Association between Cardiac Autonomic Control and Postural Control in Patients with Parkinson’s Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Health-Related Quality of Llife
2.3. RR Interval Recording
2.4. Heart Rate Variability (HRV) Analysis
2.5. Stabilometric Assessment
2.6. Stabilogram Analysis
2.7. Statistical Analysis
3. Results
3.1. Sample Characterization
3.2. Stabilometric Parameters
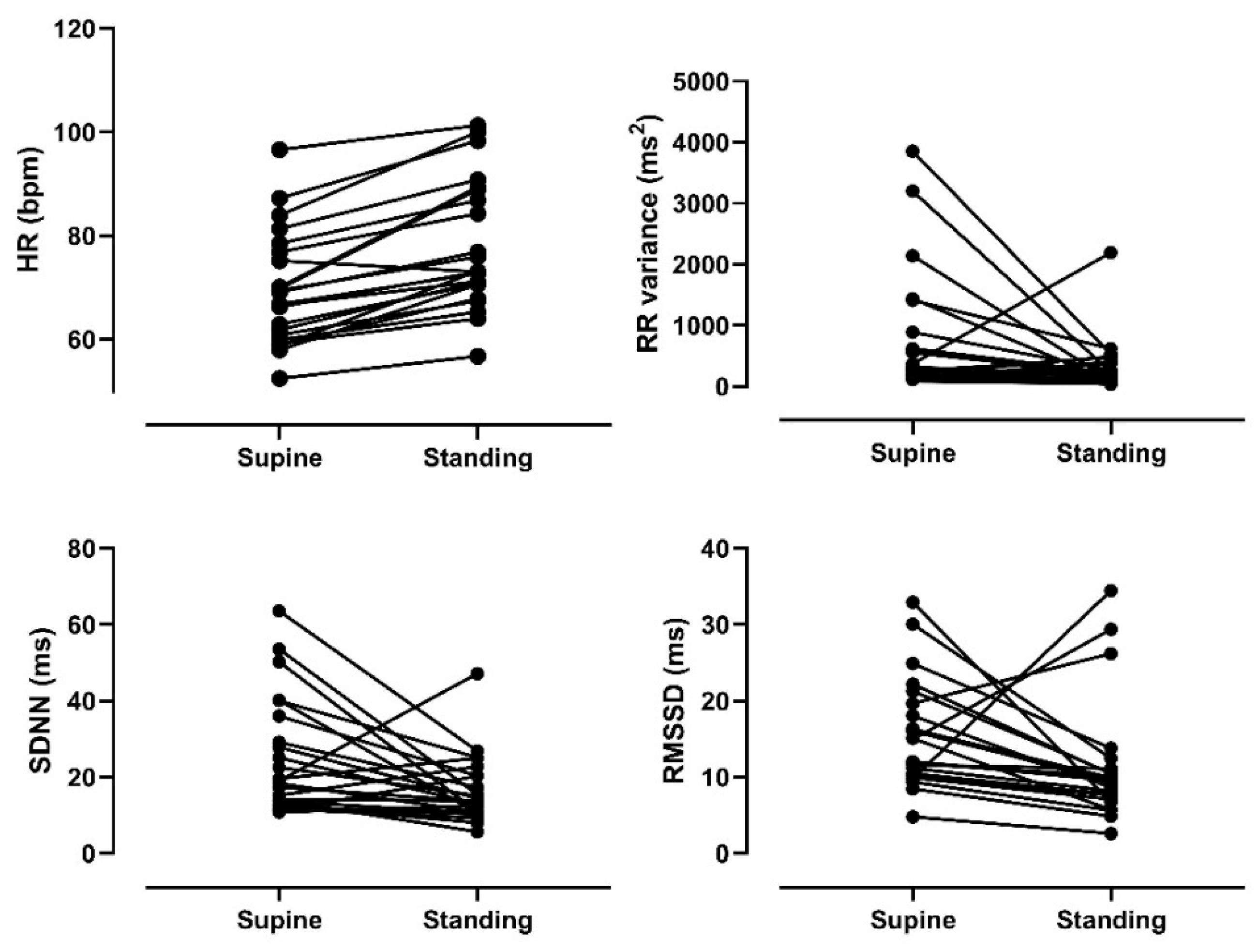
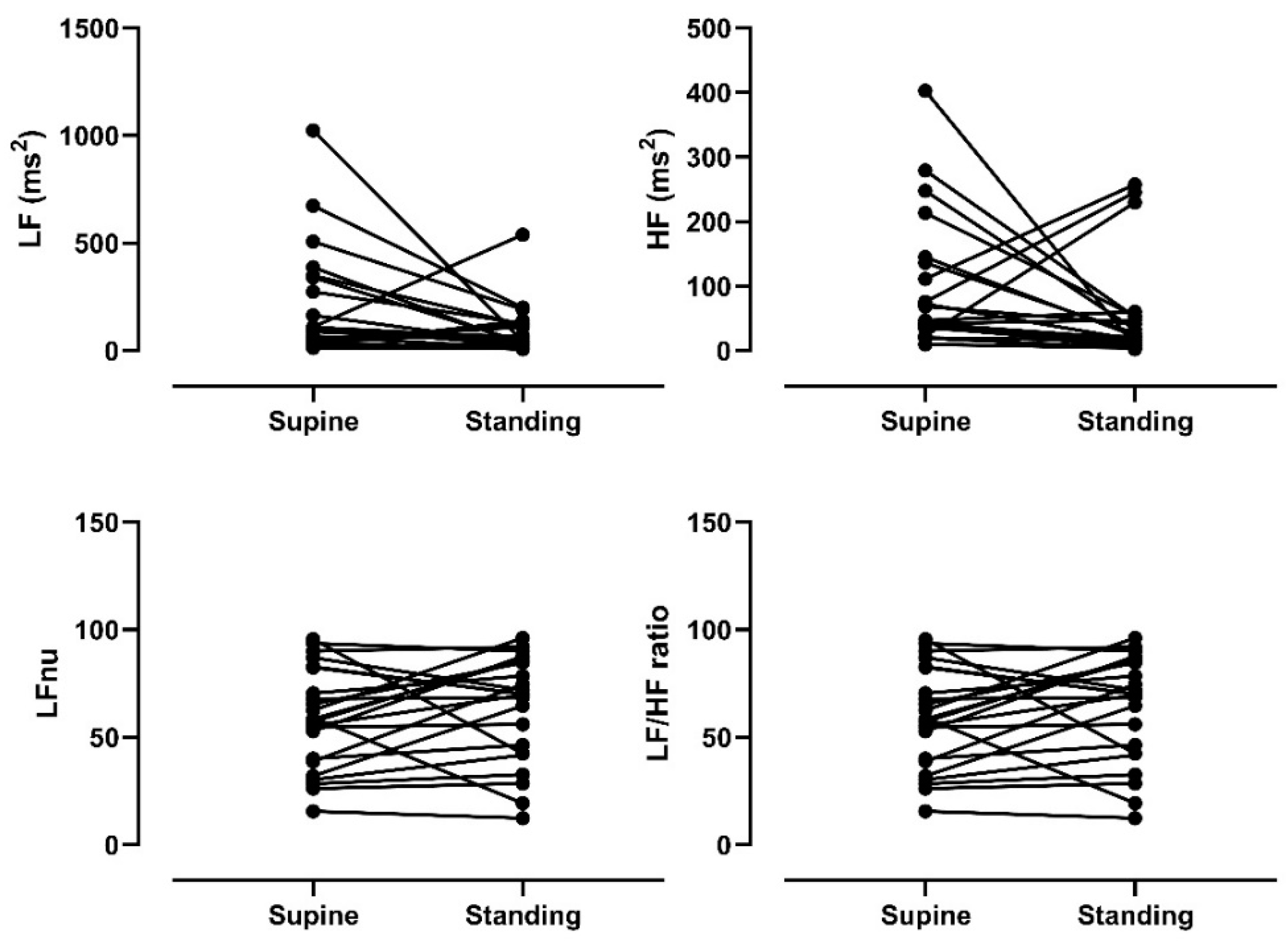
3.3. Heart Rate Variability in Response to a Gravitational Stimulus
3.4. Relationship between Heart Rate Variability in the Supine Position and Center of Pressure Stabilometric Variables
3.5. Relationship between Postural Variation in Heart Rate Variability and Center of Pressure Stabilometric Variables
4. Discussion
4.1. Cardiac Autonomic Modulation to Orthostatic Stress
4.2. The Relationship between Sympathovagal Balance in the Supine Position and Postural Control
4.3. Relationship between Cardiac Autonomic Modulation and Postural Control in Response to Postural Change
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barbosa, M.T.; Carthery, M.T.; Maia, D.P.; Cunningham, M.C.Q.; Guerra, H.L.; Cardoso, F.; Lima-Costa, M.F. Parkinsonism and Parkinson’s disease in the elderly: A community-based survey in Brazil (the Bambuí study). Mov. Disord. 2006, 21, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Beitz, J.M. Parkinson s disease: A review. Front. Biosci. 2014, S6, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Zesiewicz, T.A.; Baker, M.J.; Wahba, M.; Hauser, R.A. Autonomic nervous system dysfunction in Parkinson’s disease. Curr. Treat. Options Neurol. 2003, 5, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Asahina, M.; Vichayanrat, E.; A Low, D.; Iodice, V.; Mathias, C.J. Autonomic dysfunction in parkinsonian disorders: Assessment and pathophysiology. J. Neurol. Neurosurg. Psychiatry 2012, 84, 674–680. [Google Scholar] [CrossRef]
- Jain, S.; Goldstein, D.S. Cardiovascular dysautonomia in Parkinson disease: From pathophysiology to pathogenesis. Neurobiol. Dis. 2012, 46, 572–580. [Google Scholar] [CrossRef]
- Szili-Torok, T.; Kalman, J.; Paprika, D.; Dibo, G.; Rozsa, Z.; Rudas, L. Depressed baroreflex sensitivity in patients with Alz-heimer’s and Parkinson’s disease. Neurobiol. Aging 2001, 22, 435–438. [Google Scholar] [CrossRef]
- Ziemssen, T.; Reichmann, H. Review: Treatment of dysautonomia in extrapyramidal disorders. Ther. Adv. Neurol. Disord. 2009, 3, 53–67. [Google Scholar] [CrossRef]
- Massano, J.; Bhatia, K.P. Clinical Approach to Parkinson’s Disease: Features, Diagnosis, and Principles of Management. Cold Spring Harb. Perspect. Med. 2012, 2, a008870. [Google Scholar] [CrossRef]
- Micieli, G.; Tosi, P.; Marcheselli, S.; Cavallini, A. Autonomic dysfunction in Parkinson’s disease. Neurol. Sci. 2003, 24, s32–s34. [Google Scholar] [CrossRef]
- Gómez, R.; Hudson, L.; Venegas, P. [Autonomic disturbances in Parkinson disease]. Rev. Medica Chile 2011, 139, 100–106. [Google Scholar] [CrossRef]
- Goldstein, D.S. Orthostatic hypotension as an early finding in Parkinson’s disease. Clin. Auton. Res. 2006, 16, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, D.S. Dysautonomia in Parkinson Disease. Compr. Physiol. 2014, 4, 805–826. [Google Scholar] [CrossRef] [PubMed]
- Jasinska-Myga, B.; Heckman, M.G.; Wider, C.; Putzke, J.D.; Wszolek, Z.K.; Uitti, R.J. Loss of ability to work and ability to live independently in Parkinson’s disease. Park. Relat. Disord. 2011, 18, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Jost, W.H. An update on the recognition and treatment of autonomic symptoms in Parkinson’s disease. Expert Rev. Neurother. 2017, 17, 791–799. [Google Scholar] [CrossRef]
- Matinolli, M.; Korpelainen, J.T.; Korpelainen, R.; Sotaniemi, K.A.; Myllylä, V.V. Orthostatic hypotension, balance and falls in Parkinson’s disease. Mov. Disord. 2009, 24, 745–751. [Google Scholar] [CrossRef]
- Kanegusuku, H.; Silva-Batista, C.; Peçanha, T.; Nieuwboer, A.; Silva, N.D.; Costa, L.A.; De Mello, M.T.; Piemonte, M.E.P.; Ugrinowitsch, C.; Forjaz, C.L.D.M. Effects of Progressive Resistance Training on Cardiovascular Autonomic Regulation in Patients with Parkinson Disease: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2017, 98, 2134–2141. [Google Scholar] [CrossRef]
- Vanderlei, L.C.; Pastre, C.M.; Hoshi, R.A.; Carvalho, T.D.; Godoy, M.F. Basic notions of heart rate variability and its clinical applicability. Rev. Bras. Cir. Cardiovasc. 2009, 24, 205–217. [Google Scholar] [CrossRef]
- Hillebrand, S.; Gast, K.B.; De Mutsert, R.; Swenne, C.A.; Jukema, J.W.; Middeldorp, S.; Rosendaal, F.R.; Dekkers, O.M. Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: Meta-analysis and dose–response meta-regression. Europace 2013, 15, 742–749. [Google Scholar] [CrossRef]
- Wulsin, L.R.; Horn, P.S.; Perry, J.L.; Massaro, J.; D’Agostino, R.B. Autonomic Imbalance as a Predictor of Metabolic Risks, Cardiovascular Disease, Diabetes, and Mortality. J. Clin. Endocrinol. Metab. 2015, 100, 2443–2448. [Google Scholar] [CrossRef]
- Hohler, A.D.; Zuzuárregui, J.R.P.; Katz, D.I.; DePiero, T.J.; Hehl, C.L.; Leonard, A.; Allen, V.; Dentino, J.; Gardner, M.; Phenix, H.; et al. Differences in Motor and Cognitive Function in Patients with Parkinson’s Disease with and Without Orthostatic Hypotension. Int. J. Neurosci. 2011, 122, 233–236. [Google Scholar] [CrossRef]
- Sibley, K.M.; Mochizuki, G.; Lakhani, B.; McIlroy, W.E. Autonomic contributions in postural control: A review of the evidence. Rev. Neurosci. 2014, 25, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Kotagal, V.; Albin, R.L.; Müller, M.L.; Koeppe, R.A.; Frey, K.A.; Bohnen, N.I. Modifiable cardiovascular risk factors and axial motor impairments in Parkinson disease. Neurology 2014, 82, 1514–1520. [Google Scholar] [CrossRef] [PubMed]
- Gelb, D.J.; Oliver, E.; Gilman, S. Diagnostic Criteria for Parkinson Disease. Arch. Neurol. 1999, 56, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Nutt, J.G.; Wooten, G.F. Diagnosis and Initial Management of Parkinson’s Disease. New Engl. J. Med. 2005, 353, 1021–1027. [Google Scholar] [CrossRef] [PubMed]
- González-Hernández, J.; Aguilar, L.; Oporto, S.; Araneda, L.; Vásquez, M.; Von Bernhardi, R. Normalización del “Mini-Mental State Examination” según edad y educación, para la población de Santiage de Chile. Rev. Memoriza.com 2009, 3, 23–24. [Google Scholar]
- Gutiérrez-Espínola, C.; Torres-Ramírez, L.; Flores-Mendoza, M. Calidad de vida en pacientes con enfermedad de Parkinson que acuden a la consulta externa del Instituto Nacional de Ciencias Neurológicas. Revista Peruana Neurol. 2010, 12, 5–12. [Google Scholar]
- Task Force of the European Society of Cardiology; The North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Billman, G.E. Heart Rate Variability? A Historical Perspective. Front. Physiol. 2011, 2, 86. [Google Scholar] [CrossRef]
- Eckberg, D.L. Sympathovagal Balance. Circulation 1997, 96, 3224–3232. [Google Scholar] [CrossRef]
- Milicević, G. Low to high frequency ratio of heart rate variability spectra fails to describe sympatho-vagal balance in cardiac patients. Coll. Antropol. 2005, 29, 295–300. [Google Scholar]
- Duarte, M.; Freitas, S.M.S.F. Revisão sobre posturografia baseada em plataforma de força para avaliação do equilíbrio. Braz. J. Phys. Therapy 2010, 14, 183–192. [Google Scholar] [CrossRef]
- Gagey, P.M.; Weber, B. Posturologia: Regulacion y Alteraciones de la Bipedestacion; Elsevier: Barcelona, Spain, 2001. [Google Scholar]
- Prieto, T.; Myklebust, J.; Hoffmann, R.; Lovett, E.; Myklebust, B. Measures of postural steadiness: Differences between healthy young and elderly adults. IEEE Trans. Biomed. Eng. 1996, 43, 956–966. [Google Scholar] [CrossRef] [PubMed]
- Paillard, T.; Noé, F. Techniques and Methods for Testing the Postural Function in Healthy and Pathological Subjects. BioMed Res. Int. 2015, 2015, 1–15. [Google Scholar] [CrossRef]
- Mancini, M.; Salarian, A.; Carlson-Kuhta, P.; Zampieri, C.; King, L.; Chiari, L.; Horak, F.B. ISway: A sensitive, valid and reliable measure of postural control. J. Neuroeng. Rehabil. 2012, 9, 59. [Google Scholar] [CrossRef] [PubMed]
- Ruhe, A.; Fejer, R.; Walker, B. The test–retest reliability of centre of pressure measures in bipedal static task conditions—A systematic review of the literature. Gait Posture 2010, 32, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Barbic, F.; Perego, F.; Canesi, M.; Gianni, M.; Biagiotti, S.; Costantino, G.; Pezzoli, G.; Porta, A.; Malliani, A.; Furlan, R. Early Abnormalities of Vascular and Cardiac Autonomic Control in Parkinson’s Disease Without Orthostatic Hypotension. Hypertension 2007, 49, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Alvarado-Jalomo, S.; Alvarado-Álvarez, N.A.; Dorantes-Méndez, G. Evaluación de la Presencia de Disautonomía en Pacientes con Parkinson mediante el Análisis de Señales Cardiovasculares. Rev. Mex. Ing. Biomédica 2017, 38, 141–154. [Google Scholar]
- Furushima, H.; Shimohata, T.; Nakayama, H.; Ozawa, T.; Chinushi, M.; Aizawa, Y.; Nishizawa, M. Significance and usefulness of heart rate variability in patients with multiple system atrophy. Mov. Disord. 2012, 27, 570–574. [Google Scholar] [CrossRef]
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35, ii7–ii11. [Google Scholar] [CrossRef]
- Maurer, C.; Mergner, T.; Xie, J.; Faist, M.; Pollak, P.; Lucking, C.H. Effect of chronic bilateral subthalamic nucleus (STN) stimulation on postural control in Parkinson’s disease. Brain 2003, 126, 1146–1163. [Google Scholar] [CrossRef] [PubMed]
- Rahmati, Z.; Schouten, A.C.; Behzadipour, S.; Taghizadeh, G.; Firoozbakhsh, K. Disentangling stability and flexibility degrees in Parkinson’s disease using a computational postural control model. J. Neuroeng. Rehabil. 2019, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Rocchi, L.; Chiari, L.; Horak, F.B. Effects of deep brain stimulation and levodopa on postural sway in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 2002, 73, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Marín, M.D.S.; Carmona, V.H.; Ibarra, Q.M.; Gámez, C.M. Enfermedad de Parkinson: Fisiopatología, diagnóstico y tratamiento. Rev. Univ. Ind. Santander. Salud 2018, 50, 79–92. [Google Scholar]
- Groenewegen, H.J. The Basal Ganglia and Motor Control. Neural Plast. 2003, 10, 107–120. [Google Scholar] [CrossRef]
- Jacobs, J.V.; Horak, F.B. Cortical control of postural responses. J. Neural Transm. 2007, 114, 1339–1348. [Google Scholar] [CrossRef]
- Yin, H.H. The Basal Ganglia in Action. Neuroscience 2016, 23, 299–313. [Google Scholar] [CrossRef]
- Maki, B.E.; Holliday, P.J.; Fernie, G.R. Aging and Postural Control. J. Am. Geriatr. Soc. 1990, 38, 1–9. [Google Scholar] [CrossRef]
- Sletten, D.M.; Suarez, G.A.; Low, P.A.; Mandrekar, J.; Singer, W. COMPASS 31: A Refined and Abbreviated Composite Autonomic Symptom Score. Mayo Clin. Proc. 2012, 87, 1196–1201. [Google Scholar] [CrossRef]
- Garg, A.; Xu, D.; Laurin, A.; Blaber, A.P. Physiological interdependence of the cardiovascular and postural control systems under orthostatic stress. Am. J. Physiol. Circ. Physiol. 2014, 307, H259–H264. [Google Scholar] [CrossRef]
- Rodrigues, G.D.; Gurgel, J.L.; Galdino, I.D.S.; Da Nóbrega, A.C.L.; Soares, P.P.D.S. Respiratory pump contributions in cerebrovascular and postural control responses during orthostatic stress in older women. Respir. Physiol. Neurobiol. 2020, 275, 103384. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.K.; Garg, A.; Xu, D.; Bruner, M.; Fazel-Rezai, R.; Blaber, A.P.; Tavakolian, K. Skeletal Muscle Pump Drives Control of Cardiovascular and Postural Systems. Sci. Rep. 2017, 7, srep45301. [Google Scholar] [CrossRef] [PubMed]
- Valenza, G.; Greco, A.; Gentili, C.; Lanata, A.; Sebastiani, L.; Menicucci, D.; Gemignani, A.; Scilingo, E.P. Combining electroencephalographic activity and instantaneous heart rate for assessing brain–heart dynamics during visual emotional elicitation in healthy subjects. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2016, 374, 20150176. [Google Scholar] [CrossRef] [PubMed]
| Mean ± SD | |
|---|---|
| Age (years) | 68.52 ± 9.26 |
| Men/Women | 15/8 |
| Age of PD onset | 60.83 ± 8.52 |
| Disease duration (years) | 7.70 ± 5.38 |
| Hoehn & Yahr score (1/2/3) | 7/13/3 |
| UDPRS-III | 38 ± 16 |
| LEDD (mg/day) | 383.50 ± 271.01 |
| Weight (Kg) | 67.07 ± 13.62 |
| Height (cm) | 159.04 ± 9.66 |
| BMI (kg/m2) | 26.38 ± 4.38 |
| Mean ± SD | |
|---|---|
| PDQ-39 Mobility | 40.90 ± 28.14 |
| PDQ-39 Activities of daily living | 41.00 ± 22.56 |
| PDQ-39 Emotional Well-being | 44.17 ± 26.81 |
| PDQ-39 Stigma | 33.50 ± 24.33 |
| PDQ-39 Emotional Support | 14.50 ± 23.94 |
| PDQ-39 Cognition | 42.75 ± 21.32 |
| PDQ-39 Communication | 33.67 ± 29.90 |
| PDQ-39 Body movement | 54.00 ± 21.80 |
| PDQ-39 Summary index | 38.06 ± 16.78 |
| Supine | Standing | Delta | Effect Size | Sup vs. Stand p-Value | |
|---|---|---|---|---|---|
| HR (bpm) | 69.14 ± 10.91 | 77.80 ± 12.26 | 8.65 ± 5.01 | 0.74 | <0.001 |
| SDNN (ms) | 25.15 ± 15.18 | 16.48 ± 8.86 | −7.65 ± 16.28 | 0.65 | 0.017 |
| RMSSD (ms) | 15.55 ± 7.03 | 11.38 ± 7.89 | −1.49 ± 9.13 | 0.55 | 0.06 |
| RR variance (ms2) | 750.70 ± 1026.13 | 317.40 ± 442.27 | −433.30 ± 1102.17 | 0.70 | 0.07 |
| LF (ms2) | 200.04 ± 252.45 | 89.47 ± 113.76 | −104.38 ± 264.82 | 0.50 | 0.06 |
| LF un | 58.59 ± 23.31 | 63.96 ± 24.51 | 6.51 ± 27.26 | 0.63 | 0.27 |
| HF (ms2) | 95.17 ± 100.69 | 52.97 ± 77.78 | −29.03 ± 126.10 | 0.46 | 0.13 |
| HF un | 41.32 ± 23.28 | 35.90 ± 24.45 | −6.59 ± 24.17 | 0.23 | 0.27 |
| LF/HF | 3.53 ± 5.28 | 4.18 ± 5.46 | 0.72 ± 7.27 | 0.12 | 0.67 |
| RMS-AP (mm) | RMS-ML (mm) | MV-AP (mm/s) | MV-ML (mm/s) | Ellipse Area (mm2) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | |
| HR (bpm) | 0.15 | 0.50 | 0.03 | 0.91 | 0.25 | 0.26 | 0.04 | 0.86 | 0.15 | 0.49 |
| RR (ms) | −0.17 | 0.44 | −0.03 | 0.89 | −0.28 | 0.20 | −0.07 | 0.77 | −0.17 | 0.45 |
| SDNN (ms) | −0.16 | 0.47 | −0.21 | 0.33 | 0.06 | 0.77 | −0.045 | 0.84 | −0.25 | 0.24 |
| RMSSD (ms) | 0.28 | 0.20 | −0.22 | 0.31 | −0.15 | 0.51 | −0.09 | 0.70 | 0.02 | 0.92 |
| RR variability (ms2) | −0.20 | 0.36 | −0.17 | 0.45 | 0.18 | 0.41 | −0.02 | 0.91 | −0.26 | 0.23 |
| LF (ms2) | 0.03 | 0.90 | −0.15 | 0.51 | 0.31 | 0.15 | −0.11 | 0.62 | −0.09 | 0.69 |
| LF nu | −0.28 | 0.20 | −0.06 | 0.80 | 0.19 | 0.39 | 0.04 | 0.86 | −0.21 | 0.35 |
| HF (ms2) | 0.42 | 0.045 | −0.13 | 0.54 | −0.19 | 0.38 | −0.21 | 0.34 | 0.20 | 0.36 |
| HF nu | 0.28 | 0.20 | 0.06 | 0.80 | −0.19 | 0.39 | −0.04 | 0.86 | 0.21 | 0.34 |
| LF/HF | −0.30 | 0.16 | −0.12 | 0.57 | 0.48 | 0.02 | 0.06 | 0.77 | −0.32 | 0.13 |
| RMS-AP (mm) | RMS-ML (mm) | MV-AP (mm/s) | MV-ML (mm/s) | Ellipse Area (mm2) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | P | r | p | r | p | r | p | |
| Δ HR (bpm) | 0.13 | 0.54 | −0.15 | 0.49 | 0.40 | 0.06 | −0.14 | 0.53 | 0.04 | 0.85 |
| Δ RR (ms) | −0.08 | 0.72 | 0.17 | 0.44 | −0.18 | 0.41 | 0.14 | 0.52 | 0.04 | 0.87 |
| Δ SDNN (ms) | 0.14 | 0.51 | 0.33 | 0.12 | −0.21 | 0.34 | 0.00 | 0.99 | 0.29 | 0.18 |
| Δ RMSSD (ms) | 0.13 | 0.55 | 0.19 | 0.38 | −0.09 | 0.70 | −0.09 | 0.69 | 0.14 | 0.52 |
| Δ RR variability (ms2) | 0.15 | 0.50 | 0.22 | 0.31 | −0.24 | 0.28 | 0.00 | 0.10 | 0.24 | 0.27 |
| Δ LF | −0.06 | 0.79 | 0.25 | 0.26 | −0.40 | 0.06 | 0.05 | 0.81 | 0.12 | 0.60 |
| Δ LF nu | 0.28 | 0.20 | 0.27 | 0.21 | −0.42 | 0.04 | −0.18 | 0.40 | 0.49 | 0.02 |
| Δ HF | −0.32 | 0.14 | 0.09 | 0.70 | 0.20 | 0.36 | 0.24 | 0.28 | −0.26 | 0.23 |
| Δ HFnu | −0.35 | 0.10 | −0.31 | 0.15 | 0.42 | 0.045 | 0.16 | 0.46 | −0.57 | 0.00 |
| Δ LF/HF | 0.45 | 0.03 | 0.14 | 0.53 | −0.53 | 0.01 | −0.23 | 0.29 | 0.51 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Espinoza-Valdés, Y.; Córdova-Arellano, R.; Espinoza-Espinoza, M.; Méndez-Alfaro, D.; Bustamante-Aguirre, J.P.; Maureira-Pareja, H.A.; Zamunér, A.R. Association between Cardiac Autonomic Control and Postural Control in Patients with Parkinson’s Disease. Int. J. Environ. Res. Public Health 2021, 18, 249. https://doi.org/10.3390/ijerph18010249
Espinoza-Valdés Y, Córdova-Arellano R, Espinoza-Espinoza M, Méndez-Alfaro D, Bustamante-Aguirre JP, Maureira-Pareja HA, Zamunér AR. Association between Cardiac Autonomic Control and Postural Control in Patients with Parkinson’s Disease. International Journal of Environmental Research and Public Health. 2021; 18(1):249. https://doi.org/10.3390/ijerph18010249
Chicago/Turabian StyleEspinoza-Valdés, Yoan, Rocio Córdova-Arellano, Maiter Espinoza-Espinoza, Diego Méndez-Alfaro, Juan Pablo Bustamante-Aguirre, Hernán Antonio Maureira-Pareja, and Antonio Roberto Zamunér. 2021. "Association between Cardiac Autonomic Control and Postural Control in Patients with Parkinson’s Disease" International Journal of Environmental Research and Public Health 18, no. 1: 249. https://doi.org/10.3390/ijerph18010249
APA StyleEspinoza-Valdés, Y., Córdova-Arellano, R., Espinoza-Espinoza, M., Méndez-Alfaro, D., Bustamante-Aguirre, J. P., Maureira-Pareja, H. A., & Zamunér, A. R. (2021). Association between Cardiac Autonomic Control and Postural Control in Patients with Parkinson’s Disease. International Journal of Environmental Research and Public Health, 18(1), 249. https://doi.org/10.3390/ijerph18010249






