Factors Associated with Maternal Deaths in a Hard-To-Reach Marginalized Rural Community of Bangladesh: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Site
2.2. Data Collection Tools
2.3. Training of the Field-Level Health Workers
2.4. Death Notification
2.5. Verbal Autopsy
2.6. In-Depth Case Studies
2.7. Monitoring and Quality Assurance
2.8. Cause Assignment of Verbal Autopsy
2.9. Data Analysis
2.10. Ethical Approval
3. Results
3.1. Maternal Death Data Captured and Reported
3.2. Demographic Characteristics of the Deceased
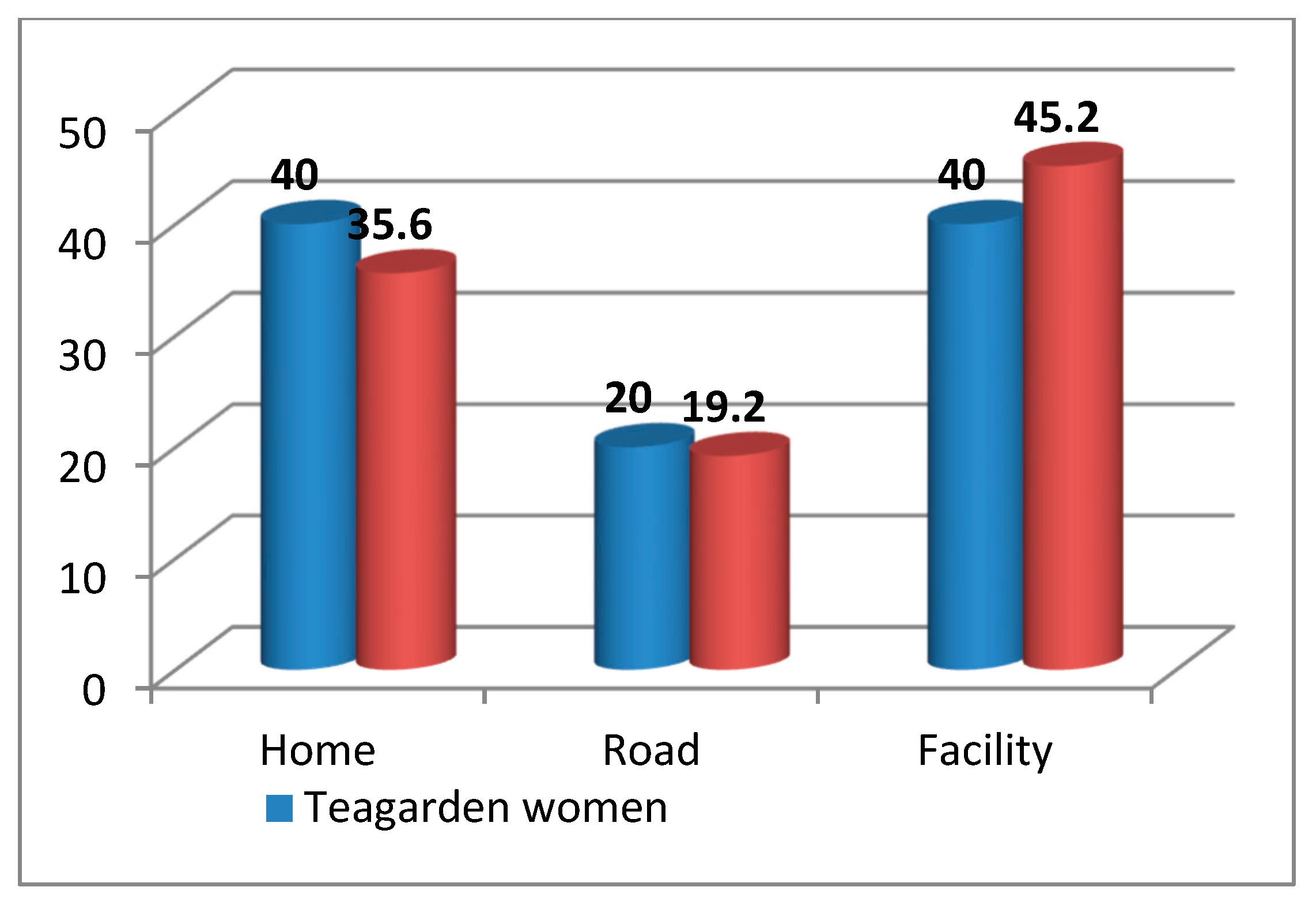
3.3. Place of Death of Women
3.4. Place of Delivery and Birth Attendant during Delivery
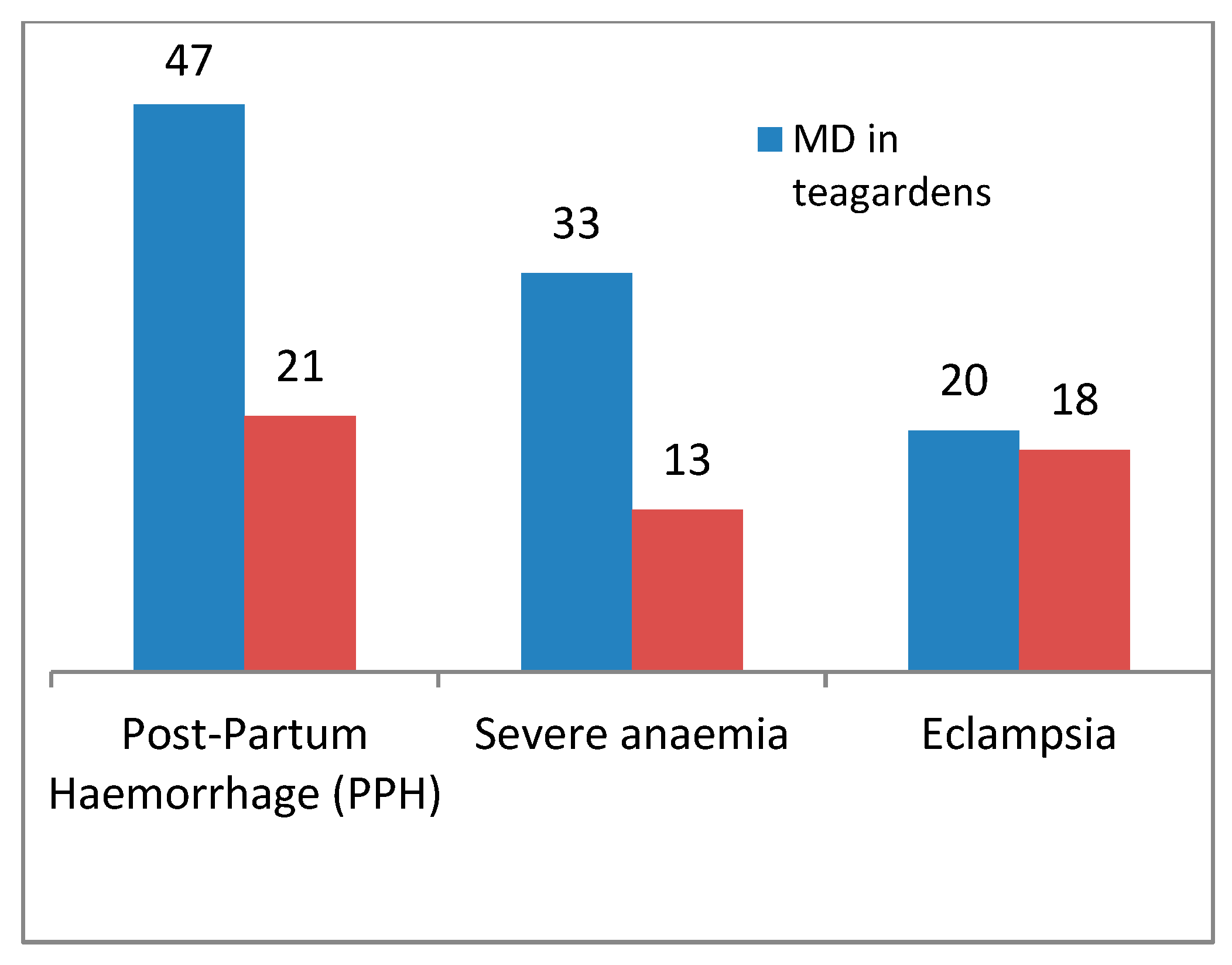
3.5. Causes of Maternal Deaths
3.6. Decision and Transportation Delay among the Deaths in Tea Gardens
3.7. Findings from the Case Studies of Maternal Deaths in the Tea Gardens
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| FWA | family welfare assistant |
| HA | health assistants |
| MPDR | Maternal and Perinatal Death Review |
| MPDSR | Maternal and Perinatal Death Surveillance and Responses |
| MoH and FW | Ministry of Health and Family Welfare |
| PPH | post-partum hemorrhage |
| QI | quality improvement |
| SDG | sustainable development goal |
| TBA | Traditional birth attendant |
References
- GBD 2015 Maternal Mortality Collaborators. Global, regional, and national levels of maternal mortality, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1775–1812. [Google Scholar] [CrossRef]
- Alkema, L.; Chou, D.; Hogan, D.; Zhang, S.; Moller, A.B.; Gemmill, A.; Fat, D.M.; Boerma, T.; Temmerman, M.; Mathers, C.; et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016, 387, 462–474. [Google Scholar] [CrossRef]
- National Institute of Population Research and Training (NIPORT). Bangladesh Demographic and Health Survey. 2014. BDHS. 2016. Available online: http://www.niport.gov.bd (accessed on 29 November 2019).
- National Institute of Population Research and Training (NIPORT); MEASURE Evaluation; Icddrb. Bangladesh Maternal Mortality and Health Care Survey 2010; NIPORT: Dhaka, Bangladesh, 2012; Available online: https://www.measureevaluation.org/resources/publications/tr-12-87 (accessed on 29 November 2019).
- Sample Vital Registration System (SVRS). Bangladesh Sample Vital Statistics Report 2017. Available online: http://bbs.portal.gov.bd/sites/default/files/files/bbs.portal.gov.bd/page/a1d32f13_8553_44f1_92e6_8ff80a4ff82e/Bangladesh%20%20Statistics-2017.pdf (accessed on 29 November 2019).
- El Arifeen, S.; Hill, K.; Ahsan, K.Z.; Jamil, K.; Nahar, Q.; Streatfield, P.K. Maternal mortality in Bangladesh: A Countdown to 2015 country case study. Lancet 2014, 384, 1366–1374. [Google Scholar] [CrossRef]
- National Institute of Population Research and Training (NIPORT). Bangladesh Demographic and Health Survey 2017–2018. Bangladesh. 2019. Available online: https://www.dhsprogram.com/pubs/pdf/PR104/PR104.pdf (accessed on 29 November 2019).
- Biswas, A.; Rahman, F.; Eriksson, C.; Dalal, K. Community Notification of Maternal, Neonatal Deaths and Still Births in Maternal and Neonatal Death Review (MNDR) System: Experiences in Bangladesh. Health 2014, 6, 2218–2226. [Google Scholar] [CrossRef][Green Version]
- Biswas, A.; Rahman, F.; Halim, A.; Eriksson, C.; Dalal, K. Maternal and Neonatal Death Review (MNDR): A Useful Approach to Identifying Appropriate and Effective Maternal and Neonatal Health Initiatives in Bangladesh. Health 2014, 6, 1669–1679. [Google Scholar] [CrossRef][Green Version]
- Halim, A.; Utz, B.; Biswas, A.; Rahman, F.; van den Broek, N. Cause of and contributing factors to maternal deaths. BJOG 2014, 121 (Suppl. 4), 86–94. [Google Scholar] [CrossRef] [PubMed]
- Biswas, A.; Rahman, F.; Halim, A.; Eriksson, C.; Dalal, K. Experiences of Community Verbal Autopsy in Maternal and Newborn Health of Bangladesh. HealthMed 2015, 9, 329–338. [Google Scholar]
- Banglapedia. Moulvibazar District. 2015. Available online: http://en.banglapedia.org/index.php?title=Maulvibazar_District (accessed on 5 March 2015).
- Gain, P. Slaves in These Times:Tea Communities of Bangladesh; Society for Health Extension and Development (SHED): Dhaka, Bangladesh, 2016; Available online: https://www.sehd.org/publications/tea-workers/121-slavesinthesetimes (accessed on 29 November 2019).
- Halim, A.; Biswas, A.; Abdullah ASMHalim, A.; Biswas, B.; Abdullah, A.S.M. Report on Baseline Survey of teagardens in Bangladesh 2016. CIPRB. Available online: https://www.researchgate.net/publication/327882331_Report_on_Baseline_Survey_of_teagardens_in_Bangladesh (accessed on 29 November 2019).
- International Labour Organization (ILO). A Study Report on Working Conditions of Tea Plantation Workers in Bangladesh. 2016. Available online: https://www.ilo.org/wcmsp5/groups/public/---asia/---ro-bangkok/---ilo-dhaka/documents/publication/wcms_563692.pdf (accessed on 29 November 2019).
- The Daily Star. Midwifery-Led Maternal Health. 2015. Available online: http://www.thedailystar.net/round-tables/midwifery-led-maternal-health-88339 (accessed on 28 June 2015).
- National Institute of Population Research and Training; International Centre for Diarrhoeal Disease Research, Bangladesh; MEASURE Evaluation. Bangladesh Maternal Mortality and Health Care Survey 2016: Preliminary Results. 2016. Available online: https://www.measureevaluation.org/resources/publications/tr-17-218 (accessed on 29 November 2019).
- Biswas, A.; Dalal, K.; Abdullah, A.S.M.; Gifford, M.; Halim, M. Maternal complications in a geographically challenging and hard to reach district of Bangladesh: A qualitative study. F1000Research 2016, 5, 2417. [Google Scholar] [CrossRef] [PubMed]
- Biswas, A.; Abdullah, A.; Ferdoush, J.; Doraisyami, S.; Halim, M.A. What’s Need for Maternal and Neonatal Health Service Delivery in the Marginalized Tea Garden Community of Bangladesh?—A Qualitative Study. Integr. J. Glob. Health 2018, 2. [Google Scholar] [CrossRef]
- Biswas, A.; Anderson, R.; Doraiswamy, S.; Abdullah, A.S.M.; Purno, N.; Rahman, F.; Halim, A. Timely referral saves the lives of mothers and newborns: Midwifery led continuum of care in marginalized tea garden communities—A qualitative case study in Bangladesh. F1000Research 2018, 7, 365. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A.S.M.; Hossian, M.S.; Rahman, F.; Halim, A.; Biswas, A. Community Delay in Decision Making and Transferring Complicated Mothers at Facilities Caused Maternal Deaths: A Qualitative Study in Rural Bangladesh. Integr. J. Glob. Health 2017, 1, 15. [Google Scholar]
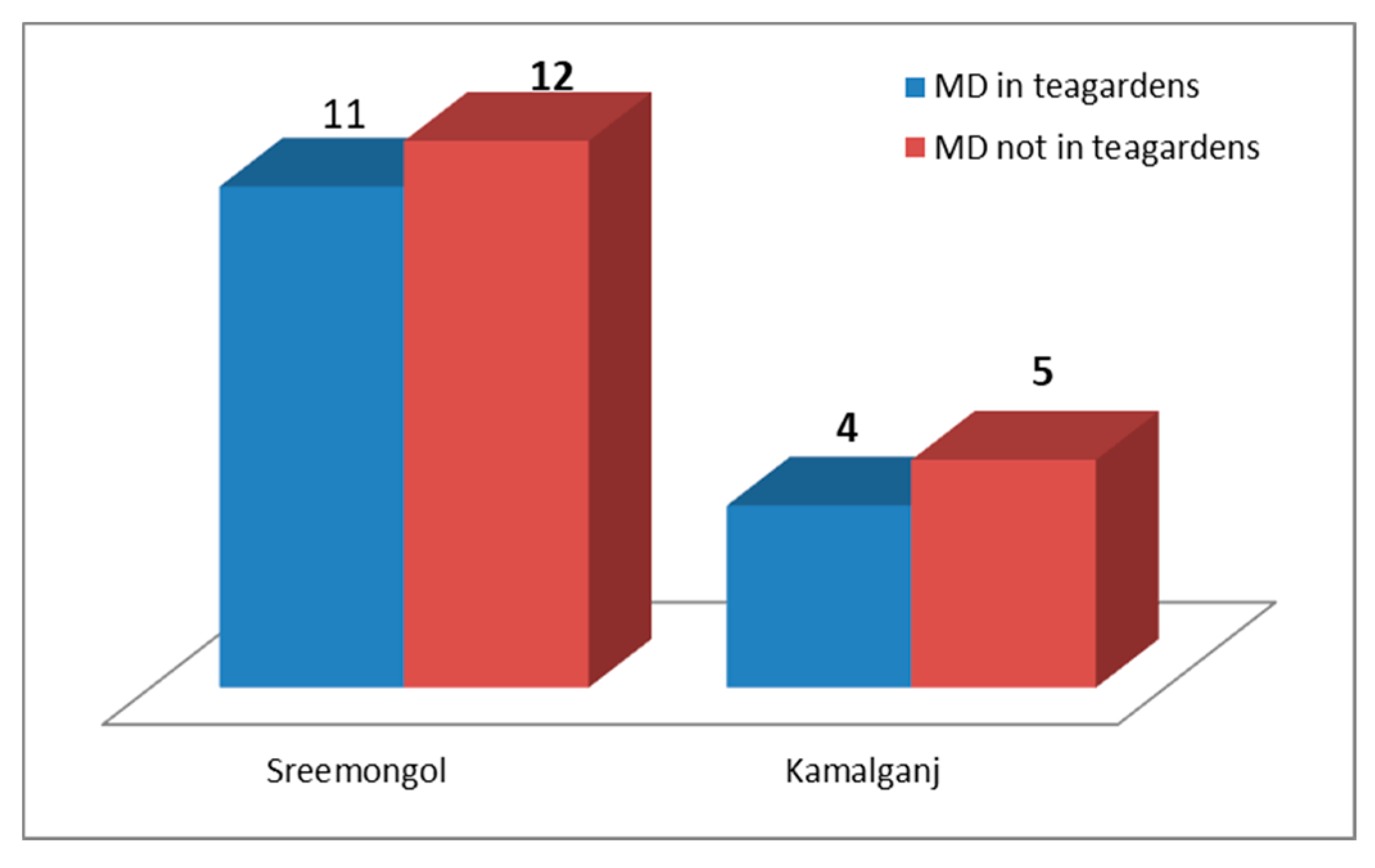
| Upazila | Union | No. of Tea Gardens | No. of Maternal Deaths |
|---|---|---|---|
| Sreemangal | Rajghat | 4 | 7 |
| Sathgaon | 1 | 1 | |
| Kalighat | 1 | 1 | |
| Ashirdrone | 1 | 2 | |
| Kamalganj | Islampur | 1 | 1 |
| Madhabpur | 1 | 1 | |
| Shamshernagar | 1 | 2 | |
| Total | 10 | 15 | |
| Characteristics | Total Deaths (n = 34) | Mothers Who Died in Tea Gardens (n = 15) | Mothers Who Died Outside of the Tea Gardens (n = 19) |
|---|---|---|---|
| Median age of mother in years [Inter Quartile Range] | 27.6 (18–38) | 24.9 (18–30) | 30.3 (20–38) |
| Mother’s education (n [%]) | |||
| Below primary level | 20 (58.8) | 15 (100) | 5 (26.3) |
| Primary education | 8 (23.5) | - | 8 (42.1) |
| Secondary education | 6 (17.7) | - | 6 (31.6) |
| Maternal characteristics | |||
| Accessed ANC four or more times | 11 (32.4) | 4 (26.7) | 7 (33.8) |
| Parity (n [%]) | |||
| 1 | 8 (23.6) | 2 (13.3) | 6 (34.0) |
| 2–4 | 20 (58.8) | 10 (66.7) | 10 (52.2) |
| 5 or more | 6 (17.6) | 3 (20.0) | 3 (14.8) |
| Delays | 15 Maternal Deaths in the Tea Gardens, n (%) |
|---|---|
| 1st delay: Decision to seek care | |
| Within 1 h | 3 (20) |
| 1–2 h | 10 (67) |
| Decided not to go to the facility | 2 (13) |
| 2nd delay: Time to transfer | |
| Within 1 h | 1 (7) |
| 1–2 h | 5 (33) |
| 2–3 h | 3 (20) |
| Could not transfer | 4 (27) |
| No transport | 2 (13) |
| Case | Gestational Period | Complications | Cause of Death | Summary Case Description Obtained from Case Reports |
|---|---|---|---|---|
| Case 1 | 36 weeks | Anemia, Edema, vomiting | Severe Anemia | It was her third pregnancy. She did not receive any ANC during her pregnancy. She was suffering from anemia and swelling of face and legs; it was overlooked by her family members. After delivery at home by TBA, the mother had continuous vomiting. Twelve days after birth, the mother died from anemia, edema and vomiting without getting any treatment. |
| Case 2 | 42 weeks | Anemia, Edema on face and leg | PPH | The mother could not detect her pregnancy for up to six months. Though she was suffering from severe abdominal pain, she attributed it to hard work. She never received any antenatal care and delivered at home by TBA. Immediately after delivery, PPH started, and she died at home. |
| Case 3 | 38 weeks | Eclampsia, Prolonged labor with PPH | PPH | It was her second pregnancy. The mother was suffering from severe headaches due to pre-eclampsia during pregnancy. But all family members ignored these issues. She had labor pain for more than 19 h, but the TBA tried to conduct the delivery in the traditional way. After delivery PPH started and the mother died at home. |
| Case 4 | 30 weeks | Anemia, Edema | PPH | It was her third pregnancy, and she had a previous history of miscarriage. She suffered from anemia and preeclampsia. She received two ANC visits at the tea garden hospital. She was advised to deliver at a facility, but her family members decided to conduct the delivery at home by TBA. PPH started immediately after birth, and the mother died at home. |
| Case 5 | 31 weeks | Anemia, Edema | Severe anemia | Though it was her third pregnancy, the mother and her family members were unaware of maternal health care. She did not receive any ANC during pregnancy and did not take any essential medicine. Her face and legs became swollen at the fifth month of pregnancy. After delivery at home by TBA, the mother died at home from severe anemia. |
| Case 6 | 32 weeks | Edema, Unconsciousness | Severe anemia | It was her fifth pregnancy, and she suffered from swelling of the face and limbs. Though she received one ANC visit during pregnancy, she did not follow the given advice. She delivered at home by TBA. The mother died at home after five hours of delivery. |
| Case 7 | 32 weeks | Retention of placenta with PPH | PPH | It was her first pregnancy, and delivery pain started at midnight while she was at home. Her husband called the TBA, who tried and delivered a baby on the morning around 6.30 am. Unfortunately, PPH began to due to the retained placenta. She was carried to Bagan hospital where a paramedic (Bagan Midwife) attempted to treat her. Then at 9 am, she was referred to the tea garden central hospital and later Osmani Medical College Hospital at 11 am, but the mother died on the road at noon. |
| Case 8 | 38 weeks | Anemia, Edema on face and leg | Severe anemia | The family members believed myths that delivery should be conducted at home because if a pregnant woman went outside, it would be bad for her pregnancy. After birth at home by TBA, her face and limbs became swollen and her abdomen distended with frothy discharge coming out of her mouth. They then carried the mother to the tea garden hospital. But the paramedic and compounder could not detect the problem. Then they decided to come back home, and the mother died on the road. |
| Case 9 | 30 weeks | Severe anemia, Retained placenta, PPH | PPH | The mother was identified as high risk with severe anemia during her first ANC visit at the tea garden hospital by a paramedic (Bagan midwife). She and her husband were counseled on the importance of pregnancy care. She went to her mother’s home at the sixth month of pregnancy and could not receive other ANC. After delivery by TBA, the placenta could not be removed, resulting in severe PPH. Then she was carried to the tea garden hospital where she was referred to UHC. She died on the road on the way to UHC. |
| Case 10 | 31 weeks | Prolonged labor with PPH | PPH | It was her first pregnancy. The mother was admitted to UHC with obstructed prolonged labor and delivered a baby by caesarian section. But PPH started immediately after delivery, and then the mother was referred to the district hospital. But the family members decided to admit her in the private hospital in that sub-district. However, this hospital could not manage the complications and referred the mother to Osmani medical hospital. But it took a long time to reach the destination and the mother died just after treatment started at Osmani Medical College Hospital. |
| Case 11 | 32 weeks | Anemia, Edema | PPH | She was suffering from severe headaches. For this complaint, her husband carried her to a traditional healer (Kabiraj) where conventional treatment was provided. After seeking treatment, the mother came to her home but suddenly fell in the yard. Convulsions started and after a while she fell unconscious. Then she was carried to the tea garden hospital, followed by the district hospital and Osmani Medical College Hospital. But she died after the last admission. |
| Case 12 | 28 weeks | Severe headache | Eclampsia | Delivery occurred at home by TBA. The TBA explained that it was challenging to remove the placenta and hemorrhage started during the removal of the placenta with rough handling. After delivery, the mother suffered from anemia, swelling of legs and face. After six days, the mother was referred to UHC from her home by a paramedic, then referred to the District Sadar hospital and then to Osmani Sadar Hospital but the mother died before reaching that facility. |
| Case 13 | 30 weeks | Twin pregnancy | Eclampsia | It was her fourth pregnancy. The last three deliveries occurred at home by TBA, and two of them were stillbirths. Though she felt a headache and abdominal pain, she did not have treatment during this pregnancy. At the time of delivery, she felt severe pain in the abdomen. She did not even know that she was carrying twins. She was taken to the tea garden hospital and then to the district hospital. But immediately after reaching the hospital, the mother died, with convulsions. |
| Case 14 | 29 weeks | Anemia, Edema | PPH | It was her third pregnancy. The mother was suffering from pre-eclampsia and severe anemia during pregnancy. She also suffered from hemorrhoids. Her family members ignored special care during pregnancy. They admitted her into hospital with complications. They delayed in seeking treatment, and the mother died after delivery due to PPH. |
| Case 15 | 30 weeks | Anemia, Abdominal pain, High blood pressure | Severe anemia | It was her fourth pregnancy, and she had a history of miscarriage. She had a symptom of pre-eclampsia (decided by a physician) during pregnancy, but her family members did not take this issue seriously. The mother delivered at home by TBA. PPH started immediately after delivery. Then the mother was carried to Bagan Hospital, later referred to UHC, and finally transferred to the district hospital, and the mother died there. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biswas, A.; Halim, A.; Md. Abdullah, A.S.; Rahman, F.; Doraiswamy, S. Factors Associated with Maternal Deaths in a Hard-To-Reach Marginalized Rural Community of Bangladesh: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 1184. https://doi.org/10.3390/ijerph17041184
Biswas A, Halim A, Md. Abdullah AS, Rahman F, Doraiswamy S. Factors Associated with Maternal Deaths in a Hard-To-Reach Marginalized Rural Community of Bangladesh: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2020; 17(4):1184. https://doi.org/10.3390/ijerph17041184
Chicago/Turabian StyleBiswas, Animesh, Abdul Halim, Abu Sayeed Md. Abdullah, Fazlur Rahman, and Sathyanaraynan Doraiswamy. 2020. "Factors Associated with Maternal Deaths in a Hard-To-Reach Marginalized Rural Community of Bangladesh: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 17, no. 4: 1184. https://doi.org/10.3390/ijerph17041184
APA StyleBiswas, A., Halim, A., Md. Abdullah, A. S., Rahman, F., & Doraiswamy, S. (2020). Factors Associated with Maternal Deaths in a Hard-To-Reach Marginalized Rural Community of Bangladesh: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 17(4), 1184. https://doi.org/10.3390/ijerph17041184




