Engagement with a Web-Based Health Promotion Intervention among Vocational School Students: A Secondary User and Usage Analysis
Abstract
1. Introduction
2. Materials and Methods
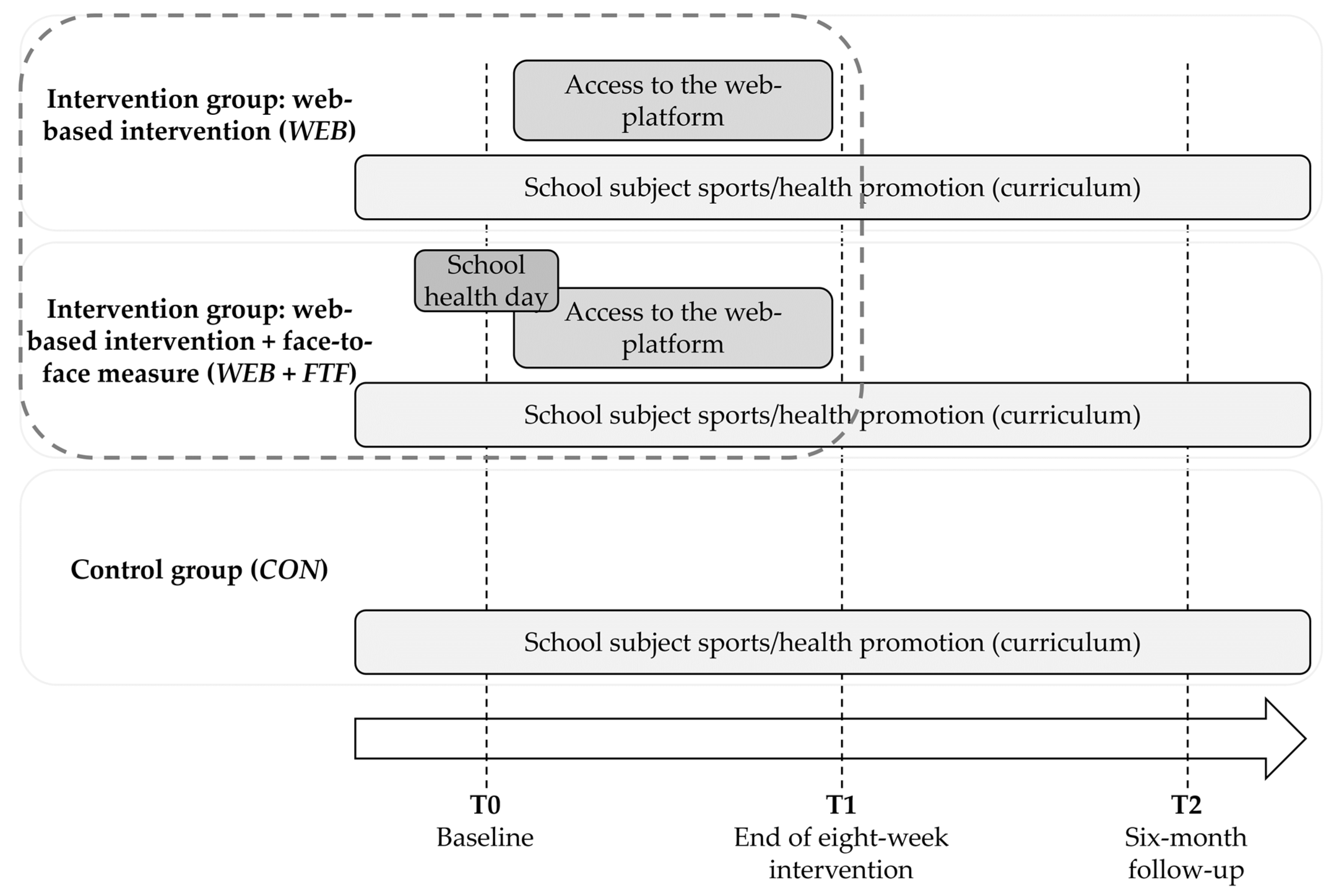
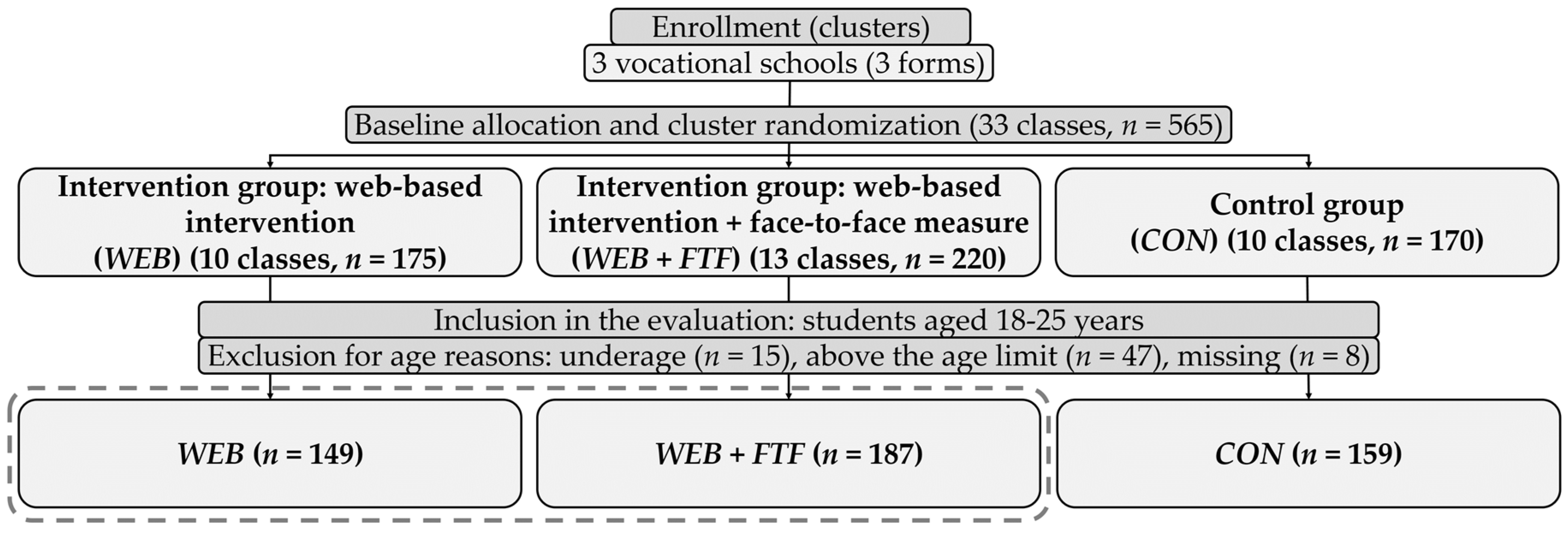
2.1. Study Design and Participants
2.2. Intervention Groups
2.2.1. Web-Based Intervention (WEB)
2.2.2. Web-Based Intervention with an Initial Face-to-Face Contact (WEB + FTF)
2.3. Log-Data
2.4. Measures
2.5. Statistical Analyses and Visualizations
3. Results
3.1. Influencing Factors on Intially Logging in
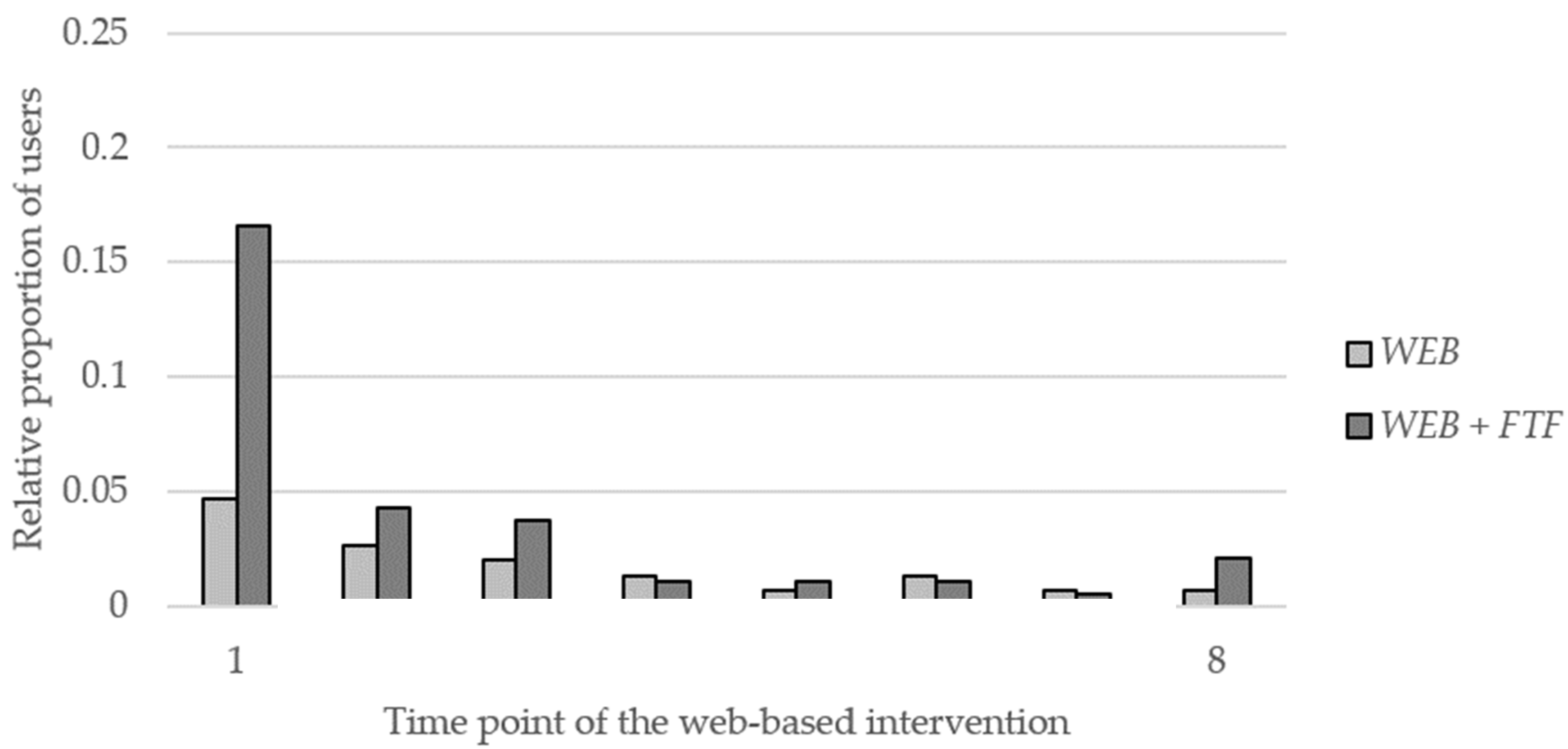
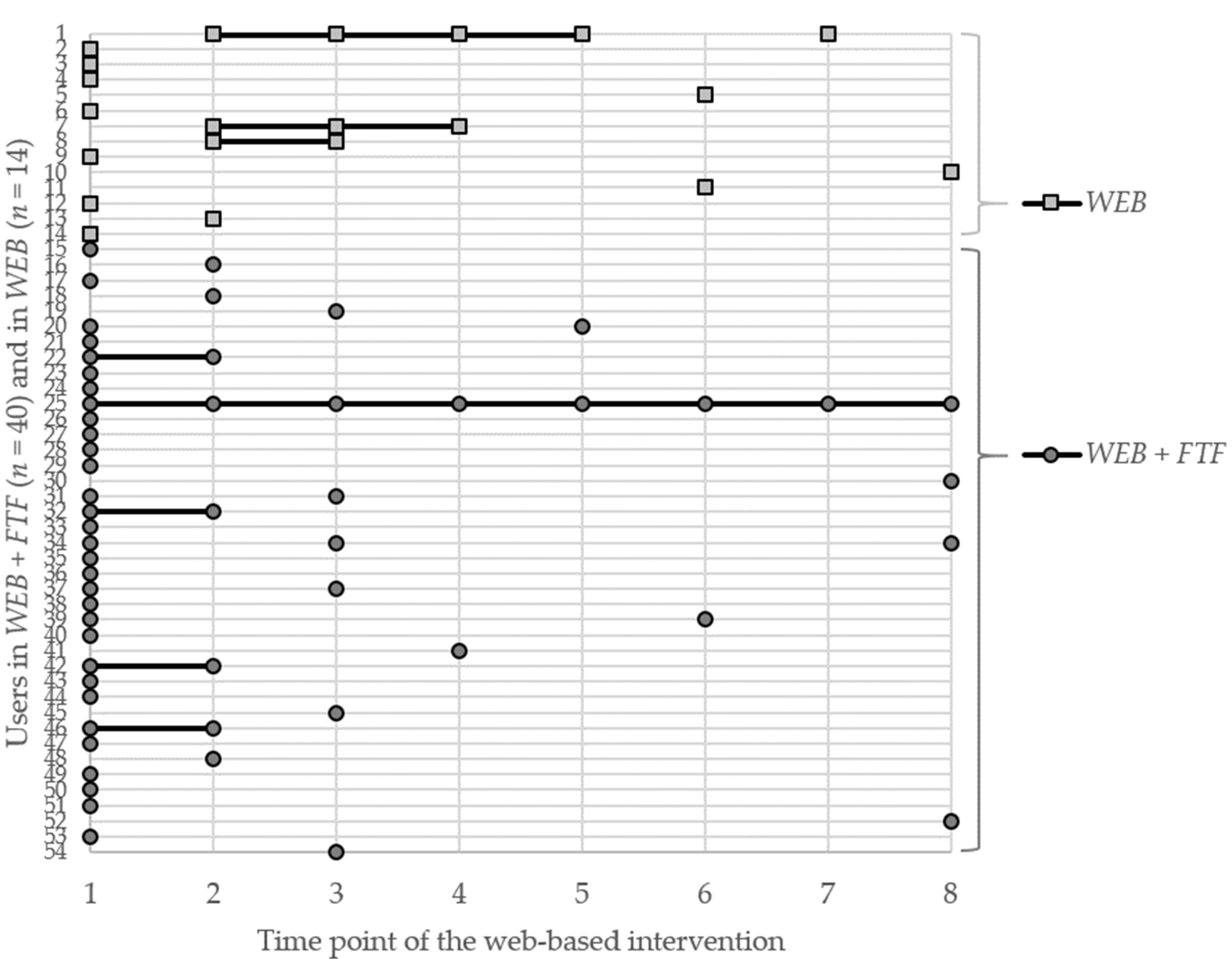
3.2. Engagement
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Muñoz, R.F. Using evidence-based internet interventions to reduce health disparities worldwide. J. Med. Internet Res. 2010, 12, e60. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Müller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, Present, and Future of eHealth and mHealth Research to Improve Physical Activity and Dietary Behaviors. J. Nutr. Educ. Behav. 2016, 48, 219–228. [Google Scholar] [CrossRef] [PubMed]
- van de Belt, T.H.; Engelen, L.J.L.P.G.; Berben, S.A.A.; Teerenstra, S.; Samsom, M.; Schoonhoven, L. Internet and social media for health-related information and communication in health care: Preferences of the Dutch general population. J. Med. Internet Res. 2013, 15, e220. [Google Scholar] [CrossRef] [PubMed]
- Beck, F.; Richard, J.-B.; Nguyen-Thanh, V.; Montagni, I.; Parizot, I.; Renahy, E. Use of the internet as a health information resource among French young adults: Results from a nationally representative survey. J. Med. Internet Res. 2014, 16, e128. [Google Scholar] [CrossRef] [PubMed]
- Montagni, I.; Cariou, T.; Feuillet, T.; Langlois, E.; Tzourio, C. Exploring Digital Health Use and Opinions of University Students: Field Survey Study. JMIR Mhealth Uhealth 2018, 6, e65. [Google Scholar] [CrossRef] [PubMed]
- Wangberg, S.C.; Bergmo, T.S.; Johnsen, J.-A.K. Adherence in Internet-based interventions. Patient Prefer. Adherence 2008, 2, 57–65. [Google Scholar]
- Geraghty, A.W.A.; Torres, L.D.; Leykin, Y.; Pérez-Stable, E.J.; Muñoz, R.F. Understanding attrition from international Internet health interventions: A step towards global eHealth. Health Promot. Int. 2013, 28, 442–452. [Google Scholar] [CrossRef]
- Eysenbach, G. The law of attrition. J. Med. Internet Res. 2005, 7, e11. [Google Scholar] [CrossRef]
- Crutzen, R.M.M. Hard to Get, Hard to Keep: Dissemination of and Exposure to Internet-delivered Health Behaviour Change Interventions Aimed at Adolescents. Ph.D. Thesis, University of Maastricht, Maastricht, The Netherlands, 2009. [Google Scholar]
- Lau, P.W.C.; Lau, E.Y.; Wong, D.P.; Ransdell, L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J. Med. Internet Res. 2011, 13, e48. [Google Scholar] [CrossRef]
- Lentferink, A.J.; Oldenhuis, H.K.; de Groot, M.; Polstra, L.; Velthuijsen, H.; van Gemert-Pijnen, J.E. Key Components in eHealth Interventions Combining Self-Tracking and Persuasive eCoaching to Promote a Healthier Lifestyle: A Scoping Review. J. Med. Internet Res. 2017, 19, e277. [Google Scholar] [CrossRef]
- Brouwer, W.; Kroeze, W.; Crutzen, R.; de Nooijer, J.; de Vries, N.K.; Brug, J.; Oenema, A. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J. Med. Internet Res. 2011, 13, e2. [Google Scholar] [CrossRef] [PubMed]
- Crutzen, R.; de Nooijer, J.; Brouwer, W.; Oenema, A.; Brug, J.; de Vries, N.K. Strategies to facilitate exposure to internet-delivered health behavior change interventions aimed at adolescents or young adults: A systematic review. Health Educ. Behav. 2011, 38, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Kelders, S.M.; Kok, R.N.; Ossebaard, H.C.; van Gemert-Pijnen, J.E.W.C. Persuasive system design does matter: A systematic review of adherence to web-based interventions. J. Med. Internet Res. 2012, 14, e152. [Google Scholar] [CrossRef] [PubMed]
- Kelders, S.M.; van Gemert-Pijnen, J.E.W.C.; Werkman, A.; Nijland, N.; Seydel, E.R. Effectiveness of a Web-based intervention aimed at healthy dietary and physical activity behavior: A randomized controlled trial about users and usage. J. Med. Internet Res. 2011, 13, e32. [Google Scholar] [CrossRef]
- Kelders, S.M.; van Gemert-Pijnen, J.E.W.C.; Werkman, A.; Seydel, E.R. Usage and effect of a web-based intervention for the prevention of overweight; a RCT. Stud. Health Technol. Inform. 2010, 160, 28–32. [Google Scholar]
- Verheijden, M.W.; Jans, M.P.; Hildebrandt, V.H.; Hopman-Rock, M. Rates and determinants of repeated participation in a web-based behavior change program for healthy body weight and healthy lifestyle. J. Med. Internet. Res. 2007, 9, e1. [Google Scholar] [CrossRef]
- Jameson, J.E. Inverse care law. Lancet 1971, 297, 648–649. [Google Scholar] [CrossRef]
- Brouwer, W.; Oenema, A.; Raat, H.; Crutzen, R.; de Nooijer, J.; de Vries, N.K.; Brug, J. Characteristics of visitors and revisitors to an Internet-delivered computer-tailored lifestyle intervention implemented for use by the general public. Health Educ. Res. 2010, 25, 585–595. [Google Scholar] [CrossRef]
- Robroek, S.J.W.; Brouwer, W.; Lindeboom, D.; Oenema, A.; Burdorf, A. Demographic, behavioral, and psychosocial correlates of using the website component of a worksite physical activity and healthy nutrition promotion program: A longitudinal study. J. Med. Internet Res. 2010, 12, e44. [Google Scholar] [CrossRef]
- van der Mispel, C.; Poppe, L.; Crombez, G.; Verloigne, M.; de Bourdeaudhuij, I. A Self-Regulation-Based eHealth Intervention to Promote a Healthy Lifestyle: Investigating User and Website Characteristics Related to Attrition. J. Med. Internet Res. 2017, 19, e241. [Google Scholar] [CrossRef]
- Mackert, M.; Mabry-Flynn, A.; Champlin, S.; Donovan, E.E.; Pounders, K. Health Literacy and Health Information Technology Adoption: The Potential for a New Digital Divide. J. Med. Internet Res. 2016, 18, e264. [Google Scholar] [CrossRef] [PubMed]
- Reinwand, D.A.; Schulz, D.N.; Crutzen, R.; Kremers, S.P.; de Vries, H. Who Follows eHealth Interventions as Recommended? A Study of Participants’ Personal Characteristics From the Experimental Arm of a Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e115. [Google Scholar] [CrossRef] [PubMed]
- National Academy of Sciences; Committee on Improving the Health, Safety and Well-Being of Young Adults; Bonnie, R.J.; Stroud, C.; Breiner, H. Investing in the Health and Well-Being of Young Adults; The National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Oosterveen, E.; Tzelepis, F.; Ashton, L.; Hutchesson, M.J. A systematic review of eHealth behavioral interventions targeting smoking, nutrition, alcohol, physical activity and/or obesity for young adults. Prev. Med. 2017, 99, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Sumanen, H.; Pietiläinen, O.; Lahti, J.; Lahelma, E.; Rahkonen, O. Sickness absence among young employees: Trends from 2002 to 2013. J. Occup. Health 2015, 57, 474–481. [Google Scholar] [CrossRef]
- Boström, M.; Holmgren, K.; Sluiter, J.K.; Hagberg, M.; Grimby-Ekman, A. Experiences of work ability in young workers: An exploratory interview study. Int. Arch. Occup. Environ. Health 2016, 89, 629–640. [Google Scholar] [CrossRef]
- United Nations. World Population Ageing 2017—Highlights; Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2017. [Google Scholar]
- Arnett, J.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef]
- Due, P.; Krølner, R.; Rasmussen, M.; Andersen, A.; Trab Damsgaard, M.; Graham, H.; Holstein, B.E. Pathways and mechanisms in adolescence contribute to adult health inequalities. Scand. J. Public Health 2011, 39 (Suppl. 6), 62–78. [Google Scholar] [CrossRef]
- Daw, J.; Margolis, R.; Wright, L. Emerging Adulthood, Emergent Health Lifestyles: Sociodemographic Determinants of Trajectories of Smoking, Binge Drinking, Obesity, and Sedentary Behavior. J. Health Soc. Behav. 2017, 58, 181–197. [Google Scholar] [CrossRef]
- Lawrence, E.M.; Mollborn, S.; Hummer, R.A. Health lifestyles across the transition to adulthood: Implications for health. Soc. Sci. Med. 2017, 193, 23–32. [Google Scholar] [CrossRef]
- Arnett, J.J.; Žukauskienė, R.; Sugimura, K. The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. Lancet Psychiatry 2014, 1, 569–576. [Google Scholar] [CrossRef]
- van ’t Riet, J.; Crutzen, R.; de Vries, H. Investigating predictors of visiting, using, and revisiting an online health-communication program: A longitudinal study. J. Med. Internet Res. 2010, 12, e37. [Google Scholar] [CrossRef] [PubMed]
- Perski, O.; Blandford, A.; West, R.; Michie, S. Conceptualising engagement with digital behaviour change interventions: A systematic review using principles from critical interpretive synthesis. Transl. Behav. Med. 2017, 7, 254–267. [Google Scholar] [CrossRef] [PubMed]
- Crutzen, R.; Cyr, D.; de Vries, N.K. Bringing loyalty to e-Health: Theory validation using three internet-delivered interventions. J. Med. Internet Res. 2011, 13, e73. [Google Scholar] [CrossRef] [PubMed]
- Grieben, C.; Stassen, G.; Froböse, I. Internetbasierte Gesundheitsförderung. Prävention und Gesundh. 2017, 12, 154–159. [Google Scholar] [CrossRef]
- Stassen, G.; Grieben, C.; Sauzet, O.; Froböse, I.; Schaller, A. Health literacy promotion among young adults: A web-based intervention in German vocational schools. Health Educ. Res. 2020, 35, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Schulsport NRW. Lehrplan zur Erprobung Sport/Gesundheitsförderung in den Fachklassen der dualen Berufsausbildung. Available online: https://www.schulsport-nrw.de/fileadmin/user_upload/schulsportpraxis_und_fortbildung/pdf/sport_gesundheitsfoerderung.pdf (accessed on 21 February 2020).
- Grieben, C.; Stassen, G.; Froböse, I. How Should Web-Based Physical Activity and Healthy Eating Interventions be Designed for Young Office Workers? A Qualitative Approach. J. Healthc. Commun. 2018, 3. [Google Scholar] [CrossRef]
- Hasselhorn, H.M.; Freude, G. Der Work Ability Index Ein Leitfaden; Wirtschaftsverl. NW Verl. für neue Wiss: Bremerhaven, Free Hanseatic City of Bremen, Germany, 2007. [Google Scholar]
- Kujala, V.; Remes, J.; Ek, E.; Tammelin, T.; Laitinen, J. Classification of Work Ability Index among young employees. Occup. Med. (Lond.) 2005, 55, 399–401. [Google Scholar] [CrossRef]
- Eskelinen, L.; Kohvakka, A.; Merisalo, T.; Hurri, H.; Wägar, G. Relationship between the self-assessment and clinical assessment of health status and work ability. Scand. J. Work Environ. Health 1991, 17 (Suppl. 1), 40–47. [Google Scholar]
- Nygård, C.H.; Eskelinen, L.; Suvanto, S.; Tuomi, K.; Ilmarinen, J. Associations between functional capacity and work ability among elderly municipal employees. Scand. J. Work Environ. Health 1991, 17 (Suppl. 1), 122–127. [Google Scholar]
- de Zwart, B.C.H.; Frings-Dresen, M.H.W.; van Duivenbooden, J.C. Test-retest reliability of the Work Ability Index questionnaire. Occup. Med. (Lond.) 2002, 52, 177–181. [Google Scholar] [CrossRef]
- Notenbomer, A.; Groothoff, J.W.; van Rhenen, W.; Roelen, C.A.M. Associations of work ability with frequent and long-term sickness absence. Occup. Med. (Lond.) 2015, 65, 373–379. [Google Scholar] [CrossRef] [PubMed]
- WHO Collaborating Center for Mental Health. WHO (Fünf)—Fragebogen zum Wohlbefinden: (Version 1998); Frederiksborg General Hospital, Frederiksberg: Copenhagen, Denmark, 1998; Available online: https://www.psykiatri-regionh.dk/who-5/Documents/WHO5_German.pdf (accessed on 28 November 2019).
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Hall, T.; Krahn, G.L.; Horner-Johnson, W.; Lamb, G. Examining functional content in widely used Health-Related Quality of Life scales. Rehabil. Psychol. 2011, 56, 94–99. [Google Scholar] [CrossRef]
- Milton, K.; Bull, F.C.; Bauman, A. Reliability and validity testing of a single-item physical activity measure. Br. J. Sports Med. 2011, 45, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Stanner, S. At Least Five a Week—A summary of the report from the Chief Medical Officer on physical activity. Nutr. Bull. 2004, 29, 350–352. [Google Scholar] [CrossRef]
- Lenartz, N. Gesundheitskompetenz und Selbstregulation; V&R unipress: Göttingen, Lower Saxony, Germany, 2012. [Google Scholar]
- Soellner, R.; Lenartz, N.; Rudinger, G. Concept mapping as an approach for expert-guided model building: The example of health literacy. Eval. Program Plann. 2017, 60, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmann, K.; Beauducel, A.; Predel, G.; Preuß, M.; Preuß, P.; Rudinger, G. Evaluation des Gesundheitsverhaltens Studierender. Diagnostica 2015, 61, 163–171. [Google Scholar] [CrossRef]
- World Health Organization. Obesity—Preventing and Managing the Global Epidemic. Report on a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Schienkiewitz, A.; Mensink, G.B.M.; Kuhnert, R.; Lange, C. Übergewicht und Adipositas bei Erwachsenen in Deutschland: Fact Sheet. J. Health Monit. 2017, 2, 21–28. [Google Scholar] [CrossRef]
- Betz, M.; Cassel, W.; Köhler, U. Schlafgewohnheiten und Gesundheit bei Jugendlichen und jungen Erwachsenen – Auswirkungenen von Schlafdefizit auf Leistungsfähigkeit und Wohlbefinden. Dtsch. med. Wochenschr. 2012, 137. [Google Scholar] [CrossRef]
- Robert Koch-Institut. Ergebnisse der Studie “Gesundheit in Deutschland aktuell 2012”. Beiträge zur Gesundheitsberichterstattung des Bundes. RKI: Berlin, Germany, 2014. [Google Scholar]
- Statistisches Bundesamt (Destatis). Bildung und Kultur: Berufliche Bildung 2018. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bildung-Forschung-Kultur/Berufliche-Bildung/Publikationen/Downloads-Berufliche-Bildung/berufliche-bildung-2110300187004.pdf?__blob=publicationFile (accessed on 23 February 2020).
- Clarke, A.M.; Kuosmanen, T.; Barry, M.M. A systematic review of online youth mental health promotion and prevention interventions. J. Youth Adolesc. 2015, 44, 90–113. [Google Scholar] [CrossRef] [PubMed]
- Nour, M.; Yeung, S.H.; Partridge, S.; Allman-Farinelli, M. A Narrative Review of Social Media and Game-Based Nutrition Interventions Targeted at Young Adults. J. Acad. Nutr. Diet. 2017, 117, 735–752. [Google Scholar] [CrossRef] [PubMed]
- Nölke, L.; Mensing, M.; Krämer, A.; Hornberg, C. Sociodemographic and health-(care-)related characteristics of online health information seekers: A cross-sectional German study. BMC Public Health 2015, 15, 31. [Google Scholar] [CrossRef] [PubMed]
- Ashton, L.M.; Hutchesson, M.J.; Rollo, M.E.; Morgan, P.J.; Collins, C.E. A scoping review of risk behaviour interventions in young men. BMC Public Health 2014, 14, 957. [Google Scholar] [CrossRef] [PubMed]
- Pagoto, S.L.; Schneider, K.L.; Oleski, J.L.; Luciani, J.M.; Bodenlos, J.S.; Whited, M.C. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity (Silver Spring) 2012, 20, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Joseph, R.P.; Durant, N.H.; Benitez, T.J.; Pekmezi, D.W. Internet-Based Physical Activity Interventions. Am. J. Lifestyle Med. 2014, 8, 42–68. [Google Scholar] [CrossRef]
- Ashton, L.M.; Morgan, P.J.; Hutchesson, M.J.; Rollo, M.E.; Collins, C.E. Young Men’s Preferences for Design and Delivery of Physical Activity and Nutrition Interventions: A Mixed-Methods Study. Am. J. Mens. Health 2017, 11, 1588–1599. [Google Scholar] [CrossRef]
- Suri, V.R.; Majid, S.; Chang, Y.-K.; Foo, S. Assessing the influence of health literacy on health information behaviors: A multi-domain skills-based approach. Patient Educ. Couns. 2016, 99, 1038–1045. [Google Scholar] [CrossRef]
- Diviani, N.; van den Putte, B.; Giani, S.; van Weert, J.C. Low health literacy and evaluation of online health information: A systematic review of the literature. J. Med. Internet Res. 2015, 17, e112. [Google Scholar] [CrossRef]
- Stellefson, M.; Hanik, B.; Chaney, B.; Chaney, D.; Tennant, B.; Chavarria, E.A. eHealth literacy among college students: A systematic review with implications for eHealth education. J. Med. Internet Res. 2011, 13, e102. [Google Scholar] [CrossRef]
- Cook, T.L.; de Bourdeaudhuij, I.; Maes, L.; Haerens, L.; Grammatikaki, E.; Widhalm, K.; Kwak, L.; Plada, M.; Moreno, L.A.; Zampelas, A.; et al. Moderators of the effectiveness of a web-based tailored intervention promoting physical activity in adolescents: The HELENA Activ-O-Meter. J. Sch. Health 2014, 84, 256–266. [Google Scholar] [CrossRef]
- Morton, C.E.; Saleh, S.N.; Smith, S.F.; Hemani, A.; Ameen, A.; Bennie, T.D.; Toro-Troconis, M. Blended learning: How can we optimise undergraduate student engagement? BMC Med. Educ. 2016, 16, 195. [Google Scholar] [CrossRef]
- Neil, A.L.; Batterham, P.; Christensen, H.; Bennett, K.; Griffiths, K.M. Predictors of adherence by adolescents to a cognitive behavior therapy website in school and community-based settings. J. Med. Internet Res. 2009, 11, e6. [Google Scholar] [CrossRef] [PubMed]
- Nitsch, M.; Adamcik, T.; Kuso, S.; Zeiler, M.; Waldherr, K. Usability and Engagement Evaluation of an Unguided Online Program for Promoting a Healthy Lifestyle and Reducing the Risk for Eating Disorders and Obesity in the School Setting. Nutrients 2019, 11, 713. [Google Scholar] [CrossRef] [PubMed]
- de Bourdeaudhuij, I.; Maes, L.; de Henauw, S.; de Vriendt, T.; Moreno, L.A.; Kersting, M.; Sarri, K.; Manios, Y.; Widhalm, K.; Sjöstrom, M.; et al. Evaluation of a computer-tailored physical activity intervention in adolescents in six European countries: The Activ-O-Meter in the HELENA intervention study. J. Adolesc. Health 2010, 46, 458–466. [Google Scholar] [CrossRef]
- Schoeppe, S.; Alley, S.; van Lippevelde, W.; Bray, N.A.; Williams, S.L.; Duncan, M.J.; Vandelanotte, C. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 127. [Google Scholar] [CrossRef] [PubMed]
- Vandelanotte, C.; Spathonis, K.M.; Eakin, E.G.; Owen, N. Website-delivered physical activity interventions a review of the literature. Am. J. Prev. Med. 2007, 33, 54–64. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, M.M.; Merry, K.J.; Locke, S.R.; Jung, M.E. Effects of Mobile Health Prompts on Self-Monitoring and Exercise Behaviors Following a Diabetes Prevention Program: Secondary Analysis From a Randomized Controlled Trial. JMIR Mhealth Uhealth 2019, 7, e12956. [Google Scholar] [CrossRef] [PubMed]
- Bidargaddi, N.; Almirall, D.; Murphy, S.; Nahum-Shani, I.; Kovalcik, M.; Pituch, T.; Maaieh, H.; Strecher, V. To Prompt or Not to Prompt? A Microrandomized Trial of Time-Varying Push Notifications to Increase Proximal Engagement With a Mobile Health App. JMIR Mhealth Uhealth 2018, 6, e10123. [Google Scholar] [CrossRef]
- Robroek, S.J.W.; Lindeboom, D.E.M.; Burdorf, A. Initial and sustained participation in an internet-delivered long-term worksite health promotion program on physical activity and nutrition. J. Med. Internet Res. 2012, 14, e43. [Google Scholar] [CrossRef]
- Fry, J.P.; Neff, R.A. Periodic prompts and reminders in health promotion and health behavior interventions: Systematic review. J. Med. Internet Res. 2009, 11, e16. [Google Scholar] [CrossRef]
- Alkhaldi, G.; Hamilton, F.L.; Lau, R.; Webster, R.; Michie, S.; Murray, E. The Effectiveness of Prompts to Promote Engagement With Digital Interventions: A Systematic Review. J. Med. Internet Res. 2016, 18, e6. [Google Scholar] [CrossRef] [PubMed]
- Tong, H.L.; Coiera, E.; Laranjo, L. Using a Mobile Social Networking App to Promote Physical Activity: A Qualitative Study of Users’ Perspectives. J. Med. Internet Res. 2018, 20, e11439. [Google Scholar] [CrossRef] [PubMed]
- Middelweerd, A.; van der Laan, D.M.; van Stralen, M.M.; Mollee, J.S.; Stuij, M.; te Velde, S.J.; Brug, J. What features do Dutch university students prefer in a smartphone application for promotion of physical activity? A qualitative approach. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 31. [Google Scholar] [CrossRef] [PubMed]
- Dute, D.J.; Bemelmans, W.J.E.; Breda, J. Using Mobile Apps to Promote a Healthy Lifestyle Among Adolescents and Students: A Review of the Theoretical Basis and Lessons Learned. JMIR Mhealth Uhealth 2016, 4, e39. [Google Scholar] [CrossRef]
- Poobalan, A.S.; Aucott, L.S.; Clarke, A.; Smith, W.C.S. Physical activity attitudes, intentions and behaviour among 18–25 year olds: A mixed method study. BMC Public Health 2012, 12, 640. [Google Scholar] [CrossRef]
- Giles, E.L.; Brennan, M. Changing the lifestyles of young adults. J. Soc. Mark. 2015, 5, 206–225. [Google Scholar] [CrossRef]
- Berry, E.; Aucott, L.; Poobalan, A. Are young adults appreciating the health promotion messages on diet and exercise? J. Public Health (Berl.) 2018, 26, 687–696. [Google Scholar] [CrossRef]
- Horvath, K.J.; Ecklund, A.M.; Hunt, S.L.; Nelson, T.F.; Toomey, T.L. Developing Internet-based health interventions: A guide for public health researchers and practitioners. J. Med. Internet. Res. 2015, 17, e28. [Google Scholar] [CrossRef]
- Blandford, A.; Gibbs, J.; Newhouse, N.; Perski, O.; Singh, A.; Murray, E. Seven lessons for interdisciplinary research on interactive digital health interventions. Digit. Health 2018, 4. [Google Scholar] [CrossRef]
- Baker, T.B.; Gustafson, D.H.; Shah, D. How can research keep up with eHealth? Ten strategies for increasing the timeliness and usefulness of eHealth research. J. Med. Internet Res. 2014, 16, e36. [Google Scholar] [CrossRef]
- Rogers, E.M. Diffusion of Innovations, 5th ed.; Simon&Schuster: New York, NY, USA, 2003. [Google Scholar]
- Couper, M.P.; Alexander, G.L.; Zhang, N.; Little, R.J.A.; Maddy, N.; Nowak, M.A.; McClure, J.B.; Calvi, J.J.; Rolnick, S.J.; Stopponi, M.A.; et al. Engagement and retention: Measuring breadth and depth of participant use of an online intervention. J. Med. Internet. Res. 2010, 12, e52. [Google Scholar] [CrossRef] [PubMed]
- Morrison, L.G.; Geraghty, A.W.A.; Lloyd, S.; Goodman, N.; Michaelides, D.T.; Hargood, C.; Weal, M.; Yardley, L. Comparing usage of a web and app stress management intervention: An observational study. Internet Interv. 2018, 12, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Short, C.E.; DeSmet, A.; Woods, C.; Williams, S.L.; Maher, C.; Middelweerd, A.; Müller, A.M.; Wark, P.A.; Vandelanotte, C.; Poppe, L.; et al. Measuring Engagement in eHealth and mHealth Behavior Change Interventions: Viewpoint of Methodologies. J. Med. Internet Res. 2018, 20, e292. [Google Scholar] [CrossRef] [PubMed]
- Ryan, C.; Bergin, M.; Wells, J.S. Theoretical Perspectives of Adherence to Web-Based Interventions: A Scoping Review. Int. J. Behav. Med. 2018, 25, 17–29. [Google Scholar] [CrossRef]
- Miller, S.; Ainsworth, B.; Yardley, L.; Milton, A.; Weal, M.; Smith, P.; Morrison, L. A Framework for Analyzing and Measuring Usage and Engagement Data (AMUsED) in Digital Interventions: Viewpoint. J. Med. Internet Res. 2019, 21, e10966. [Google Scholar] [CrossRef]
- Park, S.Y. An Analysis of the Technology Acceptance Model in Understanding University Students’ Behavioral Intention to Use e-Learning. J. Edu. Tech. Soc. 2009, 12, 150–162. [Google Scholar]
- Yardley, L.; Spring, B.J.; Riper, H.; Morrison, L.G.; Crane, D.H.; Curtis, K.; Merchant, G.C.; Naughton, F.; Blandford, A. Understanding and Promoting Effective Engagement With Digital Behavior Change Interventions. Am. J. Prev. Med. 2016, 51, 833–842. [Google Scholar] [CrossRef]
- Sieverink, F.; Kelders, S.M.; van Gemert-Pijnen, J.E. Clarifying the Concept of Adherence to eHealth Technology: Systematic Review on When Usage Becomes Adherence. J. Med. Internet Res. 2017, 19, e402. [Google Scholar] [CrossRef]
- Brouwer, W.; Oenema, A.; Crutzen, R.; de Nooijer, J.; de Vries, N.K.; Brug, J. What makes people decide to visit and use an internet-delivered behavior-change intervention? Health Edu. 2009, 109, 460–473. [Google Scholar] [CrossRef]
- Brouwer, W.; Oenema, A.; Crutzen, R.; de Nooijer, J.; de Vries, N.K.; Brug, J. An exploration of factors related to dissemination of and exposure to internet-delivered behavior change interventions aimed at adults: A Delphi study approach. J. Med. Internet. Res. 2008, 10, e10. [Google Scholar] [CrossRef]
- Reinwand, D.A.; Crutzen, R.; Elfeddali, I.; Schneider, F.; Schulz, D.N.; Smit, E.S.; Stanczyk, N.E.; Tange, H.; Voncken-Brewster, V.; Walthouwer, M.J.L.; et al. Impact of Educational Level on Study Attrition and Evaluation of Web-Based Computer-Tailored Interventions: Results From Seven Randomized Controlled Trials. J. Med. Internet Res. 2015, 17, e228. [Google Scholar] [CrossRef]
- van Poppel, M.N.M.; Chinapaw, M.J.M.; Mokkink, L.B.; van Mechelen, W.; Terwee, C.B. Physical activity questionnaires for adults: A systematic review of measurement properties. Sports Med. 2010, 40, 565–600. [Google Scholar] [CrossRef] [PubMed]
- Helmerhorst, H.J.F.; Brage, S.; Warren, J.; Besson, H.; Ekelund, U. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 103. [Google Scholar] [CrossRef] [PubMed]
- Altin, S.V.; Finke, I.; Kautz-Freimuth, S.; Stock, S. The evolution of health literacy assessment tools: A systematic review. BMC Public Health 2014, 14, 1207. [Google Scholar] [CrossRef] [PubMed]
- Haun, J.N.; Valerio, M.A.; McCormack, L.A.; Sørensen, K.; Paasche-Orlow, M.K. Health literacy measurement: An inventory and descriptive summary of 51 instruments. J. Health Commun. 2014, 19 (Suppl. 2), 302–333. [Google Scholar] [CrossRef]
- Morrison, C.; Doherty, G. Analyzing engagement in a web-based intervention platform through visualizing log-data. J. Med. Internet Res. 2014, 16, e252. [Google Scholar] [CrossRef] [PubMed]
- Arden-Close, E.J.; Smith, E.; Bradbury, K.; Morrison, L.; Dennison, L.; Michaelides, D.; Yardley, L. A Visualization Tool to Analyse Usage of Web-Based Interventions: The Example of Positive Online Weight Reduction (POWeR). JMIR Hum. Factors 2015, 2, e8. [Google Scholar] [CrossRef]

| Characteristic, Outcome | n (%) 1/Mean ± SD |
|---|---|
| Sex (female) | 209 (62.2) |
| Age (years) | 20.6 ± 1.9 |
| BMI | 23.8 ± 4.7 |
| Overweight (BMI ≥ 25) 2 | 101 (30.7) |
| WAI score (range 7–49) | 39.6 ± 4.6 |
| Poor/moderate work ability (score ≤ 40) 3 | 168 (52.2) |
| WHO-5 score (range 0–100) | 47.5 ± 17.5 |
| Reduced well-being (score ≤ 50) 4 | 187 (56.0) |
| Days/week ≥ 30 minutes of physical activity | 3.2 ± 2.0 |
| Not meeting recommendations (<5 days/week) 5 | 239 (71.3) |
| Structural model of health literacy: “advanced skills” (scale 1–4) | |
| Self-perception | 3.0 ± 0.4 |
| Proactive approach to health | 2.6 ± 0.6 |
| Dealing with health information | 2.8 ± 0.6 |
| Self-control | 2.9 ± 0.5 |
| Self-regulation | 2.6 ± 0.6 |
| Communication and cooperation | 2.6 ± 0.6 |
| Factor | B | SE | p | OR | 95%-CI |
|---|---|---|---|---|---|
| Intervention group (WEB + FTF vs. WEB) | 1.089 | 0.384 | 0.005 ** | 2.971 | 1.399; 6.309 |
| Sex (female vs. male) | 0.805 | 0.404 | 0.046 * | 2.237 | 1.014; 4.934 |
| BMI (<25 vs. ≥25) | −0.254 | 0.387 | 0.512 | 0.776 | 0.398; 1.788 |
| Work Ability (WAI score > 40 vs. ≤40) | −0.170 | 0.383 | 0.657 | 0.844 | 0.398; 1.788 |
| Well-being (WHO-5 score > 50 vs. ≤50) | 0.120 | 0.404 | 0.767 | 1.127 | 0.511; 2.487 |
| Physical activity (≥5 days vs. <5) | −0.215 | 0.403 | 0.593 | 0.806 | 0.366; 1.775 |
| Self-perception | 0.056 | 0.431 | 0.896 | 1.058 | 0.455; 2.462 |
| Proactive approach to health | −0.017 | 0.318 | 0.957 | 0.983 | 0.527; 1.833 |
| Dealing with health information | 0.799 | 0.358 | 0.030 * | 2.179 | 1.081; 4.393 |
| Self-control | 0.079 | 0.390 | 0.840 | 1.082 | 0.504; 2.324 |
| Self-regulation | −0.213 | 0.339 | 0.530 | 0.808 | 0.415; 1.572 |
| Communication and cooperation | 0.071 | 0.306 | 0.816 | 1.074 | 0.589; 1.958 |
| Measure | WEB n(%) 1/Mean ± SD | WEB + FTF n (%) 1/Mean ± SD | p |
|---|---|---|---|
| Proportion of users 2 | 14 (9.4) | 40 (21.4) | 0.003 ** |
| Proportion of revisitors 3 | 9 (64.3) | 22 (55.0) | 0.545 |
| Login frequency 3 | 3.2 ± 2.3 | 2.5 ± 4.1 | 0.124 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stassen, G.; Grieben, C.; Froböse, I.; Schaller, A. Engagement with a Web-Based Health Promotion Intervention among Vocational School Students: A Secondary User and Usage Analysis. Int. J. Environ. Res. Public Health 2020, 17, 2180. https://doi.org/10.3390/ijerph17072180
Stassen G, Grieben C, Froböse I, Schaller A. Engagement with a Web-Based Health Promotion Intervention among Vocational School Students: A Secondary User and Usage Analysis. International Journal of Environmental Research and Public Health. 2020; 17(7):2180. https://doi.org/10.3390/ijerph17072180
Chicago/Turabian StyleStassen, Gerrit, Christopher Grieben, Ingo Froböse, and Andrea Schaller. 2020. "Engagement with a Web-Based Health Promotion Intervention among Vocational School Students: A Secondary User and Usage Analysis" International Journal of Environmental Research and Public Health 17, no. 7: 2180. https://doi.org/10.3390/ijerph17072180
APA StyleStassen, G., Grieben, C., Froböse, I., & Schaller, A. (2020). Engagement with a Web-Based Health Promotion Intervention among Vocational School Students: A Secondary User and Usage Analysis. International Journal of Environmental Research and Public Health, 17(7), 2180. https://doi.org/10.3390/ijerph17072180




