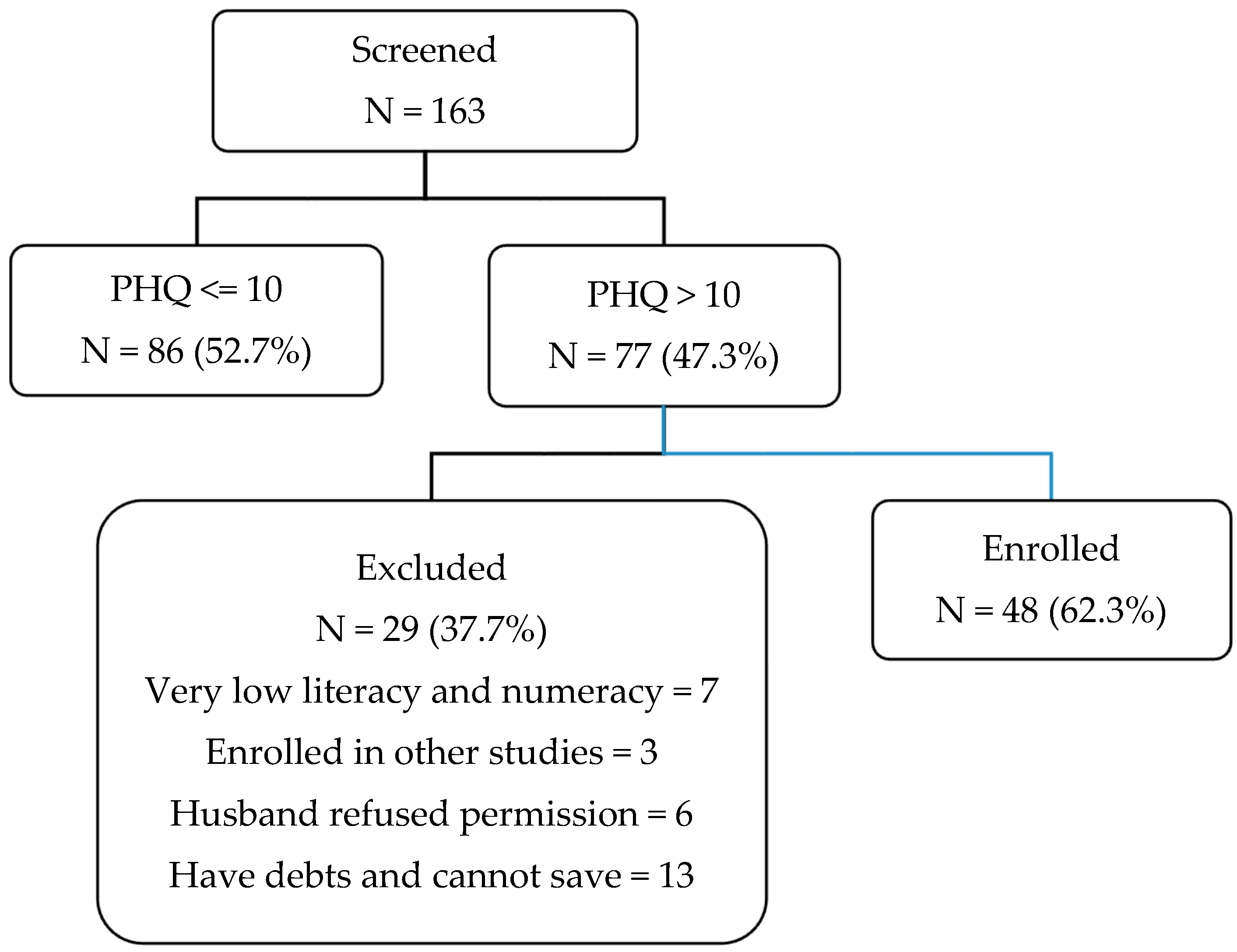
2.3. Screening and Recruitment
2.4. Measures
2.4.1. Depression
2.4.2. Other Measures
2.5. Ethics Approval and Consent to Participate
2.6. Data Analysis
3. Results
3.1. The Sample
3.2. Outcomes
3.3. Other Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Karimli, L.; Ssewamala, F.M.; Neilands, T.B.; Wells, C.R.; Bermudez, L.G. Poverty, economic strengthening, and mental health among AIDS orphaned children in Uganda: Mediation model in a randomized clinical trial. Soc. Sci. Med. 2019, 228, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Heflin, C.M.; Iceland, J. Poverty, Material Hardship and Depression. Soc. Sci. Q. 2009, 90, 1051–1071. [Google Scholar] [CrossRef] [PubMed]
- Goulding, A.N.; Rosenblum, K.L.; Miller, A.L.; Peterson, K.E.; Chen, Y.P.; Kaciroti, N.; Lumeng, J.C. Associations between maternal depressive symptoms and child feeding practices in a cross-sectional study of low-income mothers and their young children. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 75. [Google Scholar] [CrossRef] [PubMed]
- Levy, L.B.; O’Hara, M.W. Psychotherapeutic interventions for depressed, low-income women: A review of the literature. Clin. Psychol. Rev. 2010, 30, 934–950. [Google Scholar] [CrossRef]
- Miranda, J.; Green, B.L. The need for mental health services research focusing on poor young women. J. Ment. Health Policy Econ. 1999, 2, 73–80. [Google Scholar] [CrossRef]
- Patel, V.; Rodrigues, M.; DeSouza, N. Gender, Poverty, and Postnatal Depression: A Study of Mothers in Goa, India. Am. J. Psychiatry 2002, 159, 43–47. [Google Scholar] [CrossRef]
- Goldman, L.S.; Nielsen, N.H.; Champion, H.C. Awareness, diagnosis, and treatment of depression. J. Gen. Intern. Med. 1999, 14, 569–580. [Google Scholar] [CrossRef]
- Ferrari, A.J.; Charlson, F.J.; Norman, R.E.; Patten, S.B.; Freedman, G.D.; Murray, C.J.; Vos, T.; Whiteford, H.A. Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study 2010. PLoS Med. 2013, 10, e1001547. [Google Scholar] [CrossRef]
- Üstün, T.B.; Ayuso-Mateos, J.L.; Chatterji, S.; Mathers, C.; Murray, C.J.L. Global burden of depressive disorders in the year 2000. Br. J. Psychiatry 2004, 184, 386–392. [Google Scholar] [CrossRef]
- Lerman, S. The syndemogenesis of depression: Concepts and examples. Med. Anthr. Theory Open Access J. Anthr. Health Illn. Med. 2018, 5, 56–85. [Google Scholar] [CrossRef]
- Sharma, A. Syndemics: Health in context. Lancet 2017, 389, 881. [Google Scholar]
- Global Gender Gap Report World Economic Forum; World Economic Forum: Geneva, Switzerland, 2015.
- Hyde, J.S.; Mezulis, A.H.; Abramson, L.Y. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008, 115, 291–313. [Google Scholar] [CrossRef] [PubMed]
- Mumford, D.B.; Saeed, K.; Ahmad, I.; Latif, S.; Mubbashar, M.H. Stress and psychiatric disorder in rural Punjab. A community survey. Br. J. Psychiatry J. Ment. Sci. 1997, 170, 473–478. [Google Scholar] [CrossRef]
- Ogbo, F.A.; Mathsyaraja, S.; Koti, R.K.; Perz, J.; Page, A. The burden of depressive disorders in South Asia, 1990–2016: Findings from the global burden of disease study. BMC Psychiatry 2018, 18, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Buckshee, K. Impact of roles of women on health in India. Int. J. Gynecol. Obs. 1997, 58, 35–42. [Google Scholar] [CrossRef]
- Jambunathan, J. Sociocultural factors in depression in Asian Indian women. Health Care Women Int. 1992, 13, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Rani, M.; Bonu, S. Rural Indian women’s care-seeking behavior and choice of provider for gynecological symptoms 1334. Stud. Fam. Plan. 2003, 34, 173–185. [Google Scholar] [CrossRef]
- Rodrigues, M.; Patel, V.; Jaswal, S.; De Souza, N. Listening to mothers: Qualitative studies on motherhood and depression from Goa, India. Soc. Sci. Med. 2003, 57, 1797–1806. [Google Scholar] [CrossRef]
- Ulrich, H. A study of change and depression among Hanik Brahmin women in a South Indian village. Cult. Med. Psychiatry 1987, 11, 261–287. [Google Scholar] [CrossRef]
- Karasz, A. Marriage, Depression and Illness: Sociosomatic Models in a South Asian Immigrant Community. Psychol. Dev. Soc. 2005, 17, 161–180. [Google Scholar] [CrossRef]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.-Y.; Bruyere, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health 2019, 15. [Google Scholar] [CrossRef] [PubMed]
- Harpham, T.; Huttly, S.; De Silva, M.J.; Abramsky, T. Maternal mental health and child nutritional status in four developing countries. J. Epidemiol. Community Health 2005, 59, 1060–1064. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Prince, M. Global mental health: A new global health field comes of age. JAMA 2010, 303, 1976–1977. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Collins, P.Y.; Copeland, J.R.M.; Kakuma, R.; Katontoka, S.; Lamichhane, J.; Naik, S.; Skeen, S. The Movement for Global Mental Health. Br. J. Psychiatry 2011, 198, 88–90. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P.; Karyotaki, E.; Reijnders, M.; Purgato, M.; Barbui, C. Psychotherapies for depression in low- and middle-income countries: A meta-analysis. World Psychiatry 2018, 17, 90–101. [Google Scholar] [CrossRef]
- Patel, V.; Weiss, H.A.; Chowdhary, N.; Naik, S.; Pednekar, S.; Chatterjee, S. The effectiveness of a lay health worker led intervention for depressive and anxiety disorders in primary care: The MANAS cluster randomized trial in Goa, India. Lancet 2010, 376, 2086. [Google Scholar] [CrossRef]
- Shidhaye, R.; Baron, E.; Murhar, V.; Rathod, S.; Khan, A.; Singh, A.; Shrivastava, S.; Muke, S.; Shrivastava, R.; Lund, C.; et al. Community, facility and individual level impact of integrating mental health screening and treatment into the primary healthcare system in Sehore district, Madhya Pradesh, India. BMJ Glob. Health 2019, 4, e001344. [Google Scholar] [CrossRef]
- Clark, J. Medicalization of global health 1: Has the global health agenda become too medicalized? Glob. Health Action 2014, 7, 23998. [Google Scholar] [CrossRef]
- Summerfield, D. How scientifically valid is the knowledge base of global mental health? BMJ 2008, 336, 992–994. [Google Scholar] [CrossRef]
- Rahman, A.; Malik, A.; Sikander, S.; Roberts, C.; Creed, F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: A cluster-randomised controlled trial. Lancet 2008, 372, 902–909. [Google Scholar] [CrossRef]
- Brown, G.W.; Harris, T.O.; Kendrick, T.; Chatwin, J.; Craig, T.K.J.; Kelly, V.; Mander, H.; Ring, A.; Wallace, V.; Uher, R. Antidepressants, social adversity and outcome of depression in general practice. J. Affect. Disord. 2010, 121, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Warden, D.; Rush, A.J.; Wisniewski, S.R.; Lesser, I.M.; Thase, M.E.; Balasubramani, G.K. Income and attrition in the treatment of depression: A STAR*D report. Depress Anxiety 2009, 26, 622–633. [Google Scholar] [CrossRef] [PubMed]
- Jakubovski, E.; Bloch, M.H. Prognostic Subgroups for Citalopram Response in the STAR*D Trial. J. Clin. Psychiatry 2014, 75, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Falconnier, L. Socioeconomic status in the treatment of depression. Am. J. Orthopsychiatry 2009, 79, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Jain, F.A.; Hunter, A.M.; Brooks, J.O., 3rd; Leuchter, A.F. Predictive socioeconomic and clinical profiles of antidepressant response and remission. Depress Anxiety 2013, 30, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Westen, D.; Novotny, C.M.; Thompson-Brenner, H. The Empirical Status of Empirically Supported Psychotherapies: Assumptions, Findings, and Reporting in Controlled Clinical Trials. Psychol. Bull. 2004, 130, 631–663. [Google Scholar] [CrossRef]
- Rahman, A.; Fisher, J.; Bower, P.; Luchters, S.; Tran, T.; Yasamy, M.T.; Saxena, S.; Waheed, W. Interventions for common perinatal mental disorders in women in low- and middle-income countries: A systematic review and meta-analysis. Bull. World Health Organ. 2013, 91, 593–601I. [Google Scholar] [CrossRef]
- Haushofer, J.; Mudida, R.; Shapiro, J. The Comparative Impact of Cash Transfers and Psychotherapy on Psychological and Economic Well-Being; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Steinert, C.; Hofmann, M.; Kruse, J.; Leichsenring, F. Relapse rates after psychotherapy for depression—Stable long-term effects? A meta-analysis. J. Affect. Disord. 2014, 168, 107–118. [Google Scholar] [CrossRef]
- Karasz, A. The development of valid subtypes for depression in primary care settings: A preliminary study using an explanatory model approach. J. Nerv. Ment. Dis. 2008, 196, 289–296. [Google Scholar] [CrossRef]
- Karasz, A. Cultural differences in conceptual models of depression. Soc. Sci. Med. 2005, 60, 1625–1635. [Google Scholar] [CrossRef]
- Karasz, A.; Dempsey, K. Health Seeking for Ambiguous Symptoms in Two Cultural Groups: A Comparative Study. Transcult. Psychiatry 2008, 45, 415–438. [Google Scholar] [CrossRef] [PubMed]
- Karasz, A.; Garcia, N.; Ferri, L. Conceptual Models of Depression in Primary Care Patients: A Comparative Study. J. Cross Cult. Psychol. 2009, 40, 1041–1059. [Google Scholar] [CrossRef] [PubMed]
- Karasz, A.; Sacajiu, G.; Garcia, N. Conceptual models of psychological distress among low-income patients in an inner-city primary care clinic. J. Gen. Intern. Med. 2003, 18, 475–477. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Karasz, A.; Watkins, L. Conceptual Models of Treatment in Depressed Hispanic Patients. Ann. Fam. Med. 2006, 4, 527–533. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Grote, N.K.; Zuckoff, A.; Swartz, H.A.; Bledsoe, S.E.; Geibel, S. Engaging women who are depressed and economically disadvantaged in mental health treatment. Soc. Work. 2007, 52, 295–308. [Google Scholar] [CrossRef]
- Anderson, C.M.; Robins, C.S.; Greeno, C.G.; Cahalane, H.; Copeland, V.C.; Andrews, R.M. Why Lower Income Mothers Do Not Engage With the Formal Mental Health Care System: Perceived Barriers to Care. Qual. Health Res. 2006, 16, 926–943. [Google Scholar] [CrossRef]
- Schraufnagel, T.J.; Wagner, A.W.; Miranda, J.; Roy-Byrne, P.P. Treating minority patients with depression and anxiety: What does the evidence tell us? Gen. Hosp. Psychiatry 2006, 28, 27–36. [Google Scholar] [CrossRef]
- Boshara, R. Seven Surprising Findings from the Asset-Building Field; Federal Reserve Bank of St. Louis: St. Louis, MO, USA, 2011. [Google Scholar]
- Bynner, J.; Paxton, W. The Asset-Effect: Institute for Public Policy Research; Institute for Public Policy Research: Newcastle, UK, 2001. [Google Scholar]
- Angeles, G.; de Hoop, J.; Handa, S.; Kilburn, K.; Milazzo, A.; Peterman, A. Government of Malawi’s unconditional cash transfer improves youth mental health. Soc. Sci. Med. 2019, 225, 108–119. [Google Scholar] [CrossRef]
- Haushofer, J.; Shapiro, J. The Short-term Impact of Unconditional Cash Transfers to the Poor: Experimental Evidence from Kenya*. Q. J. Econ. 2016, 131, 1973–2042. [Google Scholar] [CrossRef]
- Banerjee, A.; Duflo, E.; Goldberg, N.; Karlan, D.; Osei, R.; Parienté, W. A multifaceted program causes lasting progress for the very poor: Evidence from six countries. Science 2015, 348, 1260799. [Google Scholar] [CrossRef]
- Karasz, A.; Raghavan, S.; Patel, V.; Zaman, M.; Akhter, L.; Kabita, M. ASHA: Using Participatory Methods to Develop an Asset-building Mental Health Intervention for Bangladeshi Immigrant Women. J. Epidemiol. Community Health 2015, 9, 501–512. [Google Scholar]
- Werner, D.; Bower, W. Helping Health Workers Learn: A Book of Methods, Aids and Ideas for Workers at the Village Level; Hesperian: Berkeley, CA, USA, 1982. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, A.K.; Alam, M.N.; Ali, S.M. Dasherkandi project studies. Demography, morbidity and mortality in a rural community of Bangladesh. Bangladesh Med Res. Counc. Bull. 1981, 7, 22–39. [Google Scholar] [PubMed]
- Islam, M.; Ali, M.; Ferroni, P.; Underwood, P.; Alam, F. Prevalence of psychiatric disorders in an urban community in Bangladesh. Gen. Hosp. Psychiatry 2003, 25, 353–357. [Google Scholar] [CrossRef]
- Roy, T.; Lloyd, C.E.; Parvin, M.; Mohiuddin, K.G.B.; Rahman, M. Prevalence of co-morbid depression in out-patients with type 2 diabetes mellitus in Bangladesh. BMC Psychiatry 2012, 12, 123. [Google Scholar] [CrossRef]
- Karasz, A.; Patel, V.V.; Kabita, M.; Shimu, P. “Tension” in South Asian women: Developing a measure of common mental disorder using participatory methods. Prog. Community Health Partnersh. Res. Educ. Action 2013, 7, 429–441. [Google Scholar] [CrossRef]
- Sherbourne, C.D.; Stewart, A.L. The MOS social support survey. Soc. Sci. Med. 1991, 32, 705–714. [Google Scholar] [CrossRef]
- Mason, K.; Smith, H. Women’s Empowerment and Social Context: Resutls from Five Asian Countries; World Bank: Washington, DC, USA, 2003. [Google Scholar]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The Hopelessness Scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton University Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Baum, F.; Fisher, M. Why behavioural health promotion endures despite its failure to reduce health inequities. Sociol Health Illn 2014, 36, 213–225. [Google Scholar] [CrossRef]
- Holman, D.; Lynch, R.; Reeves, A. How do health behaviour interventions take account of social context? A literature trend and co-citation analysis. Health 2018, 22, 389–410. [Google Scholar] [CrossRef]
- Golden, S.D.; Earp, J.A. Social ecological approaches to individuals and their contexts: Twenty years of health education & behavior health promotion interventions. Health education & behavior: The official publication of the Society for Public Health Education. Health Educ. Behav. 2012, 39, 364–372. [Google Scholar] [PubMed]
- Blattman, C.; Jamison, J.; Sheridan, M. Reducing crime and violence: Experimental evidence from cognitive behavioral therapy in Liberia. Am. Econ. Rev. 2015, 107, 1165–1206. [Google Scholar] [CrossRef] [PubMed]
| Variable | Intervention n = 24 Mean (SD)/% | Control n = 24 Mean (SD)/% | p Value |
|---|---|---|---|
| Age in years | 26.0 (4.9) | 26.1 (4.4) | 0.98 |
| Education (years in school) | 6.0 (2.3) | 4.4 (2.3) | 0.03 |
| Family size (number of people in household) | 4.63 (1.5) | 5.2 (1.91) | 0.25 |
| Family members (3 or more members) | 45.9 | 54.1 | 0.16 |
| Number of children (less than 2 children) | 57.1 | 42.9 | 0.16 |
| Monthly family income ($) | 76.9 (17.7) | 76.8 (22.2) | 0.99 |
| Loan/debt (US $) | 35.2 (54.7) | 40.0 (62.7) | 0.78 |
| Variable (Range) | Intervention (n = 24) | Control (n = 24) | p Value (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Baseline (T0) Mean (SD) | 12 mo. Follow Up (T1) Mean (SD) | Mean Difference of Scores (T1–T0) | Baseline (T0) Mean (SD) | 12-mo Follow Up (T1) Mean (SD) | Mean Difference of Scores (T1–T0) | ||
| PHQ-9 (0–27) | 14.5 (2.5) | 5.5 (2.8) | −9.0 | 14.5 (3.6) | 14.9 (2.8) | 0.5 | <0.001 (7.4, 11.6) |
| Tension Scale (25–100) | 55.0 (6.7) | 32.9 (4.9) | −22.1 | 55.4 (6.8) | 50.0 (7.2) | −5.3 | <0.001 (11.9, 21.7) |
| Rosenberg Self Esteem (0–32) | 18.5 (5.2) | 21.7 (4.4) | 3.2 | 18.6 (5.8) | 18.5 (3.9) | 0.1 | 0.040 (−6.0, −0.2) |
| Trait Hope Scale (12–48) | 36.5 (5.5) | 39.6 (3.2) | 3.1 | 36.4 (5.8) | 36.6 (4.3) | −1.8 | 0.005 (−8.2, −1.6) |
| MOS Social Support (19–95) | 68.6 (18.7) | 92.1 (7.2) | 23.5 | 63.4 (21.0) | 74.7 (17.1) | 11.3 | 0.024 (−22.6, −1.7) |
| Tangible Support | 16.3 (4.4) | 19.7 (1.1) | 3.4 | 15.8 (5.2) | 17.3 (4.8) | 1.5 | 0.153 (−4.6, 0.7) |
| Affectionate Support | 8.8 (3.8) | 14.1 (1.9) | 5.4 | 9.2(3.9) | 10.7 (3.9) | 1.5 | 0.001 (−6.2, −1.6) |
| Positive Social Interaction | 10.1 (4.4) | 14.2 (1.8) | 4.1 | 11.0 (4.0) | 12.0 (2.7) | 1.0 | 0.015 (−5.6, −0.6) |
| Emotional Support | 30.5 (9.8) | 39.3 (3.3) | 8.8 | 24.3 (11.9) | 30.9 (10.3) | 6.6 | 0.443 (−8.0, 3.5) |
| Additional Support | 3.0 (1.4) | 4.8 (0.6) | 1.8 | 3.0 (1.4) | 3.8 (1.0) | 0.8 | 0.030 (−1.8,−0.1) |
| Economic Decision Making (0–6) | 3.5 (2.1) | 5.0 (1.3) | 1.5 | 3.8 (2.2) | 3.6 (1.9) | −0.1 | 0.011 (−2.8, −0.4) |
| Family Size Decision Making (0–2) | 1.5 (0.8) | 1.8 (0.4) | 0.3 | 1.6 (0.7) | 1.6 (0.7) | 0.0 | 0.252 (−0.8, 0.2) |
| Freedom of Movement (0–5) | 3.7 (2.2) | 3.1 (2.5) | −0.5 | 3.1 (2.5) | 2.5 (2.6) | −6.3 | 0.916 (−1.7, 1.5) |
| Coercive Control (0–2) | 1.4 (0.6) | 0.9 (0.9) | −0.5 | 1.3 (0.8) | 1.4 (0.7) | 0.1 | 0.011 (0.2, 1.2) |
| Gender Role Norms (0–5) | 2.2 (0.4) | 2.4 (0.8) | 0.3 | 2.2 (0.5) | 2.2 (0.7) | 0.04 | 0.355 (−0.7, 0.2) |
| Outcome Measure | Regression Coefficient (Unstandardized) B ± SE (95% CI) | Standardized Coefficients Beta (β) | p Value | Effect Size |
|---|---|---|---|---|
| PHQ-9 score | −9.2 ± 0.8 (−10.9, −7.5) | −0.8 | <0.001 | −2.5 |
| Rosenberg Self Esteem | 3.5 ± 1.4 (0.7, 6.4) | 0.3 | 0.017 | 0.60 |
| Trait Hope | 4.0 ± 1.1(1.8, 6.2) | 0.5 | 0.001 | 0.68 |
| Tension Scale | −15.1 ± 1.8 (−18.8, −11.4) | −0.7 | <0.001 | −2.2 |
| MOS Social Support | 16.7 ± 3.6 (9.4, 24.0) | 0.5 | <0.001 | 0.79 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karasz, A.; Anne, S.; Hamadani, J.D.; Tofail, F. The ASHA (Hope) Project: Testing an Integrated Depression Treatment and Economic Strengthening Intervention in Rural Bangladesh: A Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 279. https://doi.org/10.3390/ijerph18010279
Karasz A, Anne S, Hamadani JD, Tofail F. The ASHA (Hope) Project: Testing an Integrated Depression Treatment and Economic Strengthening Intervention in Rural Bangladesh: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(1):279. https://doi.org/10.3390/ijerph18010279
Chicago/Turabian StyleKarasz, Alison, Shabnam Anne, Jena Derakhshani Hamadani, and Fahmida Tofail. 2021. "The ASHA (Hope) Project: Testing an Integrated Depression Treatment and Economic Strengthening Intervention in Rural Bangladesh: A Pilot Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 1: 279. https://doi.org/10.3390/ijerph18010279
APA StyleKarasz, A., Anne, S., Hamadani, J. D., & Tofail, F. (2021). The ASHA (Hope) Project: Testing an Integrated Depression Treatment and Economic Strengthening Intervention in Rural Bangladesh: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(1), 279. https://doi.org/10.3390/ijerph18010279






