Relationship of Salivary Microbiome with the Worsening of the Periodontal Health Status in Young Adults: A 3-Year Cohort Study
Abstract
1. Introduction
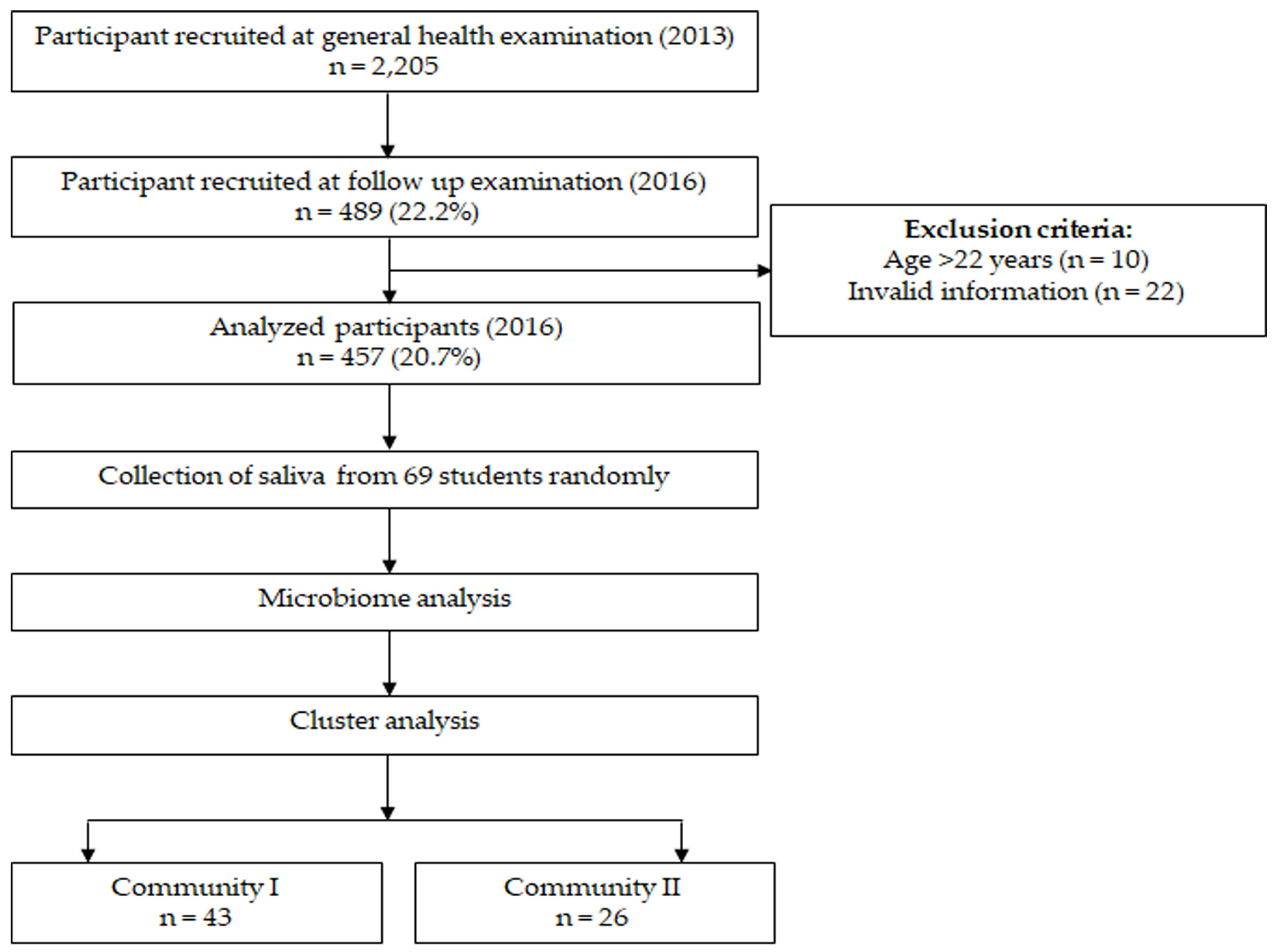
2. Materials and Methods
2.1. Ethics Statement
2.2. Study Participants
2.3. Oral Examination
2.4. Assessment of Body Mass Index (BMI)
2.5. Health-Related Questionnaire
2.6. Salivary Microbiome Analysis
2.7. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
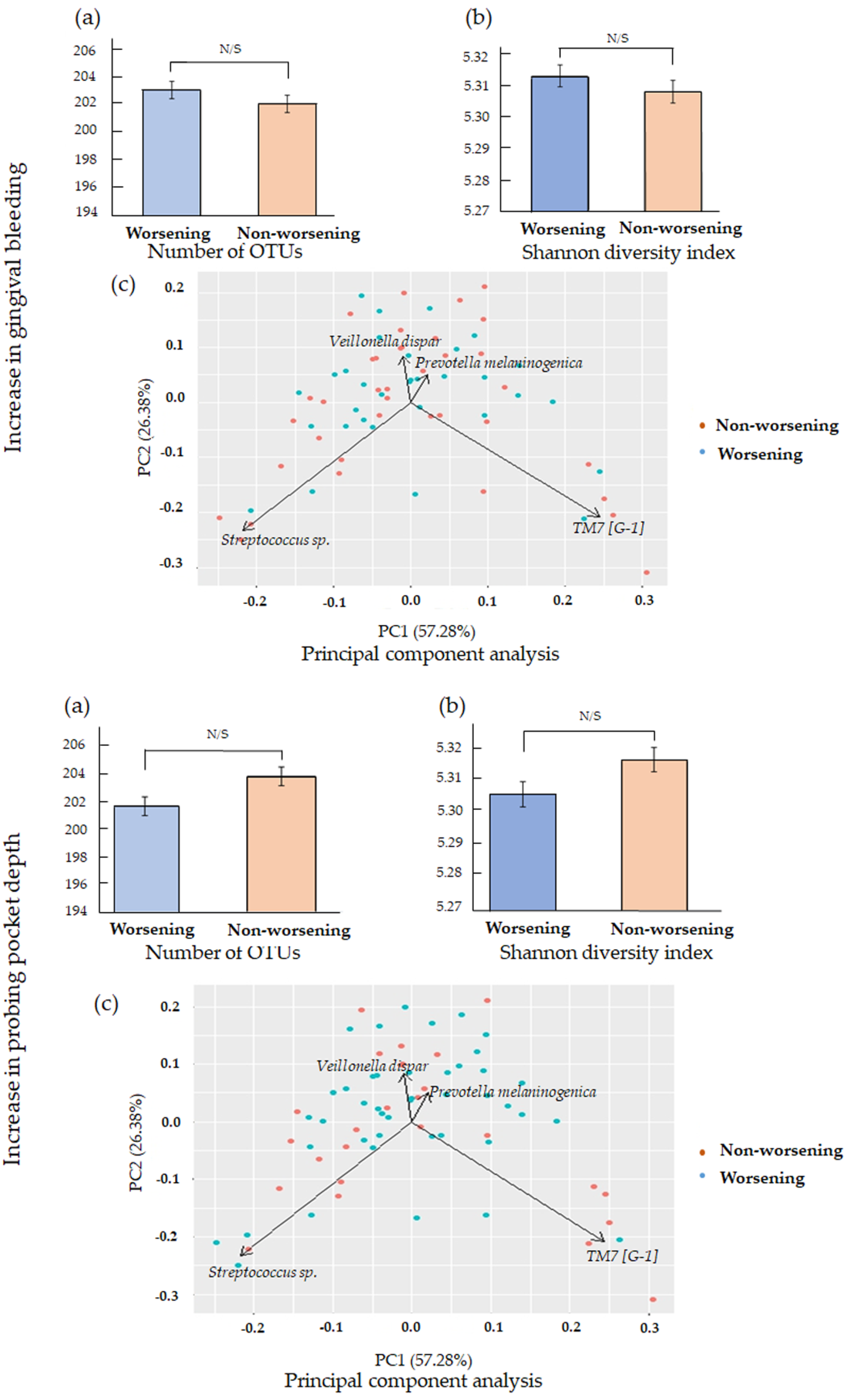
3.2. Comparison of the Salivary Microbiome Profiles
3.3. Microbiome Community Characterization
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- He, J.; Li, Y.; Cao, Y.; Xue, J.; Zhou, X. The oral microbiome diversity and its relation to human diseases. Folia Microbiol. 2014, 60, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.; Bouchard, P.; Cagetti, M.G.; Campus, G.; Carra, M.-C.; Cocco, F.; Nibali, L.; Hujoel, P.; Laine, M.L.; Lingström, P.; et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: Consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017, 44, S39–S51. [Google Scholar] [CrossRef]
- Kilian, M.; Chapple, I.L.C.; Hannig, M.; Marsh, P.D.; Meuric, V.; Pedersen, A.M.L.; Tonetti, M.S.; Wade, W.G.; Zaura, E. The oral microbiome—An update for oral healthcare professionals. Br. Dent. J. 2016, 221, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Socransky, S.S.; Haffajee, A.D. Periodontal microbial ecology. Periodontol. 2000 2005, 38, 135–187. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Chaparro, P.; Gonçalves, C.; Figueiredo, L.; Faveri, M.; Lobão, E.; Tamashiro, N.; Duarte, P.; Feres, M. Newly Identified Pathogens Associated with Periodontitis. J. Dent. Res. 2014, 93, 846–858. [Google Scholar] [CrossRef]
- Timmerman, M.; Weijden, G. Risk factors for periodontitis. Int. J. Dent. Hyg. 2006, 4, 2–7. [Google Scholar] [CrossRef]
- Kononen, E.; Paju, S.; Pussinen, P.J.; Hyvonen, M.; Tella, P.D.; Suominen-Taipale, L.; Knuuttila, M. Population-Based Study of Salivary Carriage of Periodontal Pathogens in Adults. J. Clin. Microbiol. 2007, 45, 2446–2451. [Google Scholar] [CrossRef]
- Sakamoto, M.; Umeda, M.; Ishikawa, I.; Benno, Y. Comparison of the Oral Bacterial Flora in Saliva from a Healthy Subject and Two Periodontitis Patients by Sequence Analysis of 16S rDNA Libraries. Microbiol. Immunol. 2000, 44, 643–652. [Google Scholar] [CrossRef]
- Souto, R.; Colombo, A.P.V. Prevalence of Enterococcus faecalis in subgingival biofilm and saliva of subjects with chronic periodontal infection. Arch. Oral Biol. 2008, 53, 155–160. [Google Scholar] [CrossRef]
- Belstrøm, D.; Holmstrup, P.; Nielsen, C.H.; Kirkby, N.; Twetman, S.; Heitmann, B.L.; Klepac-Ceraj, V.; Paster, B.J.; Fiehn, N.-E. Bacterial profiles of saliva in relation to diet, lifestyle factors, and socioeconomic status. J. Oral Microbiol. 2014, 6, 23609. [Google Scholar] [CrossRef]
- Salminen, A.; Kopra, K.A.E.; Hyvärinen, K.; Paju, S.; Mäntylä, P.; Buhlin, K.; Nieminen, M.S.; Sinisalo, J.; Pussinen, P.J. Quantitative PCR analysis of salivary pathogen burden in periodontitis. Front. Cell. Infect. Microbiol. 2015, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Paju, S.; Pussinen, P.J.; Suominen-Taipale, L.; Hyvonen, M.; Knuuttila, M.; Kononen, E. Detection of Multiple Pathogenic Species in Saliva Is Associated with Periodontal Infection in Adults. J. Clin. Microbiol. 2008, 47, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Kageyama, S.; Takeshita, T.; Asakawa, M.; Shibata, Y.; Takeuchi, K.; Yamanaka, W.; Yamashita, Y. Relative abundance of total subgingival plaque-specific bacteria in salivary microbiota reflects the overall periodontal condition in patients with periodontitis. PLoS ONE 2017, 12, e0174782. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, G. The Role of Bleeding upon Probing in the Diagnosis of Periodontal Disease: A Literature Review. J. Periodontol. 1984, 55, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Ekuni, D.; Mizutani, S.; Kojima, A.; Tomofuji, T.; Irie, K.; Azuma, T.; Yoneda, T.; Furuta, M.; Eshima, N.; Iwasaki, Y.; et al. Relationship between increases in BMI and changes in periodontal status: A prospective cohort study. J. Clin. Periodontol. 2014, 41, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Albandar, J.M.; Rams, T.E. Global epidemiology of periodontal diseases: An overview. Periodontol. 2000 2002, 29, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Survey on Dental Disease 2016. Available online: https://www.mhlw.go.jp/toukei/list/62-17c.html (accessed on 1 February 2019). (In Japanese).
- Furuta, M.; Ekuni, D.; Irie, K.; Azuma, T.; Tomofuji, T.; Ogura, T.; Morita, M. Sex Differences in Gingivitis Relate to Interaction of Oral Health Behaviors in Young People. J. Periodontol. 2011, 82, 558–565. [Google Scholar] [CrossRef]
- Greene, J.G.; Vermillion, J.R. The Simplified Oral Hygiene Index. J. Am. Dent. Assoc. 1964, 68, 7–13. [Google Scholar] [CrossRef]
- Ekuni, D.; Yamamoto, T.; Koyama, R.; Tsuneishi, M.; Naito, K.; Tobe, K. Relationship between body mass index and periodontitis in young Japanese adults. J. Periodontal Res. 2008, 43, 417–421. [Google Scholar] [CrossRef]
- Mizutani, S.; Ekuni, D.; Furuta, M.; Tomofuji, T.; Irie, K.; Azuma, T.; Kojima, A.; Nagase, J.; Iwasaki, Y.; Morita, M. Effects of self-efficacy on oral health behaviours and gingival health in university students aged 18- or 19-years-old. J. Clin. Periodontol. 2012, 39, 844–849. [Google Scholar] [CrossRef]
- Lang, W.P.; Farghaly, M.M.; Ronis, D.L. The relation of preventive dental behaviors to periodontal health status. J. Clin. Periodontol. 1994, 21, 194–198. [Google Scholar] [CrossRef]
- Edgar, R.C.; Haas, B.J.; Clemente, J.C.; Quince, C.; Knight, R. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics 2011, 27, 2194–2200. [Google Scholar] [CrossRef] [PubMed]
- Caporaso, J.G.; Kuczynski, J.; Stombaugh, J.; Bittinger, K.; Bushman, F.D.; Costello, E.K.; Fierer, N.; Peña, A.G.; Goodrich, J.K.; Gordon, J.I.; et al. QIIME allows analysis of high-throughput community sequencing data. Nat. Methods 2010, 7, 335–336. [Google Scholar] [CrossRef] [PubMed]
- Dewhirst, F.E.; Chen, T.; Izard, J.; Paster, B.J.; Tanner, A.C.R.; Yu, W.-H.; Lakshmanan, A.; Wade, W.G. The human oral microbiome. J. Bacteriol. 2010, 192, 5002–5017. [Google Scholar] [CrossRef]
- Takeshita, T.; Kageyama, S.; Furuta, M.; Tsuboi, H.; Takeuchi, K.; Shibata, Y.; Shimazaki, Y.; Akifusa, S.; Ninomiya, T.; Kiyohara, Y.; et al. Bacterial diversity in saliva and oral health-related conditions: The Hisayama Study. Sci. Rep. 2016, 6, 1–11. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Ren, W.; Zhang, Q.; Liu, X.; Zheng, S.; Ma, L.; Chen, F.; Xu, T.; Xu, B. Exploring the oral microflora of preschool children. J. Microbiol. 2017, 55, 531–537. [Google Scholar] [CrossRef]
- Tsai, C.-Y.; Tang, C.Y.; Tan, T.-S.; Chen, K.-H.; Liao, K.-H.; Liou, M.-L. Subgingival microbiota in individuals with severe chronic periodontitis. J. Microbiol. Immunol. Infect. 2018, 51, 226–234. [Google Scholar] [CrossRef]
- Zhuang, L.-F.; Watt, R.M.; Steiner, S.; Lang-Hua, B.H.; Wang, R.; Ramseier, C.A.; Lang, N.P. Subgingival microbiota of Sri Lankan tea labourers naïve to oral hygiene measures. J. Clin. Periodontol. 2014, 41, 433–441. [Google Scholar] [CrossRef]
- Fujiwara, N.; Tsuruda, K.; Iwamoto, Y.; Kato, F.; Odaki, T.; Yamane, N.; Hori, Y.; Harashima, Y.; Sakoda, A.; Tagaya, A.; et al. Significant increase of oral bacteria in the early pregnancy period in Japanese women. J. Investig. Clin. Dent. 2017, 8, e12189. [Google Scholar] [CrossRef]
- Brinig, M.M.; Lepp, P.W.; Ouverney, C.C.; Armitage, G.C.; Relman, D.A. Prevalence of Bacteria of Division TM7 in Human Subgingival Plaque and Their Association with Disease. Appl. Environ. Microbiol. 2003, 69, 1687–1694. [Google Scholar] [CrossRef] [PubMed]
- Abusleme, L.; Dupuy, A.K.; Dutzan, N.; Silva, N.; Burleson, J.A.; Strausbaugh, L.D.; Gamonal, J.; Diaz, P.I. The subgingival microbiome in health and periodontitis and its relationship with community biomass and inflammation. ISME J. 2013, 7, 1016–1025. [Google Scholar] [CrossRef] [PubMed]
- Ling, Z.; Liu, X.; Wang, Y.; Li, L.; Xiang, C. Pyrosequencing Analysis of the Salivary Microbiota of Healthy Chinese Children and Adults. Microb. Ecol. 2012, 65, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, Y.; Takeshita, T. The oral microbiome and human health. J. Oral Sci. 2017, 59, 201–206. [Google Scholar] [CrossRef]
- Lira-Junior, R.; Åkerman, S.; Klinge, B.; Bostrom, E.A.; Gustafsson, A. Salivary microbial profiles in relation to age, periodontal, and systemic diseases. PLoS ONE 2018, 13, e0189374. [Google Scholar] [CrossRef]
- Ai, D.; Huang, R.; Wen, J.; Li, C.; Zhu, J.; Xia, L.C. Integrated metagenomic data analysis demonstrates that a loss of diversity in oral microbiota is associated with periodontitis. BMC Genom. 2017, 18, 1041. [Google Scholar] [CrossRef]
- Oliveira, R.; Fermiano, D.; Feres, M.; Figueiredo, L.; Teles, F.; Soares, G.; Faveri, M. Levels of Candidate Periodontal Pathogens in Subgingival Biofilm. J. Dent. Res. 2016, 95, 711–718. [Google Scholar] [CrossRef]
- Velden, U.V.D.; Abbas, F.; Armand, S.; Loos, B.G.; Timmerman, M.F.; Weijden, G.A.V.D.; Winkelhoff, A.J.V.; Winkel, E.G. Java project on periodontal diseases. The natural development of periodontitis: Risk factors, risk predictors and risk determinants. J. Clin. Periodontol. 2006, 33, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Matuliene, G.; Pjetursson, B.E.; Salvi, G.E.; Schmidlin, K.; Brägger, U.; Zwahlen, M.; Lang, N.P. Influence of residual pockets on progression of periodontitis and tooth loss: Results after 11 years of maintenance. J. Clin. Periodontol. 2008, 35, 685–695. [Google Scholar] [CrossRef]
- Maciel, S.S.; Feres, M.; Gonçalves, T.E.D.; Zimmermann, G.S.; Silva, H.D.P.D.; Figueiredo, L.C.; Duarte, P.M. Does obesity influence the subgingival microbiota composition in periodontal health and disease? J. Clin. Periodontol. 2016, 43, 1003–1012. [Google Scholar] [CrossRef]
- Long, J.; Cai, Q.; Steinwandel, M.; Hargreaves, M.K.; Bordenstein, S.R.; Blot, W.J.; Zheng, W.; Shu, X.O. Association of oral microbiome with type 2 diabetes risk. J. Periodontal Res. 2017, 52, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, S.M.; Joshi, V.; Fellows, M.; Dabdoub, S.M.; Nagaraja, H.N.; Odonnell, B.; Deshpande, N.R.; Kumar, P.S. A tale of two risks: Smoking, diabetes and the subgingival microbiome. ISME J. 2017, 11, 2075–2089. [Google Scholar] [CrossRef]
- Kilian, M. The oral microbiome—Friend or foe? Eur. J. Oral Sci. 2018, 126, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Mira, A.; Simon-Soro, A.; Curtis, M.A. Role of microbial communities in the pathogenesis of periodontal diseases and caries. J. Clin. Periodontol. 2017, 44, S23–S38. [Google Scholar] [CrossRef] [PubMed]
- Belstrøm, D.; Sembler-Møller, M.L.; Grande, M.A.; Kirkby, N.; Cotton, S.L.; Paster, B.J.; Holmstrup, P. Microbial profile comparisons of saliva, pooled and site-specific subgingival samples in periodontitis patients. PLoS ONE 2017, 12, e0182992. [Google Scholar] [CrossRef]
- Belstrøm, D.; Holmstrup, P.; Bardow, A.; Kokaras, A.; Fiehn, N.-E.; Paster, B.J. Temporal Stability of the Salivary Microbiota in Oral Health. PLoS ONE 2016, 11, e0147472. [Google Scholar] [CrossRef]
- Hall, M.W.; Singh, N.; Ng, K.F.; Lam, D.K.; Goldberg, M.B.; Tenenbaum, H.C.; Neufeld, J.D.; Beiko, R.G.; Senadheera, D.B. Inter-personal diversity and temporal dynamics of dental, tongue, and salivary microbiota in the healthy oral cavity. NPJ Biofilms Microbiomes 2017, 3, 1–7. [Google Scholar] [CrossRef]
- Ursell, L.K.; Clemente, J.C.; Rideout, J.R.; Gevers, D.; Caporaso, J.G.; Knight, R. The interpersonal and intrapersonal diversity of human-associated microbiota in key body sites. J. Allergy Clin. Immunol. 2012, 129, 1204–1208. [Google Scholar] [CrossRef]
- Darveau, R.P. Periodontitis: A polymicrobial disruption of host homeostasis. Nat. Rev. Microbiol. 2010, 8, 481–490. [Google Scholar] [CrossRef]
- Shi, B.; Chang, M.; Martin, J.; Mitreva, M.; Lux, R.; Klokkevold, P.; Sodergren, E.; Weinstock, G.M.; Haake, S.K.; Li, H. Dynamic Changes in the Subgingival Microbiome and Their Potential for Diagnosis and Prognosis of Periodontitis. MBio 2015, 6, e01926-14. [Google Scholar] [CrossRef]
- Chen, C.; Hemme, C.; Beleno, J.; Shi, Z.J.; Ning, D.; Qin, Y.; Tu, Q.; Jorgensen, M.; He, Z.; Wu, L.; et al. Oral microbiota of periodontal health and disease and their changes after nonsurgical periodontal therapy. ISME J. 2018, 12, 1210–1224. [Google Scholar] [CrossRef] [PubMed]
| Co-variate | Baseline | Follow-Up | p-Value |
|---|---|---|---|
| Age (years) | 18.2 ± 0.4 1 | – | – |
| Sex (Male) | 217 (47.5) 2 | – | – |
| Daily brushing frequency (≥2 times) | 374 (81.8) | 387 (84.7) | 0.249 3 |
| Daily flossing (Yes) | 26 (5.7) | 68 (15.1) | <0.001 3 |
| Regular dental checkup (Yes) | 70 (15.3) | 66 (14.4) | 0.643 3 |
| OHI-S score | 0.6 ± 0.6 | 0.6 ± 0.7 | 0.881 4 |
| BOP (%) | 28.7 ± 24.2 | 31.4 ± 23.0 | 0.040 4 |
| DMFT | 2.3 ± 2.8 | 2.9 ± 2.7 | <0.001 4 |
| BMI (kg/m2) | 20.7 ± 2.8 | 21.0 ± 2.9 | <0.001 4 |
| Community periodontal index (CPI) | |||
| 0 | 50 (10.9) | 26 (5.7) | <0.001 5 |
| 1 | 115 (25.2) | 88 (19.3) | |
| 2 | 223 (48.8) | 128 (28.0) | |
| 3 | 69 (15.1) | 199 (43.5) | |
| 4 | 0 (0.0) | 16 (3.5) | |
| PPD ≥4 mm (Yes) | 69 (15.2) | 215 (47) | <0.001 3 |
| At Baseline | Increase in Gingival Bleeding | Increase in Probing Pocket Depth | ||||
|---|---|---|---|---|---|---|
| Worsening (n = 32) | Non-Worsening (n = 37) | p-Value | Worsening (n = 43) | Non-Worsening (n = 26) | p-Value | |
| Age (years) | 18.2 ± 0.4 1 | 18.2 ± 0.5 | 0.417 3 | 18.2 ±0.5 | 18.2 ± 0.4 | 0.689 3 |
| Sex (Male) | 7 (21.9) 2 | 14 (37.9) | 0.151 4 | 11 (25.6) | 10 (38.5) | 0.260 4 |
| OHI-S score | 0.3 ± 0.4 | 0.7 ± 0.6 | 0.003 3 | 0.6 ± 0.6 | 0.4 ± 0.3 | 0.116 3 |
| BMI (kg/m2) | 19.9 ± 2.7 | 20.2 ± 2.9 | 0.731 3 | 20.3 ± 2.9 | 19.7 ± 2.7 | 0.434 3 |
| BOP (%) | - | - | - | 29.1 ± 23.2 | 25.4 ± 24.2 | 0.532 3 |
| DMFT (number) | 1.6 ± 2.3 | 2.7 ± 3.3 | 0.101 3 | 2.6 ± 3.2 | 1.5 ± 2.3 | 0.103 3 |
| Daily brushing frequency (≥2 times) | 29 (90.6) | 30 (81.1) | 0.261 4 | 36 (83.7) | 23 (88.5) | 0.588 4 |
| Daily flossing (Yes) | 4 (12.5) | 2 (5.4) | 0.296 4 | 5 (11.6) | 1 (3.8) | 0.266 4 |
| Regular dental checkup (Yes) | 8 (25.0) | 9 (24.3) | 0.948 4 | 12 (27.9) | 5 (19.2) | 0.418 4 |
| CPI | ||||||
| 0 | 4 (12.5) | 2 (5.4) | 0.348 4 | 2 (4.7) | 4 (15.4) | 0.186 4 |
| 1 | 7 (21.9) | 9 (24.3) | 10 (23.3) | 6 (23.1) | ||
| 2 | 11 (34.4) | 19 (51.4) | 16 (37.2) | 14 (53.8) | ||
| 3 | 10 (31.3) | 7 (18.9 | 15 (34.9) | 2 (7.7) | ||
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| PPD ≥4 mm (Yes) | 10 (31.3) | 7 (18.9) | 0.236 4 | - | - | - |
| Daily brushing frequency (Increased) | 8 (25.0) | 7 (18.9) | 0.541 4 | 11 (25.6) | 4 (15.4) | 0.319 4 |
| Flossing (Increased) | 1 (3.1) | 10 (27.0) | 0.006 4 | 6 (13.9) | 5 (19.2) | 0.561 4 |
| Regular dental checkup (Increased) | 0 (0.0) | 6 (16.2) | 0.016 4 | 4 (9.3) | 2 (7.7) | 0.818 4 |
| Community I | 20 (46.5) | 23 (53.5) | 0.906 4 | 30 (69.8) | 13 (30.2) | 0.080 4 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Islam, M.M.; Ekuni, D.; Toyama, N.; Kobayashi, T.; Fujimori, K.; Uchida, Y.; Fukuhara, D.; Taniguchi-Tabata, A.; Kataoka, K.; Iwasaki, Y.; et al. Relationship of Salivary Microbiome with the Worsening of the Periodontal Health Status in Young Adults: A 3-Year Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 1764. https://doi.org/10.3390/ijerph17051764
Islam MM, Ekuni D, Toyama N, Kobayashi T, Fujimori K, Uchida Y, Fukuhara D, Taniguchi-Tabata A, Kataoka K, Iwasaki Y, et al. Relationship of Salivary Microbiome with the Worsening of the Periodontal Health Status in Young Adults: A 3-Year Cohort Study. International Journal of Environmental Research and Public Health. 2020; 17(5):1764. https://doi.org/10.3390/ijerph17051764
Chicago/Turabian StyleIslam, Md Monirul, Daisuke Ekuni, Naoki Toyama, Terumasa Kobayashi, Kohei Fujimori, Yoko Uchida, Daiki Fukuhara, Ayano Taniguchi-Tabata, Kota Kataoka, Yoshiaki Iwasaki, and et al. 2020. "Relationship of Salivary Microbiome with the Worsening of the Periodontal Health Status in Young Adults: A 3-Year Cohort Study" International Journal of Environmental Research and Public Health 17, no. 5: 1764. https://doi.org/10.3390/ijerph17051764
APA StyleIslam, M. M., Ekuni, D., Toyama, N., Kobayashi, T., Fujimori, K., Uchida, Y., Fukuhara, D., Taniguchi-Tabata, A., Kataoka, K., Iwasaki, Y., & Morita, M. (2020). Relationship of Salivary Microbiome with the Worsening of the Periodontal Health Status in Young Adults: A 3-Year Cohort Study. International Journal of Environmental Research and Public Health, 17(5), 1764. https://doi.org/10.3390/ijerph17051764






