Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
3. Results
3.1. Internal Consistency
3.2. Convergent Validity
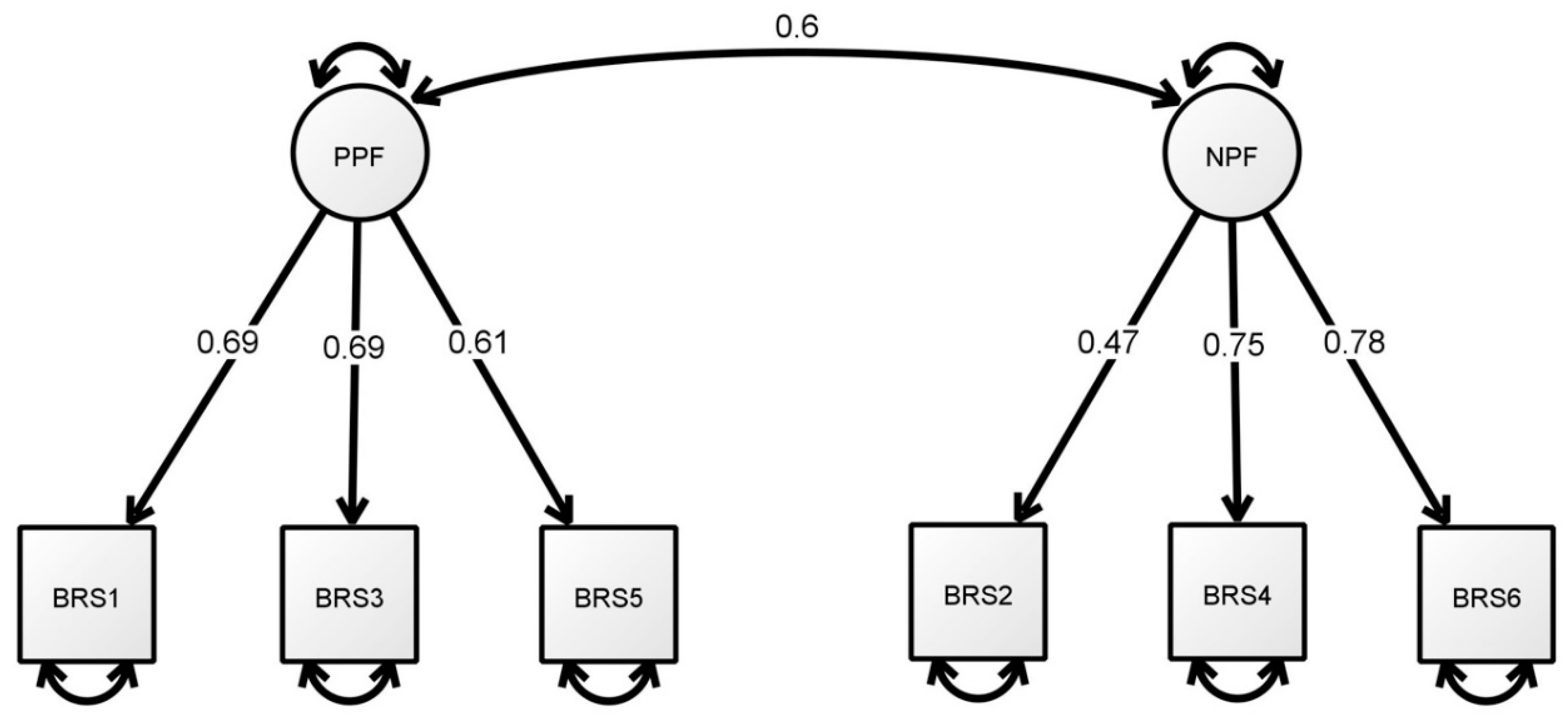
3.3. Factorial Structure
4. Discussion
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- Luthar, S.S.; Cicchetti, D.; Becker, B. The construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 2000, 71, 543–562. [Google Scholar] [CrossRef]
- Sinclair, V.G.; Wallston, K.A. The Development and Psychometric Evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef]
- Carver, C.S. Resilience and Thriving: Issues, Models, and Linkages. J. Soc. Issues 1998, 54, 245–266. [Google Scholar] [CrossRef]
- Richardson, G.E. The metatheory of resilience and resiliency. J. Clin. Psychol. 2002, 58, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Polk, L.V. Toward a middle-range theory of resilience. Adv. Nurs. Sci. 1997, 19, 1–13. [Google Scholar] [CrossRef]
- Rutter, M. Resilience in the face of adversity-protective factors and resistance to psychiatric-disorder. Br. J. Psychiatry 1985, 147, 598–611. [Google Scholar] [CrossRef]
- Rutter, M. Psychosocial resilience and protective mechanisms. Am. J. Orthopsychiatry 1987, 57, 316–331. [Google Scholar] [CrossRef] [PubMed]
- Kobasa, S.C. Stressful life events, personality, and health-inquiry into hardiness. J. Personal. Soc. Psychol. 1979, 37, 1–11. [Google Scholar] [CrossRef]
- Liu, L.; Xu, X.; Xu, N.; Wang, L. Disease activity, resilience and health-related quality of life in Chinese patients with rheumatoid arthritis: A multi-center, cross-sectional study. Health Qual. Life Outcomes 2017, 15, 149. [Google Scholar] [CrossRef]
- Li, M.-Y.; Yang, Y.-L.; Liu, L.; Wang, L. Effects of social support, hope and resilience on quality of life among Chinese bladder cancer patients: A cross-sectional study. Health Qual. Life Outcomes 2016, 14, 73. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Salisu, I.; Hashim, N. A Critical Review of Scales Used in Resilience Research. IOSR J. Bus. Manag. 2017, 19, 23–33. [Google Scholar] [CrossRef]
- Windle, G.; Bennett, K.M.; Noyes, J. A methodological review of resilience measurement scales. Health Qual. Life Outcomes 2011, 9, 8. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef]
- Bromley, E.; Johnson, J.G.; Cohen, P. Personality strengths in adolescence and decreased risk of developing mental health problems in early adulthood. Compr. Psychiatry 2006, 47, 317–326. [Google Scholar] [CrossRef]
- Coelho, G.L.D.; Hanel, P.H.P.; Cavalcanti, T.M.; Rezende, A.T.; Gouveia, V.V. Brief Resilience Scale: Testing its factorial structure and invariance in Brazil. Univ. Psychol. 2016, 15, 12. [Google Scholar]
- Kunzler, A.M.; Chmitorz, A.; Bagusat, C.; Kaluza, A.J.; Hoffmann, I.; Schafer, M.; Quiring, O.; Rigotti, T.; Kalisch, R.; Tuscher, O.; et al. Construct Validity and Population-Based Norms of the German Brief Resilience Scale (BRS). Eur. J. Health Psychol. 2018, 25, 107–117. [Google Scholar] [CrossRef]
- Chmitorz, A.; Wenzel, M.; Stieglitz, R.D.; Kunzler, A.; Bagusat, C.; Helmreich, I.; Gerlicher, A.; Kampa, M.; Kubiak, T.; Kalisch, R.; et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE 2018, 13, e0192761. [Google Scholar] [CrossRef]
- Rodriguez-Rey, R.; Alonso-Tapia, J.; Hernansaiz-Garrido, H. Reliability and Validity of the Brief Resilience Scale (BRS) Spanish Version. Psychol. Assess. 2016, 28, E101–E110. [Google Scholar] [CrossRef]
- Soer, R.; Dijkstra, M.; Bieleman, H.; Stewart, R.E.; Reneman, M.F.; Oosterveld, F.G.J.; Schreurs, K.M.G. Measurement properties and implications of the Brief Resilience Scale in healthy workers. J. Occup. Health 2019, 61, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Rasmussen, C.A.; Gonzalez-Betanzos, F. The Treatment of Acquiescence and the Factorial Structure of the Brief Resilience Scale (BRS) in Mexican and Chilean University Students. An. Psicol. 2019, 35, 26–32. [Google Scholar] [CrossRef]
- Dixon, B.G.; Corridoni, G.; Smith, B.W. Examination of construct validity of the brief resilience scale in a mixed cancer group. Pscyho-Oncology 2015, 24, 100. [Google Scholar]
- Tansey, T.N.; Kaya, C.; Moser, E.; Eagle, D.; Dutta, A.; Chan, F. Psychometric Validation of the Brief Resilience Scale in a Sample of Vocational Rehabilitation Consumers. Rehabil. Couns. Bull. 2016, 59, 108–111. [Google Scholar] [CrossRef]
- Limonero, J.T.; Tomas-Sabado, J.; Gomez-Romero, M.J.; Mate-Mendez, J.; Sinclair, V.G.; Wallston, K.A.; Gomez-Benito, J. Evidence for Validity of the Brief Resilient Coping Scale in a Young Spanish Sample. Span. J. Psychol. 2014, 17, 9. [Google Scholar] [CrossRef]
- Kocalevent, R.D.; Zenger, M.; Hinz, A.; Klapp, B.; Brahler, E. Resilient coping in the general population: Standardization of the brief resilient coping scale (BRCS). Health Qual. Life Outcomes 2017, 15, 8. [Google Scholar] [CrossRef]
- Lopez-Pina, J.A.; Meseguer-Henarejos, A.B.; Gascon-Canovas, J.J.; Navarro-Villalba, D.J.; Sinclair, V.G.; Wallston, K.A. Measurement properties of the brief resilient coping scale in patients with systemic lupus erythematosus using rasch analysis. Health Qual. Life Outcomes 2016, 14, 8. [Google Scholar] [CrossRef]
- Brislin, R.W. Back-Translation for Cross-Cultural Research. J. Cross-Cult. Psychol. 1970, 1, 185–216. [Google Scholar] [CrossRef]
- Cha, E.S.; Kim, K.H.; Erlen, J.A. Translation of scales in cross-cultural research: Issues and techniques. J. Adv. Nurs. 2007, 58, 386–395. [Google Scholar] [CrossRef]
- Chang, A.M.; Chau, J.P.C.; Holroyd, E. Translation of questionnaires and issues of equivalence. J. Adv. Nurs. 1999, 29, 316–322. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Hair, J.F. Multivariate Data Analysis, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Tabachnick, B.G. Using Multivariate Statistics, 6th ed.; Pearson Education: Boston, MA, USA, 2013. [Google Scholar]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Pavot, W.; Diener, E. Review of the Satisfaction with Life Scale. Psychol. Assess. 1993, 5, 164–172. [Google Scholar] [CrossRef]
- Pavot, W.; Diener, E. The Satisfaction with Life Scale and the emerging construct of life satisfaction. J. Posit. Psychol. 2008, 3, 137–152. [Google Scholar] [CrossRef]
- Pavot, W.; Diener, E.; Colvin, C.R.; Sandvik, E. Further validation of the Satisfaction with Life Scale: Evidence for the cross-method convergence of well-being measures. J. Personal. Assess. 1991, 57, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Bech, P. Measuring the dimensions of psychological general well-being by the WHO-5. Qual. Life Newsl. 2004, 32, 15–16. [Google Scholar]
- Bech, P. Clinical Psychometrics, 1st ed.; Wiley-Blackwell: Chichester, UK, 2012. [Google Scholar]
- Bech, P.; Olsen, L.R.; Kjoller, M.; Rasmussen, N.K. Measuring well-being rather than the absence of distress symptoms: A comparison of the SF-36 Mental Health subscale and the WHO-Five Well-Being Scale. Int. J. Methods Psychiatr. Res. 2003, 12, 85–91. [Google Scholar] [CrossRef]
- Scheier, M.F.; Carver, C.S. Effects of optimism on psychological and physical well-being-theoretical overview and empirical update. Cogn. Ther. Res. 1992, 16, 201–228. [Google Scholar] [CrossRef]
- Vautier, S.; Raufaste, E.; Cariou, M. Dimensionality of the Revised Life Orientation Test and the status of filler items. Int. J. Psychol. 2003, 38, 390–400. [Google Scholar] [CrossRef]
- Zeng, W.N.; Gu, M.X. Relationship between mindfulness and positive affect of chinese older adults: Optimism as mediator. Soc. Behav. Personal. 2017, 45, 155–162. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy mechanism in human agency. Am. Psychol. 1982, 37, 122–147. [Google Scholar] [CrossRef]
- Schwarzer, R.; Bäßler, J.; Kwiatek, P.; Schröder, K.; Zhang, J.X. The Assessment of Optimistic Self-beliefs: Comparison of the German, Spanish, and Chinese Versions of the General Self-efficacy Scale. Appl. Psychol. 1997, 46, 69–88. [Google Scholar] [CrossRef]
- Scholz, U.; Dona, B.G.; Sud, S.; Schwarzer, R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur. J. Psychol. Assess. 2002, 18, 242–251. [Google Scholar] [CrossRef]
- Rosenberg, M.; Schooler, C.; Schoenbach, C. Self-Esteem and Adolescent Problems: Modeling Reciprocal Effects. Am. Sociol. Rev. 1989, 54, 1004–1018. [Google Scholar] [CrossRef]
- Wu, Y.; Zuo, B.; Wen, F.F.; Yan, L. Rosenberg Self-Esteem Scale: Method Effects, Factorial Structure and Scale Invariance across Migrant Child and Urban Child Populations in China. J. Personal. Assess. 2017, 99, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Stewart-Brown, S.; Tennant, A.; Tennant, R.; Platt, S.; Parkinson, J.; Weich, S. Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): A Rasch analysis using data from the Scottish Health Education Population Survey. Health Qual. Life Outcomes 2009, 7, 15. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Fung, S. Psychometric Evaluation of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) with Chinese University Students. Health Qual. Life Outcomes 2019, 17, 46. [Google Scholar] [CrossRef]
- Crawford, J.R.; Henry, J.D. The positive and negative affect schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2004, 43, 245–265. [Google Scholar] [CrossRef]
- Thompson, E.R. Development and validation of an internationally reliable short-form of the positive and negative affect schedule (Panas). J. Cross-Cult. Psychol. 2007, 38, 227–242. [Google Scholar] [CrossRef]
- Liang, Y.; Zhu, D.M. Subjective Well-Being of Chinese Landless Peasants in Relatively Developed Regions: Measurement Using PANAS and SWLS. Soc. Indic. Res. 2015, 123, 817–835. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Williams, P. A User’s Guide to the General Health Questionnair; NFER-NELSON: Windsor, UK, 1988. [Google Scholar]
- Liang, Y.; Wang, L.; Yin, X.C. The factor structure of the 12-item general health questionnaire (GHQ-12) in young Chinese civil servants. Health Qual. Life Outcomes 2016, 14, 9. [Google Scholar] [CrossRef] [PubMed]
- Ye, S.Q. Factor structure of the General Health Questionnaire (GHQ-12): The role of wording effects. Personal. Individ. Differ. 2009, 46, 197–201. [Google Scholar] [CrossRef]
- Field, A.P. Discovering Statistics using IBM SPSS Statistics, 5th ed.; SAGE Publications: Los Angeles, CA, USA, 2018. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guilford Publications: New York, NY, USA, 2014. [Google Scholar]
- Jöreskog, K.G. A general approach to confirmatory maximum likelihood factor analysis. Psychometrika 1969, 34, 183–202. [Google Scholar] [CrossRef]
- Loewenthal, K.M. An Introduction to Psychological Tests and Scales, 2nd ed.; Psychology Press: Philadelphia, PA, USA, 2001. [Google Scholar]
- DiStefano, C.; Morgan, G.B. A Comparison of Diagonal Weighted Least Squares Robust Estimation Techniques for Ordinal Data. Struct. Equ. Model. Multidiscip. J. 2014, 21, 425–438. [Google Scholar] [CrossRef]
- Li, C.-H. Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav. Res. Methods 2016, 48, 936–949. [Google Scholar] [CrossRef]
- Lionetti, F.; Keijsers, L.; Dellagiulia, A.; Pastore, M. Evidence of factorial validity of parental knowledge, control and solicitation, and adolescent disclosure scales: When the ordered nature of Likert scales matters. Front. Psychol. 2016, 7, 941. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting Structural Equation Modeling and Confirmatory Factor Analysis Results: A Review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with LISREL, PRELIS, and SIMPLIS: Basic Concepts, Applications, and Programming; L. Erlbaum Associates: Mahwah, NJ, USA, 1998. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 2nd ed.; Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Satorra, A.; Bentler, P.M. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika 2001, 66, 507–514. [Google Scholar] [CrossRef]
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 36. [Google Scholar] [CrossRef]
| Item | M | SD | sk | ku | rit | aiid |
|---|---|---|---|---|---|---|
| BRS (a = 0.71) | ||||||
| 1. I tend to bounce back quickly after hard times | 3.21 | 0.87 | −0.34 | 0.30 | 0.44 | 0.67 |
| 2. I have a hard time making it through stressful events (R) | 3.34 | 0.93 | −0.35 | −0.09 | 0.33 | 0.71 |
| 3. It does not take me long to recover from a stressful event | 3.15 | 0.85 | −0.16 | 0.09 | 0.44 | 0.67 |
| 4. It is hard for me to snap back when something bad happens (R) | 3.38 | 0.91 | −0.45 | 0.06 | 0.50 | 0.65 |
| 5. I usually come through difficult times with little trouble | 3.51 | 0.76 | −0.27 | 0.39 | 0.41 | 0.68 |
| 6. I tend to take a long time to get over set−backs in my life (R) | 3.25 | 0.86 | −0.37 | 0.18 | 0.53 | 0.64 |
| Total score | 19.85 | 3.31 | −0.52 | 0.58 | ||
| BRCS (a = 0.59) | ||||||
| 1. I look for creative ways to alter difficult situations | 3.10 | 0.79 | −0.27 | 0.49 | 0.36 | 0.53 |
| 2. Regardless of what happens to me, I believe I can control my reaction to it | 3.27 | 0.83 | −0.08 | 0.16 | 0.40 | 0.50 |
| 3. I believe that I can grow in positive ways by dealing with difficult situations | 3.59 | 0.82 | −0.47 | 0.43 | 0.42 | 0.48 |
| 4. I actively look for ways to replace the losses I encounter in life | 3.33 | 0.83 | −0.21 | 0.18 | 0.31 | 0.57 |
| Total score | 13.29 | 2.19 | −0.98 | 0.59 |
| Scale | BRS r | BRCS r |
|---|---|---|
| Satisfaction with Life Scale (SWLS) | 0.23 *** | 0.35 *** |
| WHO (Five) Well-being Index (WHO-5) | 0.30 *** | 0.29 *** |
| Revised Life Orientation Test (LOT-R) | 0.30 *** | 0.39 *** |
| Rosenberg Self-esteem (RSE) Scale | 0.44 *** | 0.34 *** |
| General Self-efficacy Scale (GSE) | 0.29 *** | 0.42 *** |
| Short Warwick Edinburgh Mental Well-being Scale (SWEMWBS) | 0.45 *** | 0.44 *** |
| Positive affect–PANAS | 0.26 *** | 0.40 *** |
| 12-item General Health Questionnaire (GHQ-12) | −0.50 *** | −0.33 *** |
| Negative affect–PANAS | −0.41 *** | −0.13 ** |
| Model | χ2 | df | χ2/df | RMSEA (90% CI) | CFI | TLI | SRMR |
|---|---|---|---|---|---|---|---|
| BRS | |||||||
| 1 | 120.680 | 9 | 13.41 | 0.156 (0.132–0.181) | 0.936 | 0.893 | 0.082 |
| 2 a | 11.787 | 6 | 1.96 | 0.043 (0.000–0.080) | 0.997 | 0.992 | 0.028 |
| 3 | 13.681 | 8 | 1.71 | 0.037 (0.000–0.070) | 0.997 | 0.994 | 0.030 |
| BRCS | |||||||
| 4 | 17.538 | 2 | 8.77 | 0.123 (0.075–0.179) | 0.965 | 0.896 | 0.050 |
| 5 b | 0.807 | 1 | 0.81 | 0.000 (0.000–0.112) | 0.999 | 0.999 | 0.011 |
| Acceptable cut-off value | <3 | <0.06 | >0.95 | >0.95 | <0.08 |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fung, S.-f. Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample. Int. J. Environ. Res. Public Health 2020, 17, 1265. https://doi.org/10.3390/ijerph17041265
Fung S-f. Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample. International Journal of Environmental Research and Public Health. 2020; 17(4):1265. https://doi.org/10.3390/ijerph17041265
Chicago/Turabian StyleFung, Sai-fu. 2020. "Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample" International Journal of Environmental Research and Public Health 17, no. 4: 1265. https://doi.org/10.3390/ijerph17041265
APA StyleFung, S.-f. (2020). Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample. International Journal of Environmental Research and Public Health, 17(4), 1265. https://doi.org/10.3390/ijerph17041265





