Dental Fear and Anxiety of Kindergarten Children in Hong Kong: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size
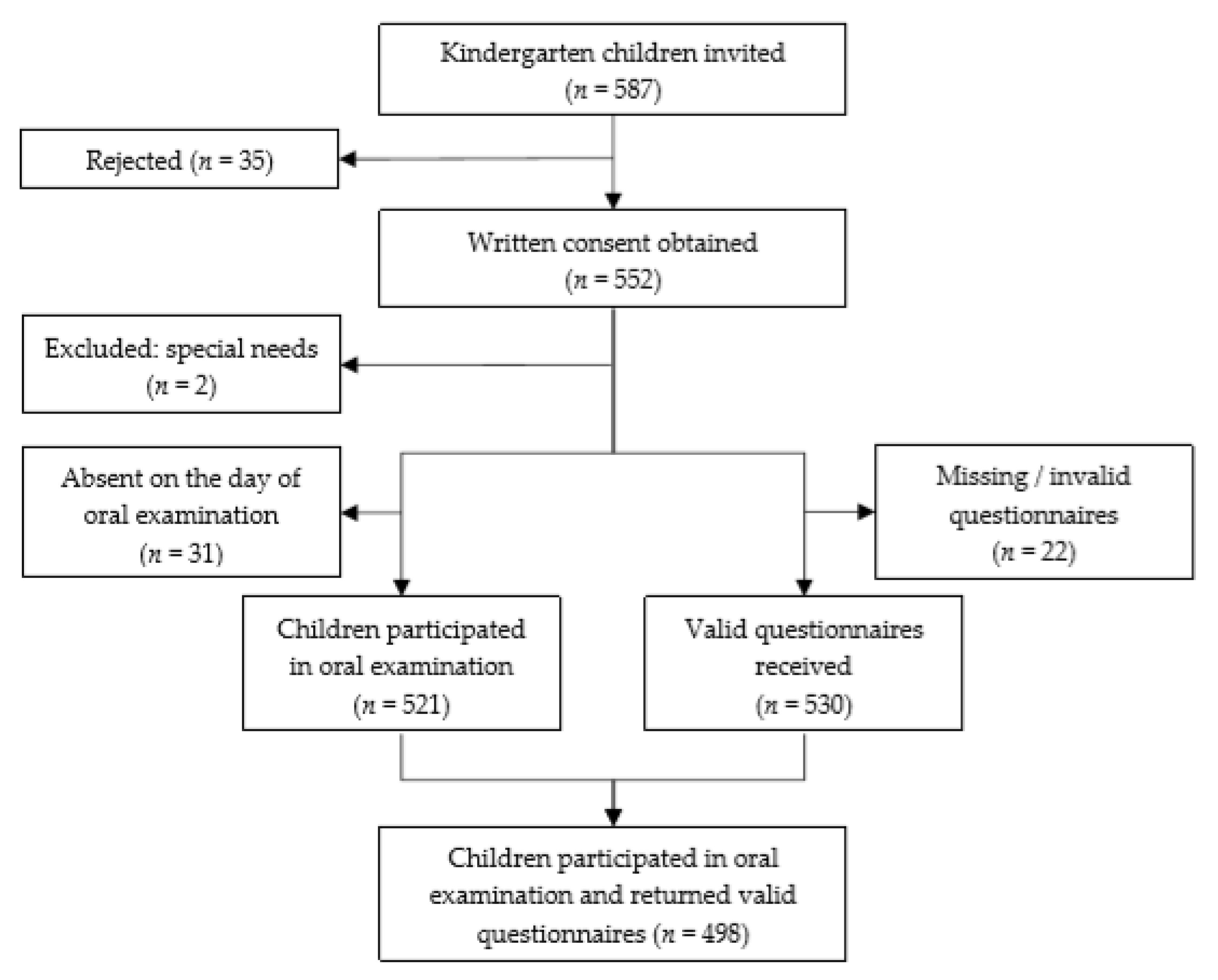
2.2. Setting & Sample
2.3. Fear Assessment and Clinical Exam
2.4. Questionnaire Survey
2.5. Data Entry and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Raadal, M.; Strand, G.V.; Amarante, E.C.; Kvale, G. Relationship between caries prevalence at 5 years of age and dental anxiety at 10. Eur. J. Paediatr. Dent. 2002, 3, 22–26. [Google Scholar] [PubMed]
- Skaret, E.; Raadal, M.; Berg, E.; Kvale, G. Dental anxiety and dental avoidance among 12 to 18 year olds in Norway. Eur. J. Oral. Sci. 1999, 107, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Ten Berge, M.; Veerkamp, J.S.; Hoogstraten, J.; Prins, P.J. Childhood dental fear in the Netherlands: Prevalence and normative data. Community Dent. Oral. Epidemiol. 2002, 30, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Leal, S.C.; Abreu, D.M.d.M.; Frencken, J.E. Dental anxiety and pain related to ART. J. Appl. Oral Sci. Rev. FOB 2009, 17, 84–88. [Google Scholar] [CrossRef]
- Wong, M.L.W.; Lai, S.H.F.; Wong, H.M.; Yang, Y.X.; Yiu, C.K.Y. Dental anxiety in Hong Kong preschool children: Prevalence and associated factors. Adv. Pediatric Res. 2017, 4, 1. [Google Scholar]
- Lee, C.Y.; Chang, Y.Y.; Huang, S.T. Prevalence of dental anxiety among 5- to 8-year-old Taiwanese children. J. Public Health Dent. 2007, 67, 36–41. [Google Scholar] [CrossRef]
- Milsom, K.M.; Tickle, M.; Humphris, G.M.; Blinkhorn, A.S. The relationship between anxiety and dental treatment experience in 5-year-old children. Br. Dent. J. 2003, 194, 503–506, discussion 495. [Google Scholar] [CrossRef]
- Klaassen, M.A.; Veerkamp, J.S.; Hoogstraten, J. Changes in children’s dental fear: A longitudinal study. Eur. Arch. Paediatr. Dent. 2008, 9, 29–35. [Google Scholar] [CrossRef]
- Wogelius, P.; Poulsen, S.; Sorensen, H.T. Prevalence of dental anxiety and behavior management problems among six to eight years old Danish children. Acta Odontol. Scand. 2003, 61, 178–183. [Google Scholar] [CrossRef]
- Yamada, M.K.; Tanabe, Y.; Sano, T.; Noda, T. Cooperation during dental treatment: The children’s fear survey schedule in Japanese children. Int. J. Paediatr. Dent. 2002, 12, 404–409. [Google Scholar] [CrossRef]
- Versloot, J.; Veerkamp, J.S.; Hoogstraten, J. Children’s self-reported pain at the dentist. Pain 2008, 137, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, S.; Bakkal, M.; Bulut, H.; Selek, S. Quantitative evaluation of dental anxiety indicators in the serum and saliva samples of children treated under general anesthesia. Clin. Oral Investig. 2018, 22, 2373–2380. [Google Scholar] [CrossRef] [PubMed]
- Klingberg, G. Reliability and validity of the Swedish version of the dental subscale of the children’s fear survey schedule, CFSS-DS. Acta Odontol Scand. 1994, 52, 255–256. [Google Scholar] [CrossRef] [PubMed]
- Okano, A.; Miyamoto, Y.; Asari, J.; Kamijo, R.; Inoue, M. Change in salivary levels of chromogranin A in children by hearing dental air turbine noise. Pediatric Dent. J. 2009, 19, 220–227. [Google Scholar] [CrossRef]
- Uehara, N.; Takagi, Y.; Miwa, Z.; Sugimoto, K. Objective assessment of internal stress in children during dental treatment by analysis of autonomic nervous activity. Int. J. Paediatr. Dent. 2012, 22, 331–341. [Google Scholar] [CrossRef]
- Eden, E.; Çoğulu, D.; Çengelci, B. Assessment of dental anxiety in children: Effect of oral health education. Balkan J. Stomatol. 2008, 12, 51–56. [Google Scholar]
- Wong, J.M.S.; Rao, N. The evolution of early childhood education policy in Hong Kong. Int. J. Child. Care Educ. Policy 2015, 9, 3. [Google Scholar] [CrossRef]
- Audit Commission. Pre-Primary Education Voucher Scheme; Education Bureau, HKSAR: Hong Kong, China, 2013.
- Oral Health Survey 2011; Department of Health, HKSAR: Hong Kong, China, 2011.
- Chen, K.J.; Gao, S.S.; Duangthip, D.; Li, S.K.Y.; Lo, E.C.M.; Chu, C.H. Dental caries status and its associated factors among 5-year-old hong kong children: A cross-sectional study. BMC Oral Health 2017, 17, 121. [Google Scholar] [CrossRef]
- School Dental Care Service. Available online: https://www.schooldental.gov.hk/wsmile/index.htm (accessed on 8 March 2020).
- Yon, M.J.Y.; Gao, S.S.; Chen, K.J.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Medical model in caries management. Dent. J. 2019, 7, 37. [Google Scholar] [CrossRef]
- Community Engagement & Projects. Available online: Facdent.hku.hk/knowledge-exchange/community-engagement-and-projects.html (accessed on 8 March 2020).
- Chu, C.H.; Lo, E.C.; Lin, H.C. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J. Dent. Res. 2002, 81, 767–770. [Google Scholar] [CrossRef]
- Davey, G.C. Dental phobias and anxieties: Evidence for conditioning processes in the acquisition and modulation of a learned fear. Behav. Res. Ther. 1989, 27, 51–58. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Klinberg, G. Dental anxiety and behaviour management problems in paediatric dentistry—A review of background factors and diagnostics. Eur. Arch. Paediatr. Dent. 2008, 9 (Suppl. 1), 11–15. [Google Scholar] [CrossRef] [PubMed]
- Townsend, J.A.; Wells, M.H. 24—Behavior guidance of the pediatric dental patient. In Pediatric Dentistry, 6th ed.; Nowak, A.J., Christensen, J.R., Mabry, T.R., Townsend, J.A., Wells, M.H., Eds.; Content Repository: Philadelphia, PA, USA, 2019; pp. 352–370. [Google Scholar]
- Luoto, A.; Tolvanen, M.; Rantavuori, K.; Pohjola, V.; Lahti, S. Can parents and children evaluate each other’s dental fear? Eur. J. Oral Sci. 2010, 118, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Alwin, N.P.; Murray, J.J.; Britton, P.G. An assessment of dental anxiety in children. Br. Dent. J. 1991, 171, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E.; Baez, R.J.; World Health, O. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Sharma, A.; Kumar, D.; Anand, A.; Mittal, V.; Singh, A.; Aggarwal, N. Factors predicting behavior management problems during initial dental examination in children aged 2 to 8 years. Int. J. Clin. Pediatr. Dent. 2017, 10, 5–9. [Google Scholar]
- Ahmad, A.; Kazi, M.S.A.; Ahmad, I. Evaluation of dental anxiety among children visiting paediatric dental department at children hospital. J. Pak. Med Assoc. 2017, 67, 1532–1535. [Google Scholar]
- Yon, M.J.Y.; Chen, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. An introduction to assessing dental fear and anxiety in children. Healthcare 2020, 8, 86. [Google Scholar] [CrossRef]
- Gustafsson, A.; Arnrup, K.; Broberg, A.G.; Bodin, L.; Berggren, U. Child dental fear as measured with the dental subscale of the children’s fear survey schedule: The impact of referral status and type of informant (child versus parent). Community Dent. Oral. Epidemiol. 2010, 38, 256–266. [Google Scholar] [CrossRef]
- Baier, K.; Milgrom, P.; Russell, S.; Mancl, L.; Yoshida, T. Children’s fear and behavior in private pediatric dentistry practices. Pediatr Dent. 2004, 26, 316–321. [Google Scholar]
- Ma, L.; Wang, M.; Jing, Q.; Zhao, J.; Wan, K.; Xu, Q. Reliability and validity of the Chinese version of the children’s fear survey schedule-dental subscale. Int. J. Paediatr. Dent. 2015, 25, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Salem, K.; Kousha, M.; Anissian, A.; Shahabi, A. Dental fear and concomitant factors in 3–6 year-old children. J. Dent. Res. Dent. Clin. Dent. Prospect. 2012, 6, 70–74. [Google Scholar]
| 1 | Definitely negative | Refusal of treatment, forceful crying, fearfulness, or any other overt evidence of extreme negativism. |
| 2 | Negative | Reluctance to accept treatment, uncooperative, some evidence of negative attitude but not pronounced (sullen, withdrawn). |
| 3 | Positive | Acceptance of treatment; cautious behaviour at times; willingness to comply with dentist, at times with reservation, but child follows dentist’s directions cooperatively. |
| 4 | Definitely positive | Good rapport with the dentist, interest in the dental procedures, laughter and enjoyment. |
| FBRS Score | 1 Definitely Negative | 2 Negative | 3 Positive | 4 Definitely Positive | p-Value |
|---|---|---|---|---|---|
| Age | <0.001 | ||||
| 3 | 5 (2.9%) | 12 (7%) | 18 (10.5%) | 137 (79.7%) | |
| 4 | 2 (1.2%) | 1 (0.6%) | 23 (13.9%) | 140 (84.3%) | |
| 5 | 0 (0%) | 0 (0%) | 12 (7.5%) | 148 (92.5%) | |
| Sex | 0.822 | ||||
| Male | 4 (1.6%) | 8 (3.2%) | 27 (10.8%) | 210 (84.3%) | |
| Female | 3 (1.2%) | 5 (2.0%) | 26 (10.4%) | 215 (86.3%) | |
| Total | 7 (1.4%) | 13 (2.6%) | 53 (10.6%) | 425 (85.3%) |
| Factors | Negative Behaviour | Positive Behaviour | p Value |
|---|---|---|---|
| Caries experience (dmft > 0) | 0.914 | ||
| Yes | 9 (45%) | 221 (46%) | |
| No | 11 (55%) | 257 (54%) | |
| Consequences of untreated caries | 1.000 | ||
| Yes | 3 (15%) | 70 (15%) | |
| No | 17 (85%) | 408 (85%) | |
| Daily toothbrushing | 1.000 | ||
| Yes | 19 (95%) | 441 (92%) | |
| No | 1 (5%) | 37 (8%) | |
| Use of toothpaste † | 0.247 | ||
| Yes | 6 (30%) | 91 (19%) | |
| No | 14 (70%) | 387 (81%) | |
| Daily snack habit | 1.000 | ||
| Yes | 18 (90%) | 418 (87%) | |
| No | 2 (10%) | 60 (13%) | |
| Parents as main caregiver | 0.768 | ||
| Yes | 15 (75%) | 339 (71%) | |
| No | 5 (25%) | 137 (29%) | |
| Child’s dental experience † | 1.000 | ||
| Yes | 3 (15%) | 70 (15%) | |
| No | 17 (85%) | 408 (85%) | |
| Hospitalisation experience | 0.402 | ||
| Yes | 10 (50%) | 194 (41%) | |
| No | 10 (50%) | 284 (59%) | |
| Born in Hong Kong | 0.711 | ||
| Yes | 19 (95%) | 426 (81%) | |
| No | 1 (5%) | 52 (11%) | |
| Parent’s satisfaction of child’s dental health | 0.121 | ||
| Yes | 5 (25%) | 203 (42%) | |
| No | 15 (75%) | 275 (58%) | |
| Parent’s satisfaction of child’s teeth appearance | 0.860 | ||
| Yes | 15 (75%) | 350 (73%) | |
| No | 5 (25%) | 128 (27%) | |
| Father attained more than mandatory education | 0.718 | ||
| Yes | 14 (70%) | 354 (74%) | |
| No | 6 (30%) | 126 (26%) | |
| Mother attained more than mandatory education | 0.347 | ||
| Yes | 12 (60%) | 334 (70%) | |
| No | 8 (40%) | 144 (30%) | |
| Household income above median | 0.798 | ||
| Yes | 15 (75%) | 346 (72%) | |
| No | 5 (25%) | 132 (28%) | |
| Mother’s dental visit experience † | 0.766 | ||
| Yes | 9 (69%) | 288 (72%) | |
| No | 4 (31%) | 114 (28%) | |
| Mother’s dental treatment experience † | 0.777 | ||
| Yes | 9 (69%) | 256 (64%) | |
| No | 4 (31%) | 146 (36%) | |
| Mother’s own dental fear † | 0.632 | ||
| Afraid | 2 (22%) | 44 (15%) | |
| Not afraid | 7 (78%) | 247 (85%) | |
| Mother rescheduled or cancelled appointments before † | 1.000 | ||
| Yes | 0 (0%) | 25 (6%) | |
| No | 13 (100%) | 377 (94%) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yon, M.J.Y.; Chen, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Dental Fear and Anxiety of Kindergarten Children in Hong Kong: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 2827. https://doi.org/10.3390/ijerph17082827
Yon MJY, Chen KJ, Gao SS, Duangthip D, Lo ECM, Chu CH. Dental Fear and Anxiety of Kindergarten Children in Hong Kong: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2020; 17(8):2827. https://doi.org/10.3390/ijerph17082827
Chicago/Turabian StyleYon, Madeline Jun Yu, Kitty Jieyi Chen, Sherry Shiqian Gao, Duangporn Duangthip, Edward Chin Man Lo, and Chun Hung Chu. 2020. "Dental Fear and Anxiety of Kindergarten Children in Hong Kong: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 17, no. 8: 2827. https://doi.org/10.3390/ijerph17082827
APA StyleYon, M. J. Y., Chen, K. J., Gao, S. S., Duangthip, D., Lo, E. C. M., & Chu, C. H. (2020). Dental Fear and Anxiety of Kindergarten Children in Hong Kong: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 17(8), 2827. https://doi.org/10.3390/ijerph17082827







