Effectiveness of Mobile Phone-Based Interventions for Improving Health Outcomes in Patients with Chronic Heart Failure: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
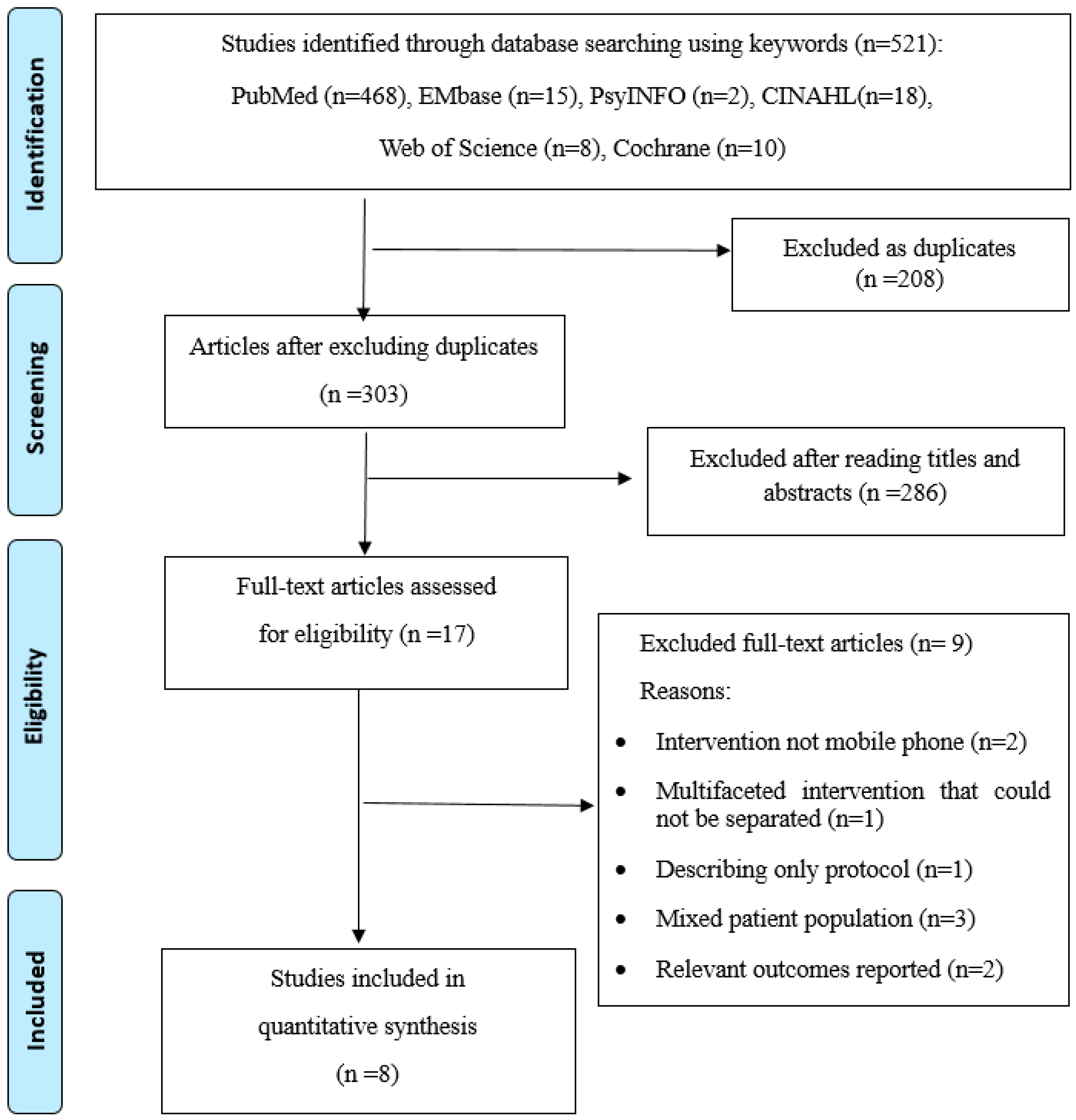
2. Methods
2.1. Search Strategies
2.2. Study Selection
2.3. Data Extraction
2.4. Assessment of Methodological Quality
2.5. Data Synthesis
3. Results
3.1. Study Quality Appraisal
3.2. Study Settings and Patient Characteristics
3.3. Types of Mobile Phone-Based Interventions
3.3.1. Voice Call Interventions
3.3.2. Telemonitoring Interventions
3.3.3. SMS Intervention
3.4. Study Outcomes
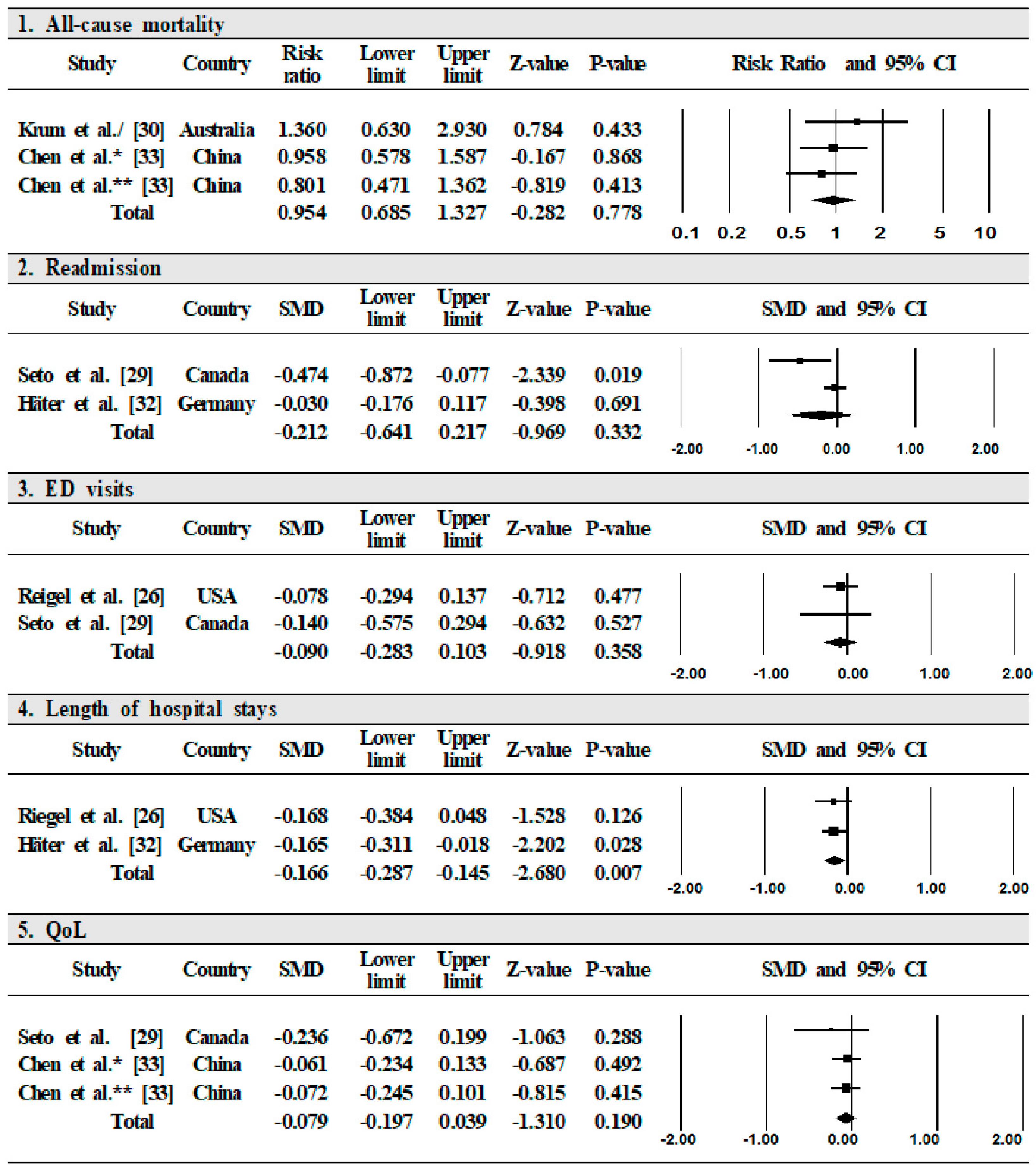
3.4.1. Primary Outcomes Using Meta-Analysis
All-Cause Mortality
Readmission
Emergency Department Visits
Length of Hospital Stays
Quality of Life
3.4.2. Secondary Outcomes Using Systematic Review
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.; Coats, A.J.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [CrossRef]
- Savarese, G.; Lund, L.H. Global public health burden of heart failure. Card. Fail. Rev. 2017, 3, 7–11. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; Howard, V.J.; et al. Heart disease and stroke statistics–2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef]
- Vasan, R.S.; Wilson, P.W.F. Epidemiology and Causes of Heart Failure. Available online: http://www.uptodate.com/contents/epidemiology-and-causes-of-heart-failure (accessed on 20 March 2018).
- Avaldi, V.M.; Lenzi, J.; Castaldini, I.; Urbinati, S.; Di Pasquale, G.; Morini, M.; Protonotari, A.; Maggioni, A.P.; Fantini, M.P. Hospital readmissions of patients with heart failure: The impact of hospital and primary care organizational factors in Northern Italy. PLoS ONE 2015, 10, e0127796. [Google Scholar] [CrossRef]
- Omersa, D.; Farkas, J.; Erzen, I.; Lainscak, M. National trends in heart failure hospitalization rates in Slovenia 2004–2012. Eur. J. Heart Fail. 2016, 18, 1321–1328. [Google Scholar] [CrossRef] [PubMed]
- Guerra, F.; Brambatti, M.; Matassini, M.V.; Capucci, A. Current therapeutic options for heart failure in elderly patients. BioMed Res. Int. 2017, 1483873. [Google Scholar] [CrossRef] [PubMed]
- Khariton, Y.; Hernandez, A.F.; Fonarow, G.C.; Sharma, P.P.; Duffy, C.I.; Thomas, L.; Mi, X.; Albert, N.M.; Butler, J.; McCague, K.; et al. Health status variation across practices in outpatients with heart failure: Insights from the CHAMP-HF (Change the Management of Patients With Heart Failure) registry. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e004668. [Google Scholar] [CrossRef] [PubMed]
- Jaarsma, T.; Cameron, J.; Riegel, B.; Stromberg, A. Factors related to self-care in heart failure patients according to the middle-range theory of self-care of chronic illness: A literature update. Curr. Heart Fail. Rep. 2017, 14, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Nordfonn, O.K.; Morken, I.M.; Bru, L.E.; Husebø, A.M.L. Patients’ experience with heart failure treatment and self-care—A qualitative study exploring the burden of treatment. J. Clin. Nurs. 2019, 28, 1782–1793. [Google Scholar] [CrossRef] [PubMed]
- Ruppar, T.M.; Cooper, P.S.; Johnson, E.D.; Riegel, B. Self-care interventions for adults with heart failure: A systematic review and meta-analysis protocol. J. Adv. Nurs. 2019, 75, 676–682. [Google Scholar] [CrossRef]
- Shao, J.H.; Chen, S.H. Randomized control trial of a self-management intervention for heart failure older adults in Northern Taiwan. Collegian 2019, 26, 288–294. [Google Scholar] [CrossRef]
- Toukhsati, S.R.; Jaarsma, T.; Babu, A.S.; Driscoll, A.; Hare, D.L. Self-care interventions that reduce hospital readmissions in patients with heart failure; towards the identification of change agents. Clin. Med. Insights Cardiol. 2019, 13, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Athilingam, P.; Jenkins, B. Mobile phone apps to support heart failure self-care management: Integrative review. JMIR Cardio 2018, 2, e10057. [Google Scholar] [CrossRef] [PubMed]
- Inglis, S.C.; Du, H.; Himmelfarb, C.D.; Davidson, P.M. mHealth education interventions in heart failure. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Athilingam, P.; Labrador, M.A.; Remo, E.F.J.; Mack, L.; San Juan, A.B.; Elliott, A.F. Features and usability assessment of a patient-centered mobile application (HeartMapp) for self-management of heart failure. Appl. Nurs. Res. 2016, 32, 156–163. [Google Scholar] [CrossRef]
- Wali, S.; Demers, C.; Shah, H.; Wali, H.; Lim, D.; Naik, N.; Ghany, A.; Vispute, A.; Wali, M.; Keshavjee, K. Evaluation of heart failure apps to promote self-care: Systematic app search. JMIR Mhealth Uhealth 2019, 7, e13173. [Google Scholar] [CrossRef]
- Cajita, M.I.; Gleason, K.T.; Han, H.R. A systematic review of mHealth-based heart failure interventions. J. Cardiovasc. Nurs. 2016, 31, E10–E22. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses; the PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Haynes, R.B.; Sacket, D.L.; Guyatt, G.H.; Tugwell, P. Clinical Epidemiology: How Clinical Practice Research, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Carbo, A.; Gupta, M.; Tamariz, L.; Palacio, A.; Levis, S.; Nemeth, Z.; Dang, S. Mobile technologies for managing heart failure: A systematic review and meta-analysis. Telemed. J. E Health 2018, 24, 958–969. [Google Scholar] [CrossRef]
- Nieminen, M.S.; Dickstein, K.; Fonseca, C.; Serrano, J.M.; Parissis, J.; Fedele, F.; Wikström, G.; Agostoni, P.; Atar, S.; Baholli, L.; et al. The patient perspective: Quality of life in advanced heart failure with frequent hospitalization. Int. J. Cardiol. 2015, 191, 256–264. [Google Scholar] [CrossRef]
- Reynolds, K.; Butler, M.G.; Kimes, T.M.; Rosales, A.G.; Chna, W.; Nichols, G.A. Relation of acute heart failure hospital length of stay to subsequent readmission and all-cause mortality. Am. J. Cardiol. 2015, 116, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.P.; Kraus, S.; Mitchell, S.; Perel, P.; Pineiro, D.; Chioncel, O.; Colque, R.; de Boer, R.A.; Gomez-Mesa, J.E.; Grancelli, H.; et al. World Heart Federation roadmap for heart failure. Glob. Heart 2019, 14, 197–214. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Soma, M.; Pulluri, D.; Nemali, N.T.; Brooks, M. The effectiveness of telemedicine in the management of chronic heart disease: A systematic review. JRSM Open 2017, 8, 1–7. [Google Scholar] [CrossRef]
- Riegel, B.; Carlson, B.; Kopp, Z.; LePetri, B.; Glaser, D.; Unger, A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch. Intern. Med. 2002, 162, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Scherr, D.; Kastner, P.; Kollmann, A.; Hallas, A.; Auer, J.; Krappinger, H.; Schuchlenz, H.; Stark, G.; Grander, W.; Jakl, G.; et al. Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: Randomized controlled trial. J. Med. Internet Res. 2009, 11, e34. [Google Scholar] [CrossRef]
- Brandon, A.F.; Schuessler, J.B.; Ellison, K.J.; Lazenby, R.B. The effects of an advanced practice nurse led telephone intervention on outcomes of patients with heart failure. Appl. Nurs. Res. 2009, 22, e1–e7. [Google Scholar] [CrossRef]
- Seto, E.; Leonard, K.J.; Cafazzo, J.A.; Barnsley, J.; Masino, C.; Ross, H.J. Mobile phone-based telemonitoring for heart failure management: A randomized controlled trial. J. Med. Internet Res. 2012, 14, 1–14. [Google Scholar] [CrossRef]
- Krum, H.; Forbes, A.; Yallop, J.; Driscoll, A.; Croucher, J.; Chan, B.; Clark, R.; Davidson, P.; Huynh, L.; Kasper, E.K.; et al. Telephone support to rural and remote patients with heart failure: The Chronic Heart Failure Assessment by Telephone (CHAT) study. Cardiovasc. Ther. 2013, 31, 230–237. [Google Scholar] [CrossRef]
- Goldstein, C.M.; Gathright, E.C.; Dolansky, M.A.; Gunstad, J.; Sterns, A.; Redle, J.D.; Josephson, R.; Hughes, J.W. Randomized controlled feasibility trial of two telemedicine medication reminder systems for older adults with heart failure. J. Telemed. Telecare 2014, 20, 293–299. [Google Scholar] [CrossRef]
- Härter, M.; Dirmaier, J.; Dwinger, S.; Kriston, L.; Herbarth, L.; Siegmund-Schultze, E.; Bermejo, I.; Matschinger, H.; Heider, D.; König, H.H. Effectiveness of telephone-based health coaching for patients with chronic conditions: A randomised controlled trial. PLoS ONE 2016, 11, 1–18. [Google Scholar] [CrossRef]
- Chen, C.; Li, X.; Sun, L.; Cao, S.; Kang, Y.; Hong, L.; Liang, Y.; You, G.; Zhang, Q. Post-discharge short message service improves short-term clinical outcome and self-care behaviour in chronic heart failure. ESC Heart Fail. 2019, 6, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Bashi, N.; Karunanithi, M.; Fatehi, F.; Ding, H.; Walters, D. Remote monitoring of patients with heart failure: An overview of systematic reviews. J. Med. Internet Res. 2017, 19, e18. [Google Scholar] [CrossRef] [PubMed]
- Changizi, M.; Kaveh, M.H. Effectiveness of the mHealth technology in improvement of healthy behaviors in an elderly population-a systematic review. Mhealth 2017, 3, 1–9. [Google Scholar] [CrossRef]
- Piette, J.D.; Striplin, D.; Marinec, N.; Chen, J.; Trivedi, R.B.; Aron, D.C.; Fisher, L.; Aikens, J.E. A Mobile Health Intervention Supporting Heart Failure Patients and Their Informal Caregivers: A Randomized Comparative Effectiveness Trial. J. Med. Internet Res. 2015, 17, e142. [Google Scholar] [CrossRef]
- Kassavou, A.; Sutton, S. Automated telecommunication interventions to promote adherence to cardio-metabolic medications: Meta-analysis of effectiveness and meta-regression of behaviour change techniques. Health Psychol. Rev. 2018, 12, 25–42. [Google Scholar] [CrossRef]
- Posadzki, P.; Mastellos, N.; Ryan, R.; Gunn, L.H.; Felix, L.M.; Pappas, Y.; Gagnon, M.P.; Julious, S.A.; Xiang, L.; Oldenburg, B. Automated telephone communication systems for preventive healthcare and management of long-term conditions. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Plakogiannis, R.; Mola, A.; Sinha, S.; Stefanidis, A.; Oh, H.; Katz, S. Impact of Pharmacy Student–Driven Postdischarge Telephone Calls on Heart Failure Hospital Readmission Rates: A Pilot Program. Hosp. Pharm. 2019, 54, 100–104. [Google Scholar] [CrossRef]
- Reid, R.D.; Pipe, A.L.; Quinlan, B.; Oda, J. Interactive voice response telephony to promote smoking cessation in patients with heart disease: A pilot study. Patient Educ. Couns. 2007, 66, 319–326. [Google Scholar] [CrossRef]
- Tsoli, S.; Sutton, S.; Kassavou, A. Interactive voice response interventions targeting behaviour change: A systematic literature review with meta-analysis and meta-regression. BMJ Open 2018, 8, e018974. [Google Scholar] [CrossRef]
- Melillo, P.; Pecchia, L.; Bracale, M. Interactive voice response system for home telemonitoring of heart failure patients. In Proceedings of the World Congress on Medical Physics and Biomedical Engineering, Munich, Germany, 7–12 September 2009. [Google Scholar]
- Maric, B.; Kaan, A.; Ignaszewski, A.; Lear, S.A. A systematic review of telemonitoring technologies in heart failure. Eur. J. Heart Fail. 2009, 11, 506–517. [Google Scholar] [CrossRef] [PubMed]
- Gurné, O.; Conraads, V.; Missault, L.; Mullens, W.; Vachiery, J.L.; van Mieghem, W.; Droogne, W.; Pouleur, A.C.; Troisfontaine, P.; Huez, S.; et al. A critical review on telemonitoring in heart failure. Acta Cardiol. 2012, 67, 439–444. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yasmin, F.; Banu, B.; Zakir, S.M.; Sauerborn, R.; Ali, L.; Souares, A. Positive influence of short message service and voice call interventions on adherence and health outcomes in case of chronic disease care: A systematic review. BMJ Med. Inform. Decis. Mak. 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Guo, X.; Peng, Z.; Lai, K.H.; Zhao, X. Investigating the Adoption of Mobile Health Services by Elderly Users: Trust Transfer Model and Survey Study. JMIR Mhealth Uhealth 2019, 7, e12269. [Google Scholar] [CrossRef]
- Ruppar, T.M.; Cooper, P.S.; Mehr, D.R.; Delgado, J.M.; Dunbar-Jacob, J.M. Medication Adherence Interventions Improve Heart Failure Mortality and Readmission Rates: Systematic Review and Meta-Analysis of Controlled Trials. J. Am. Heart Assoc. 2016, 5, e002606. [Google Scholar] [CrossRef] [PubMed]
- Dracup, K.; Moser, D.K.; Pelter, M.M.; Nesbitt, T.S.; Southard, J.; Paul, S.M.; Robinson, S.; Cooper, L.S. Randomized, controlled trial to improve self-care in patients with heart failure living in rural areas. Circulation 2014, 130, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Alessa, T.; Abdi, S.; Hawley, M.S.; de Witte, L. Mobile apps to support the self-management of hypertension: Systematic review of effectiveness, usability, and user satisfaction. JMIR Mhealth Uhealth 2018, 6, e10723. [Google Scholar] [CrossRef]
| Authors, (Publication Year)/Location | Participants | Contents of Mobile Technology | Intervention | Outcome Variables | Main Findings (of IG Compared to the CG) | |
|---|---|---|---|---|---|---|
| Intervention Group | Control Group | |||||
| Riegel et al. (2002)/United States [26] | n = 130 | n = 228 | ·Case manager led voice calls, (median 14 voice calls for counseling, monitoring, and a supply of medications) | ·IG: Nurse-led decision-support software program was used for patient education and monitoring. Additionally, printed educational material was mailed to patients monthly. -Initiation of intervention: 5 days after hospital discharge -Intervention length: 6 months ·CG: Usual care | Hospitalization, readmission, hospital days, costs, ED visits | IG scored significantly lower on hospitalization (p = 0.03), readmission (p = 0.03), hospital days (p = 0.01); no significant difference in ED visits. |
| Mean age: 72.5 | Mean age: 74.6 | |||||
| M: 62%, F: 38% | M: 46%, F: 54% | |||||
| NYHA: | NYHA: | |||||
| I–II = 2.4%, | I–II = 3.6%, | |||||
| III–IV = 97.6%, | III–IV = 96.4%, | |||||
| Scherr et al. (2009)/Austria [27] | n = 54 | n = 54 | ·Telemonitoring via mobile phone (blood pressure, heart rate, body weight, and heart failure medication on a daily basis) | ·IG: Patients were asked to measure and record their BP, HR, and body weight on a daily basis, and their dosage of HF medication in their mobile phone. -Initiation of intervention: Prior to discharge. -Intervention length: 6 months. ·CG: Usual care | Survival, NYHA class, LOS | IG showed significantly high survival (p = 0.04), improved NYHA class (p < 0.001), shorter LOS (p = 0.04). |
| Mean age: 64 | Mean age: 65 | |||||
| M: 72%, F: 28% | M: 74%, F: 26% | |||||
| NYHA: | NYHA: | |||||
| I–II = 13% | II = 13% | |||||
| III–IV = 87% | III–IV = 87% | |||||
| Brandon et al. (2009)/United States [28] | n = 10 | n = 10 | ·Nurse-led voice call (5~30 min, weekly for 2 weeks, and every 2 weeks for the following 10 weeks) for patient education and support | ·IG: Nurse-led telephone-enhanced disease management -Initiation of intervention: after enrollment at inpatient and outpatient settings -Intervention length: 10 weeks ·CG: Usual care | Readmission, QoL, self-care behaviors | IG had significantly greater self-care behaviors (p < 0.001); no significant difference in readmission, QoL. |
| Mean age: 60 | Mean age: 60 | |||||
| M: 30%, F: 70% | M: 60%, F: 40% | |||||
| NYHA: | NYHA: | |||||
| I–II = 70%, | I–II = 80%, | |||||
| III–IV = 30% | III–IV = 20% | |||||
| Seto et al. (2012)/Canada [29] | n = 50 | n = 50 | ·Telemonitoring via Bluetooth to a mobile phone (daily morning weight, blood pressure readings, as well as single-lead ECGs) ·Voice call for answering daily morning symptoms. | ·IG: Telemonitoring system (daily morning weight and blood pressure readings and weekly single-lead ECGs). Technical support provided by telephone throughout the study. -Initiation of intervention: after enrollment at the outpatient clinic. -Intervention length: 6 months ·CG: Standard care | Readmission, mortality, QoL, self-care behaviors, BNP, LVEF, ED visits | IG had significantly greater QoL (p = 0.05); no significant difference in readmission, mortality, self-care behaviors, BNP, LVEF, and ED visits. |
| Mean age: 55.1 | Mean age: 52.3 | |||||
| M: 82%, F: 18% | M: 76%, F: 24% | |||||
| NYHA: | NYHA: | |||||
| I–II = 42%, | I–II = 44% | |||||
| III–IV = 58% | III–IV = 56% | |||||
| Krum et al. (2013)/Australia [30] | n = 188 | n = 217 | ·Voice call for answering monthly HF clinical status, medical management status, social status, and receiving advice | ·IG: Patients were asked to voice call at least monthly and answer questions about the heart failure clinical status, medical management status, and social status. Additionally, patients were able at any time to dial and receive advice about management of heart failure. -Initiation of intervention: After enrollment at outpatient clinic. -Intervention length: 12 months ·CG: Individualized patient diary | All-cause mortality, hospitalization | IG had significantly less frequent hospitalization (p = 0.006); no significant difference in mortality. |
| Mean age: 73 | Mean age: 73 | |||||
| M: 62%, F: 38% | M: 64%, F: 36% | |||||
| NYHA: | NYHA: | |||||
| I–II = 58%, | II = 60%, | |||||
| III–IV = 42% | III–IV = 40% | |||||
| Goldstein et al. (2014)/United States [31] | n = 28 | n = 30 | ·Reminders (for medication taken on a daily basis) via mobile phone ·Providing information of medication via mobile phone | ·IG: Medication adherence app -Initiation of intervention: Unspecified -Intervention length: 1 month ·CG: Patients were asked to use an electronic pillbox to remind them to take medication | Medication adherence | No significant difference in medication adherence. |
| Mean age: 69 | Mean age: 69.6 | |||||
| M: 68%, F: 32% | M: 63%, F: 37% | |||||
| NYHA: none | NYHA: none | |||||
| Härter et al. (2016)/Germany [32] | n = 364 | n = 354 | ·Health coach-led voice call (every 6 weeks for 24 months) for counseling, monitoring, and support | ·IG: Telephone-based health coaching -Initiation of intervention: unspecified -Intervention length: 24 months ·CG: Usual care | Readmission, hospital days, medication adherence | IG showed significantly lower readmission (p = 0.012). No significant difference in hospital days, medication adherence. |
| Mean age: 70.6 | Mean age: 71.0 | |||||
| NYHA: none | NYHA: none | |||||
| Chen et al. (2019)/China [33] | Intervention 1 (SMS) | IG1: Sending text message via mobile phone (weekly for 1 month) for patient education and medication reminder (taking medicine, weighing) IG2: Voice call (once for 1 month) for patient education and counseling | IG1: Educational and reminder text message -Initiation of intervention: within 10 days after hospital discharge -Intervention length: 1 month IG2: Nurse-led voice call -Initiation of intervention: within 30 days after hospital discharge -Intervention length: 1 month ·CG: Standard care | All-cause mortality, hospitalization, QoL, self-care behaviors | No significant difference in mortality, QoL, self-care behaviors | |
| n = 252 | n = 260 | |||||
| Mean age: 60 | Mean age: 61 | |||||
| M: 58%, F: 42% | M: 57.3%, F: 42.7% | |||||
| NYHA: | NYHA: | |||||
| I–II = 30.6%, | I–II = 33.8%, | |||||
| III–IV = 69.4% | III–IV = 66.2% | |||||
| Intervention 2 (STS) | ||||||
| n = 255 | ||||||
| Mean age: 62 | ||||||
| M: 55%, F: 45% | ||||||
| NYHA: | ||||||
| I–II = 30.2%, | ||||||
| III–IV = 69.8% | ||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Son, Y.-J.; Lee, Y.; Lee, H.-J. Effectiveness of Mobile Phone-Based Interventions for Improving Health Outcomes in Patients with Chronic Heart Failure: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 1749. https://doi.org/10.3390/ijerph17051749
Son Y-J, Lee Y, Lee H-J. Effectiveness of Mobile Phone-Based Interventions for Improving Health Outcomes in Patients with Chronic Heart Failure: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(5):1749. https://doi.org/10.3390/ijerph17051749
Chicago/Turabian StyleSon, Youn-Jung, Yaelim Lee, and Hyeon-Ju Lee. 2020. "Effectiveness of Mobile Phone-Based Interventions for Improving Health Outcomes in Patients with Chronic Heart Failure: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 5: 1749. https://doi.org/10.3390/ijerph17051749
APA StyleSon, Y.-J., Lee, Y., & Lee, H.-J. (2020). Effectiveness of Mobile Phone-Based Interventions for Improving Health Outcomes in Patients with Chronic Heart Failure: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(5), 1749. https://doi.org/10.3390/ijerph17051749





